Abstract
C-reactive protein (CRP) has been indicated to be associated with the pathogenesis of schizophrenia (SZ) and other psychiatric disorders. The aim of this study is to investigate whether peripheral blood CRP levels are associated with the risk of SZ. We searched literature from databases of Pubmed, Embase and the Cochrane Library from inception to November 1, 2016 for studies that reported serum or plasma CRP levels in patients with SZ and non-SZ controls. At least two reviewers decided on eligibility and extracted data from included studies. Random effects meta-analyses were performed using standardized mean difference (SMD) as the effect estimate of the differences in CRP levels between subjects with SZ and healthy controls. We identified 18 studies representing 1963 patients with SZ and 3683 non-SZ controls. Compared with non-schizophrenics, blood CRP levels were moderately increased in people with SZ (SMD 0.53, 95% CI 0.30 to 0.76) irrespective of study region, sample size of included studies, patient mean age, age of SZ onset and patient body mass index. Publication bias was not detected through Egger's linear regression test (P = 0.292). We noticed that patients in Asia or Africa (n = 6, SMD 0.73, 95% CI 0.26 to 1.21) and whose age less than 30 years (n = 5, SMD 0.76, 95% CI 0.07 to 1.58) had substantially higher CRP levels. Our study provides evidence that higher CRP levels are associated with increased risk of SZ, especially for young adult patients less than 30 years. Further large-scale studies are strongly warranted to further confirm this association.
Keywords: C-reactive protein, schizophrenia, risk, meta-analysis
INTRODUCTION
Immune system dysfunctions and inflammatory processes have been implicated in the pathogenesis of schizophrenia (SZ) [1–5]. A vast observational studies, mainly case-control studies provide increasing evidence that patients with SZ have elevated levels of some inflammatory biomarkers, such as cytokines in plasma or serum [1, 4]. Furthermore, evidence from epidemiologic studies implied that some autoimmune diseases contributed to the development of SZ [6, 7]. As an acute-phase protein, C-reactive protein (CRP) is produced by some inflammatory stimula and is mainly induced by some pro-inflammatory cytokines [8]. Increased CRP levels have been reported in numerous observational studies in psychosis including SZ and in bipolar disorder [9]. Metcalf et al. reported that individuals with high (> 3 mg/L) compared with low (< 1 mg/L) CRP levels at baseline were more likely to develop SZ (adjusted odd ratio 4.25, 95% CI, 1.30 to 13.93) [55]. Zhang et al. found that high sensitivity CRP/ interleukin-10 was a potential peripheral biomarker of SZ [56].
It has also been indicated that the increase in serum or plasma CRP levels contributes the risk of a first episode of SZ [9]. Inoshita et al. conducted a mendelian randomisation study and found a causal relationship between increased CRP levels and the development of SZ [10]. However, several other studies reported no association between CRP levels and risk of SZ [11–13]. A meta-analysis by Fernandes et al published in 2015 of CRP levels in patients with SZ found that CRP was increased in SZ but was not altered by antipsychotics [14]. However, owing to the mixed studies combined for both case-control and cross-sectional studies in meta-analysis, we would like to update the evidence for only case-control studies published in English peer review journals.
RESULTS
Description of the included studies
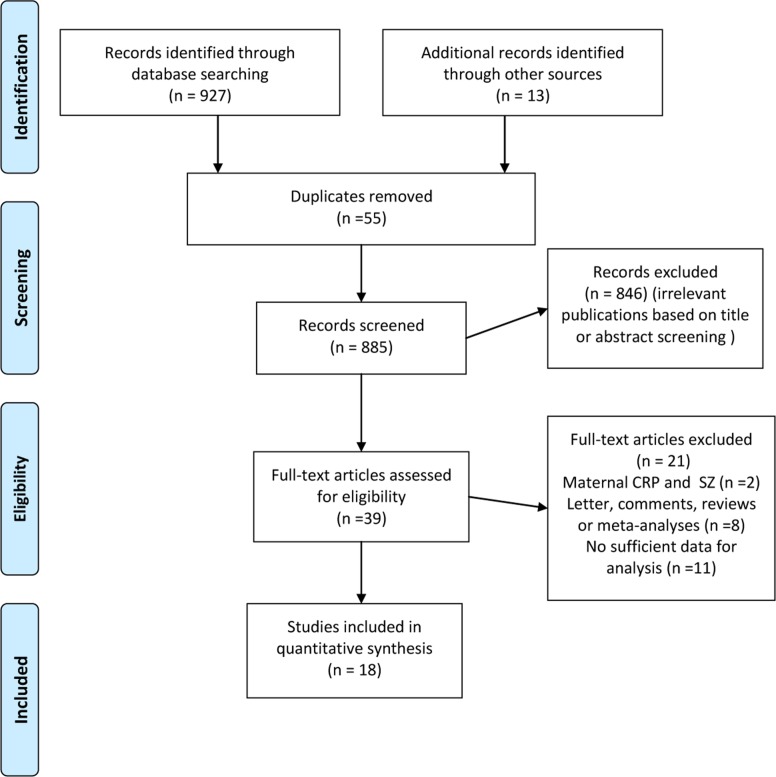
The literature search yielded 927 citations. After excluding the duplicate, 39 appeared relevant and were retrieved for full-text review afer reading the titles or abstracts (Figure 1). In summary, 18 studies recruiting 1963 patients with SZ and 3683 non-SZ controls were enrolled in this meta-analysis [10–13, 15–28]. Detailed characteristics of individual studies are presented in Table 1. The sample size of included studies ranged from 60 to 1783 participants. Eleven studies were conducted in European countries, six in Asian or African countries and one in USA. Three studies recruted participants from inpatient unit, while another three from outpatient unit, eight from both units and four from population-based samples. Seven studies enrolled patients with age of SZ onset less than 30 years and two more than 30 years. Five studies investigated participants with body mass index less than 25kg/m2 and 11 studies with the range from 25 to 30 kg/m2. Most of the studies (17/18) applied high-sensitivity CRP assay except for one [13]. Twelve of the 18 included studies were of high quality and the remaining six studies were assessed as medium quality.
Figure 1. Preferred reporting items for systematic reviews and meta-analyses flow diagram depicting overview of study-selection process for studies reporting on C-reactive protein and risk of schizophrenia.
