Abstract
This study examines the relationship between violence exposure and early substance use as mediated by trauma symptoms. The Assessment of Liability and Exposure to Substance Use and Antisocial Behavior Scale was used to assess violence exposure at age 10 and substance use by age 12. Mediation analysis indicated direct relationships between violence exposure and tobacco/illegal drug use and indirect relationships between violence exposure and girls’ substance use through trauma symptoms. Practitioners should consider violence exposure as a risk factor for early substance use in high-risk youths and potential gender differences in trauma symptom pathways to early substance use.
Keywords: substance use/alcohol use and drug use, violence/violent behavior, gender/gender differences, at risk/high risk populations
Early substance use is a potential high priority area for focused social work prevention and intervention. Early substance use occurring by age 13, the age at which approximately 25% of youths have initiated substances (Kroutil, Colliver, & Gfroerer, 2010), has been associated with elevated risk of developing a substance use disorder (Gil, Wagner, & Tubman, 2004; Sung, Erkanli, Angold, & Costello, 2004) and other adverse outcomes (e.g., poor academic performance, psychiatric disorder, suicidal behaviors, and violent/deviant behavior; Breslau, Miller, Chung, & Schweitzer, 2011; Fulwiler, Grossman, Forbes, & Ruthazer, 1997; Sung et al., 2004; Swahn, Bossarte, & Sullivent, 2008). Studies suggest that prenatally drug-exposed youths are at high risk of adverse substance use outcomes (Minnes, Singer, Min, Wu, et al., 2014; Richardson, Larkby, Goldschmidt, & Day, 2013), as well as related problems such as inattention, poor perceptual reasoning, externalizing behavior problems, and impaired executive functioning (Min, Minnes, Lang, et al., 2014; Min, Minnes, Yoon, Short, & Singer, 2014; Minnes et al., 2010; Minnes, Lang, & Singer, 2011; Minnes, Singer, Min, Lang, et al., 2014). Damage to the central nervous system from prenatal substance exposure and associated genetic and environmental factors (e.g., ongoing parental substance use, adverse experiences, and institutional or foster care placements) may place this population at higher risk for ongoing developmental impairment (Minnes et al., 2011), including the sequalae of early substance use. However, the antecedents of early substance use within this vulnerable population, including the potential roles of violence exposure and other environmental risk factors, remain unclear. A better understanding of these antecedents is needed to inform social work prevention and treatment efforts.
Violence Exposure and Substance Use in Prenatally Drug-Exposed Youth
Violence exposure (VE), witnessing or being victim to interpersonal behaviors that intentionally threaten or inflict physical harm (Aisenberg, Gavin, Mehrota, & Bowman, 2001), has been associated with higher risk of substance use in middle adolescence (i.e., 14–16 years) among prenatally drug-exposed youths. Studies focusing on prenatally drug-exposed populations have demonstrated significant associations between VE and cocaine use at 14 years (Delaney-Black et al., 2011); marijuana, alcohol, and any substance use at 16 years (Frank et al., 2011); tobacco, marijuana and any substance use at 15 years (Minnes, Singer, Min, Wu, et al., 2014); and age of marijuana use reported at 15 years (Richardson et al., 2013). General population studies have identified positive associations between VE and early substance use, including cigarette, alcohol, marijuana, and other drugs (e.g., Mrug & Windle, 2009; Sullivan, Farrell, Kliewer, Vulin-Reynolds, & Valois, 2007; Tharp-Taylor, Haviland, & D’Amico, 2009). Only one identified study focusing on early substance use among prenatally cocaine-exposed youth reported no significant VE effects on early cocaine use in 10 ½ and 12 ½ year olds (Warner, Behnke, Eyler, & Szabo, 2011). The relationship between VE and early substance use in prenatally drug-exposed populations, therefore, remains largely unclear and is in need of further study.
Trauma Symptom Pathways to Substance Use
Developmental traumatology suggests that trauma symptoms (i.e., anger, depression, anxiety, dissociation, and posttraumatic stress) mediate the relationship between VE and adolescent substance use. Stressful events are thought to overwhelm the brain’s stress response system, leading to trauma symptoms, with substances then used principally for their anxiolytic properties (De Bellis, 2002; Giaconia et al., 2000; Hovdestad, Tonmyr, Wekerle, & Thornton, 2011). Few studies, however, have utilized mediation analysis to assess the interrelationships among VE, trauma symptoms, and adolescent substance use implied by this theory. Most existing mediation studies have focused on older adolescents, with mixed results. Anger has been found to be a significant mediator between both family conflict/violence and sexual abuse and substance use in 16–19-year-olds (Asgeirsdottir, Sigfusdottir, Gudjonson, & Sigurdsson, 2011). Another study found internalizing symptoms (i.e., depression and anxiety, withdrawal, somatic complaints) to mediate the relationship between child abuse and cigarette smoking in 16-year-olds (Lewis et al., 2011). Others found that externalizing (i.e., aggression and delinquency) but not internalizing symptoms partially mediated the relationship between late childhood family conflict and late adolescent substance use disorder (Skeer, McCormick, Normand, Buka, & Gilman, 2009), or no significant mediation by depression (Asgeirsdottir et al., 2011). Scant mediation studies that include younger adolescents have reported that anger mediates the relationship between relational victimization and combined alcohol, cigarettes, and marijuana use in eighth, tenth, and twelfth graders (Weiner et al., 2004) and that negative affect, an aspect of depression, mediates the relationship between stressful life events and substance use in 10–15-year-olds (Chassin, Pillow, Curran, Molina, & Barrera, 1993). However, similar to other existing mediation studies (e.g., Asgeirsdottir et al., 2011; Skeer et al., 2009), Weiner et al., (2004) and Chassin et al. (1993) used broad measures of traumatic exposure that included nonviolent forms of victimization.
Violence Exposure and Early Substance Use
Some scholars maintain that VE and other forms of potential trauma are particularly salient to early substance use (Tonmyr, Thornton, Draca, & Wekerle, 2010; Whitesell, Bachand, Peel, & Brown, 2013), suggesting the need for studies focused on younger adolescent populations. Supporting this perspective is evidence that victimized youths use substances earlier than other youths (Kaufman et al., 2007; Kilpatrick et al., 2000) and evidence of statistically stronger relationships between adverse experiences, including physical abuse/VE and earlier substance use initiation (Anda et al., 1999; Dube et al., 2003, 2006). Studies of younger adolescents have also connected higher levels of trauma symptoms to VE (Flannery, Wester, & Singer, 2004; Lambert, Nylund-Gibson, Copeland-Linder, & Ialongo, 2010; Mrug & Windle, 2010; Singer, Flannery, Guo, Miller, & Leibbrandt, 2004) and substance use risk (Costello, Erkhanli, Federman, & Angold, 1999; King, Iacono, & McGue, 2004; Loeber, Stouthamer-Loeber, & White, 1999). However, there have been inconsistent findings in the relationships between internalizing symptoms and early substance use. Some studies have associated depression and internalizing symptoms with increased risk for early substance use (Costello et al., 1999; King et al., 2004; Loeber et al., 1999). Others have reported no relationship between depression and internalizing symptoms and early substance use (Clark, Parker, & Lynch, 1999) or protective effects (Chassin et al., 1993; Colder et al., 2013). However, these inconsistent studies have not assessed the role of VE. Additional research is needed to clarify the relationships among various trauma symptoms, VE, and early substance use.
Gender Differences in Trauma Pathways to Substance Use
Potential gender differences in trauma pathways to early substance use have been suggested by theory and empirical studies. Girls’ sensitivity to relational harm and earlier cognitive development may lead to unique vulnerabilities to the effects of VE (Zahn-Waxler, Shirtcliff, & Marceau, 2008). Alternatively, differences in levels or types of girls’ and boys’ stress exposure could lead to disparate responses (Tolin & Foa, 2006; Zahn-Waxler et al., 2008). Gender differences in the relationship between VE and trauma symptoms are relatively well established, with meta-analyses identifying stronger positive effects of violence exposure in girls than boys on anxiety/depression (Fowler, Tompsett, Braciszewski, Jacques-Tiura, & Baltes, 2009) and posttraumatic stress (Tolin & Foa, 2006). Statistically stronger associations for girls between VE and dissociation have been identified (Zona & Milan, 2011). Further studies have found associations between VE and substance use solely in girls (Lansford, Dodge, Pettit, & Bates, 2010; Tharp-Taylor et al., 2009). A mediation analysis found that the number of clinical trauma symptoms mediated the relationship between maltreatment and marijuana use only in girls (Wekerle, Leung, Goldstein, Thonton, & Tonmyr, 2009). However, another mediation analysis reported stronger effects of sexual abuse on depressed mood in girls, but direct effects of family conflict/violence on substance use in boys (Asgeirsdottir et al., 2011).
