Abstract
Context
There is a growing call to integrate palliative care for patients with advanced heart failure (HF). However, the knowledge to inform integration efforts comes largely from interview and survey research with individual patients and providers. This work has been critically important in raising awareness of the need for integration, but it is insufficient to inform solutions that must be enacted not by isolated individuals but by complex care teams. Research methods are urgently required to support systematic exploration of the experiences of patients with HF, family caregivers, and health care providers as they interact as a care team.
Objectives
To design a research methodology that can support systematic exploration of the experiences of patients with HF, caregivers, and health care providers as they interact as a care team.
Methods
This article describes in detail a methodology that we have piloted and are currently using in a multisite study of HF care teams.
Results
We describe three aspects of the methodology: the theoretical framework, an innovative sampling strategy, and an iterative system of data collection and analysis that incorporates four data sources and four analytical steps.
Conclusion
We anticipate that this innovative methodology will support groundbreaking research in both HF care and other team settings in which palliative integration efforts are emerging for patients with advanced nonmalignant disease.
Keywords: Health care team, palliative care integration, heart failure, qualitative research, grounded theory, complexity, communication, patient-centered method, interviews, text analysis
Introduction
Problem Statement
Worldwide rates of chronic heart failure (HF) are epidemic and increasing, with the number of deaths from advanced HF also increasing with an aging population.1–4 Amidst a growing call for the integration of palliative care into the care trajectory for patients with HF,5–12 research methods are required to support the systematic exploration of the experiences of HF patients, family caregivers, and health care providers, as they interact as a care team. Such research is fundamental to support the development, implementation, and assessment of palliative care integration initiatives that are responsive and resilient to the team conditions in which HF care is negotiated.
Background
Research and policy support for the integration of palliative care is expressed in a number of recent guidelines and reviews put forward by the heart specialist community,13–19 the primary care community,20–22 and the cardiac nursing community.23,24 Integration is variously defined, but usually involves both “upstreaming” the provision of chronic disease management and palliative care and a continuum of care that spans diagnosis to end of life to bereavement.25–27
This call for palliative care integration in HF care is based on evidence derived from studies of individual patients and providers. Interview and survey studies with patients with advanced HF find that they have physical, psychological, social, spiritual, and informational needs.28–33 These needs are similar to those of patients with advanced cancer;34 however, patients with HF understand less about their illness, have fewer choices regarding end-of-life care, and have more limited access to palliative care.35,36 Patients may desire communication that they do not receive: one study found that not one of 20 patients had discussed disease progression or advanced care planning with staff members.31 Similarly, patients report experiences in which prognosis communication is deferred by their physicians, although they would prefer it to occur at diagnosis or during optimal function.37 Although the majority of patients with HF die in hospital,4 patients may not be given sufficient choice regarding the place of death.38 In one study, 40% of patients received invasive life-sustaining treatments in the final days of life although their family members perceived they would have preferred palliative care.39
The needs, attitudes, and knowledge of individual providers also have been studied. Providers report HF prognostication as a key challenge because of the unpredictable HF trajectory.32,40–45 When unable to make accurate end-of-life predictions, physicians are reluctant to integrate palliative care conversations and services.19,29,46–48 Physicians may avoid discussing palliative care out of concern for destroying hope,49 or because of unfamiliarity with its principles and practices.50,51 Providers may hold the perception that palliative care is only relevant for patients who are clearly dying, as a result of its association with cessation of interventional treatment.44
The most popular proposed solutions to achieve palliative care integration are improved communication and coordination of services. Improved communication is called for in virtually every report in this domain.52 All the guidelines address communication,13–19 as do the conclusions of many empirical studies that recurrently call for sensitive and effective communication practices around end-of-life issues8,16,52,53 and improved interprofessional communication.19 However, as Jordan et al.54 have argued, “It is easy to say, ‘the issue is communication,’ and it is easy to say ‘we have to talk to each other.’ But it is hard to …create conversation that facilitates sense making and learning.”54(p. 11) For example, communication has been reported to be complicated when patients with advanced HF are unwilling to have end-of-life conversations at all.55,56
Calls for improved coordination center on a collaborative approach5 that would target points of “transfer and transition of care”57 and draw palliative specialists into the HF care team at critical junctures.58 Models proposed include new health care roles, such as the advanced practice nurse with both HF and palliative care specialization;59–61 an HF outreach model for community care;62 standard palliative care consultations for patients with advanced HF;63 and multi-professional HF management programs that formalize partnerships among cardiology, specialist palliative care, and general practice.13 A need for clear HF clinic staffing guidelines, systems of monitoring, and funding models also have been called for.64 The multidisciplinary team meeting is proposed as a communication forum to promote professional interchange regarding treatment strategies as goals of care change.8 Some coordination models are poised for trials of their effectiveness.63
In summary, the existing literature draws predominantly on interviews and survey methods with individual patients and providers. Although this research has produced compelling evidence about individual needs, attitudes, and practices, it provides little insight into how individuals work together in the complex system of an HF care team. If we base a complex organizational intervention such as palliative care integration on individuals’ knowledge alone, our efforts may yield unhelpful and uninterpretable outcomes.54,65 Therefore, we describe a robust theoretical framework and innovative methodology to support research into the experiences of patients with HF, family caregivers, and health care providers as they interactively respond to emergent palliative needs.