Table 1. Characteristics of the included studies in the meta-analysis investigating the association between C-reactive protein and risk of schizophrenia.
| Study | Year | Country | Subjects | Sex Male/Female | Setting | Meanage (years) | Meanage of onset (years) | Mean BMI | Adjusted variables for controls | Current Smokers (%) | CRP assay type | Comorbidities | Psychiatric drugs |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Sarandol et al., | 2007 | Turkey | Chronic SZ Control | 18/22 17/18 | Inpatient and outpatient unit | 34.9 33.5 | NA | 23.7 24.6 | Age, BMI, smoking status | NA | Plasma, high sensitive immunonephrelometry assay | Exclusions: DM and use of anti-inflammatory or, HAS, CVD, infections immunossupressants | Drug-naïve or free |
| Carrizo et al. | 2008 | Venezuela | Chronic SZ Control | 48/40 | Inpatient and outpatient unit | 43.2 54.79 | NA | 27.5 28.6 | No | NA | Serum, high sensitive enzime immunoassay | Exclusions: DM , HAS, CVD, infections and use of anti-inflammatory or immunossupressants | Typical and Atypical antipsychotics |
| Akanji et al., 2009 | 2009 | Kuwait | Chronic SZ Control |
141/62 | Inpatient unit | 141/62 165/0 |
NA | 39.80 39.50 | Age, race, socioeconomic status | NA | Serum, high sensitive Chemiliminescent immunometric assay |
Exclusions: DM, HAS, CVD, infections and use of anti-inflammatory or immunossupressants |
Typical antipsychotics |
| Fernandes-Egea et al., 2009 | 2009 | Spain | SZ in FEP Control | 35/15 35/15 | Populational | 29.4 28.8 | 29 | 22.9 23.9 | Age, gender, BMI,number of cigarettes/day, catchment area | NA | Serum, not high sensitive immuno assay | DM (n = 9). Exclusions: other relevant clinical pathologies | |
| Fawzi et al., 2011 | 2011 | Egypt | Chronic SZ Control | 92/0 200/0 | Outpatient unit | 28.4 28.8 | NA | 27 26.4 | Age, gender, BMI, lifestile | 147 132 | Plasma, high sensitive latex assay | Exclusions: DM , HAS, CVD, infectionsand use of anti-inflammatory orimmunos- supressants |
Drug-naïve or free Drug-naïve |
| Hope et al., 2011 | 2011 | Norway | Chronic SZ Control | 89/64 105/134 | Populational | 36.2 36 | 26 24.4 | Age, BMI, catchment area | 86 NA | Plasma, high sensitive enzime immunoassay | DM (n = 4) and CVD (n = 11). Exclusions:other relevant clinical pathologies | Typical and Atypical antipsychotics | |
| Suvisaari et al., 2011 | 2011 | Finland | Chronic SZ Control | 39/63 39/63 | Populational | 55.7 55.78 | NA | 28.6 26.4 | Age, gender, BMI | 37 27 | Plasma, high sensitive immunotur- bidometric test |
DM (n = 11). Exclusions: other relevant clinical pathologies, infections | Typical and Atypical antipsychotics |
| Hepgul et al. 2012 | 2012 | England | SZ in FEP Control | NA | Inpatient and outpatient unit | 33.5 33.1 | NA | 25.6 25.1 | No | NA | Serum, high sensitive enzime immunoassay | Exclusions: DM , HAS, CVD, infectionsand use of anti-inflammatory or immunossupressants | Drug-free |
| Dickerson et al.,2013 | 2013 | United States | Chronic SZ Control | 177/118 84/144 | Inpatient and outpatient unit | 39 32.2 | 20.3 | 30.3 27.8 | No | 183 36 | Serum, high sensitive enzime immunoassay | DM (n = 17). Exclusions: other relevant clinical pathologies | Typical and Atypical antipsychotics |
| Joshi et al., 2013 | 2013 | India | Chronic SZ Control | 29/16 21/20 | Inpatient and outpatient unit | 38.5 35.8 | 23.90 | 27.3 26.5 | Age, BMI, catchment | NA | Plasma, high sensitive enzime immunoassay | Exclusions: DM , HAS, CVD, infectionsand use of anti-inflammatory or immunossupressants | Typical antipsychotics |
| Kuo et al., 2013 | 2013 | Taiwan | Chronic SZ Control | 19/14 12/18 | Outpatient unit | 37.8 38.8 | 33.90 | 29.5 28.3 | Age, BMI | NA | Plasma, high sensitive latex assay | Exclusions: DM , HAS, CVD, infections and use of anti-inflammatory or immunossupressants | Typical and Atypical antipsychotics |
| Lin et al., 2013 | 2013 | Taiwan | Chronic SZ Control | 16/20 16/20 | Inpatient and outpatient unit | 35.7 37.3 | 23.79 | 24.6 22.9 | Age, gender, BMI, | NA | Serum, high sensitive immunonephrelometry assay | Exclusions: DM , HAS, CVD, infectionsand use of anti-inflammatory or immunossupressants | Atypical antipsychotics |
| Vuksan-Cusa et al., 2013 | 2013 | Croatia | Chronic SZ Control | NA | Inpatient unit | 26.9 24.9 | 15.7 | 26.9 24.9 | Age, gender, BMI, | NA | Plasma, high sensitive immunoturbidometric test | Exclusions: DM , HAS, CVD, infectionsand use of anti-inflammatory or immunossupressants | Atypical antipsychotics |
| Berardis et al., 2014 | 2014 | Italy | SZ in FEP Control | 13/17 13/17 | Inpatient unit | 25.9 25.5 | 24.90 | 22.1 23.5 | Age, gender | NA | Plasma, high sensitive immunonephrelometry assay | Exclusions: DM , HAS, CVD, infections and use of anti-inflammatory or immunossupressants | Drug-naïve |
| Frydecka et al., 2014 | 2014 | Poland | Chronic SZ Control | 69/82 103/91 | Inpatient and outpatient unit | 37.8 39.2 | 25.20 | 27.11 26.9 | Age, gender, BMI | NA | Serum, high sensitive enzime immunoassay | Exclusions: DM, HAS, CVD, infections and use of anti-inflammatory or immunossupressants | NA |
| Klemettila et al., 2014 | 2014 | Finland | Chronic SZ Control | 105/85 403/500 | Inpatient and outpatient unit | 42.9 46 | NA | 29.92 26.5 | No | 101 NA | Plasma, high sensitive enzime immunoassay | Exclusions: DM, HAS, CVD, infectionsand use of anti-inflammatory or immunossupressants | Clozapine |
| Stojanovic et al., 2014 | 2014 | Spain | SZ in FEP Control | 48/29 12/13 | Outpatient unit | 24.3 27.3 | NA | 24.4 21.6 | No | 53 | Plasma, high sensitive immunoturbidometric test | NA | Typical and Atypical antipsychotics |
| Inoshita et al., 2016 | 2016 | Japan | Chronic SZ Control | 241/177 422/943 | Populational | 62.5 62.6 | NA | NA | Age, gender | NA | Serum, high sensitive enzime immunoassay | Exclusions: CRP concentration either below 0.02 mg/dl or above 10 mg/dl | Typical and Atypical antipsychotics |
Abbreviations: BMI, body-mass index; CRP, C-reactive protein; CVD, cardiovascular diseases; DM, Diabetes Mellitus; HAS, hypertension; HDRS, Hamilton Depression Rating Scale; NA, not available; YMRS, Young Mania rating Scale.
