Abstract
Objectives
Spouses of older adults with functional disability often provide help with their partner’s medical care. Yet little is known about the implications of these activities for spouses’ caregiving experiences. We examined how spouses’ medical care activities are linked to both positive and negative aspects of caregiving (difficulties and gains), and whether these associations vary by their age, gender, and education.
Design
Retrospective analysis of data from the 2011 National Health and Aging Trends Study (NHATS) and National Study of Caregiving (NSOC) cross-sectional studies.
Setting
Caregivers and care recipients/proxies were interviewed by telephone at home.
Participants
Nationally representative US sample of 345 spousal caregivers and their community-dwelling care recipients aged 65 and older.
Measurements
Caregivers’ self-reported sociodemographics, care activities, health conditions, well-being, and support resources. Care recipients (or proxies) reported on their health conditions and dementia status.
Results
A higher number of health system interaction tasks (e.g., making appointments) were significantly associated with greater emotional caregiving difficulties, whereas a higher number of medical/nursing tasks (e.g., giving shots/injections) were significantly linked to greater caregiving gains. A higher number of medical/nursing tasks were also significantly associated with greater physical difficulties for caregiving wives and spouses with less education.
Conclusions
Medical care activities may have both positive and negative consequences for spousal caregivers, which depend partly on sociodemographics. This study underscores the importance of ensuring that spouses have the resources and support needed to provide complex care to their partners.
Keywords: caregivers, late-life disability, medical care, spouse
Objective
The unpaid assistance provided by family caregivers is critical for supporting persons with late-life disability so they can remain in their communities.1,2 In addition to personal care and household chores, family members commonly assist with medical care tasks.1–4 Medical care activities require a range of skills, from interacting with healthcare systems to providing care traditionally performed by medical/nursing professionals. Help with these tasks may persist for years, particularly among caregivers of older adults with chronic conditions (e.g., stroke) that require prolonged home-based care.5 Medical care activities are often complicated and may be stressful; however their implications for caregivers are largely unknown.
Spouses appear especially likely to help with medical care activities. Roughly two-thirds (65%) of caregiving spouses perform tasks including wound care and medication management, compared to 42% of non-spouse caregivers.3 Spouses may view these activities as part of their marital commitment; but they may also lack the resources to effectively provide this care. Relative to non-spouse caregivers, caregiving spouses tend to be older and have less education, lower incomes, poorer health, and fewer sources of support.3,6–8 Strikingly, more than half of caregiving spouses (58%) report no help in handling care responsibilities.3 Moreover, only 37% of spouses helping with medical care activities receive instruction in managing these tasks.3 Difficulties in performing medical care activities may expose care recipients to reduced quality of care that presents a serious health risk. Given spouses’ high engagement in medical care activities along with the vulnerabilities of both care partners, it is imperative to determine how these tasks may impact positive and negative caregiving experiences.
This study utilized a nationally representative US sample of spouses caring for community-dwelling older adults from the 2011 National Health and Aging Trends Study (NHATS) and National Study of Caregiving (NSOC) to examine two types of medical care activities (health system interaction tasks and medical/nursing tasks) and their associations with caregiving difficulties and gains. We also considered whether these links differed by caregivers’ age, gender, and education.
Stress process theorists propose that caring for an impaired older person is a chronic source of stress that may contribute to emotional and physical problems.9,10 Indeed, care-related stressors (e.g., care tasks) are associated with elevated burden, greater psychological distress, and poorer physical health.5,7,11–13 Prior work has placed a near-exclusive emphasis on two types of tasks: assistance with activities of daily living (ADLs) and instrumental activities of daily living (IADLs). ADLs encompass personal care (e.g., bathing, dressing) and mobility, whereas IADLs include household chores (e.g., shopping, paying bills). Although these activities are important elements of caregiving, they fail to capture the full spectrum of tasks that are central to many caregivers’ lives.3
Examining medical care activities and their associations with care-related outcomes would add to a more complete understanding of caregiving. It was recently reported that caregivers helping with both care coordination (e.g., speaking with physicians) and medication management have an increased risk of emotional and physical caregiving difficulties relative to caregivers who do not combine these tasks.2 Yet it remains unclear whether various types of medical care activities may have different implications for caregiving experiences.