A Robust Theoretical Framework for Studying HF Care Teams
HF care is enacted within a system that includes the patient and their primary care and specialist physicians, nurses, social workers, homecare workers, and family caregivers. Although we use the term “HF care team” to refer to this complex system, we do not intend to imply coherence or stability. Indeed, HF care is delivered by a shifting roster of individuals who are often not well coordinated or connected; they are distributed across several institutions and settings in which values, routines, tools, and resources may differ. Furthermore, each individual participating in the HF care team also participates in other subsystems, such as the primary care team and the HF clinic team. Interactions among these other “teams” are shaped by the often conflicting language of each subsystem, overlapping scopes of practice, and role ambiguities. This “nesting” of teams and settings complicates the deceptively straightforward call for palliative care integration in HF care.
To account for such nuances, complexity theory is one of two orienting theoretical lenses informing the methodology. The two fundamental premises of complexity are the interdependence of parts in a whole (nondecomposability) and the intrinsically dynamic nature of reality (nonlinearity).66,67 Nondecomposability refers to the inability to fully understand a complex system by attending to its individual components in isolation because these components are dynamic and entangled.68,69 For example, in the HF care team, relationships are not simply reducible to division of labor or specialization; interdependencies within and between the specialty roles exist, are shaped by personal and organizational history, routines, and relations, and, therefore, give rise to unforeseeable events.70–74 Nonlinearity refers to the way in which interrelations between system components tend to complicate the system’s response to external influence. Complex systems do not reflect a linear logic; rather, they comprise nonlinear interdependencies among diverse agents. Thus, predictable change is not achievable through top-down mandates, such as regulations or guidelines. It comes about more spontaneously, through what Kauffman75 calls “self-organization,” in which local interactions between agents affect the broader system even when no agent has the intention to create such effects.75 Understanding such emergent properties is critical to any change effort, as they may reinforce existing patterns or facilitate system change in unpredictable ways.72,76 The theory of complex adaptive systems has been applied productively to the question of why practice interventions succeed or fail in the setting of primary care teams.54,65
Palliative care scholars have argued that complexity theory is particularly well suited to palliative care because suffering and quality of life are usefully approached as emergent properties that result from the interactions among all agents in the palliative care system, including the patient.77 This theoretical lens “honors the complex reality of human health”78 and positions us to understand the system in a way that maximizes the chance of effective intervention.
Because the HF care system is distributed across place and time, documents are central to interactions among team members. Rhetorical theories of genre are the second orienting lens informing the methodology to ensure sophisticated attention to this dimension of interactions on the HF care team.79–82 The central premise of these theories is that generic text types such as referral letters do not merely describe the clinical work, they also construct that work by what they allow or disallow. Genres provide their users with both resources and constraints, but they are not static. Whereas they reflect and reproduce cultural values and goals, they also can be used improvisationally to achieve less sanctioned less predictable goals. In this, genre theory is epistemologically compatible with complexity theory.
The Methodological Context of the Innovation
This innovative methodology, which was developed in Ontario Canada, is situated within the constructivist grounded theory tradition,83,84 a theory that aims to develop a well-integrated series of concepts that provide a theoretical explanation of a social phenomenon.85,86 Grounded theory has recently been called on to build more robust knowledge about palliative care integration in HF care46 because of its ability both to attend to local context, which is so important in the study of socially situated practices, and to develop theory that is likely to have analytical relevance, or transferability, beyond the local context. Constructivist grounded theory combines the use of sensitizing concepts from theory in the data collection and analytical procedures with a process of inductive theory-building.
An Innovative Sampling Method
The sampling strategy takes the patient as its focal point, and uses the patient’s sense of key members of their care team to build a series of HF team “sampling units.” Patients are recruited through HF clinics or primary care practices. Because patient gender, age, and severity of condition may influence the team’s attitudes toward and actions regarding palliative care, patients are sampled purposively for these characteristics. During the interview, a patient is asked to describe the people who play an important role in their care. With permission, these individuals are recruited for interviews. All participants are interviewed about the particular HF care team centered on the patient, providing a data set that maps congruence and conflict among expectations and experiences of palliative care.
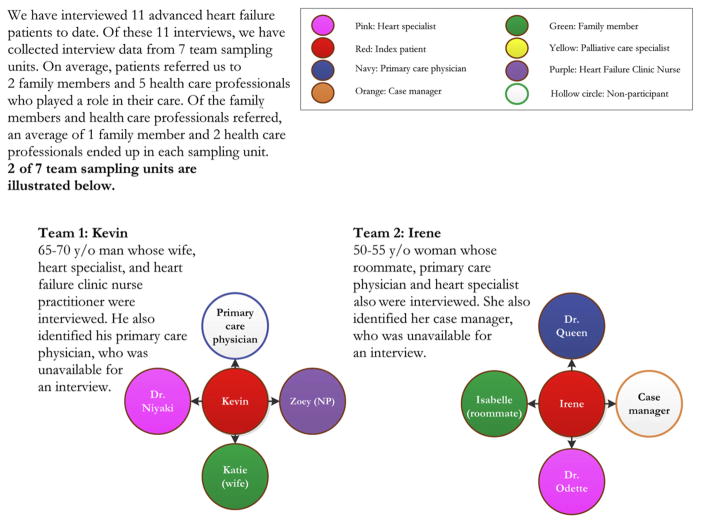
Sampling units have been used successfully to gather multiperspective data in studies of patients with chronic obstructive pulmonary disease,87,88 but have not been widely used to study HF care teams. Although Kaasalainen et al.46 interviewed patient and family caregiver dyads recruited through health care professionals, their interviews with health professionals did not explore that particular patient’s situation. An HF team sampling unit consists of at least three interviews: the index patient and at least two other team members. Pilot work has demonstrated the feasibility of this sampling method to create rich sampling units (Fig. 1).
