Abstract
Mass incarceration of young Black men has a significant impact on their network composition and stability that, in turn, may have major implications for health and well-being. A sub-group of young Black men with criminal justice involvement (CJI) identify as gay, bisexual or are non-identified men who have sex with men (hereafter MSM). This paper focuses on the potential effects of CJI on the composition of Black MSM social and sexual networks, their stability over time, and concomitant health and social outcomes. We use data from the UConnect study, a population-based cohort of young Black MSM 16–29 years of age (n=618) selected using respondent-driven sampling in Chicago from 2013–2016. Both confidant and sexual network name generators and interpreters were administered at 9-month intervals over three waves of data collection. Ego and dyadic-level data were collected on behaviors prevalent among MSM and including factors associated with network CJI, network stability, and health outcomes. Generalized Structural Equation Models (GSEM) were utilized to determine the relationship between CJI network composition, network stability and behaviors prevalent among young Black MSM and their networks. In the UConnect cohort, 46% had at least once been detained, arrested or spent time in jail or prison. In addition, 20% of participants reported incident CJI over the study period. Respondents with a history of CJI were significantly more likely to have CJI homophily in their confidant and sexual networks. Multivariate analyses demonstrate that the association between one’s history of CJI, housing instability and drug use is partially explained by one’s network CJI. In addition, a higher prevalence of network CJI is associated with increased turnover in the confidant network, and this network instability is also related to important health and social outcomes. This analysis describes the networks of criminal justice involved men among a representative sample of young Black MSM and demonstrates the relationship between CJI network homophily, network stability and their impact on several key health and social outcomes relevant to this population.
1. Introduction
In the United States, an estimated 2.3 million people are held in prisons and jails on any given day (Glaze, 2015). In addition, approximately 11 million people cycle through local jails each year (Minton, 2015). Black men are disproportionately affected by criminal justice involvement (CJI), making up 13% of the U.S. male population, but accounting for 38% of the male prison population (Carson, 2015). There is an even greater disparity seen among young men between 18–24 years of age. Black men in the 18–19 and 20–24 age groups have rates of incarceration 10.5 and 6.6 times the rate of white men in the same respective age groups despite constituting nearly 5 times fewer the population size of Whites (U.S. Census Bureau).
Mass incarceration of young Black men can have a significant impact on their network composition and stability that, in turn, can have major implications for health and well-being. A sub-group of young Black men with criminal justice involvement (CJI) identify as gay, bisexual or are non-identified men who have sex with men (hereafter YBMSM). Limited information exists on the composition and dynamics of the social and sexual networks among this sub-group, in particular, the extent to which these men are embedded within networks of CJI MSM, how stable these networks are over time and how these networks are associated with health conditions that disproportionately impact YBMSM such as substance use, housing instability and mental illness. This paper focuses on the potential effects of CJI on the composition of MSM social and sexual networks, their stability over time, and concomitant health and social conditions.
1.1 Intersectionality – Sexual Orientation and Race - within Criminal Justice Involved Contexts
Criminal justice research often focuses on a single social group (i.e. African Americans, women) in attempts to focus on how one group may have different outcomes compared to a reference group or how public health intervention may be differentially applied or targeted (Binswanger, Redmond, Steiner, & Hicks, 2012). Such a focus ignores the complexity of intersectional identities and can result in limited attention to multiple social attributes that can drive the same outcomes of interest. ‘Intersectionality’ is the study of how multiple systems of social stratification (e.g., race, ethnicity, gender, sexual orientation) influence an individuals’ identity and lived experience, recognizing that every person holds a position (privilege or disadvantage) in different systems simultaneously, and that such positions can vary in magnitude and direction depending on time, place, and circumstance (L. Bowleg, 2008; Jones & McEwen, 2000; Purdie-Vaughns & Eibach, 2008). For example, in jail, it is likely that a Black same gender loving man, may be observed as Black, and may move his Black identity to the forefront given the disadvantage that a non-normative sexual orientation might experience. Certainly, this might quickly change if the same individual is detained in a special populations unit that privileges men who have sex with men. Intersectionality also explores how different levels of a social framework influence individuals experiences, including the intrapersonal level (e.g., internalized racism) (Mossakowski, 2003), the interpersonal level (e.g., bias,discrimination) (Kessler, Mickelson, & Williams, 1999), the contextual level (e.g., societal victimization such as hate crimes) (Klest, 2012), and the macro-level, where structural inequalities (e.g., education, income distribution). The study of intersectionality within institutions has also been examined including health-care contexts and how patients and providers both view and are viewed within health care institutions (Peek et al., 2016).
One of the theoretical questions that arise from intersectionality of Black men who have sex with men in the criminal justice system is whether the intersectionality of race and sexual orientation represents an advantage or disadvantage with respect to ongoing criminal justice involvement, excessive policing or targeting for punishment. In other words, do Black men who have sex with other men experience more criminal justice involvement than Black men who have sex with women only. One could imagine that because of the number of syndemic factors that MSM experience including substance use and interpersonal violence that they would more likely be involved with criminal justice involvement (Wilson et al., 2014). In addition, following basic tenets of social network theory such as homophily, would suggest that MSM are more likely to be in social groups with other men (J. A. Schneider, Cornwell, B., Jonas, A., et al., 2017); which would put them at risk as compared to groups that are more heterogeneous by gender and thus in social proximity to groups that have lower incarceration rates. In recent work, Meyer finds that sexual minority men (including those who self-identify as gay or bisexual) are disproportionately incarcerated as compared to men who identify as straight and report having sex with women only (I. H. Meyer et al., 2017). In this analysis, however, special units are described, however, we do not know to what extent intersectionality plays a role in the lived experiences of sexual and racial minority men. The analyses described here begins that discussion and in particular how these men are engaged with others in their social environment.
1.2 Criminal justice involvement among young Black men who have sex with men
The important role of criminal justice involvement has intensified in the context of Black communities with rapidly increasing rates of incarceration over the past few decades that peaked in 2008 and continue to be higher than anywhere else in the world – with approximately 6.9 million individuals under some form of adult CJ supervision, including 1 in 108 adults incarcerated in jails or prisons and 1 in 35 under some form of correctional control (M. Epperson, El-Bassel, Gilbert, Orellana, & Chang, 2008; Harrison & Beck, 2006; Pew, 2009; PewCenter, 2008). The vast majority of the criminal justice population spends short periods locked-up prior to being returned to community as opposed to longer-term prison settings. While most criminal justice data includes race, sexual orientation and behavior have not been typically collected in most jail settings, and when collected, response bias would likely be an important limitation to the data, given the risk that some sexual minorities can face while incarcerated (Beck AJ, 2010; Dumond, 2000; Hensley, Tewksbury, & Castle, 2003; Saum, 1995). These risks have been much of the focus in prior scholarly work examining MSM in CJI contexts, particularly around HIV risk given concerns that sex, whether it be consensual or non-consensual, can increase chances of HIV acquisition within jails (T. M. Hammett, Harmon, & Rhodes, 2002; Robertson, 2003). More recent data has instead focused on reports of transmission outside of jail and a seminal meta-analysis of determinants of HIV infection has suggested that Black MSM in the US and elsewhere are more than twice as likely to have experienced incarceration as other MSM (Millett et al., 2012), and CJI is a known factor associated with HIV infection. Recent empirical data has documented high prevalence of CJI among Black men who have sex with men (31% Lim, 60% Brewer, 51% Bland) (Bland et al., 2012; Brewer et al., 2014b; Lim, Sullivan, Salazar, Spaulding, & Dinenno, 2011) and these rates are higher than that of Black men in general, suggesting that there may be other factors driving CJI among YBMSM. It may be that increased rates of substance use, mental health problems and housing instability, or so-called “syndemic factors” (Stall R, 2008; Stall et al., 2003) drive CJI among YBMSM. Alternatively, it may be that network forces, such as homophily may be greater in this population given larger numbers and higher proportions of other Black men in these networks which could increase the numbers of individuals who are criminal justice involved, or who may be experiencing factors associated with CJI such as exposure to violence, substance use and connections to other Black men.
1.3. CJI network homophily
There are high levels of CJI among Black MSM and Black communities due to drug policy and the War on Drugs, racial bias in arrests and sentencing and other structural factors, which may account for the high prevalence of CJI among young Black men and their networks (N Freudenberg, 2001). Because of the high numbers of incarcerated Black men it is not surprising that individuals who have previously experienced CJI are likely connected to others who have experienced CJI. Because of these biases, CJI has a level of randomness that might make network factors less relevant to predicting future CJI in a given individual. On the other hand, because of the density of CJI among young Black men, it may be that social influence resulting from embeddedness in criminal justice involved networks may continue to drive CJI. Much of the literature that has examined homophily in young Black men has examined gang networks and the processes that set-up homophily in experiences of community violence (Papachristos, Wildeman, & Roberto, 2015; Tracy, Braga, & Papachristos, 2016). Group identity, reciprocity (Papachristos, 2009), and assortative mixing patterns (Young, 2011) on attributes related to the characteristics or behavior of interest have been identified as the mechanistic undergirding to homophily. Similarly, among YBMSM experiencing CJI, there are multiplex associations that are shared by these men including being young, Black and living in a segregated community – all of which are related to CJI homophily. In addition, there are other aspects that further drive homophily, which include membership in cultural organizations, such as the House Ball Community (Arnold; Murrill et al., 2008; Phillips et al., 2011), experiencing high levels of community violence (Voisin, Hotton, & Neilands, 2014; Voisin et al., 2007), health conditions such as HIV (Khanna et al., 2016) and higher than average numbers of relationships with other young men in mostly friendship and sexual relationships (Shah et al., 2014). Homophilous attributes or behaviors do manifest in important health outcomes. For example, there is evidence that enabling effects of social network members may affect risk behavior and outcomes (Latkin, Forman, Knowlton, & Sherman, 2003; J. A. Schneider et al., 2013; Skeem, Eno Louden, Manchak, Vidal, & Haddad, 2009). An important area of investigation is the extent to which dynamic attributes (i.e. CJI) at the individual or network level impacts ongoing CJI or other social or health sequelae. This has implications for intervention design and policy which may need to target groups of individuals as opposed to current practices which engage individuals in service provision. The extent to which homophily of criminal justice involved persons is a major driver of health and social outcomes is unclear.
1.4 CJI and network stability
Another potential driver of incident CJI, which can also be conceptualized as a potential consequence of CJI, is network stability. Network instability may occur during socially disruptive processes and may particularly sensitive to CJI. CJI can alter networks by removing individuals from mutually supportive family and community relationships (N Freudenberg, 2001; Lopoo & Western, 2005; Western, 2000). CJI can also disrupt social networks by causing strain on family and existing friends who are dependent on the individual (Browning S, 2001; Comfort, Grinstead, McCartney, Bourgois, & Knight, 2005). Important life events can impact network turnover (Wrzus, Hanel, Wagner, & Neyer, 2013), and these can in turn impact distal health events (E. Y. Cornwell & Waite, 2009). Increasing evidence suggests that network turnover is higher among Black communities and resilience to the turnover in the form of replacing individuals is lower (B. Cornwell, 2015) among older African Americans.
CJI can also lead to formation of new ties and relationships and introduce individuals into high-risk networks with high levels of drug trade and use (N Freudenberg, 2001; Moore J, 1996). The disruptive effect of CJI on existing intimate partnerships has been well documented. Periods of incarceration disrupt stable sexual relationships, which have been found to protect against new, multiple, and concurrent partnerships (Khan et al., 2009b; Khan et al., 2008). Studies have found associations between CJI, partners with CJI and risky sexual partnerships (Adimora et al., 2004; Adimora et al., 2003; Khan et al., 2015). Most of these studies have focused on heterosexual partnerships.
Given the barriers and complex interactions a formerly incarcerated person must negotiate upon release, the experience of transitioning from the correctional setting to the community is marked by network disruption, which we conceptualize as abrupt and involuntary network change. The network disruptions experienced at the time of detention and release have important health implications for CJI YBMSM and even those connected more distally. Disruptions to social networks through the spread of infectious disease have been described in instances of disasters (e.g. earthquakes, civil wars causing genocide) and are extended to mass incarceration(Golembeski & Fullilove, 2005). For example among young men re-entering the community after detention, an estimated 50% report inconsistent social networks (interactions with different individuals pre- and post-incarceration) (D. W. Seal et al., 2007). The impact of CJI-induced disruptions to social networks has yet to be evaluated and represents a critical factor tied to the effectiveness of HIV prevention and substance-abuse interventions for CJI BMSM. A recent study in the Netherlands examined discussion network stability in Dutch prisoners measured before and after incarceration. They found that discussion networks remained relatively constant in size, however, the majority of network members had changed over the time period studied (an average of 4 months) (Volker B, 2016). Additional work is needed to examine how these network changes impact health and well-being, particularly in vulnerable populations who are targeted by the criminal justice system.