Meta-analysis of Association between CRP and Risk of Schizophrenia
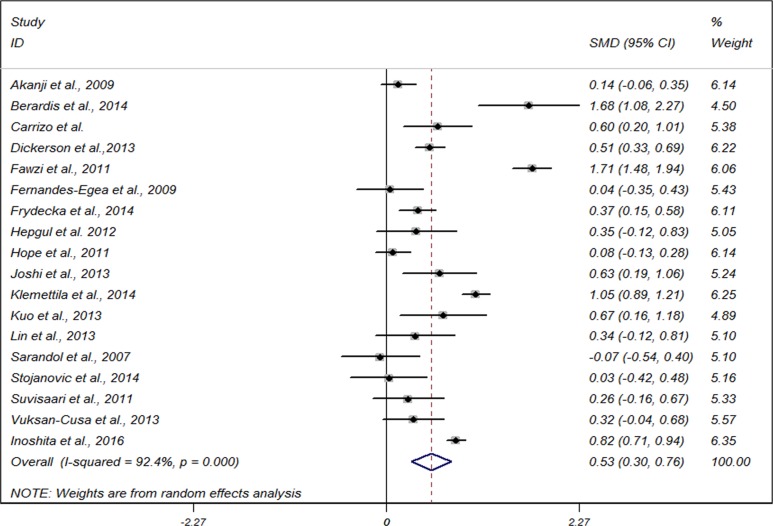
Meta-analysis based on 18 studies, showed that compared with non-schizophrenics, CRP levels were moderately increased in people with SZ (standardized mean difference (SMD) 0.53, 95% CI 0.30 to 0.76), with significant heterogeneity among studies (I2 = 92.5%, P < 0.001) (Figure 2). We then conducted subgroup analyses stratified by study region, sample size, clinical setting, mean age, age of SZ onset, body mass index, adjusted controls and high-sensitivity CRP assay used or not. The findings did not largely alter compared with that of the main analysis for most of the subgroups (Table 2). A bordine estimates were seen for studies for clinical setting of inpatient unit (SMD 0.66, 95% CI–0.05 to 1.38) and outpatient unit (SMD 0.82, 95% CI–0.05 to 1.38).
Figure 2. Forest plot for meta-analysis of the association between C-reactive protein and risk of schizophrenia with the use of a random-effects model.
SMD, standardized mean difference; CI, confidence interval.
Table 2. Main results of subgroup analyses to explore sources of heterogeneity based on some investigated variables for association between C-reactive protein levels and risk of schizophrenia.
| Variables | Heterogeneity (I2 %; Phet) |
SMD 95% CI | Pinteraction |
|---|---|---|---|
| Total | 18 (92.5; < 0.001) | 0.53 (0.30 to 0.76) | NA |
| Study region | < 0.001 | ||
| USA | 1 (–, –) | 0.51 (0.33 to 0.69) | |
| Europe | 11 (89.6, < 0.001) | 0.42 (0.12 to 0.72) | |
| Asia/Africa | 6 (95.3, < 0.001) | 0.73 (0.26 to 1.21) | |
| Sample size | 0.075 | ||
| ≥ 100 | 10 (95.5, < 0.001) | 0.52 (0.21 to 0.83) | |
| < 100 | 6 (77.7, < 0.001) | 0.63 (0.22 to 1.03) | |
| Clinical setting | < 0.001 | ||
| Inpatient unit | 3 (91.6%, < 0.001) | 0.66 (–0.05 to 1.38) | |
| Outpatient unit | 3 (92.5%, < 0.001) | 0.82 (–0.28 to 1.93) | |
| Both units | 8 (84.3, < 0.001) | 0.50 (0.24 to 0.76) | |
| Population-based | 4 (95.9, < 0.001) | 0.31 (0.17 to 0.80) | |
| Mean age | < 0.001 | ||
| < 30 years | 5 (95.9, < 0.001) | 0.76 (0.07 to 1.58) | |
| 30-50 years | 11 (87.7, < 0.001) | 0.43 (0.19 to 0.67) | |
| ≥ 50 years | 2 (84,6, < 0.001) | 0.58 (0.03 to 1.12) | |
| Age of onset | < 0.001 | ||
| ≤ 30 years | 7 (74.6, 0.001) | 0.50 (0.25 to 0.75) | |
| > 30 years | 2 (0, 0.591) | 0.81 (0.70 to 0.93) | |
| Body mass index | < 0.001 | ||
| ≤ 25 kg/m2 | 5 (85.1, < 0.001) | 0.38 (0.16 to 0.92) | |
| 25–30 kg/m2 | 11 (93.5, < 0.001) | 0.60 (0.29 to 0.92) | |
| Adjusted controls | 0.077 | ||
| Yes | 13 (93.7, < 0.001) | 0.53 (0.23 to 0.84) | |
| No | 5 (87.8, < 0.001) | 0.54 (0.19 to 0.90) | |
| High-sensitivity CRP assay | 0.003 | ||
| Yes | 17 (92.6, < 0.001) | 0.56 (0.33 to 0.80) | |
| No | 1 (–, –) | 0.04 (–0.35 to 0.43) |
Abbreviations: CI, confidence interval; CRP, C-reactive protein; het, heterogeneity; NA, not available; SMD, standardized mean difference.