Considering the broad range of medical care activities, it may useful to evaluate them using the distinctions outlined by Spillman and colleagues.4 Health system interaction tasks involve contact with healthcare providers and systems (e.g., scheduling appointments), whereas medical/nursing tasks involve nursing care in accord with medical recommendations (e.g., foot care). While both tasks can be time consuming and stressful,3 medical/nursing tasks are likely to be more physically and cognitively demanding. Many of these tasks require frequent monitoring and specialized skills for which spouses may not have received training.3 Spouses may also experience strain from worrying about making a mistake or viewing these tasks as embarrassing for their partner.3 Hence, spouses’ medical/nursing tasks may be more strongly linked to adverse caregiving experiences than health system interaction tasks.
Along with caregiving stress, spouses may derive care-related gains.14–20 Caregiving gains are distinct from difficulties and include benefits such as confidence in one’s capabilities and feeling closer to the care recipient.15–18,20 An understudied possibility is that care-related stressors may diminish positive aspects of caregiving.21 It is therefore plausible that spouses’ greater engagement in medical care activities may be linked to fewer caregiving gains.
In accord with the stress process framework, caregivers’ background characteristics play a role in determining the extent to which care-related stressors are linked to emotional and physical problems.9,10 These characteristics reflect exposure to stressors and the availability of coping resources. Older caregivers, for example, tend to have poorer health than younger caregivers, possibly due to a reduced physical capacity to provide care.7 Likewise, caregivers with less education report worse health and higher depressive symptoms than their more educated counterparts, in part because they face more stressors unrelated to caregiving and have fewer resources to manage stress.7,22 Regarding gender, caregiving women typically report greater burden and poorer mental and physical health than caregiving men.2,23–25 These differences may be partly explained by more intense care-related stressors (e.g., care tasks) and fewer resources (e.g., help with care tasks) among caregiving women.23,25
This study had two major aims. First, we evaluated the associations between spouses’ medical care activities and perceived caregiving difficulties and gains. We predicted the following: (1) a higher number of health system interaction tasks and medical/nursing tasks would be linked to greater emotional and physical caregiving difficulties; (2) A higher number of health system interaction tasks and medical/nursing tasks would be linked to fewer caregiving gains; and (3) These associations would be especially salient for medical/nursing tasks. Second, we determined the moderating role of sociodemographics. We predicted that associations in this study would be significantly stronger for spouses who are older, female, and less educated.
Methods
Sample and Procedures
The sample included 345 community-dwelling adults aged 65 and older and their spousal caregivers drawn from the 2011 National Health and Aging Trends Study (NHATS) and National Study of Caregiving (NSOC). In accord with the University of Michigan’s policies, ethical approval for this study was not required because we used publicly available secondary data with no individual identifiers.
Participants were eligible for NHATS if they were Medicare enrollees aged 65 and older, lived in the contiguous US, and received health-related assistance in the past month with mobility, personal care, and/or household chores. Participants were recruited from a Medicare enrollment database using a stratified three-stage sampling design, with the oldest age groups and Black non-Hispanic persons oversampled. In total, 14,643 enrollees were sampled. Of 12,411 enrollees released to the field, 8,245 (71%) were interviewed.26
NHATS participants were eligible for NSOC if they had at least one family or unpaid non-family helper who provided health-related assistance with mobility, self-care, household chores, and/or medical care activities. The 2,423 NHATS participants who were eligible for NSOC had 4,935 eligible caregivers. Contact information was provided for 3,362 (68.1%) caregivers, of whom 2,007 (59.7%) completed a 30-min telephone interview.
Of the 2,007 caregivers who participated in NSOC, 422 were spouses. We were interested in caregiving spouses who share a household with their partner, and so we removed 32 spouses with care recipient living in residential care and two spouses who did not live with the care recipient. In total, 388 spouses resided with the care recipient. Of these, 43 were removed due to missing data on study variables. This widely used method for addressing missing data is the simplest approach and appropriate given our relatively large sample size and small number of incomplete responders.27 Thus, we focused on 345 spousal caregivers and care recipients with complete data (see Table 1 for background characteristics and scores on key variables). Spouses were in heterosexual marriages, with the exception of one caregiving wife in a same-sex marriage. On average, couples had been married for 43.05 years (SD = 17.85, range = 0 – 72).
Table 1.
