Dear Editor,
We came across a case of 68 years old male admitted with complains of recent onset effort angina CCS class III since 45 days. On arrival to outpatient department he was hemodynamically stable with electrocardiogram showed 1 mm horizontal ST depression in antero-lateral leads. Echocardiography showed hypokinesia of distal interventricular septum and apical segments with left ventricular ejection fraction of 55%. He was subjected to coronary angiography, which revealed critical stenosis of the mid segment of left anterior descending artery and the proximal segment of diagonal artery. We decided for the percuteneous transluminal coronary angioplasty [PTCA]. Initially PTCA to the diagonal artery was done using 2.5 × 13 mm sirolimus eluting stent after predilatation with 1.5 × 10 mm balloon [Fig. 1A–D]. While predilatation of Mid LAD stenosis, there was rupture of 1.5 × 10 mm balloon and larger balloon [2.0 × 15 mm] could not be crossed. Hence we tried buddy wire technique, side branch anchoring wire techniques, but 2.0 × 15 mm balloon could not cross the lesion. We switched over to femoral access and left coronary system hooked with 7Fr. EBU catheter. The “mother-and-child” catheter was used and parked in the proximal segment of LAD. This helped us to cross the mid LAD stenosis easily with 2.0 × 15 mm balloon. The longer length, 3.0 × 36 mm, sirolimus eluting stent was deployed across the diagonal covering the mid LAD lesion. Final kissing balloon angioplasty of LAD and diagonal artery was performed which gave TIMI III flow with no residual lesions [Fig. 2A–F]. Post procedure the patient was discharged in stable condition on 2nd day on dual antiplatetet therapy.
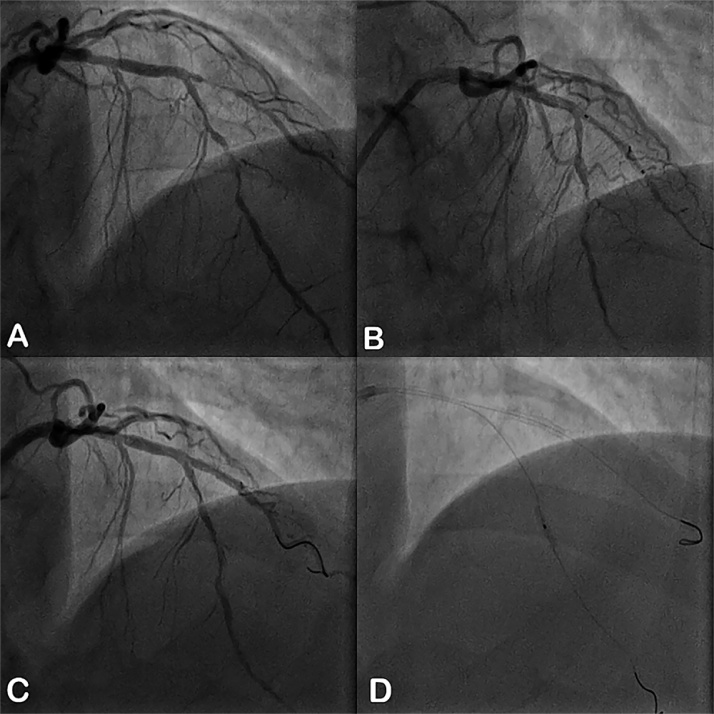
Fig. 1.
A–D: Transradial coronary angiography in AP cranial view showing critical stenosis of the mid segment of the left anterior descending artery (LAD) and the ostio-proximal segment of first diagonal artery (A); After predilatation of the first diagonal artery was deployed with 2.5 × 13 mm sirolimus eluting stent (B), with no residual stenosis of first diagonal artery with TIMI 3 flow (C); then mid segment of the LAD predilated with 1.5 × 10 mm balloon (D).
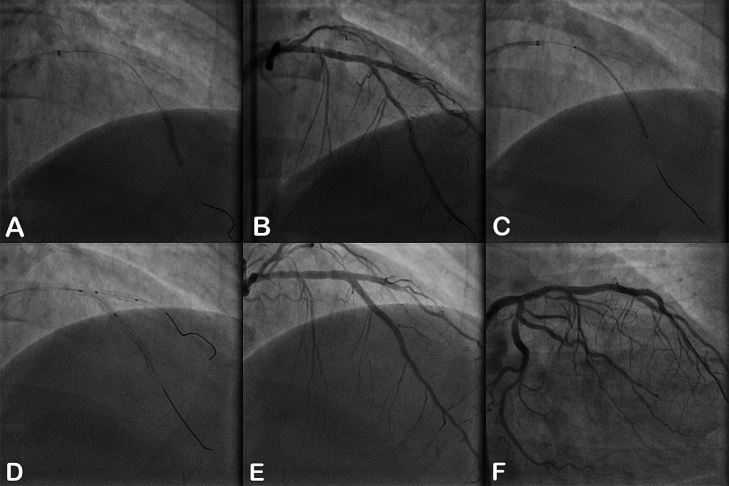
Fig. 2.
