Abstract
Background
Exercise is a physiologic stress that helps the physicians to clarify the presence or absence of cardiovascular disease which may be obscure at rest. Although it is sensitive, its specificity is affected by several parameters, such as some metabolic conditions, some structural heart diseases, and some baseline electrocardiogram abnormalities. Currently, the relationship between coronary dominance and accuracy of EET is not examined. Therefore, this study was conducted to determine the potential impact of coronary dominance on the accuracy of EET.
Methods
In this retrospective study, data were gathered from 720 patients from four medical centers. The pattern of dominancy was determined, and the coronary dominance pattern of the patients who had normal angiograms despite abnormal EETs was compared to that from all the patients.
Results
Among the patients who had a normal angiogram despite an abnormal EET, 27% were left dominant while the frequency of left dominancy in the whole population of the study was only 10.9% (P = 0.013). There were no significant differences in baseline characteristics, such as age and sex, between the two studied groups.
Conclusion
The results indicated that the presence of left dominance in patients who had normal angiograms despite an abnormal EET was significantly higher than general population. Therefore, left dominance may be considered a confounding factor for EET, producing false positive results.
Keywords: Left dominant coronary circulation, False positive, Exercise tolerance test
1. Introduction
Exercise is a physiologic stress that helps one to clarify the presence or absence of cardiovascular disease which may be obscure at rest. Electrocardiographic exercise test (EET, also known as exercise tolerance test [ETT]), is one of the most frequent non-invasive clinical modalities used for this purpose. This inexpensive test is mainly used to elicit the likelihood and extent of myocardial ischemia indirectly.1, 2 Although it is sensitive and helpful in detecting coronary artery disease (CAD), its specificity is affected by several parameters which can lead to false positive results.2 EET is less specific in patients with some metabolic conditions (anemia, glucose load, hyperventilation, and hypokalemia), some structural heart diseases (severe aortic stenosis, mitral valve prolapsed, severe aortic or mitral regurgitation, cardiomyopathies, and left ventricular hypertrophy), marked resting ST segment depression, intraventricular conduction disturbances, pre-excitation syndromes, severe hypertension, severe hypoxia, sudden excessive exercise, supra-ventricular arrhythmias or digitalis therapy.3 Furthermore, currently EET plays a gate keeper role for angiography and only patients with a positive test result are referred for further studies. This leads to a decrease in the rate of true-negative test results, which eventually increases the sensitivity and decreases the specificity (post-referral bias).3
In addition, the pattern of coronary artery disease would also affect the specificity and sensitivity of the test. In patients who underwent coronary angiography, EET sensitivity is approximately 68% and specificity is 77%. The sensitivity for those with single vessel disease varies from 25% to 71% with the involved vessel, being most sensitive to lesion in the left anterior descending coronary artery, followed by abnormalities in the right coronary artery and the least sensitivity is noticed in patients suffering from isolated lesions of left circumflex coronary artery. These figures for patients with multivessel CAD are 81% sensitivity and 66% specificity. This may rise to 86% and 53%, respectively for the patients with left main or three-vessel coronary artery disease.4 Finally, according to Bayes’ theorem, the specificity and sensitivity of the test is affected by the baseline frequency of the disease in the studied population (pretest probability).3
Currently, to the best of our knowledge, nothing is known about the relationship between coronary dominance and accuracy of EET. Therefore, we conducted this study to determine the potential impact of coronary dominance on the accuracy of EET.
2. Methods
In this retrospective study, data were gathered from 720 patients from four medical centers who had undergone angiography during the year 2013. Information regarding age, sex, coronary dominance, the presence of coronary artery disease or microvascular dysfunction (also known as cardiac syndrome X), the reason for performing angiography, lab data, medications, and echocardiographic findings including valvular heart disease, left ventricular hypertrophy, etc. were collected. Among those who were referred for coronary angiography due to abnormal EETs, those who had mentioned confounding factors were excluded. All the patients’ angiographies and EETs were reviewed by our research team to exclude potential misinterpretations and biases. Coronary angiogram was considered as the gold standard of the study, and the coronary dominance pattern of the patients who had normal angiograms despite abnormal EETs was compared to all of the patients.
3. Statistical analysis
All statistical analyses were performed using the statistical Package for Social Sciences version 17.0 (SPSS Inc., Chicago, IL, USA). Continuous variables were described as mean ± SD and we analyzed them with t-test and Mann–Whitney U test when appropriate. Fisher's exact test was used for analysis of categorical variables. Several statistical diagnostic measures of electrocardiographic exercise testing including sensitivity, specificity, positive predictive value, negative predictive value, likelihood ratio, and accuracy of EET were calculated for all patients and those with right and left dominant coronary circulation.