Background Characteristics of Spousal Caregivers
| Caregivers (N = 345) |
|
|---|---|
| Characteristic | M (SD) |
| CG Age in years | 73.39 (9.00) |
| CR Age in years | 76.88 (7.50) |
| CG Chronic conditions | 2.09 (1.42) |
| CG Psychological well-being | 3.41 (0.57) |
| CG ADL/IADL assistance | 5.15 (2.47) |
| CG Service use | 0.23 (0.51) |
| CR Chronic conditions | 3.05 (1.46) |
| CG Health system tasks | 2.57 (1.65) |
| CG Medical/nursing tasks | 2.48 (2.02) |
| CG Emotional difficulties | 1.31 (1.66) |
| CG Physical difficulties | 1.05 (1.60) |
| CG Gains | 3.54 (0.46) |
|
n (%)
|
|
| CG Gender (female) | 204 (59.1) |
| CR Gender (female) | 142 (41.2) |
| CR Dementia status | 62 (18.0) |
| CG Informal support | 158 (45.8) |
| CG Paid help | 67 (19.4) |
| CG Educational attainment | |
| High school graduate | 106 (30.7) |
| College graduate | 34 (9.9) |
| Post graduate | 24 (7.0) |
| CG Health system tasks | |
| Ordering medication | 233 (67.5) |
| Scheduling appointments | 219 (63.5) |
| Speaking to medical providers | 194 (56.2) |
| Changing/adding insurance plan | 110 (31.9) |
| Other insurance matters | 130 (37.7) |
| CG Medical/nursing tasks | |
| Keeping track of medications | 209 (60.6) |
| Managing medical tasks | 55 (15.9) |
| Giving shots/injections | 51 (14.8) |
| Foot care | 136 (39.4) |
| Caring for skin wounds/sores | 132 (38.3) |
| Caring for teeth/dentures | 64 (18.6) |
| Helping with exercises | 96 (27.8) |
| Helping with special diet | 113 (32.8) |
Measures
Medical care activities
Health system interaction tasks included ordering medication, scheduling appointments, speaking to providers, helping to change/add insurance or drug plans, and other medical insurance matters. Medical/nursing tasks included giving shots/injections, caring for skin wounds/sores, caring for teeth/dentures, foot care (e.g., clipping nails), managing medical tasks (e.g., ostomy care, IVs, testing blood), monitoring medications, helping with prescribed exercises, and assisting with a special diet. Caregivers reported whether they performed each task (1 = yes, 0 = no). Summed scores were created for health system interaction tasks (range = 0 – 5) and medical/nursing tasks (range = 0 – 8).
Caregiving difficulties
Caregivers were separately asked whether they experienced (a) emotional; and (b) physical care-related difficulties (1 = yes, 0 = no). Caregivers who reported either type of difficulties then indicated their extent from 1 (a little difficult) to 5 (very difficult). We combined these items such that caregivers who did not report difficulties were assigned a zero and those who reported difficulties received a score based on their degree (0 = no difficulty to 5 = high difficulty). Mean scores were determined for emotional and physical difficulties.
Caregiving gains
On a scale from 1 (not so much) to 4 (very much), caregivers reported how much caregiving has: (a) made them more confident about their abilities; (b) taught them to deal with difficult situations; (c) brought them closer to their partner; and (d) given them satisfaction that their partner receives good care. Mean total scores were calculated (α = .68).
Caregiver sociodemographics
We considered caregivers’ age, gender (1 = female, −1 = male), and educational attainment (1 = no schooling completed to 9 = masters, professional, or doctoral degree).
Covariates
We controlled for caregivers’ self-reported ADLs and IADLs during which they helped care recipients. ADLs included bathing, dressing, eating, toileting, getting in/out of bed, and mobility inside/outside the house. IADLs included laundry, shopping, preparing meals, banking, and managing money. Summed scores were created for total ADL/IADL assistance (range = 0 – 12).
We controlled for caregivers’ self-reported number of chronic conditions: arthritis, cancer, diabetes, heart disease, hypertension, lung disease, and osteoporosis. Additionally, we adjusted for caregivers’ psychological well-being. Caregivers indicated the extent to which they: (a) felt confident and good about themselves; (b) liked their living situation; (c) have an easy time adjusting to change; and (d) felt their life has meaning and purpose. Responses ranged from 1 (disagree strongly) to 4 (agree strongly), and mean scores were calculated (α = .62).
We also controlled for caregivers’ support resources. Informal support was determined from caregivers’ availability of friends or relatives who help with care tasks (1 = had informal support, -1 = did not have informal support). Support service use included caregivers’ use of three services in the last year: (a) a caregiver support group; (b) respite services; and (c) training to help with care tasks. Summed scores were created. Paid help was assessed with one item asking whether caregivers had found a paid helper in the past year (1 = used paid help, −1 = did not use paid help).
We controlled for care recipients’ impairment from self-reports (n = 298) or proxy reports (n = 45 spouses; n = 1 adult daughter; n = 1 adult son) of diagnosed dementia (1 = dementia, −1 = no dementia) and number of chronic conditions: arthritis, cancer, diabetes, heart disease, hypertension, lung disease, osteoporosis, and stroke.