1.5 CJI implications on the health of young Black men who have sex with men
There is great body of research of the detrimental impact of criminal justice involvement on the health and well-being of Black men and their networks. Upon release, formerly incarcerated people face a range of barriers such as a lack of community-based HIV or substance-abuse treatment options, a lack of connectivity between medical records maintained by the correctional facility and those maintained by a community provider, and disruptions in their social and sexual networks (Adimora & Schoenbach, 2005; Butler, 2012). CJI is also associated with negative health and socioeconomic consequences including unemployment, homelessness and poor health. There is a high prevalence of health conditions in CJI populations including HIV, sexually transmitted infections (STI), substance use, prior sexual abuse and assault as a child and adult and mental illness (R. L. Braithwaite & Arriola, 2003; N Freudenberg, 2001; T. M. Hammett et al., 2002). Levels of HIV in incarcerated populations are 3 to 5 times higher than in the general population (Maruschak, 2009). The stress and disruption associated with repeated criminal justice involvement exacerbates ongoing social stressors and heightens CJI’s impact upon substance use and HIV risk (Blankenship, Smoyer, Bray, & Mattocks, 2005; Khan et al., 2009a) (M. W. Epperson, El-Bassel, N., Chang, M., & Gilbert, L., 2010; Luther, 2011). Moreover, mental health conditions, addiction, and unemployment upon release from custody disproportionately impact justice-involved people (“Behind Bars II: Substance Abuse and America’s Prison Population,” 2010; Lisa Bowleg, Teti, Malebranche, & Tschann, 2013; Theodore M Hammett, Gaiter, & Crawford, 1998). These risk factors are also associated with underutilization of antiretroviral therapy which further increases HIV transmission risk (Westergaard, Spaulding, & Flanigan, 2013). Those serving time in the community under probation or parole may, in fact, have higher rates of risk factors, with lesser exposure to HIV education, prevention, and treatment interventions, than among those in custody (Belenko, Langley, Crimmins, & Chaple, 2004). For example, 35% of CJ systems have mandatory pre-release HIV instruction in the context of a constitutional right to HIV medical care (Nicholas Freudenberg, Daniels, Crum, Peridns, & Richie, 2005; Theodore M Hammett et al., 1998; T. M. Hammett, Roberts, & Kennedy, 2001).
HIV is notable among criminal justice involved populations with rates of HIV three to five times the rate of HIV in the general population (Maruschak, 2009; McQuillan et al., 2006). The HIV disparity among men in the CJ system (most of whom have a drug related charge) is well established as a serious public health concern (Boutwell & Rich, 2004; Ronald L Braithwaite, Hammett, & Arriola, 2002; David Wyatt Seal, 2005). Increased prevalence of HIV has been demonstrated in studies of offenders at various levels of CJI, including men on probation or parole (Belenko et al., 2004), formerly incarcerated drug-involved populations (D. W. Seal et al., 2007), and other individuals with history of incarceration (Boutwell & Rich, 2004). The reason for higher rates of infection are multifactorial; what is clear is that HIV transmission while in jail is likely not a major factor in the transmission pathway (Krebs & Simmons, 2002; D. W. Seal et al., 2007; Wohl et al., 2000). The social milieu that exists before and after criminal justice involvement is thus likely a key driver of transmission, which contributes to the astonishingly high rates of HIV for example among Black men who have sex with men (BMSM). Recent data from the CDC suggests that 1 in 2 will become infected within their lifetime (Centers for Disease Control and Prevention, 2015). While there is geographic variability in rates of HIV infection, these rates are similar to the high CJI rates where if current trends continue, 1 in every 3 black males born today will go to prison in their lifetime (Mauer, 2011).
We focus on Black men who have sex with men to examine these phenomena. We do this given the syndemic factors (Stall et al., 2003) that increase their likelihood of incarceration, and the unique composition of their networks which are made up predominantly of other men (J. Schneider, Michaels, & Bouris, 2012). MSM in general are more likely to use substances, experience intimate partner violence and participate in exchange sex than other men (Finneran & Stephenson, 2013; Newman, Rhodes, & Weiss, 2004; Rietmeijer, Wolitski, Fishbein, Corby, & Cohn, 1998; Stall et al., 2001). All of these factors place them at higher risk of CJI. We examine the potential effect that network composition and stability exhibit in this milieu, to what extent they mediate the relationship between CJI and health outcomes men.
We propose that CJI in YBMSM’s networks is associated with an individual’s level of CJI. The goal of this study is to explore how individual CJI, network level CJI, and network stability are related to future CJI and health outcomes in this unique population that has intersectional identity. Accordingly, we have several questions: 1) What is the relationship between the number (proportion) of people in an individual’s network (social and/sexual) with CJI and an individual’s CJI at baseline and incident CJI over the study period? 2) What is the relationship between network CJI and network stability, particularly in the context of other YBMSM? 3) What is the relative relationship between individual CJI, network CJI, and network stability with associated health outcomes relevant to YBMSM over time? These questions become important given some of the individual-level interventions that are being considered for CJI related contexts (Grant et al., 2010; Harawa, Sweat, George, & Sylla, 2010; Hedrich et al., 2012; Larney, 2010; Lubelczyk, Friedmann, Lemon, Stein, & Gerstein, 2002; Mouttapa et al., 2010). Examination of the networks that these men are embedded within are critical to understanding the pattern of CJI involvement of these men and how these are related to health outcomes most relevant to this often doubly stigmatized population. Work that follows will advance individual-level interventions just highlighted as these existing interventions are not targeted to CJI men experiencing intersectional identities; an area that needs further consideration and research.
2. Methods
2.1 Setting and Population
The South Side of Chicago is the largest contiguous Black urban community in the US (Chicago Police Department; Chicago Policy Research Team, 2010; Mari Gallagher Research & Consulting Group, 2007). Despite its many assets, the region is burdened by lack of basic resources and structural factors, including highest incarceration rates in the city, that contribute to a number of health problems, including a high HIV prevalence. We use data from the uConnect study, a longitudinal population-based cohort of YBMSM on the south side of Chicago that examines how social and sexual networks affect men’s behaviors as well as physical and mental health related to risk of sexually transmitted infections (STIs) including HIV (Khanna et al., 2016; Morgan, 2016).
2.2 Sample Selection
Recruitment for the uConnect study has been described previously (Khanna et al., 2016; Morgan, 2016; J. A. Schneider et al., 2013). Using Respondent Driven Sampling (RDS), a sample of 618 eligible YBMSM were recruited between June 2013 and July 2014. The RDS process was initiated by purposively selecting a diverse group of YBMSM to serve as seeds from which the chains were initiated. A total of 62 seeds were recruited through multiple sources including the House/Ball Community, web sites, Facebook postings, community events, college campuses, clinics and support groups. Each seed and subsequent recruit was asked to recruit other MSM into the sample. Study participants (seeds and their subsequent recruits) were eligible to be interviewed if they: 1) self-identified as African American or Black, 2) were born male, 3) were between 16 and 29 years of age; and 4) reported having had oral or anal sex with a male within the past 24 months. The distribution of the number of respondents successfully recruited was: 0 (6.4%), 1 (44.3%), 2 (24.4%), 3 (15.1%), 4 (5.9%), 5 (2.5%) and 6 (1.4%). Each respondent, whether a seed or subsequent recruit, was offered $60 for his participation in the interview and was told he would receive an additional $20 for each recruit who participated. Sample weights designed to account for unequal probabilities of selection were computed using the Giles Sequential Sampling (SS) estimator as implemented in the RDS package in R (Gile & Handcock, 2010).
2.3 Survey instrument development and administration
Development of the survey instrument has been described previously (J. A. Schneider et al., 2013). In brief, the survey instrument included items on sociodemographics, sexual behavior, drug use, confidant networks, sexual networks and attitude questions. A major focus of uConnect data collection is the enumeration and description of the social and sexual networks of YBMSM. The approach to egocentric network data collection followed the National Health, Social Life, and Aging Project (NSHAP) (B. S. Cornwell, P. L.; Laumann, E.O.; Kim, J; Kim, Y.J., 2014), although uConnect added a second sex network generator to the confidant generator used in NSHAP. The uConnect generator used the following item to generate the confidant list:
“In this next section, we will discuss your close social network, that is, the people with whom you discuss things that are important to you. So I can ask some follow-up questions, please list the names of the people with whom you discuss things that are important to you.” In a similar fashion the sex network generator was administered following procedures previously described (Laumann, 1994), with sex partners listed in reverse chronology. After generating a list of the five most recent sexual partners, a further question was asked about any current primary sexual partner. If the respondent gave the name of a current primary partner who was not among the five partners, they were added to roster as a sixth alter. Once both generators had been administered the respondent was asked to compare the list of confidants mentioned earlier with the list of sex partners that they had just named. The two lists were displayed side by side on the computer screen.
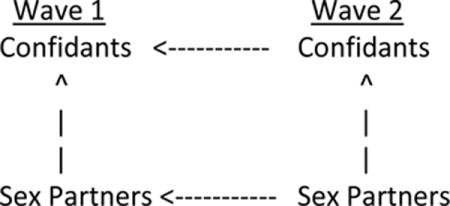
The same confidant generator was used in Wave 2 as in Wave 1. After the confidant list had been generated, the respondent was asked if any of the confidants in Wave 2 were the same person as the confidants listed in Wave 1. The list of Wave 1 confidants was displayed next to the newly generated Wave 2 confidants and matches were indicated by the respondent. The Wave 2 sex partner generator was similar to that used in Wave 1, except that the sex partner generator in Wave 2 referred to sexual partners since the last interview instead of the past six months. Similar to the confidant generator, respondents were then asked to compare sex partners listed with the list of sex partners from Wave 1. They were then asked to compare the names of the Wave 2 sex partners with the Wave 2 confidants and to confirm any that referred to the same person. It should be noted that the respondent was not asked to compare the sex partners in Wave 2 with the confidants from Wave 1. [See diagram]
Comparisons of alter lists between network generators and interviews
A similar procedure was used in Wave 3, except that the confirmation list was cumulative. For example, respondents in Wave 3 were asked whether any of the confidants listed corresponded to a combined list of confidants and sex partners from the previous interview. And in Wave 3, similarly respondents were asked whether the sex partners listed corresponded to a cumulative list of the confidants and sex partners from the current and previous interview. Name interpreters (range 20–50) were asked regarding the first five confidant and first five sex network members at each wave. Participants were interviewed at three time points approximately 9 months apart. Hereafter we will refer to these data collection time points as Wave 1 (baseline), Wave 2 (9 months) and Wave 3 (18 months).
2.4 Respondent Criminal Justice Involvement measure
History of CJI was self-reported by respondents at the baseline interview. Respondents were asked if they had ever been detained, arrested, or spent time in jail or prison. This was a dichotomous variable of yes/no. Those respondents who reported history of CJI were subsequently asked their age at first incarceration, the number of separate occasions, and the cumulative time they spent in jail or prison during their lifetime (in days, months or years). At the follow up interview, respondents were asked if they had been detained, arrested, or spent time in jail or prison since the date of their last interview. If yes, they were asked the number of times and cumulative time spent in jail since their last visit.
2.5 Confidant and Sex partner incarceration
At the baseline interview, for each sexual partner and confidant alter reported, respondents were asked if that person had ever been detained, arrested, or spent time in jail or prison. This was a dichotomous variable of yes/no. At the follow-up interviews, if the alter was the same person reported in the first wave, they were asked if the alter had been detained, arrested or spent time in jail or prison since the date of their last interview. If the respondent reported a new alter, they were asked if the alter had ever been detained, arrested or spent time in jail or prison.