Fig. 1.
Team sampling units.
A Well-Triangulated Data Collection and Data Analysis Strategy
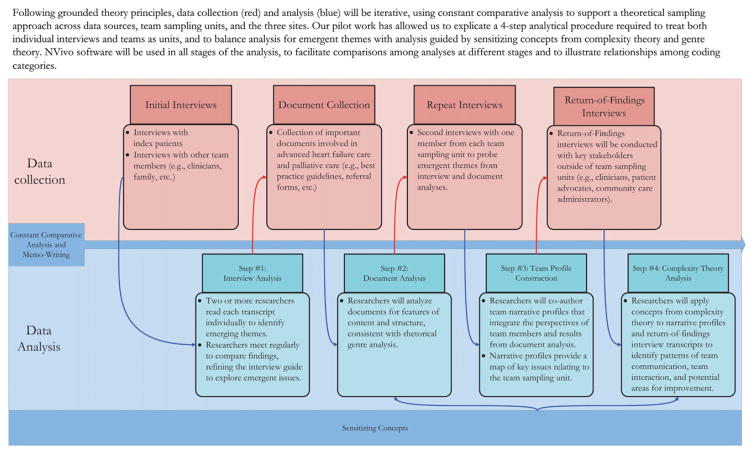
Following grounded theory principles, data collection and analysis proceed iteratively to support theoretical sampling across data sources, team sampling units, and study sites. Four kinds of data are collected (interviews, documents, repeat interviews, and return-of-findings) and a four-step analytical procedure is implemented to treat both individual interviews and teams as units, and to balance inductive analysis with analysis via sensitizing theoretical concepts. NVivo software89 (QSR International (Americas) Inc., Cambridge, MA) is used throughout the analysis to facilitate comparisons across analytical steps and coding categories. Analytical memo-writing according to grounded theory procedures is ongoing throughout the entire analysis. Fig. 2 illustrates the iterative process of data collection and analysis described in detail below.
Fig. 2.
Data collection and analysis.
Data Collection: Initial Interviews
Initial, semistructured interviews with patients explore the patients’ experiences, goals, and concerns regarding their HF condition and care trajectory and identify their expectations regarding the roles of providers on their HF care team. Their sense of key documents also is explored. The interview guide is based on patient-centered interviewing techniques.90 Because patients and family care-givers may not have had the idea of “palliative care” introduced to them previously in the care trajectory, or might not acknowledge its relevance to their situation, the interviewer does not introduce this terminology. Instead, the language of the functions of palliative care is used to pose broad questions about expectations, hopes, and fears for the future, recent changes in their health status (e.g., hospitalizations) and related needs (physical, psychological, social, spiritual, or practical), or experience of changes in their treatment plan (such as receiving an implanted cardiac defibrillator device).91 If patients or family caregivers should explicitly introduce the concept of palliative or end-of-life care, the interviewer explores this explicitly.
Initial, semistructured interviews with care-givers and health care professionals explore the participant’s expectations and experiences of palliative care in the patient’s care trajectory, including the responsibilities and involvement of various care team members. These interviews also seek to identify current communication and coordination practices, including documents in use that influence the team practice environment. Health care providers are asked to consult the patient’s medical record prior to the interview to facilitate discussion of palliative care needs in their particular case. In addition to patient-specific questions, health care providers are asked general questions that afford the opportunity to talk about the representativeness of this patient’s case in their professional experience and to consider other, anonymous examples of how palliative care can come about for patients with advanced HF. All interview transcripts are anonymized and assigned a study code for the team-sampling unit.
Data Analysis: Step 1
Analysis of individual interviews uses grounded theory’s constant comparative strategy to uncover emergent themes. Two or more researchers read each transcript independently and meet to compare and refine analyses. Following the strategy for theoretical sampling, such meetings occur after the initial two interviews and regularly thereafter to determine saturation of the themes and allow the interview guide to be refined to explore emergent issues. Analysis also attends to disconfirming data, which can signal tensions and nonlinearity.85
Data Collection: Documents
Documents that are collected are those identified by participants as important, and include both generic policy documents and items from specific patients’ charts, such as consultation requests and multidisciplinary progress notes.
Data Analysis: Step 2
Documents are analyzed by two or more researchers for features of content and structure, following genre theory’s premise that these shape the actions users can accomplish in their daily work. Sensitizing concepts to be applied in the analysis include genre tensions (competing purposes at play in the structure of a genre), visual rhetoric (the way that layout shapes what it is possible to “say” in a template document), and genre sets82,92–94 (the relationships among multiple documents that make up a complete genre, such as the patient record).83,92–94
Data Collection: Repeat Interviews
Repeat interviews probe emergent themes and clarify ambiguities in team sampling unit data. For reasons of feasibility, we propose that an average of one member of a team sampling unit be asked to participate in a repeat interview; however, more than one team member could be approached for repeat interviews if they can provide rich reflection on the emergent issues arising in that team sampling unit.