Studies examining gender differences in the relationship between trauma symptoms and substance use have been mixed. Several studies have found exclusive or stronger effects of depression and posttraumatic stress on substance use in girls (Acierno et al., 2000; Fleming, Mason, Mazza, Abbott, & Catalano, 2008; Lipschitz, Grilo, Fehon, McGlasha, & Southwick, 2000). However, another study found that depression predicted earlier age of onset for alcohol use in girls only, but earlier age of onset of any substance use, marijuana use, and substance abuse or dependence in boys only (Costello et al., 1999). Furthermore, depression predicted smoking, alcohol, marijuana, and other drug use by age 16 only in boys (Costello et al., 1999). A study of younger adolescents reported no significant gender differences in the associations between internalizing and externalizing pathology and early substance use (Colder et al., 2013). Other research reported stronger relationships between externalizing pathology and early heavy drinking in males but no gender differences in the relationship between internalizing pathology and early substance use, noting the limitation that anxiety was measured only in girls (King et al., 2004). In an examination of the effects of various dimensions of anxiety and early alcohol initiation, no significant Gender × Anxiety interaction effects were found (Kaplow, Curran, Angold, & Costello, 2001).
Overall, research examining gender differences suggests stronger relationships between VE and trauma symptoms in girls, as well as possible gender differences in the relationship between VE and early substance use. Gender differences in the relationship between trauma symptoms and early substance and potential mediating role of trauma symptoms in the VE-early substance use relationship remain unclear.
Potential Confounds
The inconsistent evaluation of potential confounds beyond basic demographic variables such as age, gender, and race/ethnicity limits current research examining the relationships among VE, trauma symptoms, and early substance use. In particular, with some notable exceptions (i.e., Chassin et al, 1993; Costello et al., 1999; Singer et al., 2004; Warner et al., 2011), there is a paucity of early substance use studies evaluating parental or home environment factors as potential confounds. Parental substance use (Acierno et al., 2000; Anda et al., 1999; Chassin et al., 1993; Dube et al., 2003, 2006; Kilpatrick et al., 2000) and psychological distress (Anda et al., 1999; Dube et al., 2003, 2006) are commonly observed as risk factors for adolescent substance use. Additionally, parental education (Whitesell et al., 2013), the quality of the home environment (Warner et al., 2011), and instrumental and affective parental controls (i.e., parental monitoring and attachment; Branstetter, Furman, & Cottrell, 2009; Chassin et al., 1993; DiClemente et al., 2001; Fagan, Van Horn, Hawkins, & Jaki, 2012; Sullivan, Kung, & Farrell, 2004; Whitesell et al., 2013) are identified protective factors.
Prenatally drug-exposed populations experience high rates of placement into out-of-home care, an additional potential confound for this high-risk population (Minnes, Singer, Min, Wu, et al., 2014). Youths in out-of-home placement may experience protection from substance use because of improved environmental conditions. Alternatively, factors such as maltreatment exposure, behavioral problems, estrangement from the biological family, and transitions in caregiver relationships may present additional substance use risk among these youths (Aarons et al., 2008). Among youths placed in out-of-home care, the number of placements has been associated with greater risk of substance use (Aarons et al., 2008; Stott, 2012).
Research Questions
This study sought to elucidate the development of substance use problems and disorder and inform social work practice in the addictions by examining substance use by 12 years in a high-risk (i.e., poly-drug-exposed, low-SES) sample. Specifically, it examined the relationship between VE and early substance use among boys and girls in this population, and the potential mediating role of trauma symptoms (anger, depression, anxiety, posttraumatic stress, and dissociation). The research questions were as follows: (1) Does VE significantly relate to substance use (alcohol and tobacco/illegal drug use) by 12 years among high-risk youths? (2) Do trauma symptoms mediate the relationship between VE and early substance use in this population? (3) Do potential mediation patterns vary by gender?
Method
Participants and Procedures
This study included 297 adolescent-caregiver dyads who participated in 10-, 11-, and 12-year assessments in a longitudinal study about the developmental effects of prenatal cocaine/poly-drug exposure. The sample was recruited from September 1994 to August 1996 starting at birth from a hospital in a large Midwestern city serving a low-income population. Dyads with mothers who lacked prenatal care, admitted to drug use, exhibited behavior characteristic of intoxication, or who had a history of involvement with the Department of Health of Human Services were eligible for the study. Dyads with mothers with diagnosed psychiatric conditions, mental retardation, HIV infection, or chronic medical conditions or whose infants had Down syndrome, fetal alcohol syndrome, or medical conditions were excluded.
Informed consents approved by the affiliated hospital’s Institutional Review Board and baseline assessments were completed with mothers at the time of birth or shortly after. Toxicology screens, maternal self-report, infant and mother urinalysis, and meconium analysis were used to determine prenatal cocaine exposure status. Subsequent assessments lasted approximately 5 hours and were conducted in a child development laboratory at 2, 4, 6, 9, 10, 11, and 12 years with current caregivers and children. Stipends of $100 ($50 for caregivers and $50 for children) as well as lunch and reimbursement for transportation costs were provided at the 12-year assessment. The current study used data from the assessments at baseline (birth), 9, 10, 11, and 12 years.
Measures
Violence Exposure
Lifetime VE was assessed at age 10 using the Assessment of Liability and Exposure to Substance Use and Antisocial Behavior Scale (ALEXSA), an illustration-based, audio, computer-assisted child self-report interview that measures early manifestations and predictors of substance use and antisocial behaviors (Ridenour, 2003). The ALEXSA has been demonstrated to have excellent test-retest reliability, construct validity, criterion validity, and cross-cultural equivalence (Ridenour et al., 2011; Ridenour, Clark, & Cottler, 2009; Ridenour, Meyer-Chilenski, & Reid, 2012). The VE scale contains eight items: ever witnessing/experiencing a beating, being chased or threatened, a robbing or mugging, and a stabbing or shooting, alpha (∝) = .74. Items are rated on a 5-point scale ranging from 0 times to 5 times with higher scores indicating greater VE. Average scores (potential range, 0–5) were used.
Youth Substance Use
Substance use was measured by a 5-item scale on the ALEXSA, collected at ages 9, 10, 11, and 12 (ever drank alcohol, even just a sip; ever used hard drugs/ inhalants/ tobacco/ marijuana; ever just to try it) and by child self-report three items from the Youth Risk Behavior Surveillance Survey (YRBSS; Centers for Disease Control and Prevention, 2009), collected at age 12 (in the last 12 months have you drunk alcohol (even one drink)/smoked a cigarette/used any illegal drug). Categorical variables were created based on any endorsement of alcohol use and tobacco/illegal drug use by age 12. The frequencies for tobacco use (8.8%) and illegal drug use (5.0%) alone were insufficient for reliable logistic regression analysis.
Trauma Symptoms
Trauma symptoms were measured by the Trauma Symptom Checklist for Children (TSCC) at 11 years (Briere, 1996). The TSCC consists of 54 items that the child rates as happening on a 4-point Likert scale ranging from 0 (never) to 3 (almost all the time). T scores of the instrument’s five major clinical scales were used (anxiety, 9 items, potential range: 32–106; depression, 9 items, potential range: 32–101; anger, 9 items, potential range: 33–86; posttraumatic stress, 10 items, potential range: 33–91; and dissociation, 10 items, potential range: 35–96). The TSCC has been demonstrated to have excellent internal reliability, ranging from α = .82 for anxiety to α = .89 for anger, and convergent, discriminant, and construct validity (Briere, 1996).
Covariates
Parental attachment and monitoring were assessed by ALEXSA scales at 10 years (Ridenour, 2003). The parental attachment scale included six items rated on a 4-point Likert scale ranging from 0 (none) to 3 (all). The scale has strong internal consistency (∝ = .81). Questions included how often the parent listened to and understood the child, and how often the child trusted the parent, could count on the parent for help with a problem, and shared thoughts and feelings with the parent. The parental monitoring scale (∝ = .70) included 5 items probing for how often the parent knows things the child buys, what child does in free time, where the child is going when he or she leaves home, when the child will be back, and how often the child checks in with the parent. Responses for both scales were rated on a 4-point Likert scale ranging from 0 (none of the time) to 3 (all of the time). Average scores were used (potential range: 0–3), with higher scores indicating more parental monitoring/attachment.