2.6 Health Outcomes
Most outcomes were measured as in pilot work for this study (J. A. Schneider et al., 2013). Drug use was asked in the following manner: “Have you used any of these substances in the past 12 months?” Drugs included MDMA, volatile nitrates, cocaine, heroin, psychoactive drugs, methamphetamines, and prescription pain killers. Drug use was a dichotomous measure indicating use of the aforementioned substances in the past 12 months. Marijuana use was measured separate from other drug use. Respondents were asked if they ever used marijuana and frequency of use from several times a day to less than once a year. On the basis of responses to these questions, we coded a 3-level measure of Never, Moderate (less than daily) and Heavy use (once a day or greater) (Morgan, 2016). Depression, anxiety and distress symptoms were analyzed using the Brief Symptom Inventory 18-question survey (BSI-18), a self-report measure of psychological symptoms over the previous week (Derogatis, 2001). For the depression variable, raw scores for the BSI-18 were converted to T-scores and defined as present if the T-score was greater than 62 as in previous research (Mustanski, Garofalo, & Emerson, 2010). Exposure to community violence was measured using the modified Exposure to Violence Probe (Stein, Walker, Hazen, & Forde, 1997), a series of questions assessing the number of times participants had been exposed to community violence in their lifetime. Responses ranged from 0 to 6 or more times. Raw scores were computed by taking the mean of items scores listed and standardized to T-scores following the strategy of previous studies (King, Voisin, & Diclemente, 2015; Voisin, Jenkins, & Takahashi, 2011). HIV infection status was determined by 4th generation, differentiation and viral load testing applied to samples eluted from dry blood spot samples.
Respondents were asked separately whether they encouraged or discouraged other MSM from engaging in the following behaviors: using condoms during anal sex, taking part in group sex, using drugs to make sex easier, last longer or feel better, and drinking alcohol to make sex easier, last longer or feel better. As has been previously described, members of at-risk communities often talk to each other about how to protect themselves. The content of such communications, which we have called intraventions, helps to maintain or establish social norms about health (Friedman, Bolyard, Maslow, Mateu-Gelabert, & Sandoval, 2005; Friedman et al., 2007; Friedman et al., 2004; Friedman et al., 2013; Mateu-Gelabert et al., 2008). An exploratory factor analysis demonstrated that discouraging condom use and encouraging group sex, drug and alcohol use loaded on a different factor from encouraging condom use and discouraging group sex, drug and alcohol use. Scales formed from the two sets of items yielded reliabilities (via Cronbach’s alpha) of 0.72 (discouraging risk behavior) and 0.50 (encouraging risk behavior). Since the two alcohol use items were not asked at 18 months, we computed each scale from the remaining three items. These three item scales were highly correlated with scales formed from all 4 items (r = 0.97 for discouraging risk behavior and 0.91 for encouraging risk behavior). Finally, as an exploratory outcome, in the last wave, we asked respondents about involvement in political movements (ie. Black Lives Matter): “In the past 12 months, have you taken part in any protests, marches, or demonstrations related to police brutality or other issues?”
2.7 Additional covariates measured
The uConnect survey instrument measured a wide range of respondent- (ego-) level sociodemographic characteristics, risk and prevention behaviors and socio-structural factors that are potentially associated with history of CJI and health outcomes. Individual-level variables that are utilized in multivariable regression models, and in particular health and risk variables, were selected based upon the existing YBMSM literature. We included respondent age at the time of the interview as a covariate. Sexual identity was collected based upon 21 unique and overlapping categories and due to the low numbers of respondents identifying in several categories (i.e., same gender loving, straight), we operationalized sexual identity into gay, bisexual and other. During instrument development, pilot interviews and cognitive testing of questions was conducted by the Survey Research Lab at the University of Chicago.
2.8 Statistical analysis
The weighted distributions of several demographic and behavioral characteristics were computed, both for the sample as a whole and separately for those with and without a history of CJI. Comparisons between these two subgroups were performed via the appropriate Wald test—either a comparison of subgroup means or test for independence in a two-way table—using the sample weights and robust variance estimates. Because the weighted distributions were very similar to the unweighted distributions (suggesting that the sample is fairly representative), and to avoid relying on the assumptions involved in the calculation of the weights or the resulting loss in precision, the remaining analyses were performed without the weights.
Generalized Linear, Latent And Mixed Models (GLLAMMs) were used to analyze the data from all three waves (Skrondal A, 2004). Let Jiw be a binary (0/1) variable with Jiw = 1 indicating that the ith respondent had been in jail (at least once) at wave w. Similarly, let Aijw = 1 indicate that the jth alter (i.e., confidant or sex partner) reported by the ith respondent at wave w had been in jail (as of wave w). We started by using logistic regression to model (Ji1 = 1) as a function of the respondent’s age and sexual orientation (both also measured at wave 1). Using the data for confidants only (i.e., excluding sex partners), we then fit a mixed effects logistic regression to P(Aij1 = 1) using Ji1, age and orientation as covariates, and including a random effect at the respondent level to account for the correlation among multiple wave 1 confidants reported. To further investigate the association between a respondent’s jail history and the composition of his network, we fit a second mixed effects logistic regression to (Aijw = 1) for w = 2, 3 and j ∈ new confidants at wave w, using the occurrence of a respondent’s arrest between waves (w − 1) and w as a covariate, and adjusting for Ji1, age, orientation and wave (3 versus 2). As with the previous model, this three-level model included a random effect at the respondent level, together with a second random effect to account for possible correlation within respondent among confidants named in a given wave.
A key question of this study was the extent to which criminal justice involvement within a respondent’s network is associated with subsequent behavioral and health outcomes, adjusting for the respondent’s own criminal justice involvement. To determine this, we began with the following model for Aij1:
This allows us to account explicitly for the fact that respondents may report only a subset of their network members during the interview, with λ0 + λ1αi being interpreted as the logit of the underlying (unobserved) proportion of respondent i’s network (including here both confidants and sex partners) at wave 1 who have been to jail. The distribution of αi was then modeled as
where X includes age and sexual orientation, and the e1i are assumed to be distributed normally with mean zero and variance one (these assumptions are necessary to identify the model). Finally, letting Yi be a continuous longitudinal outcome measured during the course of the study, we used
in which α1 describes the direct association between the respondent’s jail history at baseline and the subsequent outcome, while α2 describes the association between the prevalence of jail among the respondent’s network and the outcome (an analogous logistic regression was used for binary outcomes). This model was first fit with only Ji1 and then refit with αi added, to determine the effect of adding the network measure on α1. Figure 1a shows the model in graphical form, using the standard conventions for representing Generalized Structural Equation Models (GSEMs).
Figure 1.

Generalized Structural Equation Models (GSEMs) used for examining (A) the association between network CJI prevalence and health outcomes (Table 3), and (B) the association between network stability and health outcomes (Tables 4 and 5).
While the preceding analysis focuses on network composition, we also wanted to determine whether having spent time in jail affects network dynamics, such as the change in membership of a respondent’s confidant network between waves. Two distinct events provide information about the change in a respondent’s network between successive waves. Let Rijw = 1 represent the event that at wave w (w = 2, 3), respondent i retains (i.e., names again) confidant j from the previous wave, with Rijw = 0 indicating that confidant j (named during the last wave) is not retained. In addition, let Nijw = 1 represent the event that a new confidant is added on line j at wave w, with Nijw = 0 indicating that line j is left blank. Note that for any respondent at a given wave, both Rijw and Nijw may be observed multiple times, with Rijw observed once for every confidant (up to five) named during the previous wave and Nijw observed once for each of the roster lines (up to five) left available after the retained confidants have been accounted for. We modeled these events jointly using the following two logistic regressions:
In this model, Aij,w−1 consists of covariates that describe each confidant (e.g., whether they have been in jail) named at the previous wave and/or their relationship with the respondent (e.g., the order in which they were named on the roster), while Ziw contains time-varying (including lagged) covariates thought to directly affect the likelihood of retaining and/or naming new confidants (e.g., network size as measured by the total number of confidants named at the previous wave, and a binary indicator of wave 3 versus 2). Si is a respondent-specific latent variable representing network stability, which is hypothesized to positively affect the likelihood of retaining previous confidants and negatively affect the likelihood of naming new ones. This model thus allows us to identify the effect of stability— conceptualized here as a property of a respondent’s network that is stable over the course of the 18-month study—as distinct from other network-level and relationship-level characteristics that may on their own affect the likelihood of renaming a previous confidant and/or naming a new one.
To determine the association between network stability and respondent characteristics, we incorporated the following regression for Si (same as for αi above):
where as before, the e1i are assumed to be distributed normally with mean zero and variance one. We also incorporated the following regression for continuous respondent outcomes Yi observed over the course of the study:
where α1 describes the direct association between the respondent’s jail history at baseline and the subsequent outcome, while α2 describes the association between network stability and the outcome, both adjusting for age and sexual orientation. This model is shown in Figure 1b. As before, an analogous logistic regression was used for binary outcomes.
Finally, to estimate the association between network stability and outcomes adjusting for differences in the prevalence of jail among respondents’ networks (and vice versa), we combined the two GSEMs in Figure 1. For consistency, we modified the model for Aijw as follows:
where only confidants are included (not sex partners). This combined model thus allows us to estimate the association between both network jail prevalence at waves 1 and 2 and network stability from waves 1–2 and 2–3, on the one hand, and longitudinal outcomes on the other, adjusting for respondents’ age, sexual orientation and jail history (yes or no) at baseline.
GSEMs were fit with the gsem command in Stata version 14.1 (StataCorp, 2015), using Full Information Maximum Likelihood (FIML) evaluated via mean-variance adaptive Gauss-Hermite quadrature. For all models with multiple observations per respondent (i.e., mixed effects models and GSEMs), variances were obtained using sandwich (i.e., robust) estimator taking the clustering within respondent into account, to allow for possible misspecification of the model. P-values and confidence intervals were based on the corresponding Wald statistics.
3. Results
3.1 Descriptives
Forty-six percent of the 618 respondents in the study had been in jail at least once. The likelihood of having been in jail increased with age, and was higher among those who identified as bisexual versus those who identified as gay (Table 1, Figure 2a). As has been reported previously, a history of CJI was associated with several HIV related behaviors and poor health outcomes, such as housing instability, using and selling substances, higher likelihood of exposure to violence, a larger number of sexual partners, exchanging sex for money and a higher prevalence of STIs such as HIV and syphilis.
Table 1.
Sociodemographic, behavioral and network characteristics of Wave 1 UConnect participants, overall and by history of criminal justice involvement (N=618)
| Baseline Characteristics | All (N=617) | History of CJI (N=285) | No history of CJI (332) | P valueb |
|---|---|---|---|---|
|
| ||||
| Weighted %a | Weighted %a | Weighted %a | ||
|
|
||||
| Sociodemographics | ||||
| Age (years), mean (SD) | 22.7 (3.3) | 23.4 (3.3) | 22.2 (3.2) | 0.0012 |
| Education | ||||
| Less than high-school (HS) | 8.2 | 10.4 | 6.5 | |
| HS diploma | 38.4 | 37.5 | 39.1 | 0.542 |
| Greater than HS | 53.4 | 52.1 | 54.4 | |
| Employment | ||||
| Unemployed | 52.2 | 53.4 | 51.6 | |
| Part Time | 23.7 | 24.9 | 22.9 | 0.686 |
| Full Time | 24.0 | 21.8 | 25.5 | |
| Housing instability (past 12 months) | 24.0 | 28.9 | 20.7 | 0.063 |
| Low Income (<20,000 annually) | 83.5 | 85.5 | 82.1 | 0.412 |
| Income source: selling drugs | 5.7 | 9.1 | 3.4 | 0.059 |
| Income source: exchanging sex for money | 10.6 | 16.2 | 6.7 | 0.007 |
| Sex behavior | ||||
| Sexual identity (gay) | 59.7 | 50.8 | 66.1 | 0.003 |
| Number of partners in past 6 months, mean (SD) | 3.7 (5.1) | 5.0 (7.3) | 2.9 (2.9) | 0.001 |
| Violence Experiences | ||||
| Had close relative or friend die violently | 60.6 | 65.0 | 57.6 | 0.156 |
| Had close relative injured through violence | 64.5 | 73.1 | 58.4 | 0.003 |
| Had a close relative/friend robbed or attacked | 81.2 | 89.6 | 75.3 | 0.005 |
| Community violence exposure, mean (SD) | 2.9 (1.57) | 3.25 (1.56) | 2.63 (1.51) | <.0001 |
| Substance Use | ||||
| Used any illicit substance c in past 12 months | 74.9 | 89.3 | 64.9 | <.0001 |
| Used crack/cocaine in past 12 months | 3.0 | 5.6 | 1.2 | 0.001 |
| Sexually transmitted infections | ||||
| HIV seropositive | 34.3 | 46.0 | 25.5 | 0.001 |
| Syphilis seropositive | 28.0 | 35.1 | 22.6 | 0.023 |
| Network characteristics | ||||
| At least 1 confidant with history of CJI | 46.7 | 63.9 | 35.2 | <.0001 |
| Proportion of confidant network with CJI, mean (SD) | 0.29 (0.36) | 0.43 (0.41) | 0.20 (0.29) | <.0001 |
| At least 1 sex partner with history of CJI | 39.9 | 59.3 | 26.5 | <.0001 |
| Proportion of sexual network with CJI, mean (SD) | 0.30 (0.39) | 0.44 (0.42) | 0.20 (0.33) | <.0001 |
| Proportion of BMSM community with CJI history | ||||
| None (0%) | 45.2 | 30.0 | 56.0 | |
| A few (1–19%) | 2.8 | 2.8 | 2.9 | |
| Less than half (20–39%) | 16.9 | 18.3 | 15.9 | <.0001 |
| About half (40–59%) | 12.6 | 16.1 | 10.1 | |
| Most (60–79%) | 5.7 | 9.1 | 3.3 | |
| All or almost all (80–100%) | 16.8 | 23.8 | 11.8 | |
| Pooled Wave 2 and 3 outcomesd | ||||
| Reported CJI since last visit | 19.9 | 28.0 | 12.8 | <.0001 |
| HIV infected | 10.1 | 7.96 | 11.9 | 0.302 |
Used stata survey commands with pweight=(Giles Sequential Sampling Weight) to estimate population proportions
P values from Wald chi-square test for categorical variables and t-test for continuous variables
Injection drugs, crack/cocaine, crystal methamphetamine, ecstasy and speed
Outcomes were pooled across study waves. Participants in denominator came to wave 2 or wave 3.