Data Analysis: Step 3
To move the analysis from the consideration of individual transcripts to the exploration of the team unit, the third analytical step uses the first constant comparative interview analysis and the document genre analysis to create anonymized narrative team “profiles.” Lanham et al.65 have effectively used a similar “case summary” approach in their study of complexity in primary care. The profiles provide a map of areas of congruence and conflict in expectations, as well as strategies and actions regarding palliative care in advanced HF.
Data Collection: Return-of-Findings Interviews
A selection of narrative team profiles is presented to key informants to probe their reflections on the system issues they suggest. Key informants are purposively selected to add insight to the analysis based on disciplinary perspective (e.g., palliative care specialist), experience as a team member (e.g., a family physician involved in multiple team sampling units), or expertise regarding structural influences on the system (e.g., a regional care director).
Data Analysis: Step 4
Two or more researchers apply sensitizing concepts from complexity theory to the narrative team profiles and the return-of-findings interviews. Following Lanham et al.’s structure,65 key issues to be considered in this analytical step include but are not limited to: interdependence (what are the patterns of interdependence among HF team members?), emergence (what complex phenomena emerge in the system that seem more than the sum of their parts?), self-organization (what stable patterns in the system occur without hierarchical or formal control mechanisms?), and nonlinearity (where might small changes generate large consequences?).
Conclusion
The HF care team is a complex adaptive system that has yet to meaningfully integrate palliative care clinically or empirically. Initiatives to achieve integration cannot proceed effectively in the absence of systematic, rigorous study of the team context. Research methods are required that can support this work. This article describes an innovative and robust grounded theory methodology, framed by complexity science and genre theory, which we are currently using in a multisite research program studying how HF care teams negotiate emerging palliative care needs. We anticipate the methodology also could support innovative research in other team settings where palliative integration efforts are emerging for patients with advanced nonmalignant disease.
Acknowledgments
The authors wish to thank the patients, family members, and health professionals who participated in the pilot study. This research program is funded by the Canadian Institutes for Health Research (CIHR), the Academic Medical Association of Southwestern Ontario (AMOSO), and Dr. Lingard is also supported as a Western University Department of Medicine Program of Experimental Medicine (POEM) scientist.
Footnotes
Disclosures
The authors have no conflicts of interest to disclose.
References
- 1.Ezekowitz JA, Kaul P, Bakal JA, et al. Declining in-hospital mortality and increasing heart failure incidence in elderly patients with first myocardial infarction. J Am Coll Cardiol. 2009;53:13–20. doi: 10.1016/j.jacc.2008.08.067. [DOI] [PubMed] [Google Scholar]
- 2.Ross H, Howlett J, Arnold JM, et al. Treating the right patient at the right time: access to heart failure care. Can J Cardiol. 2006;22:749–754. doi: 10.1016/s0828-282x(06)70290-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Johansen H, Strauss B, Arnold JM, Moe G, Liu P. On the rise: the current and projected future burden of congestive heart failure hospitalization in Canada. Can J Cardiol. 2003;19:430–435. [PubMed] [Google Scholar]
- 4.Kaul P, McAlister FA, Ezekowitz JA, et al. Resource use in the last 6 months of life among patients with heart failure in canada. Arch Intern Med. 2011;171:211–217. doi: 10.1001/archinternmed.2010.365. [DOI] [PubMed] [Google Scholar]
- 5.Jaarsma T, Beattie JM, Ryder M, et al. Palliative care in heart failure: a position statement from the palliative care workshop of the Heart Failure Association of the European Society of Cardiology. Eur J Heart Fail. 2009;11:433–443. doi: 10.1093/eurjhf/hfp041. [DOI] [PubMed] [Google Scholar]
- 6.Hunt SA, Abraham WT, Chin MH, et al. ACC/AHA 2005 guideline update for the diagnosis and management of chronic heart failure in the adult: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Update the 2001 Guidelines for the Evaluation and Management of Heart Failure): developed in collaboration with the American College of Chest Physicians and the International Society for Heart and Lung Transplantation: endorsed by the Heart Rhythm Society. Circulation. 2005;112:e154–e235. doi: 10.1161/CIRCULATIONAHA.105.167586. [DOI] [PubMed] [Google Scholar]
