Abstract
Post Syntax Trial, ‘Heart Team’ Concept has been ensconsed class I recommendation in both the European and ACC/AHA guidelines and has gained increasing traction in context of complex and multi modality procedures. Despite an arrray of advantages including the much touted - ‘the patient is central’, there are a plethora of un-addressed issues, some of which sentinel to our country, which threaten to make the ‘Heart Team’ concept a perfunctory exercise. As it stands today, ‘Heart Team’ is more of a fictional euphemism, a kind of 'Platonic Illusion' rather than a pragmatic reality.
Keywords: Heart Team, Bundled payment, Venn diagram
Speciality team based health care delivery is not a concept new to medicine. Infact, it derives its origin to the Venn diagrams originally described by John Venn in 1880. These are schematic diagrams used in the logic theory of mathematics and consist of overlapping circles that demonstrate relationship between finite collection of things called ‘sets’. These diagrams have been adopted relatively recently to ‘understand the roles of various stake holders in the management of cardiovascular disease from its diagnosis through its treatment’.1 A team concept is established in a much advanced way in Oncology and Organ Transplant programmes. Tumour boards have been making multi speciality disease management decisions in oncology since 1950s.2 But the coinage of the specific term ‘Heart Team’ is rather recent and was only incorporated in guidelines subsequent to the pivotal SYNTAX Trial. European guidelines ensconse class IC recommendation to the concept of ‘Heart Team’ as do the ACC/AHA guidelines, and is at the core of ‘Integrated Practice Units’.
Not withstanding all this, the ‘Heart Team’ approach has not yet been widely implemented for a myriad of reasons including the novelty of the concept, lack of experience, lack of unequivocally proven benefit, logistical issues as well as turf protection.3 However, cardiovascular medicine is learning from efforts in parallel specialities, the most visible being oncology, and the ‘Heart Team’ concept has lately gained increasing traction in context of broad range of procedures like coronary interventions and trans catheter aortic valve replacement (TAVR) and other complex endovascular interventions. This avoids ‘cherry picking’4 of patients according to the doctor’s own expertise, preferences and interests. A glaring example is proximal LAD stenosis. If the point of first contact was an interventional cardiologist, patient landed on the cath table and if it was a surgeon, invariably the patient ended up at the operation table!
In an era of evidence based medicine, validated by salutary effects of appropriate use criteria, and rapid pace of ever changing technology, applying a vast plethora of information available in a meaningful way becomes exceedingly challenging, infact nigh impossible. Its thus very important for a physician to synthesize this vast, varied and at times confusing knowledge and present it in a form intelligible to the patient and his family. Its rather unfortunate, but never-the-less a stark reality, that the debate for any coronary artery disease (CAD) is limited to PCI (Percutaneous Coronary Intervention) and CABG (Coronary Artery Bypass Graft), oblivious to the fact that medical therapy too has marched pari-passu, with spectacular advances. There are extremes, where decision making is very simple, but majority of patients lie in an overlapping spectrum between the two polar opposites. Despite multiple randomized controlled trials like Syntax, Freedom, Excel and Ascert; large data bases like New York State Registry and robust data coming from observational studies, we still have situations where multiple options are feasible and ethical, for example, in multi vessel CAD in diabetics, chronic total occlusion, unprotected left main etc. The ‘Heart Team’ need to synthesize the information from not only controlled studies done in centres of excellence, but also from real world studies, which are applicable to an average clinician, as no single trial can provide an answer to all patients in all settings. The conclusions of such trials may be vitiated as a result of many confounding factors – the patient population, the exclusion and inclusion criteria, the way one performs the statistical analysis, the industry may influence, the personal ego, un-intentioned bias of the operator and lastly, the most gory, even the distorted financial incentives and the ulterior motives may play a part in what we come out as results. So these trials can not be applied in the face value and even if they can, the patient always remains a variable and ever moving target. Repeat revascularisation may not be an issue for a wealthy man but may be the single most important criterion for a poor man who may be brow beaten to consent for coronary revascularisation, after selling his land or putting dowry he collected for his daughter at stake.