Study region
Subgroup analysis stratified by study region showed that serum and plasma CRP levels were increased moderately in studies conducted in European countries (n =11, pooled SMD 0.42, 95% CI 0.12 to 0.72) and significantly in Asian/African countries (n = 6, pooled SMD 0.73, 95% CI 0.26 to 1.21). We found statistically significant difference for inter-study heterogeneity (P < 0.001).
Clinical setting
Meta-analysis stratified by clinical setting demonstated that serum and plasma CRP levels were increased moderately in studies performed in combination with inpatient and outpatient unit (n = 8, pooled SMD 0.50, 95% CI 0.24 to 0.76) and slightly in population-based samples (n = 4, pooled SMD 0.31, 95% CI 0.17 to 0.80). We found statistically significant difference for inter-study heterogeneity (P < 0.001).
Sample size
Subgroup analysis stratified by sample size indicated that serum and plasma CRP levels were increased moderately in studies with large sample size (≥ 100) (n = 10, pooled SMD 0.52, 95% CI 0.21 to 0.83); similar results were also obtained for studies with small sample size (< 100) (n = 6, pooled SMD 0.63, 95% CI (0.22 to 1.03).We found no statistically significant difference for inter-study heterogeneity (P = 0.075).
Age
Subgroup analysis stratified by age indicated that serum and plasma CRP levels were increased significantly in studies with participants’age <30 years (n = 5, pooled SMD 0.76, 95% CI 0.07 to 1.58); but moderately in studies with participants’age ranging from 30 to 50 years (n = 11, pooled SMD 0.43, 95% CI 0.19 to 0.67); similar results were also obtained for studies with participants’age ≥ 50 years (n = 2, pooled SMD 0.58, 95% CI 0.03 to 1.12). We found statistically significant difference for inter-study heterogeneity (P < 0.001).
Age of SZ onset
Subgroup analysis stratified by age of SZ onset showed that serum and plasma CRP levels were increased moderately in studies with participants’ age of SZ onset ≤ 30 years (n = 7, pooled SMD 0.50, 95% CI 0.25 to 0.75); but significantly in studies with participants’age ranging from 30 to 50 years (n = 11, pooled SMD 0.43, 95% CI 0.19 to 0.67); similar results were also obtained for studies with participants’ age of SZ onset > 30 years (n = 2, pooled SMD 0.81, 95% CI 0.70 to 0.93). We found statistically significant difference for inter-study heterogeneity (P < 0.001).
Adjusted variables for controls
Subgroup analysis stratified by adjusted variables for controls showed that serum and plasma CRP levels were increased moderately in studies with (n = 13, pooled SMD 0.53, 95% CI 0.23 to 0.84) and without adjusted variables for controls (n = 5, pooled SMD 0.54, 95% CI 0.19 to 0.90). We found no statistically significant difference for inter-study heterogeneity (P < 0.077).
Sensitivity analysis and publication bias
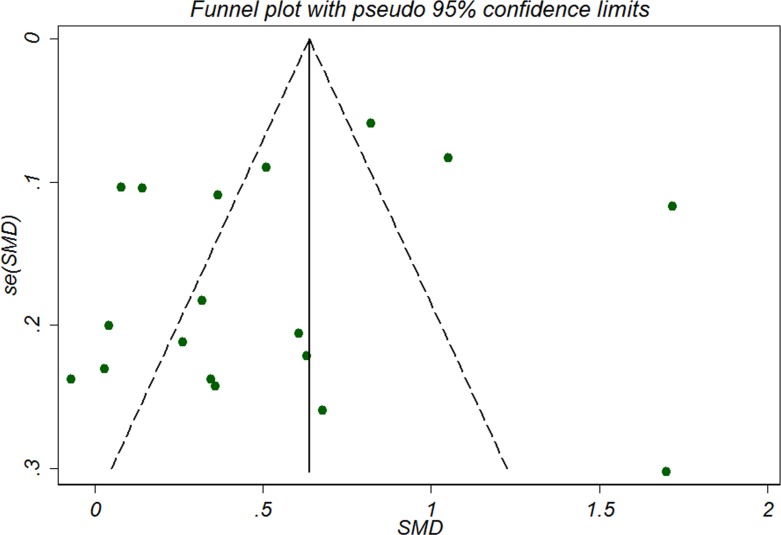
Sensitivity analysis showed that serum and plasma CRP levels were increased moderately in studies involved only high-sensitivity CRP assay (n = 17, pooled SMD 0.56, 95% CI 0.33 to 0.80). No significant funnel plot asymmetry was detected as was shown in Figure 3, indicating no publication bias, which was further confirmed by Begg’s rank correlation test (P = 0.544) and Egger’s regression test (P = 0.292). Duval and Tweedie’s trim and fill method indicated that no missing study was inputed and the adjusted SMD was the same as the primary one, confirming the robustness of the analysis.
Figure 3. Funnel plot of publication bias in the selection of studies for assessing the relationship between C-reactive protein and risk of schizophrenia.
SMD, standardized mean difference.
DISCUSSION
In this meta-analysis based on 18 case-control studies, we found that serum and plasma CRP levels were moderately increased in patients with SZ, irrespective of study region, sample size of included studies, patient mean age, age of SZ onset and patient body mass index. We noticed that patients in Asia or Africa and whose age less than 30 years were more substantially increase in CRP levels.
The potential biological mechanism for the associations between some inflammatary factors and SZ has not been fully understood. Hsuchou et al. found that high peripheral levels of CRP could increase the permeability of the blood–brain barrier through the adjustment of the function of tight junctions, which contributed to the increase in some pro-inflammatory cytokines, such as CRP to enter the central nervous system [29].
The high levels of CRP in central nervous system has been reported to play an important part in some psychiatric dysfunctions, such as SZ [30, 31]. Experimental study showed that CRP affected viability of microglia and astrocytes, accelerating cell gliosis [32], thus leading to the release of some pro-inflammatroy factors, such as IL-6 and transforming growth factor-β. In addition, reports also showed that elevated CRP levels could influence the microcirculatory system in the blood–brain barrier, thus affecting neurotransmitter synthesis and neurotransmission [33–38]. Moreover, elevated CRP levels were reported to be associated with the severity of clinical symptoms, cognitive and sensory impairments in SZ [39–42]. The rationale that plasma CRP levels were increased significantly in studies with participants’age less than 30 years probably lies in that in the early stages of SZ, a particularly large number of inflammatory substances will be secreted, such as blood CRP and interleukin-10, which are very likely to be related to the development of SZ [57].