- 7.Genest J, McPherson R, Frohlich J, et al. 2009 Canadian Cardiovascular Society/Canadian guidelines for the diagnosis and treatment of dyslipidemia and prevention of cardiovascular disease in the adult—2009 recommendations. Can J Cardiol. 2009;25:567–579. doi: 10.1016/s0828-282x(09)70715-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ryder M, Beattie JM, O’Hanlon R, McDonald K. Multidisciplinary heart failure management and end of life care. Curr Opin Support Palliat Care. 2011;5:317–321. doi: 10.1097/SPC.0b013e32834d749e. [DOI] [PubMed] [Google Scholar]
- 9.Arnold JM, Liu P, Demers C, et al. Canadian Cardiovascular Society consensus conference recommendations on heart failure 2006: diagnosis and management. Can J Cardiol. 2006;22:23–45. doi: 10.1016/s0828-282x(06)70237-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Brydie A, Chow BJ, Dennie C, et al. Canadian Cardiovascular Society/Canadian Association of Radiologists consensus training standards for cardiac computed tomography. Can J Cardiol. 2010;26:181–184. doi: 10.1016/s0828-282x(10)70366-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Silversides CK, Marelli A, Beauchesne L, et al. Canadian Cardiovascular Society 2009 Consensus Conference on the management of adults with congenital heart disease: executive summary. Can J Cardiol. 2010;26:143–150. doi: 10.1016/s0828-282x(10)70352-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.McKelvie RS. The 2011 Canadian Cardiovascular Society heart failure management guidelines update: focus on sleep apnea, renal dysfunction, mechanical circulatory support, and palliative care. Can J Cardiol. 2011;27:319–338. doi: 10.1016/j.cjca.2011.03.011. [DOI] [PubMed] [Google Scholar]
- 13.McDonagh TA, Blue L, Clark AL, et al. European Society of Cardiology Heart Failure Association Standards for delivering heart failure care. Eur J Heart Fail. 2011;13:235–241. doi: 10.1093/eurjhf/hfq221. [DOI] [PubMed] [Google Scholar]
- 14.Howlett JG, McKelvie RS, Costigan J, et al. The 2010 Canadian Cardiovascular Society guidelines for the diagnosis and management of heart failure update: heart failure in ethnic minority populations, heart failure and pregnancy, disease management, and quality improvement/assurance programs. Can J Cardiol. 2010;26:185–202. doi: 10.1016/s0828-282x(10)70367-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.McKelvie RS, Moe GW, Cheung A, et al. The 2011 Canadian Cardiovascular Society heart failure management guidelines update: focus on sleep apnea, renal dysfunction, mechanical circulatory support, and palliative care. Can J Cardiol. 2011;27:319–338. doi: 10.1016/j.cjca.2011.03.011. [DOI] [PubMed] [Google Scholar]
- 16.Howlett JG. Palliative care in heart failure: addressing the largest care gap. Curr Opin Cardiol. 2011;26:144–148. doi: 10.1097/HCO.0b013e3283437468. [DOI] [PubMed] [Google Scholar]
- 17.Lewis EF. End of life care in advanced heart failure. Curr Treat Options Cardiovasc Med. 2011;13:79–89. doi: 10.1007/s11936-010-0100-y. [DOI] [PubMed] [Google Scholar]
- 18.Lemond L, Allen LA. Palliative care and hospice in advanced heart failure. Prog Cardiovasc Dis. 2011;54:168–178. doi: 10.1016/j.pcad.2011.03.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Low J. Palliative care in advanced heart failure: an international review of the perspectives of recipients and health professionals on care provision. J Card Fail. 2011;17:231–252. doi: 10.1016/j.cardfail.2010.10.003. [DOI] [PubMed] [Google Scholar]
- 20.Arnold JMO, Liu P, Demers C. [Accessed March 2, 2012];CHF: Ethical and end-of-life issues. 2007 Available from http://www.gacguidelines.ca/site/GAC_Guidelines/assets/pdf/CHF07_Ethical_and_End_of_Life_Issues_Summary.pdf.
- 21.Gallagher R. An approach to advance care planning in the office. Can Fam Physician. 2006;52:459–464. [PMC free article] [PubMed] [Google Scholar]
- 22.Ramsaroop SD, Reid MC, Adelman RD. Completing an advance directive in the primary care setting: what do we need for success? J Am Geriatr Soc. 2007;55:277–283. doi: 10.1111/j.1532-5415.2007.01065.x. [DOI] [PubMed] [Google Scholar]
- 23.Waterworth S, Gott M. Decision making among older people with advanced heart failure as they transition to dependency and death. Curr Opin Support Palliat Care. 2010;4:238–242. doi: 10.1097/SPC.0b013e328340684f. [DOI] [PubMed] [Google Scholar]
- 24.Waterworth S, Jorgensen D. It’s not just about heart failure–voices of older people in transition to dependence and death. Health Soc Care Community. 2010;18:199–207. doi: 10.1111/j.1365-2524.2009.00892.x. [DOI] [PubMed] [Google Scholar]
- 25.Paetkau S, Switzer G, Kasperski J for the Leaders Collaborative. [Accessed April 11, 2012];Advancing high quality, high value palliative care in Ontario: declaration of partnership and commitment to action (version 6) 2011 Available from http://www.ccac-ont.ca/Upload/ww/General/ICCP-HPC/ICCP%20HPC/Vision%20and%20Declaration%20of%20Partnership_v6%20(2011-12-08)%20D2pdf.pdf.