Figure 2.
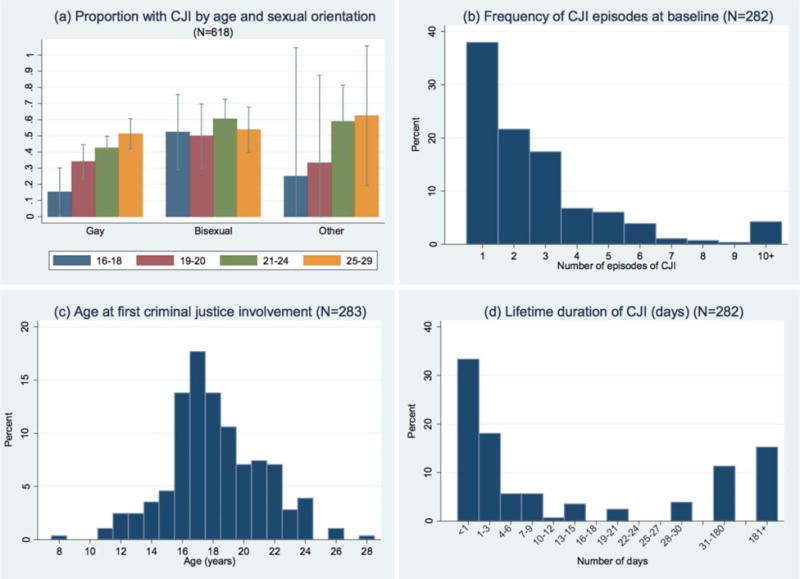
Criminal justice involvement experiences reported by YBMSM (a) Proportion with CJI involvement by age and sexual orientation (b) Frequency of CJI (c) Age at first CJI (d) Duration CJI
Among those who had been in jail, nearly two-thirds (62%) had been in jail more than once, and nearly one-quarter (23%) had been in jail four or more times (Figure 2b). The average age at first detention was 18, with 28% first detained at age 16 or younger (Figure 2c). Although most had spent no more than one week total in jail, a significant minority had spent one month or more (Figure 2d). Twenty percent of respondents reported being in jail at least once during the 18-month study, and this was more likely among those with a history of CJI at baseline than those without (28% versus 13%) (Table 1). This increased the overall percentage of respondents who had been incarcerated to 53% by the end of the study.
3.2 Factors associated with criminal justice involvement
Half of all respondents had at least one confidant who had been in jail, and on average, one-third (29%) of all confidants in respondents’ networks had been in jail. In addition, forty percent of respondents had at least one sexual partner who had been in jail during the past six months. CJI involvement of network members (both confidants and sex partners) was much higher among respondents with CJI involvement themselves. For example, the odds of a confidant having been in jail were 4.04 (95% CI [2.86, 5.70]) times higher if the respondent had also been in jail (Table 2). Moreover, even after taking this into account, there remained considerable clustering in CJI involvement within confidant networks (i.e., the estimated variance of the respondent-level random effect was 1.22, which translates into an odds ratio for a one SD increase of 3.02). Interestingly, although both age and sexual orientation were associated with the likelihood of respondent CJI, neither was associated with the likelihood of CJI among confidants. Finally, the likelihood of newly-acquired confidants (i.e., newly identified in waves 2 and 3) having been in jail was also higher for those with CJI involvement at baseline (OR = 3.51, 95% CI [2.26, 5.45]). There was also modest evidence of an association between jail incidence during the study among respondents and the likelihood of new confidants having been to jail (OR = 1.62, 95% CI [0.95, 2.77]).
Table 2.
Logistic regression models of the likelihood of ever having been in jail, fit to respondents (Wave 1) and their confidants (Wave 1, and new confidants in Waves 2 & 3)
| Respondent characteristics | Respondent ever in jail, Wave 1 (n = 616) | Confidants ever in jail, Wave 1 (n = 1,499) | New confidants in Waves 2 & 3 ever in jail (n = 1.227)a | ||||
|---|---|---|---|---|---|---|---|
| Odds ratio | 95% CI | Odds ratio | 95% CI | Odds ratio | 95% CI | ||
|
|
|||||||
| Age (yrs) | 1.10*** | 1.05, 1.16 | 1.01 | 0.96, 1.07 | 1.04 | 0.97, 1.10 | |
| Sexual orientation | |||||||
| Gay (ref.) | |||||||
| Bisexual | 1.79** | 1.24, 2.59 | 1.10 | 0.77, 1.58 | 1.54+ | 0.99, 2.42 | |
| Other | 1.70 | 0.88, 3.29 | 1.16 | 0.53, 2.53 | 1.70 | 0.63, 4.54 | |
| Respondent jail history | |||||||
| Ever in jail (Wave 1) | 4.04*** | 2.86, 5.70 | |||||
| In jail since last wave | 1.90* | 1.16, 3.12 | |||||
| Wave 3 (vs. 2) | 0.46*** | 0.32, 0.66 | |||||
| Constant | 0.07*** | 0.02, 0.25 | 0.13** | 0.04, 0.44 | 0.09** | 0.02, 0.40 | |
| Var(respondent)b | 1.22 | 0.76, 1.96 | 1.50 | 0.89, 2.52 | |||
p < 0.001;
p < 0.01;
p < 0.05;
p < 0.10
Fit to pooled sample of confidants named in Waves 2 and 3 who had not been named during the previous wave.
Estimated variance of respondent-level random effect.
3.3 Network homophily on CJI and health outcomes
Table 3 shows results of the GSEM in Figure 1a fit separately to a variety of behavioral and health outcomes. Higher prevalence of CJI among respondents’ networks (including both confidants and sex partners) was associated with a higher likelihood of CJI incidence (OR = 1.40, 95% CI [0.97, 2.01]), drug use (OR = 1.48, 95% CI [1.05, 2.10]) and housing instability (OR = 1.45, 95% CI [1.02, 2.06]), and was associated with higher anxiety (coefficient = 0.15, 95% CI [0.03, 0.27]), distress (coefficient = 0.16, 95% CI [0.04, 0.28]) and the tendency to encourage risky sexual behavior (coefficient = 0.15, 95% CI [0.00, 0.29]). In several of these cases, adding network CJI prevalence substantially reduced the association between respondent’s own CJI involvement and the outcome, consistent with the possibility that part of the association between one’s history of CJI and poorer outcomes is due to its effect on the composition of one’s network.
Table 3.
Regression models and Generalized Structural Equation Models (GSEM) fit separately to prospective outcomes, including CJI history and network CJI prevalence as covariatesa
| Outcome (Wave 2 and Wave 3) and covariates (Wave 1) | Regression models incl. respondent jail history only | GSEM models incl. jail history for respondent and network | ||
|---|---|---|---|---|
| A. Binary outcomes | Odds ratio | 95% CI | Odds ratio | 95% CI |
|
|
||||
| CJI | ||||
| Respondent with CJI ever | 2.62*** | (1.63, 4.23) | 1.65 | (0.82, 3.31) |
| Network CJI prevalence | 1.40+ | (0.97, 2.01) | ||
| Drug use (excluding marijuana) | ||||
| Respondent with CJI ever | 2.15*** | (1.42, 3.24) | 1.25 | (0.66, 2.36) |
| Network CJI prevalence | 1.48* | (1.05, 2.10) | ||
| Housing instability | ||||
| Respondent with CJI ever | 1.83** | (1.23, 2.71) | 1.08 | (0.57, 2.08) |
| Network CJI prevalence | 1.45* | (1.02, 2.06) | ||
| Depressed | ||||
| Respondent with CJI ever | 0.97 | (0.60, 1.58) | 0.82 | (0.39, 1.72) |
| Network CJI prevalence | 1.13 | (0.77, 1.64) | ||
| HIV incidence | ||||
| Respondent ever with CJI | 0.89 | (0.35, 2.26) | 1.07 | (0.29, 4.00) |
| Network CJI prevalence | 0.88 | (0.42, 1.85) | ||
| Participated in protests, marchesb | ||||
| Respondent ever with CJI | 0.87 | (0.50, 1.50) | 0.49 | (0.20, 1.19) |
| Network CJI prevalence | 1.49 | (0.91, 2.45) | ||
| B. Ordinal outcomes | Odds ratio | 95% CI | Odds ratio | 95% CI |
|
|
||||
| Frequency of marijuana usec | ||||
| Respondent ever with CJI | 2.89*** | (2.06, 4.06) | 2.11** | (1.27, 3.50) |
| Network CJI prevalence | 1.25+ | (0.97, 1.62) | ||
| C. Continuous outcomes | Coefficient | 95% CI | Coefficient | 95% CI |
|
|
||||
| Anxiety | ||||
| Respondent ever with CJI | 0.12 | (−0.06, 0.29) | −0.10 | (−0.34, 0.14) |
| Network CJI prevalence | 0.15* | (0.03, 0.27) | ||
| Distress | ||||
| Respondent ever in jail | 0.04 | (−0.13, 0.22) | −0.18 | (−0.43, 0.06) |
| Network jail prevalence | 0.16** | (0.04, 0.28) | ||
| Exposure to violenceb | ||||
| Respondent ever in jail | 0.29** | (0.11, 0.47) | 0.19 | (−0.08, 0.46) |
| Network jail prevalence | 0.07 | (−0.07, 0.21) | ||
| Discourage risky sexual behavior | ||||
| Respondent ever in jail | −0.20* | (−0.37, −0.03) | −0.15 | (−0.40, 0.10) |
| Network jail prevalence | −0.04 | (−0.18, 0.10) | ||
| Encourage risky sexual behavior | ||||
| Respondent ever in jail | 0.15+ | (−0.02, 0.33) | −0.06 | (−0.34, 0.23) |
| Network jail prevalence | 0.15* | (0.00, 0.29) | ||
p < 0.001;
p < 0.01;
p < 0.05;
p < 0.10
All models also include age and sexual orientation (both measured at Wave 1) as covariates in the structural part of the model. GSEM models include a respondent-level latent variable capturing differences between respondents in the likelihood that network members have ever been in jail (i.e., differences in network prevalence of jail history). Networks include both confidant and sex network members.
Measured in Wave 3 only.
Measured in Wave 2 only.
3.4 Network stability and health outcomes
Results of the GSEM in Figure 1b—fit initially without the outcomes—are shown in Table 4. As might be expected, the order in which a confidant was named was negatively associated with the likelihood that that confidant was retained at the next wave. Confidants were more likely to be retained at wave 3 (versus wave 2) and new confidants were less likely to be named, possibly reflecting a learning effect (e.g., respondents limiting the number of new confidants in order to avoid being asked for additional information about them). Consistent with our interpretation, network stability was positively associated with the likelihood of retaining previous confidants (OR = 2.28, 95% CI [1.94, 2.68]) and negatively associated with the likelihood of naming new ones (OR = 0.66, 95% CI [0.58, 0.76]). Network stability was greater among older respondents, but substantially less among respondents who had been in jail at baseline (coefficient = −0.48, 95% CI [−0.74, −0.23]). Interestingly, there was no association between whether a specific confidant had been in jail and his or her likelihood of being retained.