Quality of the home environment was measured by caregiver report at 11 years by the early adolescent version of the Home Observation and Environment (HOME) scale (Caldwell & Bradley, 2003). A total sum score of 60 items (yes = 1, no = 0) was computed. Higher scores indicated higher home quality (potential range: 0–60; α = .75). Baseline birthmother and current (11-year) caregiver psychological symptom severity was measured by caregiver report to the Global Severity Index of the Brief Symptom Inventory (BSI; α = .95; Derogatis & Melisaratos, 1983). Current caregiver substance use, including amount and frequency of cocaine, tobacco, alcohol, and marijuana, were measured by caregiver self-report to an adaptation of the Maternal Post-Partum Interview (Singer et al., 2002; Streissguth, 1986). Biological substance exposure measures were also collected at baseline to determine prenatal cocaine/poly-drug exposure and other prenatal substance exposure, including maternal tobacco, alcohol, marijuana, hashish, valium, amphetamine, barbiturates, LSD, heroin, and PCP use (Singer et al., 2004). Half (51.5%, n = 153) of the study sample were prenatally cocaine-exposed. Sizeable portions of the overall sample were prenatally exposed to maternal drinking (76.9%, n = 220), tobacco (64.0%, n = 183) and marijuana (32.5%, n = 93). On average, children were exposed to 2.36 substances (SD = 1.48) and almost all of the children (87.9%, n = 261) were prenatally exposed to one or more substances. Demographic measures included youth race and gender, which were extracted from hospital records at birth; current caregiver age and education in years; whether the youth was ever in nonkinship adoptive or foster care by the 11-year interview; and number of placements.
Statistical Analyses
The distribution of all variables was assessed to check normality assumptions. Because the large number of strongly intercorrelated potential covariates would cause multicollinearity, a two-stage process was used to select covariates that were most likely to confound the VE-substance use relationship (Minnes, Singer, Min, Wu, et al., 2014). First, zero-order Pearson correlation analysis was conducted to identify variables with bivariate relationships to both VE and substance use (alcohol and tobacco/illegal drug use) at the p < .20 level (Mickey & Greenland, 1988). Second, potential covariates were entered individually into a logistic regression model with gender and VE, and those that were significant at p < .10 and/or affected the VE coefficient by ≥ 10% were retained. Using these criteria, different sets of covariates were selected for different outcomes; parental monitoring and home quality were retained as covariates for tobacco/illegal drugs, whereas parental attachment, parental monitoring, and adoptive/foster care placement were retained as covariates for alcohol. “Alcohol” and “tobacco/illegal drug” subscripts denote statistical results adjusted for these respective covariates. Notably, prenatal cocaine exposure was not included as a covariate because, consistent with past findings of the study sample (Minnes, Singer, Min, Wu, et al., 2014), it was unrelated to substance use by 12 years at p < .20.
The direct effect or relationship between VE and substance use without consideration of mediators (research question 1) was assessed through logistic regression analyses. Mediation analysis testing the indirect effects of VE on substance use through trauma symptoms (research questions 2 and 3) was conducted using the distribution of the product of the coefficients method according to the recommendations of MacKinnon, Lockwood, Hoffman, West, and Sheets (2002). This method improves upon Baron and Kenny’s (1986) approach by reducing Type II error (MacKinnon et al., 2002). It has three steps, (a) analyzing the association between independent and hypothesized mediating variables (path a), (b) analyzing the association between hypothesized mediating and dependent variables, adjusting for the independent variable (path b), and (c) computation of the joint significance of paths, or indirect effect (path ab). These methods were applied to the current study by using multiple linear regression analysis to predict trauma symptoms based on VE and covariates (path a), and binary logistic regression analysis to predict the odds of alcohol use and tobacco/illegal drug use based on trauma symptoms, VE, and covariates (path b). The joint significance of paths leading from VE to trauma symptoms (depression, anxiety, anger, dissociation, and posttraumatic stress), and from trauma symptoms to substance use (alcohol use and tobacco/illegal drug use) were then tested using the RMediation package, which calculates confidence intervals of indirect effects (Tofighi & MacKinnon, 2011). Confidence intervals that do not encompass 1 are statistically significant. Multicollinearity was assessed using tolerance levels and the variance inflation factor (Allison, 1999). Cross-tabulations were run to check for sparse cells. Initially, regression analyses were run with both genders together, testing for 2-way (Gender × VE, Gender × Trauma Symptoms) and 3-way (Gender × VE × Trauma Symptoms) interactions to determine whether gender-separate analyses were appropriate. Independent t-test and chi-square analyses were used to test for gender differences on all variables.
Results
Preliminary Findings
In preliminary, one-group regression analysis evaluating gender differences, VE was significantly related to depression (Balcohol = 2.62, SE = .82, p = .002; Btobacco/illegal drug = 2.44, SE = .82, p = .003); posttraumatic stress (Balcohol = 2.35, SE = .81, p = .004; Btobacco/illegal drug = 2.39, SE = .82; p = .004); anxiety (Balcohol = 3.46, SE = .86, p < .001; Btobacco/illegal drug = 3.54, SE = .86; p < .001); anger (Balcohol = 4.87, SE = .77, p < .001; Btobacco/illegal drug = 4.56, SE = .78; p < .001); and dissociation (Balcohol = 2.39, SE = .83, p = .004; Btobacco/illegal drug = 2.23, SE = .84; p = .009). There were two significant VE × Gender interaction effects on trauma symptoms, with VE significantly related to depression and posttraumatic stress exclusively in girls. VE had direct effects on tobacco and/or illegal drug use (OR = 2.39, 95% CI = 1.55, 3.67), but not alcohol use. Anxiety (OR = 1.05, 95% CI = 1.01, 1.08), anger (OR = 1.06, 95% CI = 1.02, 1.10) and posttraumatic stress (OR = 1.05, 95% CI = 1.01, 1.08) predicted tobacco/illegal drug use. Depression (OR = 1.04, 95% CI=1.003, 1.08) predicted alcohol use, and there was a significant interaction term between depression and gender on alcohol, with higher depressive symptoms associated with higher odds of alcohol use in girls only. Given indications of gender differences among VE, trauma symptoms, and substance use from significant interaction effects and the extant literature, all analyses were assessed for boys and girls separately.
Sample Characteristics
Half of the study sample (52.3%, n = 157) were girls. The sample was predominantly African American (82.5%, n = 245). Of the children in adoptive/foster care placements (12.1%, n = 36), most (91.7%, n = 33) were adopted. Total VE scores ranged from 0 to 5.0 (M = .50, SD = .7). The VE distribution was skewed to the right, with no VE reported by 120 (40.4%) and a median of .14 (IQR: 0, .75). Average scores were 2.30 (SD = .62) for parental attachment, 2.45 (SD = .65) for parental monitoring, and 46.7 (SD = 6.9) for home quality. Average trauma symptoms scores ranged from 46.5 (SD = 10.5) for depression to 51.9 (SD = 10.6) for dissociation. The percentages of children reporting clinically elevated (≥ 65) trauma symptoms were as follows: 6.4% posttraumatic stress (6.4% boys, 6.4% girls, χ = .00, ns); 7.1% depression (8.3% boys, 5.7% girls, χ = .74, ns); 7.7% anger (5.0% boys, 10.2% girls, χ = 2.79, ns); 10.1% anxiety (7.9% boys, 12.1% girls, χ = 1.47, ns); and 11.1% dissociation (10.0% boys, 12.1% girls, χ = .33, ns). By age 12, nearly a third (31.6%, n = 94) reported using any substances, 27.3% (n = 81) reported any alcohol use, and 11.4% (n = 34) reported tobacco or illegal drug use. Among those reporting substance use, 21 (22.3%) reported both alcohol and tobacco/illegal drug use.
Table 1 shows descriptive statistics and zero-order correlations by gender. Parents reported significantly better home quality for girls (p = .03) and girls reported significantly greater parental monitoring (p = .002). Posttraumatic stress and dissociation are not displayed because no significant mediation for these trauma symptoms was found. Multiple regression analysis found significant relationships between VE and both posttraumatic stress and dissociation in girls, but only between posttraumatic stress and tobacco/illegal drug use in boys.
Table 1.