4. Results
In this study, angiographic data were gathered from four medical centers from two cities of Iran, Shiraz and Rasht. A total of 720 profiles were included in the study. Among those who were referred for coronary angiography, 102 were referred due to an abnormal EET. Among them, 39 had a normal angiogram despite having an abnormal EET. From these 39 patients, none had baseline ECG abnormalities including pre-excitation, LVH, resting ST segment depression and intraventricular conduction defects. The only baseline abnormality was presence of the left anterior fascicular blocks with left axis deviation in three patients. Baseline echocardiogram among these patients revealed normal systolic function among all and there were no other significant structural abnormalities including severe valvular heart diseases. Baseline laboratory data were within the normal range regarding kidney function and electrolyte abnormality although four patients suffered from a controlled diabetes type II. The presence of left dominance in patients who had normal angiograms despite an abnormal EET was significantly higher than all of the patients (P = 0.013) (Table 1). No significant difference in age and sex was observed between these groups (P = 0.45 and P = 0.25, respectively).
Table 1.
Comparison of coronary dominance, age and sex between the patients with normal angiogram despite an abnormal exercise tolerance test and all of the patients.
| Patients with normal angiogram despite an abnormal EETa (n = 39) | All of the patients excluding false positives (n = 681) | P value | |
|---|---|---|---|
| Right dominant (%) | 67.6 | 83.3 | 0.013 |
| Left dominant (%) | 27 | 10.9 | |
| Codominant (%) | 5.4 | 5.9 | |
| Age (mean years ± SD) | 53.09 ± 9.56 | 56.1 ± 10.93 | 0.45 |
| Male (%) | 53.1 | 42.3 | 0.25 |
| Female (%) | 46.9 | 57.7 | |
| Family history of premature coronary disease (%) | 17.94 | 20.12 | 0.09 |
| Urban residence (%) | 26.7 | 22.1 | 0.12 |
| Rural residence (%) | 74.3 | 77.9 |
EET = exercise tolerance test.
Among all the studied subjects, a total of 248 patients had no significant obstructive coronary lesions. Excluding those with false positive ETT, the pattern of dominance among these patients was 82.6% right dominant, 12.3% left dominant, and 5.1% co-dominant. When considering this population as the control group, performing the previous analysis was again significant (P = 0.019). The specificity of EET was 11.9% for all patients. This parameter was 13.8% in the right dominant coronary circulation and 9% in those with left dominancy. The full data for statistical diagnostic measures of electrocardiographic exercise testing is provided in Table 2.
Table 2.
Statistical diagnostic measures of electrocardiographic exercise testing among the patients with right and left dominant coronary circulation.
| Sensitivity | Specificity | +LR | −LR | PPV | NPV | Accuracy | |
|---|---|---|---|---|---|---|---|
| Total | 98.3% | 11.9% | 1.11 | 0.14 | 61.4% | 83.3% | 62.7% |
| Right dominant | 100% | 13.8% | 1.16 | 0.00 | 67.1% | 100% | 69% |
| Left dominant | 80% | 9% | 0.8 | 2.2 | 28.5% | 50% | 31% |
Abbreviations: +LR = positive likelihood ratio, −LR = negative likelihood ratio, PPV = positive predictive value, NPV = negative predictive value.
5. Discussion
These results confirm that the presence of left dominance in patients who have normal angiograms despite an abnormal EET is significantly higher than general population. Therefore, left dominance may be considered a confounding factor for EET, producing false positive results. In other words, the specificity of EET in diagnosis of patients with CAD is lower in patients with left dominance.
To the best of our knowledge, it is for the first time that the impact of left dominance on EET results is investigated. The accuracy of EET in diagnosis of CAD is dependent on the age, gender, clinical features of the patient and the prevalence of CAD; therefore, EET seems more reliable in excluding CAD rather than confirming it.5 Since EET has a moderate reliability with an accuracy rate of 62.2% in the diagnosis of CAD.2 Moreover, it is reported that EET has a high false positive rate in diagnosing patients with latent CAD.6
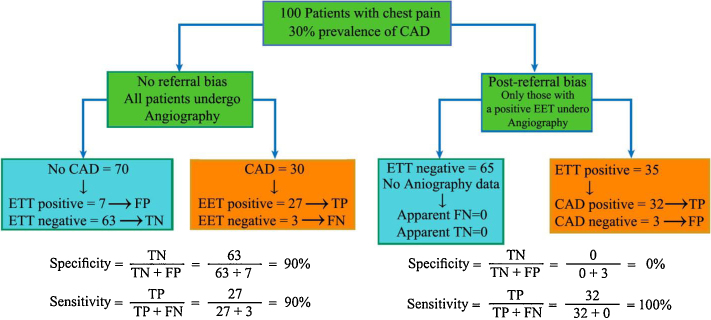
In this study, it was shown that left dominance may contribute to producing false positive results of EET, reducing its specificity in diagnosis of CAD. The specificity of EET in our study was 13.8% for those with right dominant circulation which was reduced to 9% in those with left dominancy. It should be noted that the very low specificity of EET in our study stems from the post-referral bias. As EET plays a gate keeper role for angiography, mostly those patients with a positive ETT test would be referred for angiography. Consequently, many of those with true negative and false negative tests are missed. This would derive the post-test specificity toward zero and sensitivity toward 100%, respectively (Fig. 1).7
Fig. 1.