Strength of the study
This updated literature search identified two systematic review and meta-analyses on the same topic [14, 43], but both of them focused on studies with mixed study design. Though solely one newly published study has been added to this analysis [10], this is a quite large sample size case-control study (418 cases/1365 controls) with greater statistical power. The findings of our studies are consistent with those two meta-analyses from mixed cross-sectional studies and case–control studies (60). Miller et al. [43] found that CRP levels were slightly to moderately increased in people with SZ (SMD 0.45, 95% CI 0.34 to 0.55) by pooling 8 cross-sectional studies, and Fernandes et al. [14] concluded that CRP levels were moderately to significantly increased in persons with SZ (SMD 0.66, 95% CI 0.43 to 0.88). Strength of our meta-analysis lies in the following three aspects. Firstly, most of the included studies in the previous meta-analyses were cross-sectional in study design. An known limitation of a cross-sectional study is that exposure and outcome are generally evaluated simutaneously and we therefore cannot draw conclusions on the casual-relationship between exposure and outcome. Hence, the underlying hypothesis obtained from the previous meta-analyses is that the prevalance of SZ is an immediate outcome following exposure of elevated CRP levels. The investigation of the real effects caused by continuous long-term exposure may require a different study design, such as our case-control study or cohort study [44]. Secondly, heterogeneity was noted among the included studies but we tried to account for this variation by conducting sensitivity analysis. The asymmetry of funnel plot indicated the overestimation of the effect size due to the lack of negative studies with small sample size. However, Begg’s rank correlation test and Egger’s regression test suggested little evidence of publication bias. Moreover, when applying the trim and fill method, no additional hypothised negative studies with small sample size were inputed, suggesting the robustness of the meta-analysis. Thirdly, it is the first study to suggest that younger patients with SZ whose age less than 30 years were more substantially increase in CRP levels. Though this potential reason is unclear, it has been suggested to be related with a greater reactivity of the immune system in younger patients [45]. However, further large well designed studies are warrented to validate this association.
Some inherent limitations do exist in our study. We report an increase in serum and plasma CRP levels in patients with SZ by pooling the eligible studies over the last decade. In our meta-analysis, we found the pooled SMD was 0.53 (95% CI 0.30 to 0.76) for the association between serum and plasma CRP levels and risk of SZ from the 18 studies included. The study quality of evidence obtained from NOS score was moderate and derived from case-control studies. However, still some other confounders remained due to factors that could not be accounted for such as physical activity, waist circumference, smoking habit, vitamin D intake, and subclinical infections. Most studies included in our analysis did not provide such data, which could explain the heterogeneity noted in the pooled analysis. Although subgroup analyses have been performed for some of the existing confounders, the investigated factors could only explain some of the heterogeneity. Moreover, many of the other analyses, such as dose-response relationship could not be conducted due to the lack of detailed information from original reports. Furthermore, the possible sources of heterogeneity was explored through subgroup analyses and sensitivity analyses. However, the results of these two methods did not allow us to attribute heterogeneity to any single study as the sole source of the high heterogeneity we obtained in most analyses. Secondly, this updated meta-analysis on serum and plasma CRP levels in patients with SZ compared with non-SZ controls provided us with summary estimates originating from one type of observational study (case-control study). Therefore, no definite causal conclusion can be drawn from this meta-analysis. High serum and plasma CRP level is only one of the inflammation-related factors known to be associated with the risk of SZ. Other factors such as smoking habit and subclinical infections could also be additional related factors. Thirdly, like any meta-analysis, this one is also dependent on the quality of the included studies, and our findings need to be further confirmed by studies specifically designed to demonstrate the unclear points we raised. Finally, the restriction of our meta-analysis to English language studies may have led to language bias with potentially relevant studies published in other languages being missed.
In summary, our meta-analyses provide evidence that higher CRP levels are associated with increased risk of SZ, especially for young adult patients less than 30 years. Future studies should be focused on whether changes in CRP levels have a causal relationship with the development of SZ.
MATERIALS AND METHODS
Literature search and study selection
The Preferred reporting items for systematic reviews and meta-analyses (PRISMA) statement was used when we performed this systematic literature review [46]. We systematically searched databases of Pubmed, EMBASE and the Cochrane Library from inception till November 1, 2016 for relevant studies, using the predefined search strategies (Supplementary search strategy 1–3). The following MeSH terms combined with free text words were used:schizophrenia /schizophreni* /schizoid /psychosis /schizophreniform/schizoaffective/psychotic disorders and C-reactive protein /CRP /hsCRP /hs-CRP. Additional related journal articles were identified by manual scanning of reference lists of articles, and the journals selected were JAMA Psychiatry, American Journal of Psychiatry, Molecular Psychiatry, British Journal of Psychiatry and European Psychiatry. We only included studies in English peer-review journals.
Studies were considered eligible in the meta-analysis according to the following criteria: 1) adult patients diagnosed with SZ based on Diagnostic and Statistical Manual for Mental Disorder-Fourth Edition-Text Revised (DSM–IV–TR) were enrolled in the study; 2) case-control studies with the non-SZ comparisons measuring serum or plasma CRP levels. We excluded studies with duplicate data or studies that reported CRP levels using dichotomous data (ie, positive or negative), or studies without a control group. In addition, we did not include unpublished literature due to the insufficient data obtained from these studies.
Data extraction and bias assessment
Two authors (Z.W. and P.L.) independently searched, identified the related studies, extracted data and evaluated the study quality. When discrepancies occured, a third author (G.C.) made the definitive decision for study eligibility and data extraction. We extracted the following data including first author, publication year , research country, study subjects, clinical setting, sex, age and BMI of the study subjects, age of SZ onset, adjusted variables for controls, percent of the current smokers, CRP assay type, comorbidities and psychiatric drugs used. If necessary, we consulted the original data from the authors of the studies to collect missing information. The Newcastle–Ottawa Scales (NOS) was used to assess quality of the included studies [47], which applied three domains for assessment and allocated a total score of nine points. Quality categories were determined by the NOS score of each study. We defined that the score of high quality with 7 or more, medium quality from 4 to 6 and low quality less than 4.