Descriptive Information and Correlation Matrix of Final Model Variables (n =297)
| Girls, M(SD)/%(n) |
Boys, M(SD)/%(n) |
1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. VE | .42 (.63) | .58 (.82) | - | −.064 | −.043 | −.174* | −.059 | .301** | .376** | .315** | .077 | .216** |
| 2. HQ | 47.4 (5.5) | 45.9 (6.4) | −.172* | - | .116 | .062 | −.022 | −.147 | −.074 | .082 | .019 | −.012 |
| 3. PA | 2.34 (.60) | 2.24 (.64) | −.176* | .037 | - | .334** | .065 | −.126 | −.256** | −.116 | −.176* | −.039 |
| 4. PM | 2.56 (.58) | 2.33 (.69) | −.065 | .002 | .172* | - | .020 | −.153 | −.243** | −.202* | −.173* | −.128 |
| 5. A/FC | 12.7% (20) | 11.4% (16) | −.124 | .223** | −.015 | .028 | - | −.054 | .098 | −.057 | .019 | .051 |
| 6. Depression | 47.6 (11.1) | 45.2 (9.7) | .125 | −.131 | −.020 | −.235** | .012 | - | .500** | .572** | .209** | .190* |
| 7. Anger | 48.6 (10.9) | 47.0 (9.8) | .344** | −.267** | −.061 | −.020 | −.074 | .323** | - | .401** | .179* | .298** |
| 8. Anxiety | 49.2 (11.1) | 48.2 (10.9) | .189* | −.081 | −.049 | −.082 | −.010 | .472** | .373** | - | .202* | .181* |
| 9. Alcohol | 22.9% (36) | 32.1% (45) | .113 | −.053 | −.193* | −.145 | .185* | −.036 | .043 | −.007 | - | .249** |
| 10. Tobacco/ Illegal Drugs | 10.8 % (17) | 12.1% (17) | .384** | −.322** | −.062 | −.173* | −.134 | .169* | .264** | .251** | .306** | - |
Note. Girls shown above the diagonal, boys shown below the diagonal. HQ = Home Quality, PA = Parental Attachment, PM = Parental Monitoring, A/FC = Adoptive/Foster Care.
p < .05;
p < .01;
p < .001.
Bivariate correlation analysis showed that higher VE was associated with higher levels of depression, anger, and anxiety in girls, and anxiety and anger in boys. For both genders, VE was correlated with higher tobacco/illegal drug use but not alcohol use. Furthermore, VE was associated with lower home quality and parental attachment in boys and lower parental monitoring in girls.
Depression, anger, and anxiety were correlated with alcohol use in girls only and with tobacco/illegal drug use in both boys and girls. Adoptive/foster care status was correlated with higher home quality, but also higher alcohol use in boys. Parental attachment was correlated with lower alcohol use in both genders and parental monitoring was associated with lower alcohol use in girls only.
Relationship Between Violence Exposure and Substance Use (Research Question 1)
Logistic regression analyses without the hypothesized trauma symptom mediators were initially run to assess the direct relationship between VE and alcohol and tobacco and/or illegal drug use by 12 years. As illustrated in Table 2, no significant direct relationships between VE and alcohol use were found for boys or girls. However, greater VE significantly related to tobacco/illegal drug use for both boys and girls. Furthermore, in boys, adoptive or foster care status was a risk factor for alcohol use (OR = 3.19, 95% CI = 1.03, 9.92, p = .045) and higher home quality was protective of tobacco/illegal drugs use (OR = .86, 95% CI = .78, .95, p = .003).
Table 2.
Regression Analysis Assessing the Relationships Among Violence Exposure, Trauma Symptoms, and Early Substance Use (n =297)
| Alcohol | Tobacco/Illegal Drugs | |||||||
|---|---|---|---|---|---|---|---|---|
| Boys | Girls | Boys | Girls | |||||
| B / OR | SE B/95% CI | B / OR | SE B/95% CI | B / OR | SE B/95% CI | B / OR | SE B/95% CI | |
| VE to SU | 1.33 | 84, 2.11 | 1.22 | .68, 2.19 | 2.73** | 1.44, 5.18 | 2.08* | 1.09, 3.97 |
| VE to Depression | 1.41 | 1.00 | 4.88** | 1.39 | 1.08 | .99 | 4.65** | 1.38 |
| VE to Anxiety | 2.45* | 1.11 | 5.05*** | 1.39 | 2.36* | 1.10 | 5.08*** | 1.37 |
| VE to Anger | 4.02*** | .99 | 6.24*** | 1.28 | 3.51*** | .92 | 5.87*** | 1.31 |
| Depression to SU | .98 | .94, 1.02 | 1.04* | 1.01, 1.08 | 1.02 | .96, 1.08 | 1.03 | .99, 1.08 |
| Anxiety to SU | .99 | .96, 1.03 | 1.04* | 1.01, 1.08 | 1.06* | 1.01, 1.11 | 1.03 | .99, 1.08 |
| Anger to SU | 1.01 | .97, 1.05 | 1.03 | .99, 1.07 | 1.04 | 97, 1.12 | 1.07** | 1.02, 1.12 |
Note. VE = Violence Exposure. SU = Substance Use. Parameter estimates for VE to SU without mediators in the model are displayed. Models predicting alcohol use control for parental monitoring, parental attachment, and adoptive/foster care status. Models predicting tobacco/illegal drug use control for home quality and parental monitoring. Unstandardized coefficients and SEs are presented for paths predicting trauma symptoms. ORs and 95% CIs are presented for paths predicting substance use.
p < .05;
p < .01;
p < .001.
Mediation Analyses (Research Questions 2 and 3)
The relationship between VE and trauma symptoms (path a) was assessed using ordinary least squares multivariate regression analysis. Among girls, VE at 10 years significantly predicted higher levels of depression, anger, and anxiety at 11 years. Among boys, higher VE at 10 years significantly predicted higher levels of anger and anxiety at 11 years, but not depression.
In the next step, logistic regression analysis of VE, trauma symptoms, and covariates on alcohol use and tobacco and/or illegal drug use by 12 years was conducted (path b). Among girls, depression and anxiety were significantly associated with higher odds of alcohol use, and anger was associated with higher odds of tobacco and/or drug use. In boys, these relationships were not significant.
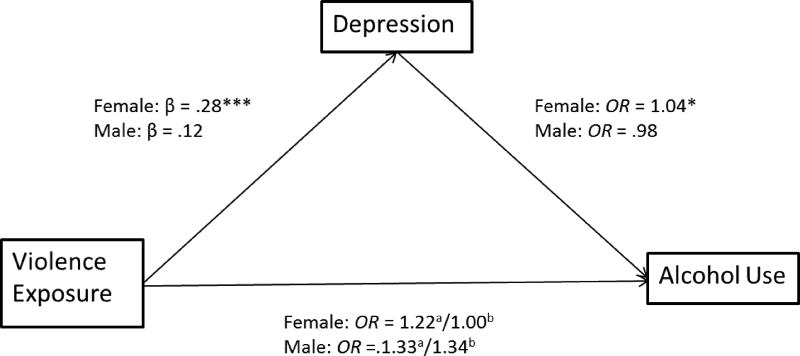
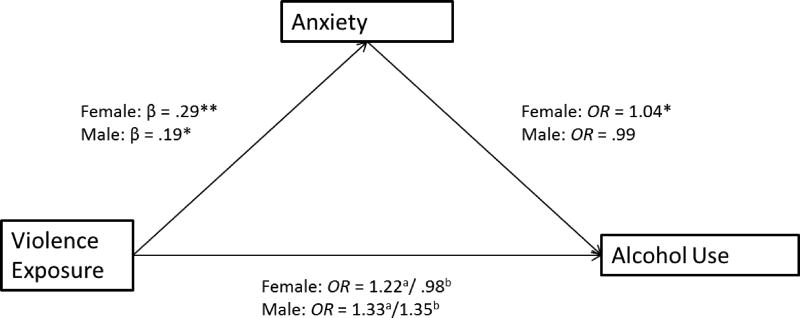
Rmediation analysis calculated indirect effects as the product of estimated coefficients for Path a × Path b, indicating significant indirect effects of VE on alcohol use in girls through both depression (4.89 × .04 = .21, 95% CI = .03, .45) and anxiety (5.05 × .04 = .22, 95% CI = .02, .48). These mediated relationships are summarized in Figures 1 and 2.
Figure 1.
The mediating effect of depression in the relationship between violence exposure and alcohol use.