The post-referral bias effect on EET specificity. When a test is used as the “gatekeeper” to coronary angiography, patients with a normal test result will not undergo angiography. Consequently, many negative data (whether true negative or false negative) are missed and their data will not be included in the specificity calculations (right). This has an effect of artificially reducing the apparent specificity of the non-invasive test (Abbreviations: EET = exercise ECG test; FN = false-negative; FP = false-positive; TN = true-negative; TP = true-positive).
Currently, some studies have shown that presence of left dominancy may affect the outcomes of patients.8 Left dominancy heightens the risk of death in the setting of ACS.9 This may be related to the fact that, in most individuals with left coronary dominance, the LCX supplies both inferior and lateral walls of the heart and its occlusion may place a larger area of the heart at risk.10 In addition, as the RCA does not reach the apex, formation of right to left collaterals is reduced and the protecting effect of collateral vessels is omitted.11 Left dominancy also may affect the prognosis of the patients surviving ACS. In the Alberta Provincial Project for Outcome Assessment in Coronary Heart Disease (APPROACH) database by Goldberg et al., a cohort of 27,289 patients with acute coronary syndrome who underwent revascularization were followed for 3.5 years. In that study, it was shown that patients with LD had a significantly higher mortality (hazard ratio 1.18). The mortality of patients with mixed and right dominance was similar.12 Left dominancy also increases the possibility of cardiac syndrome X,13 especially in women.14
To explain the mentioned effect of left dominancy, Gupta and colleagues performed a cadaveric study. They studied 75 cadaveric hearts. They injected the coronary vessels with colored cellulose acetate and determined the dominance. In those with a left-dominant circulation, they studied the branches and termination of the right coronary artery. They found that the RCA and its branching pattern had an important effect on developing myocardial ischemia in patients with left coronary dominance. They showed that the blood supply to the posterior surface of the right ventricle is meager. In 10% of the specimens, the RCA terminated on the anterior surface of the right ventricle with no branch to the posterior surface and the posterior right ventricular branch of the second segment of the RCA was absent in 20% of the hearts, while in 60% of the hearts, the size of these vessels was small, ranging from 5 to 15 mm, with majority (40%) having a length of 5 mm only. Overall, they noticed that in the majority of the hearts with left dominant circulation (60%), the blood supply to the posterior surface of the right ventricle was found to be sparse.15 This finding may help explain the effect of left dominancy on survival and exercise test.
This study had some limitations. It had a retrospective design and a prospective study with a greater sample size is needed for confirmation of our findings although realistically conducting such prospective study faces several technical and ethical issues. In addition, whether these results are true negative results or not is a matter of debate. It is now known that the angiographic demonstration of the absence of significant stenosis at coronary arteries is not sufficient to exclude myocardial ischemia and compared to intravascular ultrasonograms, luminal angiogram underestimates the magnitude of coronary atherosclerosis. So, mildly abnormal coronary angiograms cannot rule out the possibility of ischemia.16, 17 However, as this problem can be applied to both case and control groups, its effect is minimized.
These findings may raise the question of whether left dominance is a normal variation or a frequent anomaly. Once it was thought that early repolarization is a benign variant, but now some forms of it are proved as true malignant disease with possibility to transform into VF.18 There may be the same scenario about the left dominance.
6. Conclusion
These results confirm that the presence of left dominant coronary circulation in patients who have normal angiograms although an abnormal EET is significantly higher than general population and EET's specificity and accuracy are lower for patients with left dominant coronary circulation than those with right dominant one. So, left dominance may be considered a confounding factor for EET.
Conflicts of interest
The authors have none to declare.
Acknowledgment
This investigation is the result of a graduation thesis supported by grant number 95-11518 from vice-chancellery of research in Shiraz University of Medical Sciences. The authors would like to thank Dr. Nasrin Shokrpour at Center for Development of Clinical Research of Nemazee Hospital for editorial assistance.