Statistical Analysis
We estimated hierarchical regression models, which permitted examination of the amount of variance in the outcome that is explained with each step of the model. In the first step, we entered covariates along with caregivers’ age, gender, and education. We added health system interaction tasks and medical/nursing tasks in the second step to examine their independent links to caregiving outcomes. In the third step, we entered an interaction term (e.g., Health System Interaction Tasks × Caregiver Age) to determine whether associations differed by caregivers’ age, gender, and education. Interaction terms were analyzed separately. Continuous variables were mean centered. To probe the significant moderating effects, we analyzed simple slopes using two-way interaction plots from the following website: http://www.jeremydawson.co.uk/slopes.htm. We estimated slopes for caregiving wives and husbands to examine gender differences. For age and education, the statistical significance of links between medical care activities and caregiving outcomes was evaluated at one standard deviation above and below the moderator mean to represent high and low values, respectively.28 Models were estimated in SAS 9.4 and used the NSOC analytic weight with statistical procedures to account for nonresponse and differential probability of sample selection.29
Results
Bivariate associations between study variables were examined in preliminary analyses (Table 2). Compared with husbands, wives reported significantly more emotional (t(342.55) = 5.64, p < .001) and physical (t(340.83) = 5.57, p < .001) caregiving difficulties; but there were no gender differences for caregiving gains (t(343) = 0.97, p =.33). Wives reported significantly more health system interaction tasks (t(343) = 4.30, p < .001) and medical/nursing tasks (t(329.89) = 4.65, p < .001) than husbands.
Table 2.
Pearson Correlations Among Key Study Variables for Spousal Caregivers
| Variable | 1 | 2 | 3 | 4 | 5 | 6 | 7 |
|---|---|---|---|---|---|---|---|
| 1. Age | |||||||
| 2. Gender (female) | −.24*** | ||||||
| 3. Educational attainment | .12* | −.11* | |||||
| 4. Health system tasks | −.04 | .23*** | .05 | ||||
| 5. Medical/nursing tasks | −.13* | .24*** | −.14** | .52*** | |||
| 6. Emotional difficulties | −.07 | .28*** | .11* | .28*** | .22*** | ||
| 7. Physical difficulties | −.02 | .27*** | .03 | .26*** | .29*** | .54*** | |
| 8. Caregiving gains | .01 | .05 | −.20*** | .05 | .22*** | −.13* | −.01 |
Note. N = 345 spousal caregivers.
p ≤ .05.
p ≤ .01.
p ≤ .001.
Table 3 presents the hierarchical regression models. To adjust for multiple comparisons, we used a Bonferroni correction (α/n, where α = .05 and n = 3 models) such that p values less than or equal to .02 were considered statistically significant.
Table 3.
Associations Between Spousal Caregivers’ Medical Care Activities and Caregiving Outcomes
| Predictor | Emotional Caregiving Difficulties | Physical Caregiving Difficulties | Caregiving Gains | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||||
| B(SE) | β | t | df | B(SE) | β | t | df | B(SE) | β | t | df | |
| Step 2 | ||||||||||||
| CG Health system tasks | .15(.05)** | .15 | 2.81 | 56 | .09(.06) | .10 | 1.48 | 56 | −.03(.02) | −.09 | −1.27 | 56 |
| CG Medical/nursing tasks | −.06(.04) | −.07 | −1.35 | 56 | .01(.06) | .01 | 0.13 | 56 | .07(.02)*** | .29 | 3.85 | 56 |
| ΔR2 | .02 | .01 | .05 | |||||||||
| Step 3 | ||||||||||||
| Health system tasks × Gender | .02(.05) | .02 | 0.38 | 56 | .06(.05) | .06 | 1.22 | 56 | .01(.02) | .04 | 0.53 | 56 |
| ΔR2 | .000 | .004 | .001 | |||||||||
| Health system tasks × Education | −.002(.03) | −.004 | −0.06 | 56 | −.05(.04) | −.11 | −1.34 | 56 | .01(.01) | .04 | 0.58 | 56 |
| ΔR2 | .000 | .01 | .001 | |||||||||
| Medical/nursing tasks × Gender | .03(.05) | .04 | 0.71 | 56 | .12(.05)* | .15 | 2.50 | 56 | −.01(.01) | −.02 | −0.38 | 56 |
| ΔR2 | .001 | .02 | .000 | |||||||||
| Medical/nursing tasks X Education | .04(.02) | .09 | 1.63 | 56 | −.07(.02)** | −.16 | −2.69 | 56 | .01(.01) | .09 | 1.33 | 56 |
| ΔR2 | .01 | .03 | .01 | |||||||||
| Total R2 | .31 – .32 | .25 –.27 | .18 | |||||||||
Note. CG = caregiver. In Step 1, models controlled for caregiver age, gender, educational attainment, chronic conditions, psychological well−being, assistance with activities of daily living and instrumental activities of daily living (ADL/IADL), informal support, paid help, and service use. Models also controlled for care recipient dementia status and chronic conditions. Interaction terms in Step 3 were analyzed separately. Age was not a significant moderator for any of the outcomes (analysis not shown). Degrees of freedom accounted for the sampling design. N = 345 spousal caregivers.
p ≤ .02.
p ≤ .01.
p ≤ .001.
