Abstract
Background
Isolated Coronary artery ectasia (CAE) is considered an uncommon angiographic finding with varying patterns of presentation and carries significant morbidity burden to the patient. Our objective was to evaluate the prevalence of this condition, to analyse its clinical, angiographic, and follow up characteristics.
Patients and methods
Coronary angiography was performed in 4950 patients from January 2009 to August 2014. The epidemiological, clinical, angiographic, and follow up characteristics of 52 patients with isolated CAE were examined.
Results
Of the 4950 angiograms analysed, isolated CAE was found in 52 patients, a prevalence of 1.05 %. The mean age of patients was 53.4 years. A predominance of the male sex was observed (71.1%). Angina on exertion was the most common presenting symptom (61.5%). Single vessel was involved in 61.5%. Left anterior descending artery was the most commonly involved vessel followed by right coronary artery, left circumflex and left main coronary artery. Type IV CAE as per Markis classification was the most common involvement. The median follow-up was 28 ± 20 months, during which 10 patients (19.2%) had recurrent chest pain, and four patients were re-hospitalised, three for unstable angina, one for myocardial infarction.
Conclusion
The prevalence of isolated coronary ectasia was 1.05%. The majority of patients had single vessel involvement, and left anterior descending branch was the most common involved vessel. This condition may not be considered completely benign, as it is associated with atherosclerotic risk factors and occurrence of coronary events including angina and myocardial infarction.
Keywords: Coronary artery disease, Coronary artery angiography, Isolated Coronary artery ectasia
1. Introduction
Coronary artery ectasia (CAE) is a rare, yet well-recognized abnormality of the coronary anatomy. It is defined as dilation of >1.5 times normal adjacent segments of vessels, which can either be localized or diffuse.1
The first case report of this condition was described by Bourgon2 in1812, while the term ectasia was coined by Bjork3 in 1966. The first literature review was published by Packard and Wechsler,4 while Markis et al.5 provided the first prospective evaluation of the incidence of CAE.
Isolated CAE, which excludes atherosclerosis, connective tissue disorders, and other cardiac defects, is very rare with an angiographic frequency of 0.1–0.32%.6, 7
Almost 20–30% of cases of coronary ectasia are congenital and the rest are acquired. Of the acquired cases, 50% are associated with atherosclerosis while 10%–20% are associated with inflammatory and connective tissue diseases, syphilis, and bacterial infections. 8, 9, 10, 11
The clinical symptoms of patients with isolated CAE vary greatly and may include typical angina, atypical angina or myocardial infarction. 12, 13, 14
All three coronary vessels can be ectatic, but an isolated artery is involved in 75% of patients.15 Markis5 classified CAE in four types: type 1 includes diffuse ectasia involving two or three vessels, type 2 includes diffuse ectasia in one vessel and discrete ectasia in another vessel, type 3 includes diffuse ectasia in only one vessel, and type 4 includes localized or segmental ectasia in only one vessel.
Previous studies have shown isolated coronary ectasia not to be completely innocuous condition as half of the patients presents with myocardial infarction (MI) and many have angina. Markis et al.5 found a 15% mortality rate after 7 years, which was similar to the mortality rate of medically treated triple vessel disease.
The evaluation and characterization of isolated coronary ectasia represent a great diagnostic challenge with clinical and therapeutic implications. The present study aims to study the epidemiological, clinical, angiographic, and follow up characteristics of patients with isolated CAE.
2. Subjects and methods
2.1. Study population
The study group consisted of 52 patients found to have isolated coronary ectasia among the 4950 consecutive patients we reviewed, who underwent coronary angiography from January 2009 to August 2014, in the Department of Cardiology, NEIGRIHMS, Meghalaya, India. Indication for coronary angiography was typical angina or chest pain suggestive of angina, atypical chest pain, previous history of MI, and/or a positive exercise test. Patients with concomitant significant coronary artery disease (CAD), history of myocardial revascularisation and valvular heart disease were excluded from the study. The patient clinical characteristics including age, sex, smoking status, diabetes mellitus, dyslipidemia, and hypertension were recorded. Written consents were taken from all the patients. This study has been approved by institutional review committee and institute medical ethical committee.