Standardized estimates are shown. Parameter estimates are adjusted for parental monitoring, parental attachment, and adoptive/foster care status. Superscript a denotes the effect of VE, not controlling for trauma symptoms. Superscript b denotes direct effects of VE, controlling for trauma symptoms. *p<.05; **p < .01; ***p <.001.
Figure 2.
The mediating effect of anxiety in the relationship between violence exposure and alcohol use.
Standardized estimates are shown. Parameter estimates are adjusted for parental monitoring, parental attachment, and adoptive/foster care status. Superscript a denotes the effect of VE, not controlling for trauma symptoms. Superscript b denotes direct effects of VE, controlling for trauma symptoms. *p<.05; **p < .01; ***p <.001.
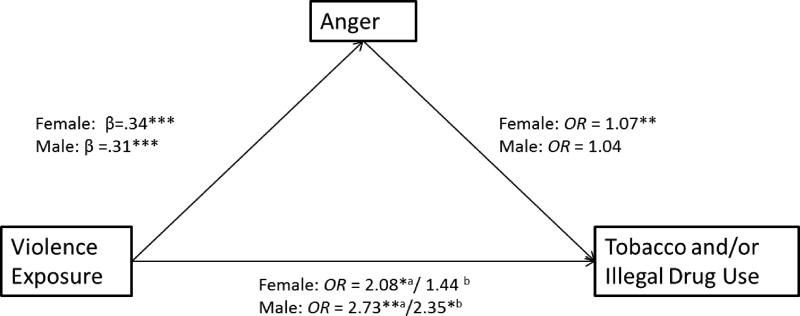
The indirect effect of VE on tobacco/illegal drug through anger in girls was also significant (5.87 × .06 = .37, 95% CI = .08, .73).
Discussion
This study expands upon knowledge of early substance use by examining the relationship between lifetime VE reported at 10 years and alcohol and tobacco/illegal drug use by 12 years among boys and girls in a highly drug-exposed, low-SES, and mostly African American sample. Significant direct relationships between VE and tobacco/illegal drug use in both genders were found, as well as an indirect relationship between VE and alcohol use in girls. The associations between VE and tobacco/illegal drug use in both boys and girls are consistent with past general population research (Acierno et al., 2000; Anda et al., 1999; Dube et al., 2003; Kilpatrick et al., 2000). Indirect paths from VE to alcohol use in girls but not boys have precedent in past general population research that has found significant associations between VE and composite measures of early substance use in girls only (Lansford et al., 2010; Tharp-Taylor, 2009). These findings also corroborate research in prenatally cocaine-exposed samples indicating associations between VE and substance use occurring in middle adolescence (Delaney-Black et al., 2011; Frank et al., 2011; Minnes, Singer, Min, Wu, et al., 2014). The current study’s findings suggest that VE is an important risk factor for early substance use, including alcohol and tobacco/illegal drug use, within this high-risk population. Future research should continue to examine how vulnerabilities related to VE, prenatal drug exposure, and early substance use affect the development of substance use problems over the course of adolescence.
This study also contributes to knowledge of early substance use by suggesting gender differences in the mediation of trauma symptoms in the relationship between VE and alcohol and tobacco/illegal drug use by 12 years. Mediation analysis indicated significant indirect relationships between VE and alcohol use through depression and anxiety and between VE and tobacco/illegal drug use through anger in girls. No significant trauma symptom mediation was found in boys.
Few studies have examined the mediating role of trauma symptoms in the relationship between VE and adolescent substance use. Existing studies have shown significant mediation by anger (Asgeirsdottir et al., 2011; Weiner et al., 2004) but have had mixed results as to the mediating roles of depression, anxiety, and overall internalizing symptoms (Asgeirsdottir et al., 2011; Chassin et al., 1993; Lewis et al., 2011; Skeer et al., 2009). Furthermore, although gender-specific mediation of trauma symptoms has been identified (Wekerle et al., 2009), gender differences in these relationships, particularly in early adolescence, have been understudied. Findings of significant indirect paths in the current study are consistent with the perspective that trauma symptom pathways are relevant to early substance use (Loeber et al., 1999; Tonmyr et al., 2010; Whitesell et al., 2013). However, this study suggests that the trauma symptom pathways to early substance use apply primarily to girls.
The study’s finding of gender-specific mediation resulted from distinct gender patterns in both the VE-trauma symptom (path a) and trauma symptom-substance use (path b) relationships. VE was related to higher levels of all trauma symptoms (anger, anxiety, depression, posttraumatic stress, and dissociation) in girls, but only to anger and anxiety in boys. Depression and anxiety predicted alcohol use, and anger predicted tobacco/illegal drugs use in girls, while only posttraumatic stress related to tobacco/illegal drug use in boys in multivariate analysis. Although these patterns suggest gender differences, caution is warranted in interpreting these findings as parameter estimates among most paths were similar. However, findings of Gender × VE interaction effects on depression and Gender × Depression interaction effects on alcohol indicate statistical gender differences in the VE - alcohol relationship as mediated by depression. Future research is needed to investigate these potential gender differences and to determine the potential mediators of the associations between VE and substance use in boys, including aggression and other externalizing problems, which are more common in boys (Zahn-Waxler et al., 2008).
These findings extend past research showing gender-specific mediation (Wekerle et al., 2009), gender moderation in the relationship between VE and trauma symptoms (Fowler et al., 2009; Tolin & Foa, 2006; Zona & Milan, 2011), and stronger relationships between trauma symptoms and substance use in girls (Acierno et al., 2000; Fleming et al., 2008; Lipschitz et al., 2000) to a high-risk 12 year-old sample. They are consistent with the theory that girls show differential responses to traumatic exposure (Zahn-Waxler et al., 2008) and that early substance use in girls is more closely linked to traumatic exposure (Lansford et al., 2010). VE may have stronger associations with trauma symptoms in girls because of their higher levels of social attunement and sensitivity, the importance placed on interpersonal relationships, or vulnerability related to their relatively high cognitive maturity (Zahn-Waxler et al., 2008). However, differential exposure, including differential rates of poly-victimization in girls or other meaningful differences in the level or nature of victimization not captured by the VE measure in this study could explain findings of disparate responses among girls. In particular, girls’ higher exposure to sexual maltreatment may explain apparent gender differences in trauma symptom pathways to substance use. However, results of other studies have suggested that gender differences in levels and types of trauma experienced do not fully explain gender disparities in psychological response (Tolin & Foa, 2006).
Although trauma symptoms did not mediate the relationship between VE and substance use in boys, VE was connected to boys’ early tobacco/illegal drug use, anxiety, and anger. Additionally, adoptive/foster care status was a significant risk factor for alcohol use, and home quality was a protective factor for tobacco/illegal drug use among boys. Although it is unclear why adoptive/foster care status and home quality did not significantly predict substance use in both genders, it may be meaningful that individual-level factors (trauma symptoms) were significant predictors of alcohol and tobacco/illegal drug use in girls, whereas home environment factors (adoptive/foster care placement and home quality) were significant predictors in boys. The risk associated with adoptive/foster care could indicate vulnerabilities associated with earlier traumatic exposure in boys or stress associated with being removed from the biological family’s care.
The current study has several strengths and limitations to consider in interpreting results. The rich, longitudinal dataset from which the study was drawn allowed for the evaluation of many potential confounds in the relationship between VE and early substance use. Furthermore, the use of the TSCC allowed for a relatively nuanced examination of a variety of potential responses to trauma. The utilization of mediation analysis also provided an improved understanding of the interrelationships among VE, trauma symptoms, and substance use. Furthermore, the distribution of the product of coefficients approach to mediation analysis is less prone to Type 2 error than Baron and Kenny’s (1986) method. The prospective measurement of substance use is an improvement from the many previous studies’ reliance on retrospective report. Finally, the ability to examine VE and trauma symptoms as continuous versus categorical variables may have captured more variability.
Study Limitations
The limitations of the current study include the challenges of studying early substance use as a low-frequency, sensitive behavior. Self-report measures are prone to misreporting because of social desirability bias. This study utilized a liberal measure of alcohol use, which included sips of alcohol, which could have affected results. Furthermore, low frequencies of tobacco and illegal drug use required a variable combining these substances, which could have masked meaningful substance type differences. Future research, including research using biological substance measures using hair and urinalysis, is needed to confirm findings and to further examine substance type differences. Finally, given our regionally recruited high-risk sample, external generalizability is a concern.