References
- 1.Fletcher G.F., Mills W.C., Taylor W.C. Update on exercise stress testing. Am Fam Physician. 2006;74:1749–1754. [PubMed] [Google Scholar]
- 2.Habeeb Q.S. Reliability and accuracy of exercise tolerance test in the diagnosis of coronary heart disease. Dohuk Med J. 2007;1:98–104. [Google Scholar]
- 3.Chaitman B.R. Exercise stress testing. In: Bonow R.O., editor. Braunwald's Heart Disease: A Textbook of Cardiovascular Medicine. 9th ed. Saunders; Philadelphia: 2012. pp. 168–199. [Google Scholar]
- 4.Gibbons R.J., Balady G.J., Bricker J.T. ACC/AHA 2002 guideline update for exercise testing. Summary article: a report of the ACC/AHA Task Force on Practice Guidelines (Committee to Update the 1997 Exercise Testing Guidelines) J Am Coll Cardiol. 2002;40:1531–1540. doi: 10.1016/s0735-1097(02)02164-2. [DOI] [PubMed] [Google Scholar]
- 5.Banerjee A., Newman D.R., Van den Bruel A., Heneghan C. Diagnostic accuracy of exercise stress testing for coronary artery disease: a systematic review and meta-analysis of prospective studies. Int J Clin Pract. 2012;66:477–492. doi: 10.1111/j.1742-1241.2012.02900.x. [DOI] [PubMed] [Google Scholar]
- 6.Megnien J.L., Simon A. Exercise tolerance test for predicting coronary heart disease in asymptomatic individuals: a review. Atherosclerosis. 2009;205:579–583. doi: 10.1016/j.atherosclerosis.2008.12.034. [DOI] [PubMed] [Google Scholar]
- 7.Rozanski A., Diamond G.A., Berman D. The declining specificity of exercise radionuclide ventriculography. N Engl J Med. 1983;309:518–522. doi: 10.1056/NEJM198309013090902. [DOI] [PubMed] [Google Scholar]
- 8.Vasheghani- Farahani A., Kassaian S.E., Yaminisharif A. The association between coronary arterial dominancy and extent of coronary artery disease in angiography and paraclinical studies. Clin Anat. 2008;21:519–523. doi: 10.1002/ca.20669. [DOI] [PubMed] [Google Scholar]
- 9.Khan A.R., Khan Luni F., Bavishi C., Khan S., Eltahawy E.A. Left dominant circulation increases mortality in acute coronary syndrome: a systematic review and meta-analysis of observational studies involving 255,718 patients. Catheter Cardiovasc Interv. 2016;88:201–208. doi: 10.1002/ccd.26281. [DOI] [PubMed] [Google Scholar]
- 10.Raphael M.J., Hawtin D.R., Allwork S.P. The angiographic anatomy of the coronary arteries. Br J Surg. 1980;67:181–187. doi: 10.1002/bjs.1800670307. [DOI] [PubMed] [Google Scholar]
- 11.Hutchinson M.C. A study of the atrial arteries in man. J Anat. 1978;125:39–54. [PMC free article] [PubMed] [Google Scholar]
- 12.Goldberg A., Southern D.A., Galbraith P.D. Coronary dominance and prognosis of patients with acute coronary syndrome. Am Heart J. 2007;154:1116–1122. doi: 10.1016/j.ahj.2007.07.041. [DOI] [PubMed] [Google Scholar]
- 13.Nepal R., Murti A.O., Sayami A. Association between cardiac syndrome X and non-dominant right coronary artery. J Clin Prev Cardiol. 2015;4(3):54–57. [Google Scholar]
- 14.Makarovic Z., Makarovic S., Billic-Curcic I. Sex- dependent association between coronary vessel dominance and cardiac syndrome X: a case–control study. BMC Cardiovasc Disord. 2014;14:142. doi: 10.1186/1471-2261-14-142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gupta T., Saini A., Sahni D. Terminal branching pattern of the right coronary artery in left-dominant hearts: a cadaveric study. Cardiovasc Pathol. 2013;22:179–182. doi: 10.1016/j.carpath.2012.08.001. [DOI] [PubMed] [Google Scholar]
- 16.Attar A., Rezaee M., Kheirkhah J. Left ventricular dysfunction: Neither a matter of atherosclerosis nor an anomalous originated right coronary artery from left anterior descending artery. ARYA Atheroscler. 2015;11:252–255. [PMC free article] [PubMed] [Google Scholar]
- 17.Maharlooei K.M., Attar A., Goran A., Amuee S., Dehghan A., Monabati A. Hydatid cyst of ovary: a case report. Iran J Med Sci. 2009;34:76–79. [Google Scholar]
- 18.Adler A., Rosso R., Viskin D., Halkin A., Viskin S. What do we know about the “malignant form” of early repolarization? J Am Coll Cardiol. 2013;62:863–868. doi: 10.1016/j.jacc.2013.05.054. [DOI] [PubMed] [Google Scholar]