Statistical analysis
For continuous outcomes reported on different measurement methods for CRP levels, we applied standardised mean difference (SMD) estimates of the differences in CRP levels between patients with SZ and non-SZ controls as the effect size. The value of SMD being 0.2 was set to indicate a slight effect, meaning a small difference in CRP levels between patients with SZ and non-SZ controls, 0.5 a moderate effect, and 0.8 a significant effect [48]. The heterogeneity among the included studies was investigated using I2 and Q test statistics, with an I2 more than 50% or a P value less than 0.1 from Cochran’s Q-test indicating significant heterogeneity [49]. Summary estimates in the present meta-analysis were pooled using a random-effects model due to the predictable significant inter-study difference in the enrolled population, study design, or the treatment strategy [50]. We used funnel plots to visually inspect publication bias, along with Begg’s rank correlation test [51] and Egger’s regression test [52]. We also estimated the number of potential missing studies from a meta-analysis using the trim and fill method [53]. Some planned subgroup analyses were performed to explore possible causes of heterogeneity and between-subgroup interactions were calculated using the chi-squared significance test [54]. All meta-analyses were conducted using the software STATA version 12.0 (StataCorp LP, College Station, TX).
SUPPLEMENTARY MATERIALS TABLES
Footnotes
CONFLICTS OF INTEREST
None.
GRANT SUPPORT
This work was supported by the Natural Science Foundation of Heilongjiang, China (H201497).
REFERENCES
- 1.Potvin S, Stip E, Sepehry AA, Gendron A, Bah R, Kouassi E. Inflammatory cytokine alterations in schizophrenia: a systematic quantitative review. Biological psychiatry. 2008;63:801–808. doi: 10.1016/j.biopsych.2007.09.024. [DOI] [PubMed] [Google Scholar]
- 2.Brown AS, Derkits EJ. Prenatal infection and schizophrenia: a review of epidemiologic and translational studies. The American journal of psychiatry. 2010;167:261–280. doi: 10.1176/appi.ajp.2009.09030361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Brown AS. The environment and susceptibility to schizophrenia. Progress in neurobiology. 2011;93:23–58. doi: 10.1016/j.pneurobio.2010.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Miller BJ, Buckley P, Seabolt W, Mellor A, Kirkpatrick B. Meta-analysis of cytokine alterations in schizophrenia: clinical status and antipsychotic effects. Biological psychiatry. 2011;70:663–671. doi: 10.1016/j.biopsych.2011.04.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Richard MD, Brahm NC. Schizophrenia and the immune system: pathophysiology, prevention, and treatment. American journal of health-system pharmacy. 2012;69:757–766. doi: 10.2146/ajhp110271. [DOI] [PubMed] [Google Scholar]
- 6.Canetta S, Sourander A, Surcel HM, Hinkka-Yli-Salomaki S, Leiviska J, Kellendonk C, McKeague IW, Brown AS. Elevated maternal C-reactive protein and increased risk of schizophrenia in a national birth cohort. The American journal of psychiatry. 2014;171:960–968. doi: 10.1176/appi.ajp.2014.13121579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Canetta SE, Bao Y, Co MD, Ennis FA, Cruz J, Terajima M, Shen L, Kellendonk C, Schaefer CA, Brown AS. Serological documentation of maternal influenza exposure and bipolar disorder in adult offspring. The American journal of psychiatry. 2014;171:557–563. doi: 10.1176/appi.ajp.2013.13070943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Dantzer R, O’Connor JC, Freund GG, Johnson RW, Kelley KW. From inflammation to sickness and depression: when the immune system subjugates the brain. Nature reviews Neuroscience. 2008;9:46–56. doi: 10.1038/nrn2297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wium-Andersen MK, Orsted DD, Nordestgaard BG. Elevated C-reactive protein and late-onset bipolar disorder in 78 809 individuals from the general population. The British journal of psychiatry. 2016;208:138–145. doi: 10.1192/bjp.bp.114.150870. [DOI] [PubMed] [Google Scholar]
- 10.Inoshita M, Numata S, Tajima A, Kinoshita M, Umehara H, Nakataki M, Ikeda M, Maruyama S, Yamamori H, Kanazawa T, Shimodera S, Hashimoto R, Imoto I, et al. A significant causal association between C-reactive protein levels and schizophrenia. Scientific reports. 2016;6:26105. doi: 10.1038/srep26105. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 11.Sarandol A, Kirli S, Akkaya C, Ocak N, Eroz E, Sarandol E. Coronary artery disease risk factors in patients with schizophrenia: effects of short term antipsychotic treatment. Journal of psychopharmacology (Oxford, England) 2007;21:857–863. doi: 10.1177/0269881107077609. [DOI] [PubMed] [Google Scholar]
- 12.Hope S, Dieset I, Agartz I, Steen NE, Ueland T, Melle I, Aukrust P, Andreassen OA. Affective symptoms are associated with markers of inflammation and immune activation in bipolar disorders but not in schizophrenia. Journal of psychiatric research. 2011;45:1608–1616. doi: 10.1016/j.jpsychires.2011.08.003. [DOI] [PubMed] [Google Scholar]
- 13.Fernandez-Egea E, Bernardo M, Donner T, Conget I, Parellada E, Justicia A, Esmatjes E, Garcia-Rizo C, Kirkpatrick B. Metabolic profile of antipsychotic-naive individuals with non-affective psychosis. The British journal of psychiatry. 2009;194:434–438. doi: 10.1192/bjp.bp.108.052605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Fernandes BS, Steiner J, Bernstein HG, Dodd S, Pasco JA, Dean OM, Nardin P, Goncalves CA, Berk M. C-reactive protein is increased in schizophrenia but is not altered by antipsychotics: meta-analysis and implications. Molecular psychiatry. 2016;21:554–564. doi: 10.1038/mp.2015.87. [DOI] [PubMed] [Google Scholar]