A–F: After initial predilatation and despite use of buddy wire not able to pass bigger sized balloons across the mid LAD. Hence we switched over to transfemoral approach using “Mother-and-child” catheter system for the better guide catheter support. Following the predilatation using 2.0 × 15 mm balloon (A), which achieved the adequate predilatation (B) to pass the 3.0 × 36 mm sirolimus eluting stent across the mid segment of LAD and the first diagonal artery (C). The final kissing balloon angioplasty was performed to complete the ‘T’ stenting technique (D). The final coronary angiography in AP cranial (E) and RAO caudal (F) showed no residual stenosis, no dissection with TIMI 3 flow of LAD and first diagonal artery.
Patient experienced fever with chills with rigors, mild chest discomfort after 10 days of index procedure. His ECG was unremarkable with echocardiography revealed moderate pericardial effusion with early signs of pericardial tamponade. Patient was readmitted and intravenous antibiotics were started. His complete blood picture revealed leucocytosis with prominence of lymphocytes. Chest X-ray showed bilateral infiltrates suggestive of bronchopneumonia. Patient had mild breathlessness at the rest, after discussion we decided for the pericardiocentesis. We removed 300 ml of straw colored pericardial fluid. Analysis of pericardial fluid was exudative with predominance of lymphocytes with normal sugar and chloride levels. ADA value was suggestive of non-tubercuous in nature. Hence, patient remained in the hospital for more than 1 week and again was discharged in stable condition after his fever subsided and total leukocyte count normalized. Patient presented to emergency department after 1 week again with complains of retrosternal chest discomfort. His electrocardiogram showed 1 mm ST- segment elevation in V1-4 with reciprocal ST segment depression in II, III, aVF. We suspected stent thrombosis, so he was shifted to cath lab for the check coronary angiography. It revealed large coronary aneurysm of mid segment of LAD with swirling of contrast [Fig. 3]. We retrospectively suspected the diagnosis of mycotic pseudo aneurysm in the background of history of a febrile episode. CT coronary angiography also showed myocotic pseudo aneurysm with sluggish flow into the distal segments of LAD and diagonal artery [Fig. 4A,B]. Patient refused any further treatment and was discharged with dual antiplatetet and anti-anginal therapy. Patient was asymptomatic while discharge. He has completed 3 month follow up without further deterioration.
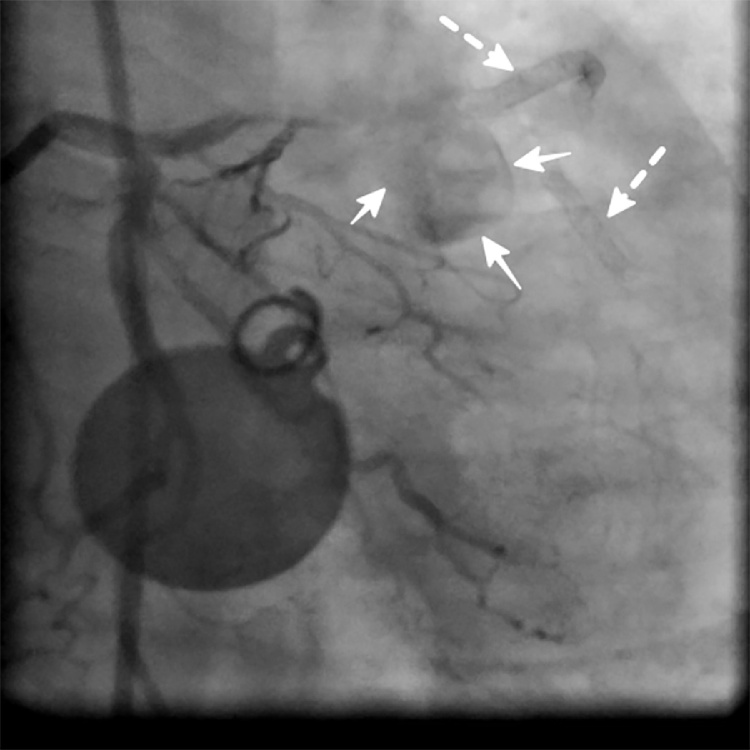
Fig. 3.
Check angiography in RAO caudal view showed coronary aneurysm arising from the proximal segment of LAD with phasic flow in to the aneurysmal sac. [Encircling solid arrows] There was TIMI 0 flow in the mid LAD and the first diagonal artery stents [Dashed arrows]. [There is metallic artifact in the background].