- 26.Byram EK. Upstream palliative care for the patient with a left ventricular assist device as destination therapy. Dimens Crit Care Nurs. 2012;31:18–24. doi: 10.1097/DCC.0b013e31823a537c. [DOI] [PubMed] [Google Scholar]
- 27.Buck HG, Hoyt Zambroski C. Upstreaming palliative care for patients with heart failure. J Cardiovasc Nurs. 2012;27:147–153. doi: 10.1097/JCN.0b013e318239f629. [DOI] [PubMed] [Google Scholar]
- 28.Rustoen T, Stubhaug A, Eidsmo I, et al. Pain and quality of life in hospitalized patients with heart failure. J Pain Symptom Manage. 2008;36:497–504. doi: 10.1016/j.jpainsymman.2007.11.014. [DOI] [PubMed] [Google Scholar]
- 29.Selman L, Harding R, Beynon T, et al. Improving end-of-life care for patients with chronic heart failure: “Let’s hope it’ll get better, when I know in my heart of hearts it won’t”. Heart. 2007;93:963–967. doi: 10.1136/hrt.2006.106518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Horne G, Payne S. Removing the boundaries: palliative care for patients with heart failure. Palliat Med. 2004;18:291–296. doi: 10.1191/0269216304pm893oa. [DOI] [PubMed] [Google Scholar]
- 31.Harding R, Selman L, Beynon T, et al. Meeting the communication and information needs of chronic heart failure patients. J Pain Symptom Manage. 2008;36:149–156. doi: 10.1016/j.jpainsymman.2007.09.012. [DOI] [PubMed] [Google Scholar]
- 32.Levenson JW, McCarthy EP, Lynn J, Davis RB, Phillips RS. The last six months of life for patients with congestive heart failure. J Am Geriatr Soc. 2000;48(Suppl 5):S101–S109. doi: 10.1111/j.1532-5415.2000.tb03119.x. [DOI] [PubMed] [Google Scholar]
- 33.Barnes S, Gott M, Payne S, et al. Prevalence of symptoms in a community-based sample of heart failure patients. J Pain Symptom Manage. 2006;32:208–216. doi: 10.1016/j.jpainsymman.2006.04.005. [DOI] [PubMed] [Google Scholar]
- 34.Bekelman DB, Rumsfeld JS, Havranek EP, et al. Symptom burden, depression, and spiritual well-being: a comparison of heart failure and advanced cancer patients. J Gen Intern Med. 2009;24:592–598. doi: 10.1007/s11606-009-0931-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Murray SA, Boyd K, Kendall M, et al. Dying of lung cancer or cardiac failure: prospective qualitative interview study of patients and their carers in the community. BMJ. 2002;325:929. doi: 10.1136/bmj.325.7370.929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Exley C, Field D, Jones L, Stokes T. Palliative care in the community for cancer and end-stage cardiorespiratory disease: the views of patients, lay-carers and health care professionals. Palliat Med. 2005;19:76–83. doi: 10.1191/0269216305pm973oa. [DOI] [PubMed] [Google Scholar]
- 37.Caldwell PH, Arthur HM, Demers C. Preferences of patients with heart failure for prognosis communication. Can J Cardiol. 2007;23:791–796. doi: 10.1016/s0828-282x(07)70829-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.McCarthy M, Hall JA, Ley M. Communication and choice in dying from heart disease. J R Soc Med. 1997;90:128–131. doi: 10.1177/014107689709000304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Lynn J, Harrell F, Jr, Cohn F, Wagner D, Connors AF., Jr Prognoses of seriously ill hospitalized patients on the days before death: implications for patient care and public policy. New Horiz. 1997;5:56–61. [PubMed] [Google Scholar]
- 40.Keay T. Palliative care in the nursing home. Generations. 1999;2:96–98. [Google Scholar]
- 41.Latimer EJ. Palliative care: more than just cancer. Can J CME. 2003;15:99–106. [Google Scholar]
- 42.Lunney JR, Lynn J, Foley DJ, Lipson S, Guralnik JM. Patterns of functional decline at the end of life. JAMA. 2003;289:2387–2392. doi: 10.1001/jama.289.18.2387. [DOI] [PubMed] [Google Scholar]
- 43.Stuart B, Alexander C, Arenella C, et al. Medical guidelines for determining prognosis in selected non-cancer diseases. The National Hospice and Palliative Care Organization publication. Hosp J. 1996;11:47–63. doi: 10.1080/0742-969x.1996.11882820. [DOI] [PubMed] [Google Scholar]
- 44.Murray SA, Kendall M, Boyd K, Sheikh A. Illness trajectories and palliative care. BMJ. 2005;330:1007–1011. doi: 10.1136/bmj.330.7498.1007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Gott M. Dying trajectories in heart failure. Palliat Med. 2007;21:95–99. doi: 10.1177/0269216307076348. [DOI] [PubMed] [Google Scholar]
- 46.Kaasalainen S, Strachan PH, Brazil K, et al. Managing palliative care for adults with advanced heart failure. Can J Nurs Res. 2011;43:38–57. [PubMed] [Google Scholar]
- 47.Chattoo S, Atkin KM. Extending specialist palliative care to people with heart failure: semantic, historical and practical limitations to policy guidelines. Soc Sci Med. 2009;69:147–153. doi: 10.1016/j.socscimed.2009.02.025. [DOI] [PubMed] [Google Scholar]