Table 4.
Generalized Structural Equation Model (GSEM) showing effect of network stability on the likelihood of retaining confidants from the previous wave and the likelihood of reporting new confidants, fit to pooled changes from W1–W2 and from W2–W3
| A. Probability of retaining previous confidant | |||
|---|---|---|---|
| Odds ratio | p-value | 95% CI | |
|
|
|||
| Relationship attributes (last wave) | |||
| Order named (1–5) | 0.66 | < 0.001 | (0.60, 0.72) |
| Confidant ever with CJI | 1.07 | 0.531 | (0.87, 1.30) |
| Respondent attributes | |||
| No. of alters (last wave) | 1.16 | 0.003 | (1.05, 1.29) |
| Network stability (latent) | 2.28 | < 0.001 | (1.94, 2.68) |
| Wave 3 (vs. Wave 2) | 1.30 | 0.003 | (1.09, 1.55) |
| B. Probability of reporting new confidant | |||
| Odds ratio | p-value | 95% CI | |
|
|
|||
| Respondent attributes | |||
| No. of alters (last wave) | 0.90 | 0.003 | (0.84, 0.97) |
| Network stability (latent) | 0.66 | < 0.001 | (0.58, 0.76) |
| Wave 3 (vs. Wave 2) | 0.82 | 0.004 | (0.72, 0.94) |
| C. Regression of confidant network stability on Wave 1 respondent characteristics | |||
| Coefficient | p-value | 95% CI | |
|
|
|||
| Age (per year) | 0.08 | < 0.001 | (0.04, 0.12) |
| Ever with CJI | −0.48 | < 0.001 | (−0.74, −0.23) |
| Sexual orientation | |||
| Gay (ref.) | |||
| Bisexual | −0.04 | 0.784 | (−0.32, 0.24) |
| Other | −0.13 | 0.700 | (−0.78, 0.52) |
The association between confidant network stability and outcomes is shown in Table 5. Despite adjusting for respondents’ CJI history, network stability was associated with a reduction in the likelihood of drug use (OR = 0.76, 95% CI [0.55, 1.04]), housing instability (OR = 0.70, 95% CI [0.52, 0.95]) and depression (OR = 0.67, 95% CI [0.45, 0.99]). Network stability was also associated with less distress (coefficient = −0.15, 95% CI [−0.29, −0.01]) and exposure to violence (coefficient = −0.15, 95% CI [−0.27, −0.03]). Finally, those with more stable networks were less likely to participate in protests, demonstrations, etc. (OR = 0.64, 95% CI [0.43, 0.95]). These effects were essentially unchanged when adjusting for the prevalence of CJI involvement in the confidant network, indicating that stability and CJI involvement represent distinct mechanisms by which social networks may affect outcomes in this population.
Table 5.
Generalized Structural Equation Models (GSEM) fit separately to outcomes, including respondent CJI history (Wave 1), confidant network CJI prevalence (Waves 1 & 2) and confidant network stability (W1–W3) as covariatesa
| Models incl. respondent jail history and network stability | Models incl. respondent jail history, network stability and confidant jail history | |||
|---|---|---|---|---|
| Outcome (Wave 2 and Wave 3) and covariates | ||||
| A. Binary outcomes | Odds ratio | 95% CI | Odds ratio | 95% CI |
|
|
||||
| In jail | ||||
| Respondent ever with CJI (Wave 1) | 2.45*** | (1.49, 4.04) | 1.86* | (1.01, 3.41) |
| Network stability (since last wave) | 0.80 | (0.57, 1.14) | 0.80 | (0.56, 1.15) |
| Network CJI prevalence (last wave) | 1.31+ | (0.97, 1.78) | ||
| Drug use (excluding marijuana) | ||||
| Respondent ever with CJI (Wave 1) | 1.85** | (1.21, 2.83) | 1.53 | (0.90, 2.59) |
| Network stability (since last wave) | 0.76+ | (0.55, 1.04) | 0.76+ | (0.56, 1.04) |
| Network CJI prevalence (last wave) | 1.20 | (0.91, 1.58) | ||
| Housing instability | ||||
| Respondent ever with CJI (Wave 1) | 1.56* | (1.01, 2.43) | 1.28 | (0.75, 2.16) |
| Network stability (since last wave) | 0.70* | (0.52, 0.95) | 0.70* | (0.51, 0.96) |
| Network CJI prevalence (last wave) | 1.21 | (0.93, 1.59) | ||
| Depressed | ||||
| Respondent ever with CJI (Wave 1) | 0.78 | (0.46, 1.32) | 0.76 | (0.41, 1.41) |
| Network stability (since last wave) | 0.67* | (0.45, 0.99) | 0.67* | (0.45, 0.99) |
| Network CJI prevalence (last wave) | 1.03 | (0.75, 1.41) | ||
| HIV incidence | ||||
| Respondent ever with CJI (Wave 1) | 1.02 | (0.37, 2.83) | 1.41 | (0.42, 4.80) |
| Network stability (since last wave) | 1.36 | (0.72, 2.57) | 1.35 | (0.70, 2.60) |
| Network CJI prevalence (last wave) | 0.76 | (0.43, 1.34) | ||
| Participated in protests, marches, etc.b | ||||
| Respondent ever with CJI (Wave 1) | 0.68 | (0.38, 1.20) | 0.50+ | (0.25, 1.01) |
| Network stability (since last wave) | 0.64* | (0.43, 0.95) | 0.64* | (0.43, 0.95) |
| Network CJI prevalence (last wave) | 1.33 | (0.87, 2.05) | ||
| B. Ordinal outcomes | Odds ratio | 95% CI | Odds ratio | 95% CI |
|
|
||||
| Frequency of marijuana usec | ||||
| Respondent ever with CJI (Wave 1) | 2.90*** | (2.02, 4.16) | 2.61*** | (1.66, 4.10) |
| Network stability (since last wave) | 1.03 | (0.82, 1.30) | 1.03 | (0.82, 1.30) |
| Network CJI prevalence (last wave) | 1.10 | (0.88, 1.37) | ||
| C. Continuous outcomes | Coefficient | 95% CI | Coefficient | 95% CI |
|
|
||||
| Anxiety | ||||
| Respondent ever with CJI (Wave 1) | 0.06 | (−0.13, 0.25) | −0.07 | (−0.29, 0.15) |
| Network stability (since last wave) | −0.10 | (−0.25, 0.04) | −0.10 | (−0.24, 0.04) |
| Network CJI prevalence (last wave) | 0.12* | (0.02, 0.22) | ||
| Distress | ||||
| Respondent ever with CJI (Wave 1) | −0.04 | (−0.22, 0.14) | −0.14 | (−0.35, 0.07) |
| Network stability (since last wave) | −0.15* | (−0.29, −0.01) | −0.15* | (−0.29, −0.01) |
| Network CJI prevalence (last wave) | 0.09+ | (−0.01, 0.20) | ||
| Exposure to violenceb | ||||
| Respondent ever with CJI (Wave 1) | 0.21* | (0.03, 0.38) | 0.16 | (−0.06, 0.38) |
| Network stability (since last wave) | −0.15* | (−0.27, −0.03) | −0.15* | (−0.27, −0.02) |
| Network CJI prevalence (last wave) | 0.05 | (−0.06, 0.16) | ||
| Discourage risky sexual behavior | ||||
| Respondent ever with CJI (Wave 1) | −0.19* | (−0.36, −0.01) | −0.22* | (−0.42, −0.01) |
| Network stability (since last wave) | 0.04 | (−0.09, 0.16) | 0.04 | (−0.09, 0.16) |
| Network CJI prevalence (last wave) | 0.03 | (−0.09, 0.14) | ||
| Encourage risky sexual behavior | ||||
| Respondent ever in jail (Wave 1) | 0.14 | (−0.05, 0.33) | −0.07 | (−0.31, 0.17) |
| Network stability (since last wave) | 0.01 | (−0.14, 0.11) | −0.01 | (−0.14, 0.12) |
| Network jail prevalence (last wave) | 0.19** | (0.06, 0.32) | ||
p < 0.001;
p < 0.01;
p < 0.05;
p < 0.10
Models include age and sexual orientation (both measured at Wave 1) as covariates in the structural part of the model. The measurement model for network stability is identical to that for the model in Table 4. Measurement models fit to pooled dataset of network changes from W1–W2 and from W2–W3.
Measured in Wave 3 only.
Measured in Wave 2 only.
4. Discussion
The uConnect sample is one of the first representative samples of young Black MSM and the largest single location sample of young Black MSM. Within uConnect we find high rates of CJI, with nearly half of respondents experiencing CJI prior to the baseline interview. This high rate of CJI is similar to those reported in other cohorts of YBMSM (Brewer et al., 2014a, 2014b; Lim et al., 2011).
We also observe a high rate of homophily with respect to CJI, reflected not only in the tendency of respondents with a history of CJI to name confidants who also have a history of CJI but also in the clustering of CJI within confidant networks (i.e., even after adjusting for respondent/alter homophily). This CJI homophily raises questions about the possible underlying mechanisms and their relationship to subsequent CJI. For example, despite adjusting for the well documented association between one’s past and future CJI (Gendreau, Little, & Goggin, 1996; Uggen, 2000)), our data suggest an association between past network CJI and a respondent’s subsequent CJI. Moreover, both past and current CJI (i.e., during the study period) are associated with the likelihood that new confidants will have a history of CJI. This strong evidence for an association between network CJI and one’s own CJI has important implications for recidivism interventions which have tended to focus only on the individual (Lipsey & Cullen, 2007; MacKenzie, Wilson, & Kider, 2001). At the same time however, more work is needed to disentangle the effects of one’s network on one’s own CJI (e.g., via peer influence regarding behaviors that are tied to CJI such as drug use) from the effects of CJI on one’s network (e.g., via consequences such as unemployment which create circumstances for other close network members to become involved in criminal justice (The Pew Charitable Trusts, 2010)). The direct relationship between unemployment and recidivism and the impacts of recidivism on unemployment are well established. Important health effects from recidivism, including virological failure in HIV infected persons and the resulting poor health, can also serve as indirect effects on future employment.(J. P. Meyer et al., 2014)
In addition to future episodes of CJI, we also find evidence of strong associations between network CJI and a range of important health and social outcomes, and this appears to account for a large portion of the association between an individual’s prior experiences with CJI and such outcomes. For example, adding network CJI prevalence to models predicting drug use and housing instability yields significant coefficients and substantially reduces the (previously large) effect of the respondent’s own CJI involvement. Drug use usually occurs with other network members and housing instability is related to an ability to secure housing within networks which themselves may be subject to housing instability due to CJI. Network CJI was also associated with higher levels of anxiety and distress. An explanation for this finding may be that network CJI involvement limits access to the types of relationships that are required to maintain mental health (Kawachi & Berkman, 2001) and/or creates situations of economic and social instability which further exacerbate mental health problems by those who are left to manage life on the outside (Christian, Mellow, & Thomas, 2006; Mumola, 2000).
Finally, there is strong evidence that network stability affects both an individual’s likelihood to have CJI as well as specific health and social outcomes. These effects were essentially unchanged when adjusting for the prevalence of CJI involvement in the confidant network, indicating that stability and CJI involvement represent distinct mechanisms by which social networks may affect outcomes in this population. Network instability reflects instability in the broader social environment which may include lack of reliable familial and other social support. Previous research has shown that network instability with emphasis on network losses is associated with increased morbidity (d’Epinay, 2010; Gerstorf, Rocke, & Lachman, 2011; Stroebe, 2007). These circumstances may be different from CJI network homophily. Network instability can include loss and gain of individuals who are CJI involved as well as loss and gain of those who are not. For gains and losses of CJI network members, there is limited evidence that gaining or losing these individuals has any net benefit on the health and well-being of individuals. Regardless of CJI involvement, network members who are designated as confidants often provide social support and their presence have been shown to be associated with health outcomes and behaviors such as excessive risk taking (J. Schneider et al., 2012). Network stability, thus exhibits protective qualities with respect to health and social outcomes. It should be noted that one of our outcomes, participation in protest movements around police brutality was associated with network instability. While it may be that social justice efforts are of benefit if realized in marginalized communities, the motivation of specific individuals to these movements may be based upon previous experiences with criminal justice systems or other systems deemed to be oppressive (Klandermans, 2007). The role that CJI persons participating in political movements plays requires additional study to determine what are the drivers of involvement in such movements and whether network instability is a driver or symptom of this participation.