Besides, convincing arguments that the ‘Heart Team’ should play a central role in decision making, it should be integral to the performance of the procedure itself as most procedures entail a complex interplay of multispeciality & multi modality skills. A case in point, ‘TAVR requires an assortment of technical and cognitive skills, including surgical expertise for vascular access, catheter-based skills for device delivery and placement, and imaging expertise for device positioning and follow-up assessments’4. Given that few, if any, physician would have a mastery of all these skills, a team based approach becomes not only desirable, but mandatory. Such teams will be required, and infact are sine qua non, for other complex processes like carotid revascularisation, percutaneous mitral valve repair, atrial fibrillation and endovascular stent graft for aortic aneurysm.
The ‘Heart Team’ concept has additional positives. It improves the results and helps perform the centre and operator credentialing. More over shared decision making may reduce culpability for decisions gone wrong & subsequent medico-legal litigations.3 This convergence is now being mandated even for reimbursement by federal agencies in USA and although there are practical institutional implementation issues, increasing collaboration is being demanded by the intelligentsia in the society too. There is this unverified anecdote in which Steve Jobbs invited all doctors involved in his care to a dinner meeting at his house with a view to stream lining the multi disciplinary care that his malignancy demanded, but as he noticed, was sadly lacking. Even intuity demands this kind of convergence for treatment of cardiovascular disorders, wherein all facets of atherosclerosis across all beds could be handled under one umbrella.
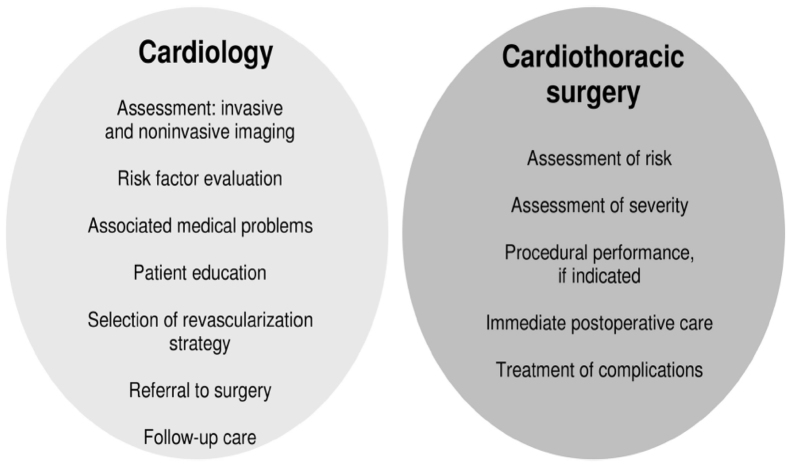
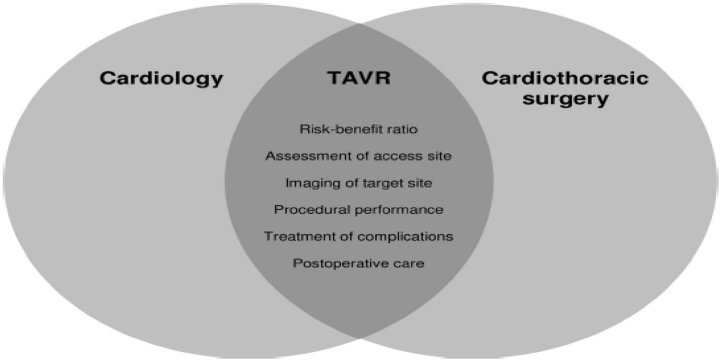
This contrasts starkly with our silo bound professional societies where each silo touches the others rather competitively, to the point of even being antagonistic, and rarely if ever collaboratively, even though they have same or similar agendas (Fig. 1). ‘While each professional society serves its core constituency well, there are many disadvantages to such a situation, including overlapping efforts that are inefficient; conflicting aims that confuse patients, payers and regulators alike; and diffusion of efforts to obtain increasingly scarce industry and government funding’.1 The blending of various stakeholders will have salutary effect complementing the efforts of each silo (Fig. 2).