- 15.Vuksan-Cusa B, Sagud M, Jakovljevic M, Peles AM, Jaksic N, Mihaljevic S, Zivkovic M, Mikulic SK, Jevtovic S. Association between C-reactive protein and homocysteine with the subcomponents of metabolic syndrome in stable patients with bipolar disorder and schizophrenia. Nordic journal of psychiatry. 2013;67:320–325. doi: 10.3109/08039488.2012.745601. [DOI] [PubMed] [Google Scholar]
- 16.Suvisaari J, Loo BM, Saarni SE, Haukka J, Perala J, Saarni SI, Viertio S, Partti K, Lonnqvist J, Jula A. Inflammation in psychotic disorders: a population-based study. Psychiatry research. 2011;189:305–311. doi: 10.1016/j.psychres.2011.07.006. [DOI] [PubMed] [Google Scholar]
- 17.Stojanovic A, Martorell L, Montalvo I, Ortega L, Monseny R, Vilella E, Labad J. Increased serum interleukin-6 levels in early stages of psychosis: associations with at-risk mental states and the severity of psychotic symptoms. Psychoneuroendocrinology. 2014;41:23–32. doi: 10.1016/j.psyneuen.2013.12.005. [DOI] [PubMed] [Google Scholar]
- 18.Lin CC, Chang CM, Liu CY, Huang TL. Increased high-sensitivity C-reactive protein levels in Taiwanese schizophrenic patients. Asia-Pacific psychiatry. 2013;5:E58–63. doi: 10.1111/appy.12078. [DOI] [PubMed] [Google Scholar]
- 19.Kuo FC, Lee CH, Hsieh CH, Kuo P, Chen YC, Hung YJ. Lifestyle modification and behavior therapy effectively reduce body weight and increase serum level of brain-derived neurotrophic factor in obese non-diabetic patients with schizophrenia. Psychiatry research. 2013;209:150–154. doi: 10.1016/j.psychres.2012.11.020. [DOI] [PubMed] [Google Scholar]
- 20.Klemettila JP, Kampman O, Seppala N, Viikki M, Hamalainen M, Moilanen E, Leinonen E. Cytokine and adipokine alterations in patients with schizophrenia treated with clozapine. Psychiatry research. 2014;218:277–283. doi: 10.1016/j.psychres.2014.04.049. [DOI] [PubMed] [Google Scholar]
- 21.Joshi KB, Nillawar A, Thorat AP. Cardiovascular disease risk in schizophrenia patients: a case control study. Journal of clinical and diagnostic research. 2013;7:2694–2696. doi: 10.7860/JCDR/2013/7592.3734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hepgul N, Pariante CM, Dipasquale S, DiForti M, Taylor H, Marques TR, Morgan C, Dazzan P, Murray RM, Mondelli V. Childhood maltreatment is associated with increased body mass index and increased C-reactive protein levels in first-episode psychosis patients. Psychological medicine. 2012;42:1893–1901. doi: 10.1017/S0033291711002947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Frydecka D, Misiak B, Pawlak-Adamska E, Karabon L, Tomkiewicz A, Sedlaczek P, Kiejna A, Beszlej JA. Interleukin-6: the missing element of the neurocognitive deterioration in schizophrenia? The focus on genetic underpinnings, cognitive impairment and clinical manifestation. European archives of psychiatry and clinical neuroscience. 2015;265:449–459. doi: 10.1007/s00406-014-0533-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Fawzi MH, Fawzi MM, Fawzi MM, Said NS. C-reactive protein serum level in drug-free male Egyptian patients with schizophrenia. Psychiatry research. 2011;190:91–97. doi: 10.1016/j.psychres.2011.05.010. [DOI] [PubMed] [Google Scholar]
- 25.Dickerson F, Stallings C, Origoni A, Vaughan C, Khushalani S, Yang S, Yolken R. C-reactive protein is elevated in schizophrenia. Schizophrenia research. 2013;143:198–202. doi: 10.1016/j.schres.2012.10.041. [DOI] [PubMed] [Google Scholar]
- 26.De Berardis D, Conti CM, Marini S, Serroni N, Moschetta FS, Carano A, Valchera A, Iasevoli F, Fornaro M, Perna G, Di Iorio G, Martinotti G, Niolu C, et al. C-reactive protein level and its relationship with suicide risk and alexithymia among newly diagnosed, drug-naïve patients with non-affective psychosis. European Journal of Inflammation. 2013;11:215–221. [Google Scholar]
- 27.Carrizo E, Fernandez V, Quintero J, Connell L, Rodriguez Z, Mosquera M, Acosta A, Baptista T. Coagulation and inflammation markers during atypical or typical antipsychotic treatment in schizophrenia patients and drug-free first-degree relatives. Schizophrenia research. 2008;103:83–93. doi: 10.1016/j.schres.2008.03.004. [DOI] [PubMed] [Google Scholar]
- 28.Akanji AO, Ohaeri JU, Al-Shammri S, Fatania HR. Association of blood levels of C-reactive protein with clinical phenotypes in Arab schizophrenic patients. Psychiatry research. 2009;169:56–61. doi: 10.1016/j.psychres.2008.06.010. [DOI] [PubMed] [Google Scholar]
- 29.Hsuchou H, Kastin AJ, Mishra PK, Pan W. C-reactive protein increases BBB permeability: implications for obesity and neuroinflammation. Cellular physiology and biochemistry. 2012;30:1109–1119. doi: 10.1159/000343302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Najjar S, Pearlman DM, Devinsky O, Najjar A, Zagzag D. Neurovascular unit dysfunction with blood-brain barrier hyperpermeability contributes to major depressive disorder: a review of clinical and experimental evidence. Journal of neuroinflammation. 2013;10:142. doi: 10.1186/1742-2094-10-142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Uranova NA, Zimina IS, Vikhreva OV, Krukov NO, Rachmanova VI, Orlovskaya DD. Ultrastructural damage of capillaries in the neocortex in schizophrenia. The world journal of biological psychiatry. 2010;11:567–578. doi: 10.3109/15622970903414188. [DOI] [PubMed] [Google Scholar]
- 32.Hsuchou H, Kastin AJ, Pan W. Blood-borne metabolic factors in obesity exacerbate injury-induced gliosis. Journal of molecular neuroscience. 2012;47:267–277. doi: 10.1007/s12031-012-9734-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.van der Mast RC. Pathophysiology of delirium. J Geriatr Psychiatry Neurol. 1998;11:138–145. doi: 10.1177/089198879801100304. discussion 157–138. [DOI] [PubMed] [Google Scholar]