Associations Between Medical Care Activities and Caregiving Outcomes
Caregiving difficulties
As shown in Table 3 , a higher number of health system interaction tasks were significantly linked to greater emotional difficulties (B = .15, β = .15, t = 2.81, df = 56, p = .01, 95% CI [.04, .25]). Therefore, each additional health system interaction task increased scores for emotional caregiving difficulties by .15 (on a scale from 0 – 5).
The link between medical/nursing tasks and physical difficulties was moderated by caregiver gender (B = .12, β = .15, t = 2.50, df = 56, p = .02, 95% CI [.02, .21]) and education (B = −.07, β = −.16, t = −2.69, p = .01, df = 56, 95% CI [−.11, −.02]); but the simple slopes were not significant in the full models. Reduced models controlling for sociodemographics and both care partners’ health conditions revealed that a higher number of medical/nursing tasks were linked to greater physical difficulties for wives (B = .17, β = .22, t = 2.36, df = 56, p = .02, 95% CI [.02, .32]) but not for husbands (B = −.04, β = −.05, t = −0.55, df = 56, p = .59, 95% CI [−.17, .09]) and that more medical/nursing tasks were linked to greater physical difficulties when caregivers’ education was low (B = .21, β = .27, t = 2.79, df = 56, p = .01, 95% CI [.06, .36]) rather than high (B = −.06, β = −.07, t = −0.71, df = 56, p = .48, 95% CI [−.21, .10]) (Figure 1). In other words, each additional medical/nursing task increased scores for physical caregiving difficulties by .17 for wives and by .21 for spouses with lower education (on a scale from 0 – 5).
Figure 1.
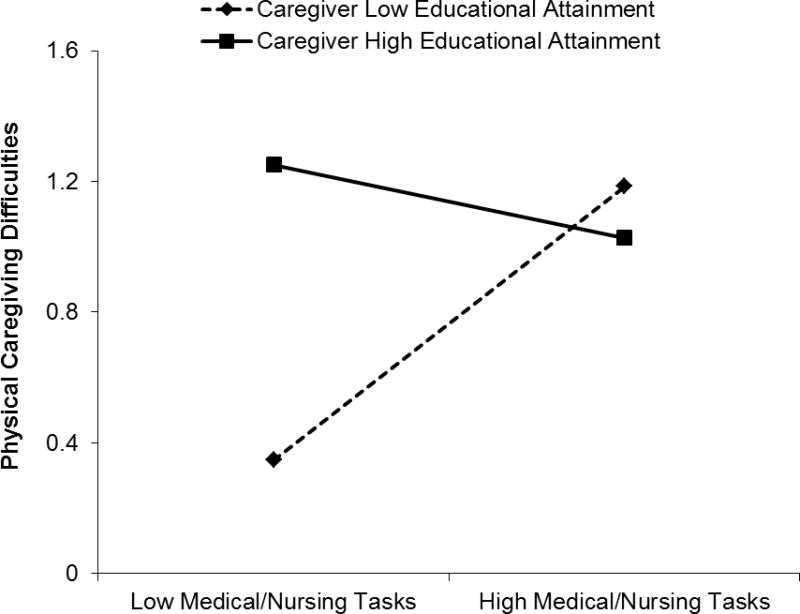
The moderating effect of caregivers’ educational attainment on the association between medical/nursing tasks and physical caregiving difficulties.
Caregiving gains
Table 3 shows that a higher number of medical/nursing tasks were significantly associated with greater caregiving gains (B = .07, β = .29, t = 3.85, df = 56, p < .001, 95% CI [.03, .10]). Hence, each additional medical/nursing task increased scores for gains by .07 (on a scale from 1 – 4).
Conclusions
This study builds upon the literature by examining medical care activities and their associations with spouses’ positive and negative perceptions of caregiving. Spouses who reported a higher number of health system interaction tasks had greater emotional care-related difficulties, whereas spouses with a higher number of medical/nursing tasks perceived more caregiving gains. Caregivers’ age did not moderate the associations in this study, but their gender and education each played significant moderating roles. Overall, the findings indicate that although medical care activities are likely to be stressful for many caregivers, these tasks may also be a source of personal gains.