- 48.Hanratty B, Hibbert D, Mair F, et al. Doctors’ perceptions of palliative care for heart failure: focus group study. BMJ. 2002;325:581–585. doi: 10.1136/bmj.325.7364.581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Curtis JR, Treece PD, Nielsen EL, et al. Integrating palliative and critical care: evaluation of a quality-improvement intervention. Am J Respir Crit Care Med. 2008;178:269–275. doi: 10.1164/rccm.200802-272OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Nordgren L, Olsson H. Palliative care in a coronary care unit: a qualitative study of physicians’ and nurses’ perceptions. J Clin Nurs. 2004;13:185–193. doi: 10.1111/j.1365-2702.2004.00816.x. [DOI] [PubMed] [Google Scholar]
- 51.Green E, Gardiner C, Gott M, Ingleton C. Exploring the extent of communication surrounding transitions to palliative care in heart failure: the perspectives of health care professionals. J Palliat Care. 2011;27:107–116. [PubMed] [Google Scholar]
- 52.Ratcliffe TM. Healthcare providers need to improve communication with patients who have heart failure. Br J Gen Pract. 2007;57:180–182. [PMC free article] [PubMed] [Google Scholar]
- 53.Murray S, Boyd K. Using the ‘surprise question’ can identify people with advanced heart failure and COPD who would benefit from a palliative care approach. Palliat Med. 2011;25:382–384. doi: 10.1177/0269216311401949. [DOI] [PubMed] [Google Scholar]
- 54.Jordan ME, Lanham HJ, Crabtree BF, et al. The role of conversation in health care interventions: enabling sensemaking and learning. Implement Sci. 2009;4:15. doi: 10.1186/1748-5908-4-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Barclay S, Momen N, Case-Upton S, Kuhn I, Smith E. End-of-life care conversations with heart failure patients: a systematic literature review and narrative synthesis. Br J Gen Pract. 2011;61:e49–e62. doi: 10.3399/bjgp11X549018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Momen NC, Barclay SI. Addressing ‘the elephant on the table’: barriers to end of life care conversations in heart failure–a literature review and narrative synthesis. Curr Opin Support Palliat Care. 2011;5:312–316. doi: 10.1097/SPC.0b013e32834b8c4d. [DOI] [PubMed] [Google Scholar]
- 57.Arnold J, Howlett J, Ducharme A. Canadian Cardiovascular Society Consensus Conference guidelines on heart failure–2008 update: best practices for transition of care of heart failure patients, and the recognition, investigation and treatment of cardiomyopathies. Can J Cardiol. 2008;24:21–40. doi: 10.1016/s0828-282x(08)70545-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Swetz KM, Freeman MR, AbouEzzeddine OF, et al. Palliative medicine consultation for preparedness planning in patients receiving left ventricular assist devices as destination therapy. Mayo Clin Proc. 2011;86:493–500. doi: 10.4065/mcp.2010.0747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Daley A. Heart failure and palliative care services working in partnership: report of a new model of care. Palliat Med. 2006;20:593–601. doi: 10.1177/0269216306071060. [DOI] [PubMed] [Google Scholar]
- 60.Johnson MJ, Houghton T. Palliative care for patients with heart failure: description of a service. Palliat Med. 2006;20:211–214. doi: 10.1191/0269216306pm1120oa. [DOI] [PubMed] [Google Scholar]
- 61.Jaarsma T, van der Wal MH, Lesman-Leegte I, et al. Effect of moderate or intensive disease management program on outcome in patients with heart failure: Coordinating Study Evaluating Outcomes of Advising and Counseling in Heart Failure (COACH) Arch Intern Med. 2008;168:316–324. doi: 10.1001/archinternmed.2007.83. [DOI] [PubMed] [Google Scholar]
- 62.Bekelman DB. Outpatient palliative care for chronic heart failure: a case series. J Palliat Med. 2011;14:815–821. doi: 10.1089/jpm.2010.0508. [DOI] [PubMed] [Google Scholar]
- 63.Schwarz ER, Baraghoush A, Morrissey RP, et al. Pilot study of palliative care consultation in patients with advanced heart failure referred for cardiac transplantation. J Palliat Med. 2012;15:12–15. doi: 10.1089/jpm.2011.0256. [DOI] [PubMed] [Google Scholar]
- 64.Jessup M, Albert NM, Lanfear DE, et al. ACCF/AHA/HFSA 2011 survey results: current staffing profile of heart failure programs, including programs that perform heart transplant and mechanical circulatory support device implantation: a report of the ACCF Heart Failure and Transplant Committee, AHA Heart Failure and Transplantation Committee, and Heart Failure Society of America. Circ Heart Fail. 2011;4:378–387. doi: 10.1161/HHF.0b013e3182186210. [DOI] [PubMed] [Google Scholar]
- 65.Lanham HJ, McDaniel RR, Crabtree BF, et al. How improving practice relationships among clinicians and nonclinicians can improve quality in primary care. Jt Comm J Qual Patient Saf. 2009;35:457–466. doi: 10.1016/s1553-7250(09)35064-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Capra F. The web of life: A new scientific understanding of living systems. 1. New York: Anchor Books; 1996. [Google Scholar]