Fig. 1.
At the present time, for patients with coronary artery disease, the professional silos of cardiology and cardio-thoracic surgery often do not overlap, despite the fact that the underlying missions have great similarity. Merging of these Venn diagrams either administratively or as a part of Heart Team could substantially improve patient education and care.1
Fig. 2.
The development of a TAVR Heart Team and blending the disciplines of cardiology and cardio-thoracic surgery will enhance optimal patient selection, procedural performance and outcome.1
This ‘Heart Team’ concept therefore can also be extended to our professional bodies. STS and the ACC jointly lobbied with federal agencies and industry for TAVR related issues and similar successful model exists in Germany. In 2010, German Society of Cardiology and German Society of Thoracic and Cardiovascular Surgery maintained a common registry of conventional and catheter based aortic valve replacement. These two societies have also written joint position papers and are designing cross professional training programmes and certifications.1 Further proof of the concept is that recently in Germany, a cardiac surgeon – Friedrich Mohr served as the President of the German Cardiology Meeting and a cardiologist Prof. Christian W. Hamm as the president of German Cardiac Surgery Annual Meeting. So this is not just clinical patient care, it can go down to administrative level also. That would be the day when we have just one professional society which incorporates, all elements of care of atherosclerosis, including coronary, cerebral and peripheral, be it medical, interventional or surgical, under one umbrella, besides ‘coordinating the educational and scientific initiatives, the disease management registries and outcome analyses, advocacy approach towards reimbursement and the training, education and credentialing of physicians and allied health professionals’.1 This would be ‘in everyone’s best interest – most of all the patients we serve’.1 In mathematical terms, the overlapping circles of Venn diagram will converge and coalesce into one.
However, not all is hunky dory with this kind of concept. There are obstacles, barriers and concerns regarding self interest and loss of autonomy that naturally arise with such a disruptive and far reaching proposal, but they are not insurmountable. Infact the theme of a recently concluded German Society for Thoracic and Cardiovascular Surgery Annual meeting was “ein Herz, ein Team”, converted into English, ‘one heart – one team’. Holmes et al.1 in an editorial in European Heart Journal, go a step further in advocating ‘One Heart, One Team, One Society’ – indeed an utopian wish.
Just as it has become fashionable and the ‘in-thing’ to talk of evidence based medicine, we must realize that recommending treatment based on these approaches remain somewhat imprecise because of lack of specificity in accurate risk prediction for an individual patient. Practice of Medicine is as much a ‘Science’, as an ‘Art’ and is imprecise, unpredictable and quite often patient specific. Even the patient’s expectations matter and the matrix on which patients base their expectations, and take decisions, are highly subjective & ill understood, and therefore it is important that the care should be customized to the patient needs and values. Besides factoring disease specific hard end points, ones assessment of the patient, his physical and psychological needs, his mental capabilities and his financial status should all form the basis of personalized treatment recommendations.
At this juncture, a few caveats are in order. Firstly there is no ‘I’ in the heart team4 and there is not even a ‘We’. Its all ‘You’ and the ‘You’ is the patient. The patient should be in control of his treatment strategies and his destiny. The doctor should only help him in making this decision by arming him with knowledge as contra distinct from prescribing it, or forcing it down his gullet. He should do hand holding and even if a wrong decision is being taken by a patient, it should be a gentle cajoling rather than a dogmatic dictat. Secondly, although it is a common and probable universal goal of patients to take the least invasive approach, that approach may not necessarily be the best strategy, specially for long term outcomes. ‘Patient wishes and physicians agreeing to bend to this is no reason to offer an inferior treatment’.5 The third caveat – institutions, after incorporating ‘Heart Team’ into care pathways, must also produce evidence of superior outcomes in terms of hard end points of mortality, CV morbidity and repeat interventions, as also cost effectiveness, quality of life and patient satisfaction.
Logistics too remain a major barrier3 The infrastructure has to be created where the images can be projected, angios played and data presented. Members may not be available, all at the pre annointed time. It may be disruptive for a busy cardiologist or a surgeon doing 3–4 heart surgeries a day and taking that time off for an half-hour interaction with the patient may be resented. Conflict of interest and even charisma and position on the hierarchical tree3 may play a role with more than a genuine chance that ‘Evidence Based’ medicine may give way to ‘Eminence Based’ medicine.