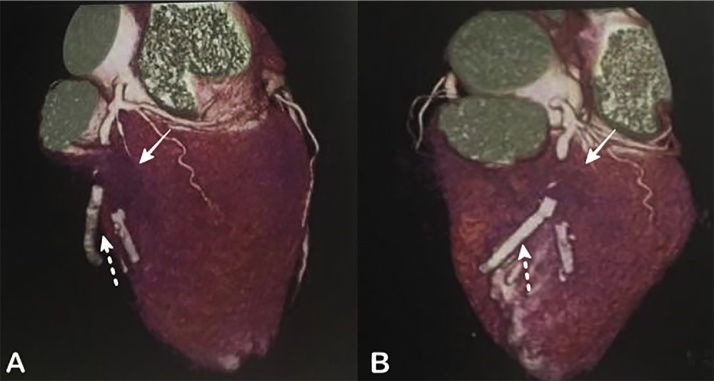
Fig. 4.
A, B – 3D volume-rendered Computed tomographic (CT) coronary angiography revealed thin walled coronary mycotic pseudoaneurysm [Solid arrow] with patent mid LAD and diagonal artery stents [Dashed arrow].
We reviewed the literature to find out any association between the use of the Mother-and-child’ guiding catheter and the development of coronary mycotic pseudoaneurysm. But there is no such association; on the contrarary there are reports of use of “mother-and-child” catheter for the delivery of stent graft to isolate coronary aneurysm from the main vessel and the use of coils for the closure of coronary artery fistula (CAF).1, 2 Mechanical factors like the use of oversized stents and balloons which can lead to arterial wall injury and direct infection commonly by Staphylococcus aureus, Pseudomonas species, fungal infection etc. is the main mechanism for the formation of coronary mycotic pseudoaneurysm. 3 The possibility of direct introduction of infection into the coronary artery vessel wall due to injury caused the deep intubation of “mother-and-child” catheter leading to formation of the mycotic aneurysm was thought in our case. “Mother-and-child” catheter comprises a flexible-tipped long 5-6-7 Fr catheter advanced through a standard 6-7-8 Fr guiding catheter to deeply intubate the target vessel, thus providing enough back-up support to enable the stent delivery.4 García-Blas et al. in their series of 16 patients who underwent complex percutaneous coronary intervention, one case of proximal type B coronary dissection was reported with the use of Mother-and-child” catheter.5 But minor injuries to the intimal layer of coronary artery may go unnoticed and not studied so far. In our case, coronary mycotic pseudoaneurysm developed at the site where the “child” catheter was placed and both the stents distal to it were unaffected.
In conclusion, as per corroborative evidences the development of coronary mycotic pseudoaneurysm in our case was secondary to minor trauma with the use of the “Mother-and-child” catheter and introduction of direct infection while prolonged procedure. To our knowledge, this is a first association in the literature. The proper precaution like co-axial alignment of the “Mother-and-child” catheter could avoid the injury to the coronary artery and sterilization techniques, the use of prophylactic antibiotics in case of prolonged procedures particularly in immunocomprised hosts like elderly patients, early removal of femoral or other indwelling catheters to limit bacteremia.
References
- 1.Boukhris M., Azzarelli S., Tomasello S.D., Elhadj Z.I., Marzà F., Galassi A.R. The guideliner catheter: a useful tool in the armamentarium of the interventional cardiologist. J Tehran Univ Hear Cent. 2015;10:208–214. [PMC free article] [PubMed] [Google Scholar]
- 2.Kodaira M., Numasawa Y. Successful percutaneous coil embolization of a severely tortuous coronary artery fistula using the mother-child-grandchild technique via a GuideLiner catheter. SAGE Open Med Case Rep. 2017;5:1–4. doi: 10.1177/2050313X16672382. Available from: http://journals.sagepub.com/doi/10.1177/2050313x16672382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chen I.-C., Chao T.-H., Wu I.-H., Kan C.-D., Fang C.-C. Afebrile mycotic aneurysm with rupture in right coronary artery after bare-metal stent implantation. Acta Cardiol Sin. 2012;28:344–348. [Google Scholar]
- 4.Kumar S., Gorog D.A., Secco G.G., Di Mario C, Kukreja N. The GuideLiner ‘child’ catheter for percutaneous coronary intervention – early clinical experience. J Invasive Cardiol. 2010;22:495–498. Available from: http://www.ncbi.nlm.nih.gov/pubmed/20944191. [PubMed] [Google Scholar]
- 5.García-Blas S., Núñez J., Mainar L. Usefulness and safety of a guide catheter extension system for the percutaneous treatment of complex coronary lesions by a transradial approach. Med Princ Pract. 2015;24:171–177. doi: 10.1159/000369620. [DOI] [PMC free article] [PubMed] [Google Scholar]