There were several limitations to our analysis. First, our analysis was underpowered to determine how CJI networks and network instability might be related to incident HIV infection. We find that over 1/3 of our sample was HIV infected at baseline and that nearly 40 new infections occurred over the 18 month study period. While it is likely that network change and HIV status homophily are linked to incident HIV, these network factors are distal to more proximal causes of HIV transmission such as sex risk behavior and use of some substances (Fujimoto K, in press; Valleroy et al., 2000). Careful attention to these proximal factors in the context of network change would be required in the analyses to examine HIV infection in more detail and was beyond the scope of this analysis. Second, our measure of CJI was not limited to longer jail and prison stays, but included arrest and other shorter term detention. It is unclear whether network stability and CJI homophily is based upon the duration of stay. We find that any CJI at the individual level is associated with important health outcomes when controlling for duration of stay and the main impact that CJI has on health outcomes occurs when CJI events are recurring or cyclical in nature (data not shown). Additional work should examine the relative importance of the different categories of involvement (including probation) and how these impact network composition and dynamism. Finally, we did not explore the potential association between geographic propinquity to crime and its association with future criminal justice involvement. Others have found spatial proximity to be an important factor in future behaviors (Schafer, 2015). For example, Papachristos finds that adjacency of gang turf is independently associated with violence (Papachristos, Hureau, & Braga, 2013). He finds that both networks and spatial properties are important generators of gang violence, however, spatial proximity does not limit the effect of social ties on gang violence. We would expect that spatial proximity would have less of an effect on CJI or health behaviors given that the population we focus on is highly mobile. The high mobility is evidenced by socializing that occurs outside of local communities throughout the city with over half of sex partners, for example, found outside of local community areas (data not shown).
In conclusion, this analysis is the first to describe the networks of CJI MSM among a representative sample of MSM and to examine the relationship between network composition, stability and important social and health outcomes. We find that individuals who are criminal justice involved MSM are highly likely to be associated with other CJI MSM in both their confidant and sexual networks. In addition, these networks exhibit limited network stability and both the composition of network members who are CJI and the network dynamism have independent effects on health and social outcomes over time. Most notable among these are the effects on drug use and mental health indicators such as anxiety and depression. Health interventions that focus on the individual are thus unlikely to be effective in limiting morbidity and focus on networks of CJI involved persons and those they are connected to are likely to be more effective in achieving outcomes of interest (Bouris et al., 2013). Moreover, recent limitations in programming that have defunded mental health, housing and substance use treatment initiatives in Chicago and elsewhere could exacerbate the impact that networks change due to CJI may have on marginalized populations in the United States.
Highlights.
Examine the networks of criminal justice involved (CJI) young Black MSM from a population-based cohort
CJI respondents are more likely to have CJI homophily in their confidant and sexual networks
Higher prevalence of network CJI is associated with increased turnover in the confidant network
Network CJI and network instability are related to important health and social outcomes
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Adimora AA, Schoenbach VJ. Social context, sexual networks, and racial disparities in rates of sexually transmitted infections. J Infect Dis. 2005;191(Suppl 1):S115–122. doi: 10.1086/425280. [DOI] [PubMed] [Google Scholar]
- Adimora AA, Schoenbach VJ, Martinson F, Donaldson KH, Stancil TR, Fullilove RE. Concurrent sexual partnerships among African Americans in the rural south. Ann Epidemiol. 2004;14(3):155–160. doi: 10.1016/S1047-2797(03)00129-7. [DOI] [PubMed] [Google Scholar]
- Adimora AA, Schoenbach VJ, Martinson FE, Donaldson KH, Stancil TR, Fullilove RE. Concurrent partnerships among rural African Americans with recently reported heterosexually transmitted HIV infection. J Acquir Immune Defic Syndr. 2003;34(4):423–429. doi: 10.1097/00126334-200312010-00010. [DOI] [PubMed] [Google Scholar]
- Arnold EAS,E, Jonas A, Pollack L. HIV-related Social Support and Social Support Network Structures are related to sexual risk behavior and delayed testing in the San Francisco Bay Area House Ball Community. Global Public Health [Google Scholar]
- Beck AJ, H P, Berzofsky M, Caspar R, Krebs C. National Inmate Survey, 2008–09. Washington, D.C: U.S. Department of Justice; 2010. Sexual Victimization in Prisons and Jails Reported by Inmates, 2008–2009. [Google Scholar]
- Behind Bars II: Substance Abuse and America’s Prison Population. 2010 Retrieved October 6 2014, from http://www.casacolumbia.org/download/file/fid/487.
- Belenko S, Langley S, Crimmins S, Chaple M. HIV risk behaviors, knowledge, and prevention education among offenders under community supervision: A hidden risk group. Aids Education and Prevention. 2004;16(4):367–385. doi: 10.1521/aeap.16.4.367.40394. [DOI] [PubMed] [Google Scholar]
- Binswanger IA, Redmond N, Steiner JF, Hicks LS. Health disparities and the criminal justice system: an agenda for further research and action. J Urban Health. 2012;89(1):98–107. doi: 10.1007/s11524-011-9614-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bland SE, Mimiaga MJ, Reisner SL, White JM, Driscoll MA, Isenberg D, Mayer KH. Sentencing risk: history of incarceration and HIV/STD transmission risk behaviours among Black men who have sex with men in Massachusetts. Cult Health Sex. 2012;14(3):329–345. doi: 10.1080/13691058.2011.639902. [DOI] [PubMed] [Google Scholar]
- Blankenship KM, Smoyer AB, Bray SJ, Mattocks K. Black-White disparities in HIV/AIDS: The role of drug policy and the corrections system. Journal of Health Care for the Poor and Underserved. 2005;16:140–156. doi: 10.1353/hpu.2005.0110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bouris A, Voisin D, Pilloton M, Flatt N, Eavou R, Hampton K, Schneider JA. Project nGage: Network Supported HIV Care Engagement for Younger Black Men Who Have Sex with Men and Transgender Persons. J AIDS Clin Res. 2013;4 doi: 10.4172/2155-6113.1000236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boutwell A, Rich JD. HIV Infection Behind Bars. Clinical Infectious Diseases. 2004;38:1761–1763. doi: 10.1086/421410. [DOI] [PubMed] [Google Scholar]
- Bowleg L. When Black plus Lesbian plus Woman not equal Black Lesbian Woman: The methodological challenges of qualitative and quantitative intersectionality research. Sex Roles. 2008;59(5–6):312–325. doi: 10.1007/s11199-008-9400-z. [DOI] [Google Scholar]
- Bowleg L, Teti M, Malebranche DJ, Tschann JM. “It’s an uphill battle everyday”: Intersectionality, low-income Black heterosexual men, and implications for HIV prevention research and interventions. Psychology of men & masculinity. 2013;14(1):25. doi: 10.1037/a0028392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Braithwaite RL, Arriola KR. Male prisoners and HIV prevention: a call for action ignored. Am J Public Health. 2003;93(5):759–763. doi: 10.2105/ajph.93.5.759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Braithwaite RL, Hammett T, Arriola KRJ. Introduction to the Special Issue: HIV/AIDS in Correctional Settings. AIDS Education and Prevention. 2002;14(Supplement B):1–6. [Google Scholar]
- Brewer RA, Magnus M, Kuo I, Wang L, Liu TY, Mayer KH. Exploring the relationship between incarceration and HIV among black men who have sex with men in the United States. J Acquir Immune Defic Syndr. 2014a;65(2):218–225. doi: 10.1097/01.qai.0000434953.65620.3d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brewer RA, Magnus M, Kuo I, Wang L, Liu TY, Mayer KH. The high prevalence of incarceration history among Black men who have sex with men in the United States: associations and implications. Am J Public Health. 2014b;104(3):448–454. doi: 10.2105/AJPH.2013.301786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Browning S MS, Lisa M. Criminal incarceration dividing the ties that bind: black men and their families. J Afr Am Men. 2001;6(1):87–102. [Google Scholar]
- Butler B. Jails and Health Information Technology: A Framework for Creating Connectivity. Community Oriented Correctional Health Services 2012 [Google Scholar]
- Carson EA. In: Prisoners in 2014. BoJ Statistics, editor. Bureau of Justice Statistics; 2015. [Google Scholar]
- Centers for Disease Control and Prevention. HIV Among African American Gay and Bisexual Men. 2015 Retrieved May, 2016 from http://www.cdc.gov/hiv/group/msm/bmsm.html.
- Chicago Police Department. CLEARMAP Crime Summary. Retrieved January 5, 2013 from http://gis.chicagopolice.org/CLEARMap_crime_sums/startPage.htm#.