2.2. Coronary angiography
Coronary angiograms were evaluated by two independent observers to identify the coronary artery anatomy and the presence of any ectasia as well as obstructive lesions in each vessel. Coronary ectasia was defined as dilatation of a coronary artery to 1.5 times or more the normal adjacent coronary segment.5 Isolated CAE was defined as coronary ectasia in absence of concomitant obstructive CAD. Classification proposed by Markis5 was used to describe the type of ectasia. Type I – diffuse ectasia of two or three vessels, Type II- diffuse disease in one vessel and localized disease in another vessel, Type III- diffuse ectasia of one vessel only, Type IV- localized or segmental ectasia.
2.3. Follow up
Follow-up data of the study patients were evaluated retrospectively and prospectively for a mean of 28 ± 20 months. Data on—recurrent chest pain, unstable angina(UA), MI, hospital admission for chest pain and cardiac death were collected from hospital medical records, by clinical examination and by telephone questionnaire.
2.4. Statistical analysis
Continuous variables were expressed as mean ± standard deviation and percentages were used for categorical variables.
3. Results
Among the 4950 coronary angiograms reviewed, 270 patients were found to have coronary ectasia (5.45%). Of them, 52 patients had isolated coronary ectasia (19.19%). Overall the incidence of isolated CAE was 1.05%.
3.1. Clinical characteristics
The mean age was 53.4 years. A predominance of the male sex was seen (71.1%). Hypertension and diabetes were present in 59.6% and 30.7% of total patients,respectively. Smoking and dyslipidemia was present in 38% and 42.3%, respectively. 17.3% of patients had a family history of CAD, and 15.4% had previous history of MI. Two patients (3.8%) had associated abdominal aortic aneurysm. Most patients presented with angina on exertion (61.5%). Exertional dyspnoea was mode of presentation in eleven patients (21%), while nine patients (17%) presented with atypical chest pain. (Table 1).
Table 1.
Baseline Parameters.
| Variable | Patients (n = 52) |
|---|---|
| Age (years) (mean ± SD) |
53.4 ± 2.5 |
| Male, n (%) Female, n (%) |
37 (71.1%) 15 (28.9%) |
| Hypertension,n (%), | 31 (59.6%) |
| Diabetes, n (%) | 16 (30.7%) |
| Smoking, n (%) | 20 (38%) |
| Dyslipidemia, n (%) | 22 (42.3%) |
| F/H of CAD, n (%) | 9 (17.3%) |
| History of MI, n (%) | 8 (15.4%) |
| Aortic Aneurysm, n (%) | 2 (3.8%) |
Abbreviations: F/H = family history, CAD = coronary artery disease, MI = Myocardial Infarction.
3.2. Angiographic characteristics
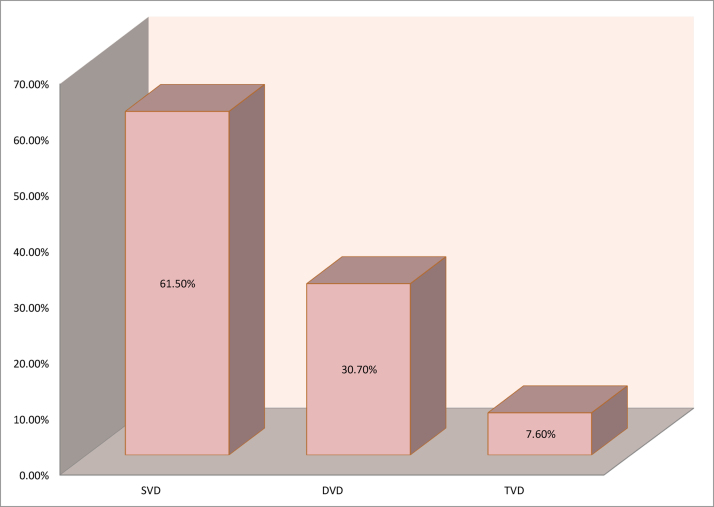
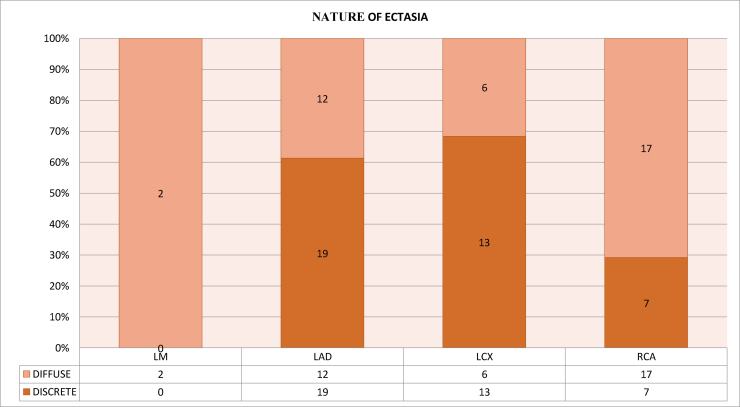
Ectasia affected single vessel in 61.5%, double vessel in 30.7%, and triple vessel in only 7.6% (Fig. 1). The frequency of arterial involvement, in descending order was: left anterior descending artery (LAD) in 59.6%, right coronary artery (RCA) in 46.1%, left circumflex artery (LCX) in 36.5% and left main (LM) in 3.8% (Table 2). Out of total 76 lesions, discrete ectasia was found in 51.31%, and diffuse ectasia in 48.68%. Diffuse ectasia was seen more in RCA, whereas discrete ectasia was more common in LAD (Fig. 2).