- 67.Capra F. The turning point: Science, society, and the rising culture. New York: Simon and Schuster; 1982. The systems view of life; pp. 265–304. [Google Scholar]
- 68.Eoyang GH, Berkas TH. Evaluating performance in a complex, adaptive system (CAS) In: Lissack M, Gunz H, editors. Managing complexity in organizations: a view in many directions. Westport, CT: Quorum Books; 1999. pp. 313–335. [Google Scholar]
- 69.Marion R, Bacon J. Organizational extinction and complex systems. Emergence. 2000;1:71–96. [Google Scholar]
- 70.Plesk P. Institute of Medicine, Committee on Quality of Health Care in America, editor. Crossing the quality chasm: a new health system for the 21st century. Washington, DC: National Academy Press; 2001. Redesigning health care with insights from the science of complex adaptive systems; pp. 322–335. [Google Scholar]
- 71.Holland JH. Emergence: From chaos to order. Reading, MA: Addison-Wesley; 1998. [Google Scholar]
- 72.McDaniel RR, Jr, Jordan ME, Fleeman BF. Surprise, surprise, surprise! A complexity science view of the unexpected. Health Care Manage Rev. 2003;28:266–278. doi: 10.1097/00004010-200307000-00008. [DOI] [PubMed] [Google Scholar]
- 73.McKelvey B. Avoiding complexity catastrophe in coevolutionary pockets: strategies for rugged landscapes. Organ Sci. 1999;10:294–321. [Google Scholar]
- 74.Waldrop MM. Complexity: The emerging science at the edge of order and chaos. New York: Simon & Schuster; 1992. [Google Scholar]
- 75.Kauffman SA. At home in the universe: The search for laws of self-organization and complexity. New York: Oxford University Press; 1995. [Google Scholar]
- 76.Goldstein J. Emergence as a construct: history and issues. Emergence. 2000;1:49–71. [Google Scholar]
- 77.Munday DF, Johnson SA, Griffiths FE. Complexity theory and palliative care. Palliat Med. 2003;17:308–309. doi: 10.1191/0269216303pm771oa. [DOI] [PubMed] [Google Scholar]
- 78.Roy DJ. Ethics and complexity in palliative care. J Palliat Care. 1995;11:3–4. [PubMed] [Google Scholar]
- 79.Miller C. Genre as social action. Q J Speech. 1984;70:151–167. [Google Scholar]
- 80.Schryer CF. Walking a fine line: writing ‘negative news’ letters in an insurance company. J Bus Tech Comm. 2000;14:445–497. [Google Scholar]
- 81.Bazerman C. Shaping written knowledge: The genre and activity of the experimental article in science. Madison, WI: University of Wisconsin Press; 1988. [Google Scholar]
- 82.Devitt AJ. Writing genres. Carbondale, IL: Southern Illinois University Press; 2004. [Google Scholar]
- 83.Charmaz K. Constructing grounded theory: A practical guide through qualitative analysis. London, UK: SAGE; 2006. [Google Scholar]
- 84.Charmaz K. Constructivist and objectivist grounded theory. In: Denzin NK, Lincoln YS, editors. Handbook of qualitative research. 2. Thousand Oaks, CA: Sage Publications; 2000. pp. 509–535. [Google Scholar]
- 85.Kennedy TJ, Lingard LA. Making sense of grounded theory in medical education. Med Educ. 2006;40:101–108. doi: 10.1111/j.1365-2929.2005.02378.x. [DOI] [PubMed] [Google Scholar]
- 86.Strauss AL, Corbin JM. Basics of qualitative research: Techniques and procedures for developing grounded theory. 2. Thousand Oaks, CA: Sage Publications; 1998. [Google Scholar]
- 87.Pinnock H, Kendall M, Murray SA, et al. Living and dying with severe chronic obstructive pulmonary disease: multi-perspective longitudinal qualitative study. BMJ. 2011;342:d142. doi: 10.1136/bmj.d142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Kendall M, Murray SA, Carduff E, et al. Use of multiperspective qualitative interviews to understand patients’ and carers’ beliefs, experiences, and needs. BMJ. 2009;339:b4122. doi: 10.1136/bmj.b4122. [DOI] [PubMed] [Google Scholar]
- 89.Richards L. Handling qualitative data: A practical guide. 2. Thousand Oaks, CA: Sage Publications; 2009. [Google Scholar]
- 90.Stewart M. Patient-centered medicine: Transforming the clinical method. 2. Abingdon, UK: Radcliffe Medical Press; 2003. [Google Scholar]
- 91.Grant RW, Ashburner JM, Hong CC, et al. Defining patient complexity from the primary care physician’s perspective: a cohort study. Ann Intern Med. 2011;155:797–804. doi: 10.7326/0003-4819-155-12-201112200-00001. [DOI] [PubMed] [Google Scholar]
- 92.Lingard L, Schryer C, Garwood K, Spafford M. ‘Talking the talk’: school and workplace genre tension in clerkship case presentations. Med Educ. 2003;37:612–620. doi: 10.1046/j.1365-2923.2003.01553.x. [DOI] [PubMed] [Google Scholar]
- 93.Varpio L, Schryer CF, Lehoux P, Lingard L. Working off the record: physicians’ and nurses’ transformations of electronic patient record-based patient information. Acad Med. 2006;81(Suppl 10):S35–S39. doi: 10.1097/01.ACM.0000237699.49711.35. [DOI] [PubMed] [Google Scholar]
- 94.Varpio L, Spafford MM, Schryer CF, Lingard L. Seeing and listening–a visual and social analysis of optometric record-keeping practices. J Bus Tech Comm. 2007;21:343–375. [Google Scholar]