- Chicago Policy Research Team. Deserted?: A Policy Report on Food Access in Four South Side Chicago Neighborhoods: The Chicago Policy Research Team 2010 [Google Scholar]
- Christian J, Mellow J, Thomas S. Social and economic implications of family connections to prisoners. Journal of Criminal Justice. 2006;34(4):443–452. doi: 10.1016/j.jcrimjus.2006.05.010. [DOI] [Google Scholar]
- Comfort M, Grinstead O, McCartney K, Bourgois P, Knight K. “You cannot do nothing in this damn place”: sex and intimacy among couples with an incarcerated male partner. J Sex Res. 2005;42(1):3–12. doi: 10.1080/00224490509552251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cornwell B. Social disadvantage and network turnover. J Gerontol B Psychol Sci Soc Sci. 2015;70(1):132–142. doi: 10.1093/geronb/gbu078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cornwell BS,PL, Laumann EO, Kim J, Kim YJ. Assessment of social network change in a National Longitudinal Survey. Journals of Gerontology, Series B: Psychological Sciences and Social Sciences. 2014;69(Suppl 2):S75–S82. doi: 10.1093/geronb/gbu037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cornwell EY, Waite LJ. Social disconnectedness, perceived isolation, and health among older adults. J Health Soc Behav. 2009;50(1):31–48. doi: 10.1177/002214650905000103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- d’Epinay CJC,S, Guillet LA. Bereavement in very old age: impact on health and relationships of the loss of a spouse, a child, a sibling, or a close friend. OMEGA-Journal of Death and Dying. 2010;60(4):301–325. doi: 10.2190/om.60.4.a. [DOI] [PubMed] [Google Scholar]
- Derogatis LR. NCS Pearson, Incorporated. 2001. Brief Symptom Inventory 18: Administration, scoring and procedures manual. [Google Scholar]
- Dumond R. Inmate sexual assault: The plague that persists. The Prison Journal. 2000;80:407–414. [Google Scholar]
- Epperson M, El-Bassel N, Gilbert L, Orellana E, Chang M. Increased HIV risk associated with criminal justice involvement among men on methadone. AIDS and Behavior. 2008;12(1):51–57. doi: 10.1007/s10461-007-9298-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Epperson MW, El-Bassel N, Chang M, Gilbert L. Examining the temporal relationship between criminal justice involvement and sexual risk behaviors among drug-involved men. Journal of Urban Health. 2010;87(2):324–336. doi: 10.1007/s11524-009-9429-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Finneran C, Stephenson R. Intimate partner violence among men who have sex with men: a systematic review. Trauma Violence Abuse. 2013;14(2):168–185. doi: 10.1177/1524838012470034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Freudenberg N. Jails, prisons, and the health of urban populations: a review of the impact of the correctional system on community health. J Urban Health. 2001;78(2):214–235. doi: 10.1093/jurban/78.2.214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Freudenberg N, Daniels J, Crum M, Peridns T, Richie BE. Coming home from jail: The social and health consequences of community reentry for women, male adolescents, and their families and communities. American Journal of Public Health. 2005;95(10):1725–1736. doi: 10.2105/AJPH.2004.056325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Friedman SR, Bolyard M, Maslow C, Mateu-Gelabert P, Sandoval M. Harnessing the power of social networks to reduce HIV risk. Focus. 2005;20(1):5–6. [PubMed] [Google Scholar]
- Friedman SR, Bolyard M, Mateu-Gelabert P, Goltzman P, Pawlowicz MP, Singh DZ, Flom PL. Some data-driven reflections on priorities in AIDS network research. AIDS Behav. 2007;11(5):641–651. doi: 10.1007/s10461-006-9166-7. [DOI] [PubMed] [Google Scholar]
- Friedman SR, Maslow C, Bolyard M, Sandoval M, Mateu-Gelabert P, Neaigus A. Urging others to be healthy: “intravention” by injection drug users as a community prevention goal. AIDS Educ Prev. 2004;16(3):250–263. doi: 10.1521/aeap.16.3.250.35439. [DOI] [PubMed] [Google Scholar]
- Friedman SR, Sandoval M, Mateu-Gelabert P, Rossi D, Gwadz M, Dombrowski K, Perlman D. Theory, measurement and hard times: some issues for HIV/AIDS research. AIDS Behav. 2013;17(6):1915–1925. doi: 10.1007/s10461-013-0475-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fujimoto K, K J-Y, Ross MW, Williams L. Multiplex crack smoking and sexual networks: Associations between network members’ incarceration and HIV risks among high-risk MSM. Journal of Behavioral Medicine. doi: 10.1007/s10865-016-9754-6. (in press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gendreau P, Little T, Goggin C. A meta-analysis of the predictors of adult offender recidivism: What works. Criminology. 1996;34(4):575–607. doi: 10.1111/j.1745-9125.1996.tb01220.x. [DOI] [Google Scholar]
- Gerstorf D, Rocke C, Lachman ME. Antecedent-consequent relations of perceived control to health and social support: longitudinal evidence for between-domain associations across adulthood. J Gerontol B Psychol Sci Soc Sci. 2011;66B(1):61–71. doi: 10.1093/geronb/gbq077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gile KJ, Handcock MS. Respondent-Driven Sampling: An Assessment of Current Methodology. Sociol Methodol. 2010;40(1):285–327. doi: 10.1111/j.1467-9531.2010.01223.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glaze L, Kaeble D, Tsoutis A, Minton T. Correctional Populations in the United States, 2014. In: Bureau of Justice Statistics, editor. Correctional Populations in the United States. Bureau of Justice Statistics; 2015. [Google Scholar]
- Golembeski C, Fullilove R. Criminal (in)justice in the city and its associated health consequences. Am J Public Health. 2005;95(10):1701–1706. doi: 10.2105/AJPH.2005.063768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grant RM, Lama JR, Anderson PL, McMahan V, Liu AY, Vargas L, iPrEx Study, T. Preexposure chemoprophylaxis for HIV prevention in men who have sex with men. N Engl J Med. 2010;363(27):2587–2599. doi: 10.1056/NEJMoa1011205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hammett TM, Gaiter JL, Crawford C. Reaching seriously at-risk populations: Health interventions in criminal justice settings. Health Education & Behavior. 1998;25(1):99–120. doi: 10.1177/109019819802500108. [DOI] [PubMed] [Google Scholar]
- Hammett TM, Harmon MP, Rhodes W. The burden of infectious disease among inmates of and releasees from US correctional facilities, 1997. Am J Public Health. 2002;92(11):1789–1794. doi: 10.2105/ajph.92.11.1789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hammett TM, Roberts C, Kennedy S. Health-related issues in prisoner reentry. Crime & Delinquency. 2001;47(3):390–411. [Google Scholar]
- Harawa NT, Sweat J, George S, Sylla M. Sex and condom use in a large jail unit for men who have sex with men (MSM) and male-to-female transgenders. J Health Care Poor Underserved. 2010;21(3):1071–1087. doi: 10.1353/hpu.0.0349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harrison P, Beck A. Prison and jail inmates at midyear 2005. Bureau of Justice Statistics Bulletin, NCJ 213133. 2006:1–13. [Google Scholar]
- Hedrich D, Alves P, Farrell M, Stover H, Moller L, Mayet S. The effectiveness of opioid maintenance treatment in prison settings: a systematic review. Addiction. 2012;107(3):501–517. doi: 10.1111/j.1360-0443.2011.03676.x. [DOI] [PubMed] [Google Scholar]
- Hensley C, Tewksbury R, Castle T. Characteristics of prison sexual assault targets in male Oklahoma correctional facilities. Journal of Interpersonal Violence. 2003;18(6):595–606. doi: 10.1177/0886260503251132. [DOI] [PubMed] [Google Scholar]
- Jones SR, McEwen MK. A conceptual model of multiple dimensions of identity. Journal of College Student Development. 2000;41(4):405–414. [Google Scholar]
- Kawachi I, Berkman LF. Social ties and mental health. Journal of Urban Health-Bulletin of the New York Academy of Medicine. 2001;78(3):458–467. doi: 10.1093/jurban/78.3.458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Mickelson KD, Williams DR. The prevalence, distribution, and mental health correlates of perceived discrimination in the United States. J Health Soc Behav. 1999;40(3):208–230. [PubMed] [Google Scholar]
- Khan MR, Doherty I, Schoenbach VJ, Taylor E, Epperson M, Adimora AA. Incarceration and high-risk sexual partnerships among men in the United States. Journal of Urban Health. 2009a;86(4):584–601. doi: 10.1007/s11524-009-9348-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khan MR, Doherty IA, Schoenbach VJ, Taylor EM, Epperson MW, Adimora AA. Incarceration and High-Risk Sex Partnerships among Men in the United States. Journal of Urban Health-Bulletin of the New York Academy of Medicine. 2009b;86(4):584–601. doi: 10.1007/s11524-009-9348-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khan MR, Golin CE, Friedman SR, Scheidell JD, Adimora AA, Judon-Monk S, Wohl DA. STI/HIV Sexual Risk Behavior and Prevalent STI Among Incarcerated African American Men in Committed Partnerships: The Significance of Poverty, Mood Disorders, and Substance Use. AIDS Behav. 2015;19(8):1478–1490. doi: 10.1007/s10461-015-1062-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khan MR, Wohl DA, Weir SS, Adimora AA, Moseley C, Norcott K, Miller WC. Incarceration and risky sexual partnerships in a Southern US city. Journal of Urban Health-Bulletin of the New York Academy of Medicine. 2008;85(1):100–113. doi: 10.1007/s11524-007-9237-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khanna AS, Michaels S, Skaathun B, Morgan E, Green K, Young L, uConnect Study, T. Preexposure Prophylaxis Awareness and Use in a Population-Based Sample of Young Black Men Who Have Sex With Men. JAMA Intern Med. 2016;176(1):136–138. doi: 10.1001/jamainternmed.2015.6536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- King KM, Voisin DR, Diclemente RJ. The Relationship Between Male Gang Involvement and Psychosocial Risks for their Female Juvenile Justice Partners with Non-gang Involvement Histories. Journal of Child and Family Studies. 2015;24(9):2555–2559. doi: 10.1007/s10826-014-0057-7. [DOI] [Google Scholar]
- Klandermans B. The Demand and Supply of Participation: Social-Psychological correlates of participation in social movements. In: S S, Snow DA, Kriesi H, editors. The Blackwell Companion to Social Movements. Oxford, UK: Blackwell Publishing; 2007. [Google Scholar]
- Klest B. Childhood Trauma, Poverty, and Adult Victimization. Psychological Trauma-Theory Research Practice and Policy. 2012;4(3):245–251. doi: 10.1037/a0024468. [DOI] [Google Scholar]
- Krebs CP, Simmons M. Intraprison HIV transmission: an assessment of whether it occurs, how it occurs, and who is at risk. AIDS Educ Prev. 2002;14(5 Suppl B):53–64. doi: 10.1521/aeap.14.7.53.23865. [DOI] [PubMed] [Google Scholar]
- Larney S. Does opioid substitution treatment in prisons reduce injecting-related HIV risk behaviours? A systematic review. Addiction. 2010;105(2):216–223. doi: 10.1111/j.1360-0443.2009.02826.x. [DOI] [PubMed] [Google Scholar]
- Latkin CA, Forman V, Knowlton A, Sherman S. Norms, social networks, and HIV-related risk behaviors among urban disadvantaged drug users. Soc Sci Med. 2003;56(3):465–476. doi: 10.1016/s0277-9536(02)00047-3. [DOI] [PubMed] [Google Scholar]
- Laumann EOG,J, Michael R, Michaels S. The social organization of sexuality: Sexual Practices in the United States. Chicago: University of Chicago Press; 1994. [Google Scholar]
- Lim JR, Sullivan PS, Salazar L, Spaulding AC, Dinenno EA. History of arrest and associated factors among men who have sex with men. J Urban Health. 2011;88(4):677–689. doi: 10.1007/s11524-011-9566-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lipsey MW, Cullen FT. The effectiveness of correctional rehabilitation: A review of systematic reviews. Annual Review of Law and Social Science. 2007;3:297–320. doi: 10.1146/annurev.lawsocsci.3.081806.112833. [DOI] [Google Scholar]
- Lopoo LM, Western B. Incarceration and the formation and stability of marital unions. Journal of Marriage and Family. 2005;67(3):721–734. doi: 10.1111/j.1741-3737.2005.00165.x. [DOI] [Google Scholar]
- Lubelczyk RA, Friedmann PD, Lemon SC, Stein MD, Gerstein DR. HIV prevention services in correctional drug treatment programs: do they change risk behaviors? AIDS Educ Prev. 2002;14(2):117–125. doi: 10.1521/aeap.14.2.117.23898. [DOI] [PubMed] [Google Scholar]
- Luther JB, Reichert ES, Holloway ED, Roth AM, Aalsma MC. An exploration of community reentry needs and services for prisoners: a focus on care to limit return to high-risk behavior. AIDS Patient Care and STDs. 2011;25(8):475–481. doi: 10.1089/apc.2010.0372. [DOI] [PubMed] [Google Scholar]
- MacKenzie DL, Wilson DB, Kider SB. Effects of correctional boot camps on offending. Annals of the American Academy of Political and Social Science. 2001;578:126–143. doi: 10.1177/0002716201578001008. [DOI] [Google Scholar]
- Mari Gallagher Research & Consulting Group. Examining the impact of food deserts on public health in Chicago 2007 [Google Scholar]
- Maruschak LM. HIV in Prisons, 2007–08. Washington, D.C.: Dept of Justice Bureau of Justice Statistics; 2009. [Google Scholar]
- Mateu-Gelabert P, Bolyard M, Maslow C, Sandoval M, Flom PL, Friedman SR. For the common good: measuring residents’ efforts to protect their community from drug- and sex-related harm. SAHARA J. 2008;5(3):144–157. doi: 10.1080/17290376.2008.9724913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mauer M. Addressing Racial Disparities in Incarceration. The Prison Journal. 2011;91(3):875–1015. [Google Scholar]