A higher number of health system interaction tasks were linked to greater emotional caregiving difficulties, regardless of age, gender, or education. Interacting with health systems may be frustrating and/or highly impersonal in ways that are emotionally taxing (e.g., calling automated systems to schedule appointments; feeling as if one is getting the “run around” in trying to coordinate care between providers). Health system interaction tasks are also relatively passive and involve little direct control, which may heighten spouses’ distress. Supporting this possibility, caregivers’ lower perceived control has been associated with elevated depressive symptoms.30,31
By contrast, more medical/nursing tasks were linked to greater physical caregiving difficulties for wives and less educated spouses. Compared with their male counterparts, caregiving women report poorer physical health6,13,23,32 Helping with medical/nursing tasks requires considerable stamina and strength (e.g. turning or lifting a spouse), and so these tasks may be more physically challenging for wives. Gender differences in caregiving styles may also partly explain these findings. Men tend have a managerial approach to caregiving that features delegating tasks to other helpers.33 This approach may help caregiving husbands to preserve their own health, ultimately protecting them from physical care-related difficulties. Finally, husbands may be less willing to report physical caregiving difficulties. Relative to men, women show greater awareness of their health problems34 and are more likely to express difficulties with managing their health.35
Spouses with less education may report greater physical caregiving difficulties when they help with more medical/nursing tasks in part because they encounter more caregiving stressors and non-caregiving stressors (e.g., financial problems, job instability) than spouses with higher education.22,36 One might expect such stressors to intensify emotional care-related difficulties; however they may be especially salient to physical difficulties. Over time, stress contributes to worsening physical health that could diminish spouses’ ability to perform medical/nursing tasks.37 Relatedly, caregivers with lower education have fewer resources to manage stress and maintain health.7,22,36 Less educated spouses may, for instance, have limited access to health care that hinders their long-term physical capacity to assist with medical/nursing tasks. People with lower education also often have poor health habits, which may further reduce their ability to meet caregiving demands.38 There was a rather counterintuitive trend for spouses with higher education to report fewer physical difficulties when they provided more medical/nursing tasks. Highly educated spouses who view caregiving as physically difficult may be less likely to perform these tasks because they are more able to utilize support resources (e.g., paid help).
Unexpectedly, more medical/nursing tasks were linked to greater caregiving gains. This finding is counter to our hypothesis and suggests that, while these tasks may be stressful, they present opportunities for personal growth such as coping successfully with challenges and learning new skills. Performing a higher number of medical/nursing tasks may increase spouses’ exposure to these opportunities, thereby enhancing the positive aspects of caregiving. Contrary to the more passive health system interaction tasks, medical/nursing tasks also involve the provision of active help. Consequently, it is plausible that spouses who assist with more medical/nursing tasks feel they are directly benefitting their partner, which further enhances perceptions of gains. Indeed, providing active help may promote positive feelings among spousal caregivers.39
Strengths of this study include a nationally representative sample, data on medical care activities, and the assessment of positive and negative caregiving outcomes. Our emphasis on medical care activities is timely1,3 and accounts for a more complete picture of caregiving. Medical care activities were shown to be a robust correlate of caregiving difficulties and gains, independent of care recipients’ impairment and caregivers’ sociodemographics, ADL/IADL assistance, health, well-being, and support resources. Moreover, considering sociodemographic moderators sheds light on the conditions under which these activities may be linked to worse caregiving outcomes.
We acknowledge several limitations. First, cross-sectional analyses do not allow us to determine causal associations. Second, on average, spouses reported low caregiving difficulties and high gains. As such, the findings may not generalize to more distressed spouses. Third, the findings may not apply to specific care contexts (e.g., dementia, cancer). Fourth, the effect sizes were small to medium, accounting for 2–5% of the variance in outcomes. Yet even small effects may have a large clinical and public health impact.40 Future research should further investigate the clinical significance of the current findings. This study sets the stage for subsequent work to obtain deeper knowledge regarding for whom and under what conditions medical care activities are linked to spouses’ caregiving difficulties and gains.