Fig. 1.
vessel involvement.
Table 2.
Involvement of coronaries.
| Artery | n,% |
|---|---|
| LAD | 31 (59.6%) |
| RCA | 24 (46.1%) |
| LCX | 19 (36.5%) |
| LM | 2 (3.8%) |
Abbreviations: LAD – left anterior descending artery, RCA – right coronary artery, LCX – left circumflex artery, LM – left main.
Fig. 2.
Nature of ectasia.
Using the Markis5 classification of coronary ectasia, type IV ectasia was most common (51.92%), followed by type II (26.92%), type I (11.53%) and type III (9.61%), (Table 3).
Table 3.
Types of ectasia.
| Type | No. of Patients | Percentage (%) |
|---|---|---|
| I | 6 | 11.53 |
| II | 14 | 26.92 |
| III | 5 | 9.61% |
| IV | 27 | 51.92% |
3.3. Follow up characteristics
The mean follow up period was 28 ± 20 months. Out of 52 patients, 38 patients were asymptomatic, 10 patients (19.2%) had recurrent chest pain, 3 patients (5.7%) had unstable angina, and 1 patient (1.9%) had MI (Table 4).
Table 4.
Follow-up characteristics of study population.
| Follow Up (mean ± SD) |
28 ± 20 months (N = 52) |
|---|---|
| Total events, n,% | 14/52 (26.9%) |
| Recurrent chest pain, n,% | 10 (19.2%) |
| UA, n,% | 3 (5.7%) |
| MI, n,% | 1 (1.9%) |
| Heart Failure, n | 0 |
| Arrhythmias, n | 0 |
| Death, n | 0 |
Abbreviation; UA = Unstable Angina, MI = Myocardial Infarction.
4. Discussion
Coronary artery ectasia is considered an uncommon angiographic finding. Incidence varies from 0.3 to 4.9% in the general population.16 In the three studies of ectasia from India, the incidence reported were 3.9% (1042 patients), 10.2% (185 patients) and 5.6% (300 patients) respectively.17, 18, 19 In our study the incidence of CAE was 5.45%.
Isolated CAE, in absence of coronary stenosis and other heart diseases, is rare, occurring in 0.1–0.32% of patients according to angiographic measurements.6, 7 According to Al-Harthi et al.20 the incidence of isolated CAE is 0.1–0.79%. In present study the incidence of isolated CAE was found to be 1.05%.
Male sex was predominant (71.1%), which was consistent with the results of CASS registry.7 Age does not have any additional influence according to most investigators.15, 21 In the present study mean age was 53.4 years.
Markis et al.5 had noted a higher incidence of hypertension, in the present study the incidence was 59.6%. Hypercholesterolemia was suggested as a predisposing factor, as one study showed increased prevalence of ectasia in familial hypercholesterolemia patients.21 In our study 42.3% patients were dyslipidemic.
The incidence of diabetes, smoking and family history of CAD, is consistent with previous study by Cheng et al.22
In the present study abdominal aortic aneurysm was found in only 3.8%, which defers from previously reported strong association with aortic aneurysms.23
Demopoulos et al.15 found an incidence of previous MI in the isolated CAE group to be 38.7%, which is much higher than in the present study (15.7%).