Further, the way we practice ‘Heart Team’ concept today is rather fragmented, inconsistent and uneven with shades of grey all over. Should it be applicable to straight forward decisions also or only to complex procedures? Will patients see each physician individually or in a group? Patient may not take a decision at the first meeting and may seek follow up meetings. What about patients mandating early or immediate surgery? Is there a possibility that if an exemption is made for early and immediate surgeries, physicians with dubious reputation may exploit that situation and certain physicians may do routine work masquerading as emergency to avoid the ‘Heart Team’. This is not just a theoretical consideration. This was infact an allegation that one of the New York based doctor faced and was investigated for doing routine coronary interventions through emergency route, for better reimbursement and for not putting the patients on the waiting list! Will the health system in the hospitals provide enough administrative and logistical support to make this a meaningful exercise because that would involve financial layouts? Who pays for the time of the physicians involved and even the institution’s efforts? Will the patient bear the cost or who would reimburse is point to debate. So we may have to incentivize multi disciplinary care.4
Even the attitude of our reimbursers and payers must change. At the present, physical time spent on procedures continues to be re-imbursed much more generously than the cognitive efforts put therein. Therefore without tackling reimbursement head on, ‘Heart Team’ risks becoming a perfunctory process with poor engagement of disgruntled physicians. May be bundled payment model4 may have some applicability here, that the entire heart team is compensated for a particular episode, irrespective of what methodology of treatment is followed. Playing the devil’s advocate, would this lead to all patients being put on medical therapy and no one is willing to do any interventions at all!
Is ‘Heart Team’ concept thus a reality or is it a ‘Platonic Illusion’? By the latter phase, I refer to the illusion of the intelligentsia class, drawing origins from Plato’s illusionary desire to set up an ideal republic on seeing his master Socrates being put to death by the Athenians – a society of enlightened men where no Socrates had to die or undergo desecration. Indeed a noble concept but destined to fail as it was ahead of it's times. So the moot question – Is the ‘Heart Team’ concept in cardiovascular medicine ahead of its time too? Neither do I have an answer to this conundrum nor I have the wherewithal to even attempt an answer. Most surely, as it stands today, the ‘Heart Team’ concept is more of a fad, a kind of fashionable euphemism, that seems to have caught on the fascination of medical fraternity. Most of it has been an empty rhetoric, suiting the medical fraternity, but much to the indignation and disadvantage of the hapless Indian patient.
Food for thought …
References
- 1.Holmes D.R., Jr., Mohr F., Hamm C.W., Mack M.J. Venn diagrams in cardiovascular disease: the Heart Team concept. Eur Heart J. 2014;35(2):66–68. doi: 10.1093/eurheartj/ehs466. [DOI] [PubMed] [Google Scholar]
- 2.Kesson E.M., Allardice G.M., George W.D., Burns H.J., Morrison D.S. Effects of multidisciplinary teams working on breast cancer survival: retrospective, comparative, interventional cohort study of 13,722 women. Br Med J. 2012;344:e2718. doi: 10.1136/bmj.e2718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Head S.J., Kaul S., Mack M.J. The rationale for Heart Team decision making for patients with stable, complex coronary artery disease. Eur Heart J. 2013:2510–2518. doi: 10.1093/eurheartj/eht059. [DOI] [PubMed] [Google Scholar]
- 4.Nallamothu B.K., Cohen D.J. No ‘I’ in Heart Team: incentivizing multidisciplinary care in cardiovascular medicine. Circ Cardiovasc Qual Outcomes. 2012;5:410–413. doi: 10.1161/CIRCOUTCOMES.112.966101. [DOI] [PubMed] [Google Scholar]
- 5.Goldenberg G., Kornowski R. Coronary bypass surgery versus percutaneous coronary intervention. Interv Cardiol. 2012;4(6):653–660. [Google Scholar]