The present findings identify wives and less educated spouses as two subgroups of caregivers who may experience particular challenges with medical care activities. Given the physical and emotional vulnerabilities experienced by both subgroups,7,22,23,32 along with estimates that almost half (45%) of caregiving spouses have a high school education or less,3 it is critical to determine ways to best support these caregivers. Future work that explores strategies to maximize gains from medical care activities may also be beneficial. Notably, caregiving gains are linked to reduced caregiver burden and depression,14 better caregiver-care recipient relationship quality,19 and a lower likelihood of nursing home placement.41
In sum, this study implies that health policymakers and providers should proactively consider spouses in the coordination and monitoring of geriatric care.42 Spouses hold a vital and increasingly complex role in sustaining the well-being of persons with late-life disability that should be recognized and supported in innovative care models.
Supplementary Material
Acknowledgments
This work was supported by training grant T32 MH 073553-11 from the National Institute of Mental Health (Stephen J. Bartels, MD, Principal Investigator) and the University of Michigan Program for Positive Aging (Helen C. Kales, MD, Director).
Funding statement
The National Health and Aging Trends Study (NHATS) and National Study of Caregiving (NSOC) are sponsored by the National Institute on Aging (grant number NIA U01AG032947) through a cooperative agreement with the Johns Hopkins Bloomberg School of Public Health.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Disclosures: No disclosures to report.
References
- 1.National Alliance for Caregiving and the American Association of Retired Persons Public Policy Institute. Caregiving in the US. 2015 Available at: http://www.aarp.org/content/dam/aarp/ppi/2015/caregiving-in-the-united-states-2015-report-revised.pdf. Accessed September 25, 2016.
- 2.Wolff JL, Spillman BC, Freedman VA, et al. A national profile of family and unpaid caregivers who assist older adults with health care activities. JAMA Intern Med. 2016;176:372–379. doi: 10.1001/jamainternmed.2015.7664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Reinhard SC, Levine C, Samis S. Family caregivers providing complex chronic care to their spouses. Washington, DC: American Association of Retired Persons and United Hospital Fund; 2014. Available at: http://www.aarp.org/content/dam/aarp/research/public_policy_institute/health/2014/family-caregivers-providing-complex-chronic-care-spouses-AARP-ppi-health.pdf. Accessed September 25, 2016. [Google Scholar]
- 4.Spillman BC, Wolff J, Freedman VA, et al. Informal caregiving for older Americans: An analysis of the 2011 National Study of Caregiving. Washington, DC: US Department of Health and Human Services; 2014. [Google Scholar]
- 5.Gaugler JE. The longitudinal ramifications of stroke caregiving: A systematic review. Rehabil Psychol. 2010;55:108–125. doi: 10.1037/a0019023. [DOI] [PubMed] [Google Scholar]
- 6.Navaie-Waliser M, Feldman PH, Gould DA, et al. When the caregiver needs care: The plight of vulnerable caregivers. J Public Health. 2002;92:409–413. doi: 10.2105/ajph.92.3.409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Pinquart M, Sörenson S. Correlates of physical health of informal caregivers: A meta-analysis. J Gerontol B Psych Sci Soc Sci. 2007;62:126–137. doi: 10.1093/geronb/62.2.p126. [DOI] [PubMed] [Google Scholar]
- 8.Pinquart M, Sörenson S. Spouses, adult children, and children in-law as caregivers of older adults: A meta-analytic comparison. Psychol Aging. 2011;26:1–14. doi: 10.1037/a0021863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Aneshensel CS, Pearlin LI, Mullan JT, et al. Profiles in caregiving The unexpected career. San Diego, CA: Academic Press; 1995. [Google Scholar]
- 10.Pearlin LI, Mullan JT, Semple SJ, et al. Caregiving and the stress process: An overview of concepts and their measures. Gerontol. 1990;30:583–594. doi: 10.1093/geront/30.5.583. [DOI] [PubMed] [Google Scholar]
- 11.Lavela SL, Nazneen A. Psychological health in older adult spousal caregivers of older adults. Chronic Ill. 2010;6:67–80. doi: 10.1177/1742395309356943. [DOI] [PubMed] [Google Scholar]
- 12.Li QP, Mak YW, Loke AY. Spouses’ experience of caregiving for cancer patients: A literature review. Int Nurs Rev. 2013;60:178–187. doi: 10.1111/inr.12000. [DOI] [PubMed] [Google Scholar]