- 34.Singh B, Chaudhuri TK. Role of C-reactive protein in schizophrenia: an overview. Psychiatry research. 2014;216:277–285. doi: 10.1016/j.psychres.2014.02.004. [DOI] [PubMed] [Google Scholar]
- 35.Kuhlmann CR, Librizzi L, Closhen D, Pflanzner T, Lessmann V, Pietrzik CU, de Curtis M, Luhmann HJ. Mechanisms of C-reactive protein-induced blood-brain barrier disruption. Stroke. 2009;40:1458–1466. doi: 10.1161/STROKEAHA.108.535930. [DOI] [PubMed] [Google Scholar]
- 36.Irani S, Lang B. Autoantibody-mediated disorders of the central nervous system. Autoimmunity. 2008;41:55–65. doi: 10.1080/08916930701619490. [DOI] [PubMed] [Google Scholar]
- 37.Hanson DR, Gottesman II. Theories of schizophrenia: a genetic-inflammatory-vascular synthesis. BMC medical genetics. 2005;6:7. doi: 10.1186/1471-2350-6-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Breslow MJ, Miller CF, Parker SD, Walman AT, Traystman RJ. Effect of vasopressors on organ blood flow during endotoxin shock in pigs. The American journal of physiology. 1987;252:H291–300. doi: 10.1152/ajpheart.1987.252.2.H291. [DOI] [PubMed] [Google Scholar]
- 39.Micoulaud-Franchi JA, Faugere M, Boyer L, Fond G, Richieri R, Faget C, Cermolacce M, Philip P, Vion-Dury J, Lancon C. Elevated C-reactive protein is associated with sensory gating deficit in schizophrenia. Schizophrenia research. 2015;165:94–96. doi: 10.1016/j.schres.2015.03.018. [DOI] [PubMed] [Google Scholar]
- 40.Fan X, Pristach C, Liu EY, Freudenreich O, Henderson DC, Goff DC. Elevated serum levels of C-reactive protein are associated with more severe psychopathology in a subgroup of patients with schizophrenia. Psychiatry research. 2007;149:267–271. doi: 10.1016/j.psychres.2006.07.011. [DOI] [PubMed] [Google Scholar]
- 41.Dickerson F, Stallings C, Origoni A, Vaughan C, Khushalani S, Yolken R. Additive effects of elevated C-reactive protein and exposure to Herpes Simplex Virus type 1 on cognitive impairment in individuals with schizophrenia. Schizophrenia research. 2012;134:83–88. doi: 10.1016/j.schres.2011.10.003. [DOI] [PubMed] [Google Scholar]
- 42.Barzilay R, Lobel T, Krivoy A, Shlosberg D, Weizman A, Katz N. Elevated C-reactive protein levels in schizophrenia inpatients is associated with aggressive behavior. European psychiatry. 2016;31:8–12. doi: 10.1016/j.eurpsy.2015.09.461. [DOI] [PubMed] [Google Scholar]
- 43.Miller BJ, Culpepper N, Rapaport MH. C-reactive protein levels in schizophrenia: a review and meta-analysis. Clinical schizophrenia & related psychoses. 2014;7:223–230. doi: 10.3371/CSRP.MICU.020813. [DOI] [PubMed] [Google Scholar]
- 44.Lahkola A, Tokola K, Auvinen A. Meta-analysis of mobile phone use and intracranial tumors. Scandinavian journal of work, environment & health. 2006;32:171–177. doi: 10.5271/sjweh.995. [DOI] [PubMed] [Google Scholar]
- 45.Akiyama K. Serum levels of soluble IL-2 receptor alpha, IL-6 and IL-1 receptor antagonist in schizophrenia before and during neuroleptic administration. Schizophrenia research. 1999;37:97–106. doi: 10.1016/s0920-9964(98)00140-6. [DOI] [PubMed] [Google Scholar]
- 46.Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gotzsche PC, Ioannidis JP, Clarke M, Devereaux PJ, Kleijnen J, Moher D. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. Journal of clinical epidemiology. 2009;62:e1–34. doi: 10.1016/j.jclinepi.2009.06.006. [DOI] [PubMed] [Google Scholar]
- 47.Stang A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol. 2010;25:603–605. doi: 10.1007/s10654-010-9491-z. [DOI] [PubMed] [Google Scholar]
- 48.Higgins JP, Green S. Cochrane handbook for systematic reviews of interventions. John Wiley & Sons; 2011. [Google Scholar]
- 49.Hedges LV, Pigott TD. The power of statistical tests in meta-analysis. Psychological methods. 2001;6:203–217. [PubMed] [Google Scholar]
- 50.DerSimonian R, Laird N. Meta-analysis in clinical trials. Controlled clinical trials. 1986;7:177–188. doi: 10.1016/0197-2456(86)90046-2. [DOI] [PubMed] [Google Scholar]
- 51.Begg CB, Mazumdar M. Operating characteristics of a rank correlation test for publication bias. Biometrics. 1994;50:1088–1101. [PubMed] [Google Scholar]
- 52.Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. Bmj. 1997;315:629–634. doi: 10.1136/bmj.315.7109.629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Duval S, Tweedie R. Trim and fill: A simple funnel-plot-based method of testing and adjusting for publication bias in meta-analysis. Biometrics. 2000;56:455–463. doi: 10.1111/j.0006-341x.2000.00455.x. [DOI] [PubMed] [Google Scholar]
- 54.Altman DG, Bland JM. Interaction revisited: the difference between two estimates. Bmj. 2003;326:219. doi: 10.1136/bmj.326.7382.219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Metcalf SA, Jones PB, Nordstrom T, Timonen M, Mäki P, Miettunen J, Jääskeläinen E, Järvelin MR, Stochl J, Murray GK, Veijola J, Khandaker GM. Serum C-reactive protein in adolescence and risk of schizophrenia in adulthood: A prospective birth cohort study. Brain, Behavior, and Immunity. 2017;59:53–259. doi: 10.1016/j.bbi.2016.09.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Zhang Q, Hong W, Li H, Peng F, Wang F, Li N, Xiang H, Zhang Z, Su Y, Huang Y, Zhang S, Zhao G, Zhou R, et al. Increased ratio of high sensitivity C-reactive protein to interleukin-10 as a potential peripheral biomarker of schizophrenia and aggression. International journal of psychophysiology. 2017;114:9–15. doi: 10.1016/j.ijpsycho.2017.02.001. [DOI] [PubMed] [Google Scholar]
- 57.Goto M, Sugimoto K, Hayashi S, Ogino T, Sugimoto M, Furuichi Y, Matsuura M, Ishikawa Y, Iwaki-Egawa S, Watanabe Y. Aging-associated inflammation in healthy Japanese individuals and patients with Werner syndrome. Experimental gerontology. 2012;47:936–9. doi: 10.1016/j.exger.2012.08.010. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.