In the present study, majority of patients presented with angina. Previous studies5, 13 have suggested that coronary ectasia, without significant stenosis may be a cause of angina. The aneurysmal segments produces sluggish blood flow, with increased incidence of angina pectoris and even MI, regardless of the severity of coexisting coronary artery stenosis. This is attributed either to thrombotic occlusion of the aneurysmal vessel or to the repeated dissemination of microemboli to segments distal to the ectasia.20, 24, 25 Slow coronary flow may also be a causative factor.26
The pathophysiology of CAE is unclear. Various hypotheses have been proposed. Celik et al.27 have postulated the role of atherosclerosis in the pathogenesis of isolated CAE, as they have shown increased carotid intima-media-thickness in patients of isolated CAE. Patients with isolated CAE, as compared with CAD and control group, showed higher concentration of soluble ICAM-1 suggesting the presence of a more severe chronic inflammation in the coronary circulation in these patients.28 England et al.29 has reported an increased frequency of CAE in individuals who had been exposed to acetylcholinesterase inhibitors containing herbicide sprays, thus implicating the role of nitric oxide in the pathogenesis of CAE.
In our study we found LAD to be most commonly involved vessel followed by RCA and the LCX, which is different from many previous studies15, 17, 30 but similar to Nyamu et al.31
All three coronary vessels can be affected be ectatic, however in almost 75% of patients an isolated artery is ectatic.20, 23 In the present study single vessel involvement was 61.50%. Ectasia of diffuse nature was predominantly seen in RCA, with LAD showing predominantly the discrete form of ectasia.
In contrast to previous studies,11, 15 in the present study Markis type IV ectasia was most common (51.92%), followed by type II (26.92%), type I (11.53%) and type III (9.61%).
In our study we had a mean follow up period of 28 ± 20 months. Follow up data were obtained for all patients.
Recurrent episodes of chest pain without any dynamic ECG changes or enzyme rises were defined in 19.2% of the patients. This may lead to the conclusion that patients with isolated CAE have a relatively higher risk for angina.
Four patients were re-hospitalised, three for UA and one for MI. The exact pathophysiology of myocardial ischemia in patients with CAE is unknown. Various mechanisms including slow coronary flow and altered-flow dynamics have been implicated. Sayin et al.32 postulated that CAE renders patients to higher risk of myocardial ischemia irrespective of extent of stenosis. Papadakis et al.26 demonstrated that presence of CAE was associated with higher TIMI frame count indicating slower coronary flow, which was later confirmed by Akyurek et al.33 Other possible mechanisms involved are spasm of the dilated arteries and dissection of the vessel wall.
Similar to previous study by Demopoulos15 there was no mortality in the present study. The accurate rate of mortality is unclear yet. In the literature, different CAE mortality rate is reported such as biannually 15%, and annually 1.5% in medically treated patients.5, 3
However, Demopoulos et al.15 reported good prognosis for isolated CAE despite history of previous MI. According to CASS study, there is no survival difference between patients with or without CAE.7
The medical management of patients with ectatic vessels has not been adequately addressed. Some investigators recommended long-term anticoagulation therapy34, 35 while others recommended only aspirin in asymptomatic individuals. Nitrates have been shown to exacerbate myocardial ischemia by causing, further coronary artery dilation, and are discouraged in patients with isolated CAE.12
This study has some limitations. First, the number of patients was relatively small and a larger study is needed to reach a major conclusion. Second, lack of suitable control group. Third, data on drugs received by the patients and the impact of the drugs on clinical outcomes was not available.
5. Conclusion
The present study was a retrospective analysis of angiograms reported to have ectasia, with prospective follow up aimed at determining the incidence of specific cardiac events. Our study shows a relatively high angiographic prevalence of isolated coronary ectasia. LAD was the most commonly involved vessel by ectasia followed by RCA, LCX and LM coronary artery. Coronary ectasia without flow-limiting coronary artery disease may not be completely innocuous, since there is an association with angina and MI.
To conclude, isolated CAE is an important clinical condition requiring aggressive risk stratification.
Conflict of interest
None to declare.