Although repeated data collection of the substance use variables at four time points provided adequate group sizes to conduct reliable logistic regression analysis of alcohol use and tobacco/illegal drug use, it may raise questions about sequential ordering for youths reporting substance use at ages 9 and 10. This affected only a portion of tobacco/illegal drug users (5 at age 9, 6 at age 11) and alcohol users (16 at age 9, 13 at age 10). The use of a lifetime as opposed to past-year measure of VE at age 10 also somewhat mitigates this concern. Nonetheless, alternative directional relationships are feasible. For example, substance use may interfere with healthy coping, making exposed individuals more vulnerable to trauma symptoms (Giaconia et al., 2000). Substance use also may place adolescents at risk for VE (Brady, Tschann, Pasch, Flores, & Ozer, 2008), or this relationship could be bidirectional (Begle et al., 2011; Brady et al., 2008). Ongoing VE after the 10-year assessment could explain associations with trauma symptoms and substance use in the current study. Future studies focused on these questions of sequential ordering and chronic VE are needed.
Future research utilizing other samples, including those of other populations, is needed to clarify the generalizability of these findings and to examine the relationships among VE, trauma symptoms, and substance use later in adolescence. Studies examining the associations between a wider range of victimization experiences over the course of childhood are needed to further understand the possible effects of early, concurrent, and polyvictimization on early substance use and to more thoroughly assess differential exposure theories of gender differences. Future research should also more thoroughly examine issues related to trauma symptom co-occurrence and potential confounding genetic effects in the VE-early substance use relationship.
Conclusion
The current study’s findings have implications for clinical practice. Most notably, this study suggests the importance of early screening and treatment of youths for VE, trauma symptoms, and substance use. In assessing substance use and risk in a clinical setting, this study implies that a trauma-informed approach with consideration of both potential VE and trauma symptoms is appropriate. It suggests the importance of violence prevention in impeding the development of substance use problems within prenatally drug-exposed populations. Populations at high risk for VE are in need of targeted gender-sensitive therapy to treat and prevent potential trauma symptoms and substance use. In particular, violence-exposed girls may benefit from learning coping strategies to prevent anxiolytic use of substances and the ongoing development of substance use problems. Finally, given our sample demographics, therapeutic approaches that are cognizant and sensitive to issues of race and culture are warranted.
Figure 3.
The mediating effect of anger in the relationship between violence exposure and tobacco and/or illegal drug use.
Standardized estimates are shown. Parameter estimates are adjusted for home quality and parental monitoring. Superscript a denotes the effect of VE, not controlling for trauma symptoms. Superscript b denotes direct effects of VE, controlling for trauma symptoms. *p<.05; **p < .01; ***p <.001.
Acknowledgments
Funding support for this project was provided by grant number NIDA R01 07957 from the National Institute of Drug Abuse.
Contributor Information
Julia M. Kobulsky, Doctoral Candidate, Mandel School of Applied Social Sciences, Case Western Reserve University, Cleveland, OH, USA
Sonia Minnes, Associate Professor, Mandel School of Applied Social Sciences, Case Western Reserve University, Cleveland, OH, USA
Meeyoung O. Min, Research Associate Professor, Mandel School of Applied Social Sciences, Case Western Reserve University, Cleveland, OH, USA
Mark I. Singer, Leonard W. Mayo Professor, Mandel School of Applied Social Sciences, Case Western Reserve University, Cleveland, OH, USA
References
- Aarons GA, Hazen AL, Leslie LK, Hough RL, Monn AR, Connelly CD, Brown SA. Substance involvement among youths in child welfare: The role of common and unique risk factors. American Journal of Orthopsychiatry. 2008;78(3):340–349. doi: 10.1037/a0014215. [DOI] [PubMed] [Google Scholar]
- Acierno R, Kilpatrick DG, Resnick H, Saunders B, De Arellano M, Best C. Assault, PTSD, family substance use, and depression as risk factors for cigarette use in youth: Findings from the National Study of Adolescents. Journal of Traumatic Stress. 2000;13(3):381–396. doi: 10.1023/A:1007772905696. [DOI] [PubMed] [Google Scholar]
- Aisenberg E, Gavin A, Mehrotra G, Bowman J. Defining violence. In: Herrenkohl TI, Aisenberg E, Williams JH, Jenson JM, editors. Violence in context. New York, NY: Oxford University Press; 2001. pp. 13–24. [Google Scholar]
- Allison P. Multiple regression: A primer. Thousand Oaks, CA: Sage; 1999. [Google Scholar]
- Anda RF, Croft JB, Felitti VJ, Nordenberg D, Giles WH, Williamson DF, Giovino GA. Adverse childhood experiences and smoking during adolescence and adulthood. Journal of the American Medication Association. 1999;282:1652–1658. doi: 10.1001/jama.282.17.1652. [DOI] [PubMed] [Google Scholar]
- Asgeirsdottir BB, Sigfusdottir ID, Gudjonson GH, Sigurdsson JF. Associations between sexual abuse and family conflict/violence, self-injurious behavior, and substance use: The mediating role of depressed mood and anger. Child Abuse and Neglect. 2011;35:210–219. doi: 10.1016/j.chiabu.2010.12.003. [DOI] [PubMed] [Google Scholar]
- Baron RM, Kenny DA. The moderator-mediator variable distinction in social psychological research: Conceptual, strategic and statistical considerations. Journal of Personality and Social Psychology. 1986;51:1173–1182. doi: 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- Begle AM, Hanson RF, Danielson CK, McCart MR, Ruggiero KJ, Amstadter AB, Kilpatrick DG. Longitudinal pathways to victimization, substance use and delinquency: Findings from the National Survey of Adolescents. Addictive Behaviors. 2011;36:682–689. doi: 10.1016/j.addbeh.2010.12.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brady SS, Tschann JM, Pasch LA, Flores E, Ozer EJ. Violence involvement, substance use, and sexual activity among Mexican-American and European-American adolescents. Journal of Adolescent Health. 2008;43:285–95. doi: 10.1016/j.jadohealth.2008.02.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Branstetter SA, Furman W, Cottrell L. The influence of representations of attachment, maternal-adolescent relationship quality, and maternal monitoring on adolescent substance use: A 2-year longitudinal examination. Child Development. 2009;80:1448–1462. doi: 10.1111/j.1467-8624.2009.01344.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Breslau J, Miller E, Chung WJJ, Schweitzer JB. Childhood and adolescent onset psychiatric disorders, substance use, and failure to graduate high school on time. Journal of Psychiatric Research. 2011;45:295–301. doi: 10.1016/j.jpsychires.2010.06.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Briere J. Trauma Symptom Checklist for Children™ (TSCC™) Lutz, FL: Psychological Assessment Resources, Inc.; 1996. [Google Scholar]
- Caldwell BM, Bradley RH. Home Observation for Measurement of the Environment Inventory, Early Adolescent Version. Little Rock, AR: University of Arkansas for Medical Sciences; 2003. [Google Scholar]
- Centers for Disease Control and Prevention. YRBSS: Youth Risk Behavior Surveillance System. 2009 Retrieved from http://www.cdc.gov/HealthyYouth/yrbs/index.htm.