- McQuillan GM, Kruszon-Moran D, Kottiri BJ, Kamimoto LA, Lam L, Cowart MF, Spira TJ. Prevalence of HIV in the US household population: the National Health and Nutrition Examination Surveys, 1988 to 2002. J Acquir Immune Defic Syndr. 2006;41(5):651–656. doi: 10.1097/01.qai.0000194235.31078.f6. [DOI] [PubMed] [Google Scholar]
- Meyer IH, Flores AR, Stemple L, Romero AP, Wilson BD, Herman JL. Incarceration Rates and Traits of Sexual Minorities in the United States: National Inmate Survey, 2011–2012. Am J Public Health. 2017;107(2):267–273. doi: 10.2105/AJPH.2016.303576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meyer JP, Cepeda J, Springer SA, Wu J, Trestman RL, Altice FL. HIV in people reincarcerated in Connecticut prisons and jails: an observational cohort study. Lancet HIV. 2014;1(2):e77–e84. doi: 10.1016/S2352-3018(14)70022-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Millett GA, Peterson JL, Flores SA, Hart TA, Jeffries WLt, Wilson PA, Remis RS. Comparisons of disparities and risks of HIV infection in black and other men who have sex with men in Canada, UK, and USA: a meta-analysis. Lancet. 2012;380(9839):341–348. doi: 10.1016/s0140-6736(12)60899-x. [DOI] [PubMed] [Google Scholar]
- Minton TDZ,Z. Jail Inmates at Midyear 2014. In: Bureau of Justice Statistics, editor. Prison and Jail Inmates at Midyear. 2015. [Google Scholar]
- Moore J. The Unintended Consequences of Incarceration. New York, NY: Vera Institute of Justice; 1996. Bearing the burden: how incarceration weakens inner-city communities. [Google Scholar]
- Morgan E, Khanna A, Livak B, Voisin D, Young LE, Coombs B, Friedman S, Chang M, DuVoisin R, Michaels S, Schneider JA. Marijuana use among young men who have sex with men and the HIV Care Continuum: Findings from the uConnect Study (in press) Substance Use and Misuse. 2016 doi: 10.1080/10826084.2016.1197265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mossakowski KN. Coping with perceived discrimination: does ethnic identity protect mental health? J Health Soc Behav. 2003;44(3):318–331. [PubMed] [Google Scholar]
- Mouttapa M, Watson DW, McCuller WJ, Reiber C, Tsai W, Plug M. HIV prevention among incarcerated male adolescents in an alternative school setting. J Correct Health Care. 2010;16(1):27–38. doi: 10.1177/1078345809348202. [DOI] [PubMed] [Google Scholar]
- Mumola CJ. Incarcerated Parents and Their Children. Washington, D.C: Bureau of Justice Statistics; 2000. [Google Scholar]
- Murrill CS, Liu KL, Guilin V, Colon ER, Dean L, Buckley LA, Torian LV. HIV prevalence and associated risk behaviors in New York City’s house ball community. Am J Public Health. 2008;98(6):1074–1080. doi: 10.2105/AJPH.2006.108936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mustanski BS, Garofalo R, Emerson EM. Mental health disorders, psychological distress, and suicidality in a diverse sample of lesbian, gay, bisexual, and transgender youths. Am J Public Health. 2010;100(12):2426–2432. doi: 10.2105/AJPH.2009.178319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Newman PA, Rhodes F, Weiss RE. Correlates of sex trading among drug-using men who have sex with men. Am J Public Health. 2004;94(11):1998–2003. doi: 10.2105/ajph.94.11.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Papachristos AV. Murder by structure: dominance relations and the social structure of gang homicide. AJS. 2009;115(1):74–128. doi: 10.1086/597791. [DOI] [PubMed] [Google Scholar]
- Papachristos AV, Hureau DM, Braga AA. The Corner and the Crew: The Influence of Geography and Social Networks on Gang Violence. American Sociological Review. 2013;78(3):417–447. doi: 10.1177/0003122413486800. [DOI] [Google Scholar]
- Papachristos AV, Wildeman C, Roberto E. Tragic, but not random: the social contagion of nonfatal gunshot injuries. Soc Sci Med. 2015;125:139–150. doi: 10.1016/j.socscimed.2014.01.056. [DOI] [PubMed] [Google Scholar]
- Peek ME, Lopez FY, Williams HS, Xu LJ, McNulty MC, Acree ME, Schneider JA. Development of a Conceptual Framework for Understanding Shared Decision making Among African-American LGBT Patients and their Clinicians. J Gen Intern Med. 2016;31(6):677–687. doi: 10.1007/s11606-016-3616-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pew. One in 31: The long reach of American corrections. Washington, DC: The Pew Charitable Trusts; 2009. [Google Scholar]
- PewCenter. One in 100: Behind bars in America, 2008. Washington DC: The Pew Center on the States: Public Safety Performance Project; 2008. [Google Scholar]
- Phillips G, 2nd, Peterson J, Binson D, Hidalgo J, Magnus M, Group, Y. o. c. S. I. S House/ball culture and adolescent African-American transgender persons and men who have sex with men: a synthesis of the literature. AIDS Care. 2011;23(4):515–520. doi: 10.1080/09540121.2010.516334. [DOI] [PubMed] [Google Scholar]
- Purdie-Vaughns V, Eibach RP. Intersectional invisibility: The distinctive advantages and disadvantages of multiple subordinate-group identities. Sex Roles. 2008;59(5–6):377–391. doi: 10.1007/s11199-008-9424-4. [DOI] [Google Scholar]
- Rietmeijer CA, Wolitski RJ, Fishbein M, Corby NH, Cohn DL. Sex hustling, injection drug use, and non-gay identification by men who have sex with men. Associations with high-risk sexual behaviors and condom use. Sex Transm Dis. 1998;25(7):353–360. doi: 10.1097/00007435-199808000-00006. [DOI] [PubMed] [Google Scholar]
- Robertson JE. Rape among incarcerated men: sex, coercion and STDs. AIDS Patient Care STDS. 2003;17(8):423–430. doi: 10.1089/108729103322277448. [DOI] [PubMed] [Google Scholar]
- Saum CAS,HL, Inciardi JA, Bennett RE. Sex in prison: Exploring the myths and realities. The Prison Journal. 1995;75:413–430. [Google Scholar]
- Schafer MH. On the locality of asymmetric close relations: spatial proximity and health differences in a senior community. J Gerontol B Psychol Sci Soc Sci. 2015;70(1):100–110. doi: 10.1093/geronb/gbu043. [DOI] [PubMed] [Google Scholar]
- Schneider J, Michaels S, Bouris A. Family network proportion and HIV risk among black men who have sex with men. J Acquir Immune Defic Syndr. 2012;61(5):627–635. doi: 10.1097/QAI.0b013e318270d3cb. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schneider JA, Cornwell B, Ostrow D, Michaels S, Schumm P, Laumann EO, Friedman S. Network mixing and network influences most linked to HIV infection and risk behavior in the HIV epidemic among black men who have sex with men. Am J Public Health. 2013;103(1):e28–36. doi: 10.2105/AJPH.2012.301003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schneider JA, Cornwell B, Jonas A, et al. Network dynamics of HIV risk and prevention in a population-based cohort of young Black men who have sex with men. Network Science. 2017:1–29. doi: 10.1017/nws.2016.27. [DOI] [Google Scholar]
- Seal DW. HIV-related issues and concerns for imprisoned persons throughout the world. Current Opinion in Psychiatry. 2005;18(5):530–535. doi: 10.1097/01.yco.0000179492.08064.de. [DOI] [PubMed] [Google Scholar]
- Seal DW, Eldrige GD, Kacanek D, Binson D, MacGowan RJ, Grp PSS. A longitudinal, qualitative analysis of the context of substance use and sexual behavior among 18-to 29-year-old men after their release from prison. Social Science & Medicine. 2007;65(11):2394–2406. doi: 10.1016/j.socscimed.2007.06.014. [DOI] [PubMed] [Google Scholar]
- Shah NS, Iveniuk J, Muth SQ, Michaels S, Jose JA, Laumann EO, Schneider JA. Structural bridging network position is associated with HIV status in a younger Black men who have sex with men epidemic. AIDS Behav. 2014;18(2):335–345. doi: 10.1007/s10461-013-0677-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Skeem J, Eno Louden J, Manchak S, Vidal S, Haddad E. Social networks and social control of probationers with co-occurring mental and substance abuse problems. Law Hum Behav. 2009;33(2):122–135. doi: 10.1007/s10979-008-9140-1. [DOI] [PubMed] [Google Scholar]
- Skrondal A,R-HS. Generalized Latent Variable Modeling. New York: Chapman & Hall/CRC; 2004. [Google Scholar]
- Stall R,FM, Catania JA. Interacting epidemics and gay men’s health: A theory of syndemic production among urban gay men. In: W R, Stall R, Valiserri RO, editors. Unequal opportunity: Health disparities affecting gay and bisexual men in the United States. New York: Oxford University Press; 2008. [Google Scholar]
- Stall R, Mills TC, Williamson J, Hart T, Greenwood G, Paul J, Catania JA. Association of co-occurring psychosocial health problems and increased vulnerability to HIV/AIDS among urban men who have sex with men. Am J Public Health. 2003;93(6):939–942. doi: 10.2105/ajph.93.6.939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stall R, Paul JP, Greenwood G, Pollack LM, Bein E, Crosby GM, Catania JA. Alcohol use, drug use and alcohol-related problems among men who have sex with men: the Urban Men’s Health Study. Addiction. 2001;96(11):1589–1601. doi: 10.1080/09652140120080723. [DOI] [PubMed] [Google Scholar]
- StataCorp. Statistical Software. College Station, TX: StataCorp LP; 2015. Stata: Release 14. [Google Scholar]
- Stein MB, Walker JR, Hazen AL, Forde DR. Full and partial posttraumatic stress disorder: Findings from a community survey. American Journal of Psychiatry. 1997;154(8):1114–1119. doi: 10.1176/ajp.154.8.1114. [DOI] [PubMed] [Google Scholar]
- Stroebe MS,H, Stroebe W. Health outcomes of bereavement. Lancet. 2007;370:1960–1973. doi: 10.1016/S0140-6736(07)61816-9. [DOI] [PubMed] [Google Scholar]
- The Pew Charitable Trusts. Collateral Costs: Incarceration’s Effect on Economic Mobility. Washington, D.C.: The Pew Charitable Trusts; 2010. [Google Scholar]
- Tracy M, Braga AA, Papachristos AV. The Transmission of Gun and Other Weapon-Involved Violence Within Social Networks. Epidemiol Rev. 2016;38(1):70–86. doi: 10.1093/epirev/mxv009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- U.S. Census Bureau. American Community Survey 5-Year Estimates. 2005–2009 Retrieved January 3, 2013. [Google Scholar]
- Uggen C. Work as a turning point in the life course of criminals: A duration model of age, employment, and recidivism. American Sociological Review. 2000;65(4):529–546. doi: 10.2307/2657381. [DOI] [Google Scholar]
- Valleroy LA, MacKellar DA, Karon JM, Rosen DH, McFarland W, Shehan DA, Janssen RS. HIV prevalence and associated risks in young men who have sex with men. Young Men’s Survey Study Group. JAMA. 2000;284(2):198–204. doi: 10.1001/jama.284.2.198. doi: joc92135 [pii] [DOI] [PubMed] [Google Scholar]
- Voisin DR, Hotton AL, Neilands TB. Testing pathways linking exposure to community violence and sexual behaviors among African American youth. J Youth Adolesc. 2014;43(9):1513–1526. doi: 10.1007/s10964-013-0068-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Voisin DR, Jenkins EJ, Takahashi L. Toward a conceptual model linking community violence exposure to HIV-related risk behaviors among adolescents: directions for research. J Adolesc Health. 2011;49(3):230–236. doi: 10.1016/j.jadohealth.2011.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Voisin DR, Salazar LF, Crosby R, Diclemente RJ, Yarber WL, Staples-Horne M. Witnessing community violence and health-risk behaviors among detained adolescents. Am J Orthopsychiatry. 2007;77(4):506–513. doi: 10.1037/0002-9432.77.4.506. [DOI] [PubMed] [Google Scholar]
- Volker B DCR, Mollenhorst G, Dirzwager A, van der Laan P, Nieuwbeerta P. Changes in the social networks of prisoners: A comparison of their networks before and after imprisonment. Social Networks. 2016;47:47–58. [Google Scholar]
- Westergaard RP, Spaulding AC, Flanigan TP. HIV among persons incarcerated in the US: a review of evolving concepts in testing, treatment and linkage to community care. Current opinion in infectious diseases. 2013;26(1):10. doi: 10.1097/QCO.0b013e32835c1dd0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Western BM,S. Fathers behind bars: the impact of incarceration on family formation. In: B M, Fox GL, editors. Families, Crime and Criminal Justice: Contemporary Persepctives in Family Research. New York: Elsevier Science; 2000. pp. 309–324. [Google Scholar]
- Wilson PA, Nanin J, Amesty S, Wallace S, Cherenack EM, Fullilove R. Using syndemic theory to understand vulnerability to HIV infection among Black and Latino men in New York City. J Urban Health. 2014;91(5):983–998. doi: 10.1007/s11524-014-9895-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wohl AR, Johnson D, Jordan W, Lu S, Beall G, Currier J, Kerndt PR. High-risk behaviors during incarceration in African-American men treated for HIV at three Los Angeles public medical centers. J Acquir Immune Defic Syndr. 2000;24(4):386–392. doi: 10.1097/00126334-200008010-00014. [DOI] [PubMed] [Google Scholar]
- Wrzus C, Hanel M, Wagner J, Neyer FJ. Social Network Changes and Life Events Across the Life Span: A Meta-Analysis. Psychological Bulletin. 2013;139(1):53–80. doi: 10.1037/a0028601. [DOI] [PubMed] [Google Scholar]
- Young JTN. How Do They ‘End Up Together’? A Social Network Analysis of Self-Control, Homophily, and Adolescent Relationships. Journal of Quantitative Criminology. 2011;27(3):251–273. doi: 10.1007/s10940-010-9105-7. [DOI] [Google Scholar]