References
- 1.Yilmaz H., Sayar N., Yilmaz M. Coronary artery ectasia: clinical and angiographical evaluation. Turk Kardiyol Dern Ars. 2008;36:530–535. [PubMed] [Google Scholar]
- 2.Bourgon A. Biblioth Med. 1812;37:183. cited in Packard M, Wechsler HF: Aneurysm of the coronary arteries, Arch Intern Med. 1929;43:1–14. [Google Scholar]
- 3.Bjork L. Ectasia of the coronary arteries. Radiology. 1996;87:33–34. doi: 10.1148/87.1.33. [DOI] [PubMed] [Google Scholar]
- 4.Packard M., Wechsler H.F. Aneurysm of the coronary arteries. Arch Intern Med. 1929;43:1–14. [Google Scholar]
- 5.Markis J.E., Joffe C.D., Cohen P.F. Clinical significance of coronary arterial ectasia. Am J Cardiol. 1976;37:217–222. doi: 10.1016/0002-9149(76)90315-5. [DOI] [PubMed] [Google Scholar]
- 6.Hartnell G.G., Parnell B.M., Pridie R.B. Coronary artery ectasia. Its prevalence and clinical significance in 4,993 patients. Br Heart J. 1985;54(4):392–395. doi: 10.1136/hrt.54.4.392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Swaye P.S., Fisher L.D., Litwin P. Aneurysmal coronary artery disease. Circulation. 1983;67(1):134–138. doi: 10.1161/01.cir.67.1.134. [DOI] [PubMed] [Google Scholar]
- 8.Sultana R., Sultana N., Ishaq M. The prevalence and clinical profile of angiographic coronary ectasia. J Pak Med Assoc. 2011;61(4):372–375. [PubMed] [Google Scholar]
- 9.Aksu T., Uygur B., Kosar M.D. Coronary artery ectasia: its frequency and relationship with atherosclerotic risk factors in patients undergoing cardiac catheterization. Anadolu Kardiyol Derg. 2011;11(4):280–284. doi: 10.5152/akd.2011.076. [DOI] [PubMed] [Google Scholar]
- 10.Pinar Bermúdez E., López Palop R., Lozano Martínez-Luengas I. Coronary ectasia: prevalence, and clinical and angiographic characteristics. Revista Española de Cardiologia. 2003;56(5):473–479. doi: 10.1016/s0300-8932(03)76902-4. [DOI] [PubMed] [Google Scholar]
- 11.Harikrishnan S., Krishnakumar N., Jaganmohan T. Coronary artery ectasia–is it time for reappraisal? Clin Cardiol. 2007;30(10):536. doi: 10.1002/clc.20216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Krüger D., Stierle U., Herrmann G. Exercise-induced myocardial ischemia in isolated coronary artery ectasias and aneurysms (‘dilated coronopathy’) J Am Coll Cardiol. 1999;34:1461–1470. doi: 10.1016/s0735-1097(99)00375-7. [DOI] [PubMed] [Google Scholar]
- 13.Befeler B., Aranda M.J., Embi A. Coronary artery aneurysms: study of their etiology, clinical course and effect on left ventricular function and prognosis. Am J Med. 1977;62:597–607. doi: 10.1016/0002-9343(77)90423-5. [DOI] [PubMed] [Google Scholar]
- 14.Rath S., Har-Zahav Y., Battler A. Fate of non-obstructive aneurysmatic coronary artery disease: angiographic and clinical follow-up report. Am Heart J. 1985;109:785–791. doi: 10.1016/0002-8703(85)90639-8. [DOI] [PubMed] [Google Scholar]
- 15.Demopoulos V., Olympios C., Fakiolas C. The natural history of aneurysmal coronary artery disease. Heart. 1997;78:136–141. doi: 10.1136/hrt.78.2.136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Manginas A., Cokkinos D.V. Coronary artery ectasias: imaging, functional assessment and clinical implications. Eur Heart J. 2006;2(2):1026–1031. doi: 10.1093/eurheartj/ehi725. [DOI] [PubMed] [Google Scholar]
- 17.Bhargava M., kaul U.A., Bhat A. Prevalence and clinical significance of coronary artery ectasia (An angiographic study) Indian Heart J. 1989;41(5) [PubMed] [Google Scholar]
- 18.Krishnaswami S., Sathyamurthi I., Uthaman C.B. Angiographic pattern of CAD. IHJ. 1983;35:200–203. [PubMed] [Google Scholar]