- Chassin L, Pillow DR, Curran PJ, Molina BSG, Barrera M. Relation of parental alcoholism to early substance use: A test of three mediating mechanisms. Journal of Abnormal Psychology. 1993;102:3–19. doi: 10.1037//0021-843x.102.1.3. [DOI] [PubMed] [Google Scholar]
- Clark DC, Parker AM, Lynch KC. Psychopathology and substance-related problems during early adolescence: A survival analysis. Journal of Clinical Child Psychology. 1999;28(3):333–341. doi: 10.1207/S15374424jccp280305. [DOI] [PubMed] [Google Scholar]
- Colder CR, Scalco M, Trucco EM, Read JP, Lengua LJ, Wieczorek WF, Hawk LW. Prospective associations of internalizing and externalizing problems and their co-occurrence with early adolescent substance use. Journal of Abnormal Child Psychology. 2013;41:667–677. doi: 10.1007/s10802-012-9701-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Costello EJ, Erkanli A, Federman E, Angold A. Development of psychiatric comorbidity with substance abuse in adolescents: Effects of timing and sex. Journal of Clinical Child Psychology. 1999;28(3):298–311. doi: 10.1207/S15374424jccp280302. [DOI] [PubMed] [Google Scholar]
- De Bellis MD. Developmental traumatology: A contributory mechanism for alcohol and substance use disorders. Psychoneuroendocrinology. 2002;27:155–170. doi: 10.1016/s0306-4530(01)00042-7. [DOI] [PubMed] [Google Scholar]
- Delaney-Black V, Chiodo LM, Hannigan JH, Greenwald MK, Janisse J, Patterson G, Sokol RJ. Prenatal and postnatal cocaine exposure predict teen cocaine use. Neurotoxicology and Teratology. 2011;33:110–119. doi: 10.1016/j.ntt.2010.06.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Derogatis LR, Melisaratos N. The Brief Symptom Inventory: An introductory report. Psychological Medicine. 1983;13:595–605. [PubMed] [Google Scholar]
- DiClemente RJ, Wingood GM, Crosby R, Sionean C, Cobb BK, Harrington K, Oh MK. Parental monitoring: Association with adolescents’ risk behaviors. Pediatrics. 2001;107(6):1363–1368. doi: 10.1542/peds.107.6.1363. [DOI] [PubMed] [Google Scholar]
- Dube SR, Felitti VJ, Dong M, Chapman DP, Giles WH, Anda RF. Childhood abuse, neglect, and household dysfunction and the risk of illicit drug use: The adverse childhood experiences study. Pediatrics. 2003;111:564–572. doi: 10.1542/peds.111.3.564. [DOI] [PubMed] [Google Scholar]
- Dube SR, Miller JW, Brown DW, Giles WH, Felitti VJ, Dong M, Anda RF. Adverse childhood experiences and the association with ever using alcohol and initiating alcohol use during adolescence. Journal of Adolescent Health. 2006;38:444. doi: 10.1016/j.jadohealth.2005.06.006. e1–444.e10. [DOI] [PubMed] [Google Scholar]
- Fagan AA, Van Horn ML, Hawkins JD, Jaki T. Differential effects of parental controls on adolescent substance use: For whom is the family most important? Journal of Quantitative Criminology. 2012 doi: 10.1007/s10940-012-9183-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Flannery DJ, Wester KL, Singer MI. Impact of exposure to violence in school on child and adolescent mental health and behavior. Journal of Community Psychology. 2004;32:559–573. [Google Scholar]
- Fleming CB, Mason WA, Mazza JJ, Abbott RD, Catalano RF. Latent growth modeling of the relationship between depressive symptoms and substance use during adolescence. Psychology of Addictive Behaviors. 2008;22(2):186–197. doi: 10.1037/0893-164X.22.2.186. [DOI] [PubMed] [Google Scholar]
- Fowler PJ, Tompsett CJ, Braciszewski JM, Jacques-Tiura AJ, Baltes BB. Community violence: A meta-analysis on the effect of exposure and mental health outcomes of children and adolescents. Development and Psychopathology. 2009;21:227–259. doi: 10.1017/S0954579409000145. [DOI] [PubMed] [Google Scholar]
- Frank DA, Rose-Jacobs R, Crooks D, Cabral HJ, Gertreis J, Hacker KA, Heeren T. Adolescent initiation of licit and illicit substance use: Impact of intrauterine exposures and post-natal exposure to violence. Neurotoxicology and Teratology. 2011;33:100–109. doi: 10.1016/j.ntt.2010.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fulwiler C, Grossman H, Forbes C, Ruthazer R. Early onset substance abuse and community violence by outpatients with chronic mental illness. Psychiatric Services. 1997;48:1181–1185. doi: 10.1176/ps.48.9.1181. [DOI] [PubMed] [Google Scholar]
- Giaconia RM, Reinherz HZ, Hauf AC, Paradis AD, Wasserman MS, Langhammer DM. Comorbidity of substance use and post-traumatic stress disorders in a community sample of adolescents. American Journal or Orthopsychiatry. 2000;70:253–262. doi: 10.1037/h0087634. [DOI] [PubMed] [Google Scholar]
- Gil AG, Wagner EF, Tubman JG. Associations between early-adolescent substance use and subsequent young-adult substance use disorders and psychiatric disorders among a multiethnic male sample in South Florida. American Journal of Public Health. 2004;94:1603–1609. doi: 10.2105/ajph.94.9.1603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hovdestad WE, Tonmyr L, Wekerle C, Thornton T. Why is childhood maltreatment associated with adolescent substance abuse? A critical review of explanatory models. International Journal of Mental Health and Addiction. 2011;9(5):525–542. [Google Scholar]
- Kaplow JB, Curran PJ, Angold A, Costello EJ. The prospective relation between dimension of anxiety and the initiation of adolescent alcohol use. Journal of Clinical Child Psychology. 2001;30(3):316–326. doi: 10.1207/S15374424JCCP3003_4. [DOI] [PubMed] [Google Scholar]
- Kaufman J, Yang B, Douglas-Palumberi H, Crouse-Artus M, Lipschitz D, Krystal JH, Gelernter J. Genetic and environmental predictors of early alcohol use. Biological Psychiatry. 2007;61:1228–1234. doi: 10.1016/j.biopsych.2006.06.039. [DOI] [PubMed] [Google Scholar]
- Kilpatrick DG, Acierno R, Saunders B, Resnick HS, Best CL, Schnurr PP. Risk factors for adolescent substance use and dependence: Data from a national sample. Journal of Consulting and Clinical Psychology. 2000;68:19–30. doi: 10.1037//0022-006X.68.1.19. [DOI] [PubMed] [Google Scholar]
- King SM, Iacono WG, McGue M. Childhood externalizing and internalizing psychopathology in the prediction of early substance use. Addiction. 2004;99:1548–1559. doi: 10.1111/j.1360-0443.2004.00893.x. [DOI] [PubMed] [Google Scholar]
- Kroutil L, Colliver J, Gfroerer J. Age and cohort patterns of substance use among adolescents. OAS Data Review. 2010 Sep; Retrieved from http://www.samhsa.gov/data/2k10/DataReview/OAS_DataReview003CohortAnalysis.pdf.
- Lambert SF, Nylund-Gibson K, Copeland-Linder N, Ialongo NS. Patterns of community violence exposure during adolescence. American Journal of Community Psychology. 2010;46:289–302. doi: 10.1007/s10464-010-9344-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lansford JE, Dodge KA, Pettit GS, Bates JE. Does physical abuse in early childhood predict substance use in adolescence and early adulthood? Child Maltreatment. 2010;15:190–194. doi: 10.1177/1077559509352359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lewis TL, Kotch J, Wiley TRA, Litrownik AJ, English DJ, Thompson R, Dubowitz H. Internalizing problems: A potential pathway from child maltreatment to adolescent smoking. Journal of Adolescent Health. 2011;48:247–252. doi: 10.1016/j.jadohealth.2010.07.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lipschitz DS, Grilo CM, Fehon D, McGlashan T, Southwick S. Gender differences in the associations between posttraumatic stress symptoms and problematic substance use in psychiatric inpatient adolescents. The Journal of Nervous and Mental Disease. 2000;188:349–356. doi: 10.1097/00005053-200006000-00005. [DOI] [PubMed] [Google Scholar]
- Loeber R, Stouthamer-Loeber M, White HR. Developmental aspects of delinquency and internalizing problems and their association with persistent juvenile substance use between ages 7 and 18. Journal of Clinical Child Psychology. 1999;28(3):322–332. doi: 10.1207/S15374424jccp280304. [DOI] [PubMed] [Google Scholar]
- MacKinnon DP, Lockwood CM, Hoffman JM, West SG, Sheets V. A comparison of methods to test mediation and other intervening variable effects. Psychological Methods. 2002;7:83–104. doi: 10.1037/1082-989x.7.1.83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mickey RM, Greenland S. The impact of confounder selection criteria on effect estimation. American Journal of Epidemiology. 1988;129(1):125–137. doi: 10.1093/oxfordjournals.aje.a115101. [DOI] [PubMed] [Google Scholar]
- Min MO, Minnes S, Lang A, Weishampel P, Short EJ, Yoon S, Singer LT. Externalizing behavior and substance use related problems at 15 years in prenatally cocaine exposed adolescents. Journal of Adolescence. 2014;37:269–279. doi: 10.1016/j.adolescence.2014.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Min MO, Minnes S, Yoon S, Short EJ, Singer LT. Self-reported adolescent behavioral adjustment: Effects of prenatal cocaine exposure. Journal of Adolescent Health. 2014;55:167–74. doi: 10.1016/j.jadohealth.2013.12.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Minnes S, Lang A, Singer LT. Prenatal tobacco, marijuana, stimulant, and opiate exposure: Developmental outcomes and practice implications. Addiction Science and Clinical Practice. 2011;6(1):57–70. [PMC free article] [PubMed] [Google Scholar]
- Minnes S, Singer LT, Kirchner HL, Short E, Lewis B, Satayathum S, Queh D. The effects of prenatal cocaine exposure on problem behavior in children 4–10 years. Neurotoxicology and Teratology. 2010;32:443–451. doi: 10.1016/j.ntt.2010.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Minnes S, Singer LT, Min MO, Lang AM, Ben-Harush A, Short E, Wu M. Comparison of 12-year-old children with prenatal exposure to cocaine and non-exposed controls on caregiver ratings of executive function. Journal of Youth and Adolescence. 2014;43:53–69. doi: 10.1007/s10964-013-9927-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Minnes S, Singer L, Min MO, Wu M, Lang A, Yoon S. Effects of prenatal cocaine/polydrug exposure on substance use by age 15. Drug and Alcohol Dependence. 2014;134:201–210. doi: 10.1016/j.drugalcdep.2013.09.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mrug S, Windle M. Initiation of alcohol use in early adolescence: Links with exposure to community violence across time. Addictive Behaviors. 2009;34:779–781. doi: 10.1016/j.addbeh.2009.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mrug S, Windle M. Prospective effects of violence exposure across multiple contexts on early adolescents’ internalizing and externalizing problems. Journal of Child Psychology and Psychiatry. 2010;51:953–961. doi: 10.1111/j.1469-7610.2010.02222.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Richardson GA, Larkby C, Goldschmidt L, Day NL. Adolescent initiation of drug use: Effects of prenatal cocaine exposure. Journal of the American Academy of Child and Adolescent Psychiatry. 2013;52(1):37–46. doi: 10.1016/j.jaac.2012.10.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ridenour TA. Assessment of Liability and Exposure to Substance Use and Antisocial Behavior© (ALEXSA ©) Allison Park, PA: CORE Measures; 2003. [DOI] [PubMed] [Google Scholar]
- Ridenour TA, Clark DB, Cottler LB. The Illustration-based Assessment of Liability and Exposure to Substance Use and Antisocial Behavior for Children. The American Journal of Drug and Alcohol Abuse. 2009;35:242–252. doi: 10.1080/00952990902998715. [DOI] [PubMed] [Google Scholar]
- Ridenour TA, Meyer-Chilenski S, Reid EE. Developmental momentum toward substance dependence: Natural histories and pliability of risk factors in youth experiencing chronic stress. Drug and Alcohol Dependence. 2012:S87–S98. doi: 10.1016/j.drugalcdep.2011.12.016. http://dx.doi.org/10.1016/j.drugalcdep.2011.12.016. [DOI] [PMC free article] [PubMed]
- Ridenour TA, Minnes S, Maldonado-Molina MM, Reynolds MD, Tarter RE, Clark DB. Psychometrics and cross-cultural comparisons of the Illustration-based Assessment of Liability and Exposure to Substance Use and Antisocial Behavior for Children. Open Family Studies Journal. 2011;4:17–26. doi: 10.2174/1874922401104010017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singer LT, Minnes S, Short E, Arendt R, Farkas K, Lewis B, Klein N, Kirschner HL. Cognitive outcomes of preschool children with prenatal cocaine exposure. JAMA: The Journal of the American Medical Association. 2004;291(20):2448–2456. doi: 10.1001/jama.291.20.2448. http://dx.doi.org/10.1001/jama.291.20.2448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singer L, Salvator A, Arendt R, Minnes S, Farkas K, Kliegman R. Effects of cocaine/polydrug exposure and maternal psychological distress on infant birth outcomes. Neurotoxicology and Teratology. 2002;24:127–135. doi: 10.1016/s0892-0362(01)00208-2. [DOI] [PubMed] [Google Scholar]
- Singer MI, Flannery DJ, Guo S, Miller D, Leibbrandt S. Exposure to violence, parental monitoring, and television viewing as contributors to children’s psychological trauma. Journal of Community Psychology. 2004;32(5):489–504. [Google Scholar]
- Skeer M, McCormick MC, Normand ST, Buka SL, Gilman SE. A prospective study of familial conflict, psychological stress, and the development of substance use disorders in adolescence. Drug and Alcohol Dependence in Adolescence. 2009;104:65–72. doi: 10.1016/j.drugalcdep.2009.03.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stott T. Placement instability and risky behaviors of youth aging out of foster care. Child and Adolescent Social Work Journal. 2012;29:61–83. [Google Scholar]
- Streissguth AP. The behavioral teratology of alcohol: Performance, behavioral, and intellectual deficits in prenatally exposed child. In: West JR, editor. Alcohol and brain development. New York, NY: Oxford University Press; 1986. pp. 3–44. [Google Scholar]
- Sullivan TN, Farrell AD, Kliewer W, Vulin-Reynolds M, Valois RF. Exposure to violence in early adolescence: The impact of self-restraint, witnessing violence, and victimization on aggression and drug use. Journal of Early Adolescence. 2007;27(3):296–323. [Google Scholar]
- Sullivan TN, Kung EM, Farrell AD. Relation between witnessing violence and drug use initiation among rural adolescents: Parental monitoring and family support as protective factors. Journal of Clinical Child and Adolescent Psychology. 2004;33:488–498. doi: 10.1207/s15374424jccp3303_6. [DOI] [PubMed] [Google Scholar]
- Sung M, Erkanli A, Angold A, Costello EJ. Effects of age at first substance use and psychiatric comorbidity on the development of substance use disorders. Drug and Alcohol Dependence. 2004;75:287–299. doi: 10.1016/j.drugalcdep.2004.03.013. [DOI] [PubMed] [Google Scholar]
- Swahn MH, Bossarte RM, Sullivent EE. Age of alcohol use initiation, suicidal behavior, and peer and dating violence victimization and perpetration among high-risk, seventh-grade adolescents. Pediatrics. 2008;121:297–305. doi: 10.1542/peds.2006-2348. [DOI] [PubMed] [Google Scholar]
- Tharp-Taylor S, Haviland A, D’Amico EJ. Victimization from mental and physical bullying and substance use in early adolescence. Addictive Behaviors. 2009;34:561–567. doi: 10.1016/j.addbeh.2009.03.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tofighi D, MacKinnon DP. RMediation: An R package for mediation analysis confidence intervals. Behavioral Research. 2011;43:692–700. doi: 10.3758/s13428-011-0076-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tolin DF, Foa EB. Sex differences in trauma and posttraumatic stress disorder: A quantitative review of 25 years of research. Psychological Bulletin. 2006;132(6):959–992. doi: 10.1037/0033-2909.132.6.959. [DOI] [PubMed] [Google Scholar]
- Tonmyr L, Thornton T, Draca J, Wekerle C. A review of childhood maltreatment and adolescent substance use relationship. Current Psychiatry Review. 2010;6(3):223–234. [Google Scholar]
- Warner TD, Behnke M, Eyler FD, Szabo NJ. Early adolescent cocaine use as determined by hair analysis in a prenatal cocaine exposure cohort. Neurotoxicology and Teratology. 2011;33:88–99. doi: 10.1016/j.ntt.2010.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weiner MD, Pentz MA, Skara SN, Li C, Chou C, Dwyer JH. Relationship of substance use and associated predictors of violence in early, middle, and late adolescence. Journal of Child and Adolescent Substance Abuse. 2004;13(4):97–117. [Google Scholar]
- Wekerle C, Leung E, Goldstein AL, Thonton T, Tonmyr L. Substance use among adolescents in child welfare versus adolescents in the general population: A comparison of the Maltreatment and Adolescent Pathways (MAP) longitudinal study and the Ontario Student Drug Use Survey (OSDUS) datasets. London, ON: University of Western Ontario; 2009. [Google Scholar]
- Whitesell M, Bachand A, Peel J, Brown M. Familial, social, and individual factors contributing to risk for adolescent substance use. Journal of Addiction. 2013 doi: 10.1155/2013/579310. Article ID 579310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zahn-Waxler C, Shirtcliff EA, Marceau K. Disorders of childhood and adolescence: Gender and psychopathology. Annual Review of Clinical Psychology. 2008;4:275–303. doi: 10.1146/annurev.clinpsy.3.022806.091358. [DOI] [PubMed] [Google Scholar]
- Zona K, Milan S. Gender differences in the longitudinal impact of exposure to violence on mental health in urban youth. Journal of Youth and Adolescence. 2011;40:1674–1690. doi: 10.1007/s10964-011-9649-3. [DOI] [PubMed] [Google Scholar]