- 19.Krishnaswami S., Abraham T.M., Sukumar I.P. Ectasia of coronary arteries. IHJ. 1980;30:342–345. [PubMed] [Google Scholar]
- 20.Al-Harthi S.S., Nouh M.S., Arafa M. Aneurysmal dilatation of the coronary arteries: diagnostic patterns and clinical significance. Int J Cardiol. 1991;30:191–194. doi: 10.1016/0167-5273(91)90094-6. [DOI] [PubMed] [Google Scholar]
- 21.Sudhir K., Ports T., Amidon T. Increased prevalence of coronary ectasia in heterozygous familial hypercholesterolemia. Circulation. 1995;91:1375–1380. doi: 10.1161/01.cir.91.5.1375. [DOI] [PubMed] [Google Scholar]
- 22.Zhongwei Cheng, Yingxian Liu, Shuyang Zhang. Clinical characteristics and coronary features of coronary ectasia and aneurysm in China. World J Cardiovasc Dis. 2013;3:18–21. [Google Scholar]
- 23.Daoud A.S., Pankin D., Tulgan H. Aneurysms of the coronary artery-report of ten cases and review of literature. Am J Cardiol. 1963;11:228–237. doi: 10.1016/0002-9149(63)90064-x. [DOI] [PubMed] [Google Scholar]
- 24.Rab S.T., Smith D.W., Alimurung B.N. Thrombolytic therapy in coronary ectasia and acute myocardial infarction. Am Heart J. 1990;119:955–957. doi: 10.1016/s0002-8703(05)80338-2. [DOI] [PubMed] [Google Scholar]
- 25.La Mendola C.L., Culliford A.T., Harris L.J. Multiple aneurysms of the coronary arteries in a patient with systemic aneurysmal disease. Ann Thorac Surg. 1990;49:1009–1010. doi: 10.1016/0003-4975(90)90892-a. [DOI] [PubMed] [Google Scholar]
- 26.Papadakis M.C., Manginas A., Cotileas P. Documentation of slow coronary flow by the TIMI frame count in patients with coronary ectasia. Am J Cardiol. 2001;88:1030–1032. doi: 10.1016/s0002-9149(01)01984-1. [DOI] [PubMed] [Google Scholar]
- 27.Celik S., Erdogan T., Kasap H. carotid intima-media thickness in patients with isolated coronary artery ectasia. Atherosclerosis. 2017;190(2):385–387. doi: 10.1016/j.atherosclerosis.2006.02.015. [DOI] [PubMed] [Google Scholar]
- 28.Daoud Eid Mohamed, Abdelaziz Ayman Ahmed, Hassan Nahed Abdallah. Isolated coronary artery ectasia debate: inflammation versus atherosclerosis. Egypt Heart J. 2012;64:185–190. [Google Scholar]
- 29.England J.F. Herbicides and coronary artery ectasia. Med J Aust. 1981;1:140. doi: 10.5694/j.1326-5377.1981.tb135392.x. [DOI] [PubMed] [Google Scholar]
- 30.Syed Mushabbar, Lesch Michael. Coronary artery aneurysm: a review. Prog Cardiovasc Dis. 1997;40(1):77–84. doi: 10.1016/s0033-0620(97)80024-2. [DOI] [PubMed] [Google Scholar]
- 31.Nyamu Peter, Ajit Mullasari S., Joseph Peter K. The prevalence and clinical profile of angiographic coronary ectasia. Asian Cardiovasc Thorac Ann. 2003;11:122–126. doi: 10.1177/021849230301100207. [DOI] [PubMed] [Google Scholar]
- 32.Sayin T., Doven O., Berkalp B. Exercise-induced myocardial ischemia in patients with coronary artery ectasia without obstructive coronary artery disease. Int J Cardiol. 2001;78(2):143–149. doi: 10.1016/s0167-5273(01)00365-5. [DOI] [PubMed] [Google Scholar]
- 33.Akyurek O., Berkalp B., Sayin T. Altered coronary flow properties in diffuse coronary artery ectasia. Am Heart J. 2003;145(1):66–72. doi: 10.1067/mhj.2003.48. [DOI] [PubMed] [Google Scholar]
- 34.Sadr Ameli M., Sharifi M. The natural history of ectatic coronary artery disease. Iran Heart J. 2001;2(1):12–16. [Google Scholar]
- 35.Fukuhara S., Takase E., Fujimoto T. Coronary ectasia resulting in thrombotic coronary occlusion after warfarin interruption: a case report. J Cardiol. 2005;46:195–200. [PubMed] [Google Scholar]