- 13.Vitaliano P, Zhang J, Scanlan JM. Is caregiving hazardous to one’s physical health? A meta-analysis Psychol Bull. 2003;129:946–972. doi: 10.1037/0033-2909.129.6.946. [DOI] [PubMed] [Google Scholar]
- 14.Cohen A, Colantonio A, Vernich L. Positive aspects of caregiving: Rounding out the caregiver experience. Int J Geriatr Psychiatry. 2002;17:184–188. doi: 10.1002/gps.561. [DOI] [PubMed] [Google Scholar]
- 15.Kramer BJ. Gain in the caregiving experience: Where are we? What are we? What next? Gerontol. 1997;37:218–232. doi: 10.1093/geront/37.2.218. [DOI] [PubMed] [Google Scholar]
- 16.Lawton MP, Moss M, Kleban MH, et al. A two-factor model of caregiving appraisal and psychological well-being. J Gerontol. 1991;46:181–189. doi: 10.1093/geronj/46.4.p181. [DOI] [PubMed] [Google Scholar]
- 17.Li Q, Loke AY. The positive aspects of caregiving for cancer patients: A critical review of the literature and directions for future research. Psychooncology. 2013;22:2399–2407. doi: 10.1002/pon.3311. [DOI] [PubMed] [Google Scholar]
- 18.Rapp SR, Chao D. Appraisals of strain and of gain: Effects on psychological wellbeing of caregivers of dementia patients. Aging Ment Health. 2000;4:142–147. [Google Scholar]
- 19.Sánchez-Izquierdo M, Prieto-Ursúa M, Caperos JM. Positive aspects of family caregiving of dependent elderly. Educ Gerontol. 2015;41:745–756. [Google Scholar]
- 20.Riedel SE, Fredman L, Langenberg P. Associations among caregiving difficulties, burden, and rewards in caregivers to older post-rehabilitation patients. J Gerontol B Psych Sci Soc Sci. 1998;53B:165–174. doi: 10.1093/geronb/53b.3.p165. [DOI] [PubMed] [Google Scholar]
- 21.Pinquart M, Sörensen S. Association of stressors and uplifts of caregiving with caregiver burden and depressive mood: A meta-analysis. J Gerontol B Psych Sci Soc Sci. 2003;58:112–128. doi: 10.1093/geronb/58.2.p112. [DOI] [PubMed] [Google Scholar]
- 22.Brodaty H, Thomson C, Thompson C, et al. Why caregivers of people with dementia and memory loss don’t use services. Int J Geriatr Psychiatry. 2005;20:537–546. doi: 10.1002/gps.1322. [DOI] [PubMed] [Google Scholar]
- 23.Pinquart M, Sörenson S. Gender differences in caregiver stressors, social resources, and health: An updated meta analysis. J Gerontol B Psych Sci Soc Sci. 2006;61:33–45. doi: 10.1093/geronb/61.1.p33. [DOI] [PubMed] [Google Scholar]
- 24.Chappell NL, Dujela C, Smith A. Caregiver well-being: Intersections of relationship and gender. Res Aging. 2015;37:623–645. doi: 10.1177/0164027514549258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Yee JL, Schulz R. Gender differences in psychiatric morbidity among family caregivers: A review and analysis. Gerontol. 2000;40:147–164. doi: 10.1093/geront/40.2.147. [DOI] [PubMed] [Google Scholar]
- 26.Montaquila J, Freedman VA, Edwards B, et al. National Health and Aging Trends Study round 1 sample design and selection NHATS Technical Paper #1. Baltimore, MD: Johns Hopkins University School of Public Health; 2012. Available at: https://www.nhats.org/scripts/sampling/NHATS%20Round%201%20Sample%20Design%2005_10_12.pdf. Accessed August 15, 2016. [Google Scholar]
- 27.Schafer JL, Graham JW. Missing data: Our view of the state of the art. Psychol Methods. 2002;7:147–177. [PubMed] [Google Scholar]
- 28.Aiken LS, West SG. Multiple regression: Testing and interpreting interactions. Newbury Park, London: Sage Publications; 1991. [Google Scholar]
- 29.Kasper JD, Freedman VA, Spillman B. National Study of Caregiving user guide. Baltimore, MD: Johns Hopkins University School of Public Health; 2013. Available at: https://www.nhats.org/scripts/documents%5CNSOC_Round_1_User_Guide.pdf. Accessed August 15, 2016. [Google Scholar]
- 30.Chung ML, Pressler SJ, Dunbar SB, et al. Predictors of depressive symptoms in caregivers of patients with heart failure. J Cardiovasc Nurs. 2010;25:411–419. doi: 10.1097/JCN.0b013e3181d2a58d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Chung ML, Bakas T, Plue LD, et al. Effects of self-esteem, optimism, and perceived control on depressive symptoms in stroke survivor-spouse dyads. J Cardiovasc Nurs. 2016;31:E8–E16. doi: 10.1097/JCN.0000000000000232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Neri AL, Yassuda MS, Fortes-Burgos AC, et al. Relationships between gender, age, family conditions, physical and mental health, and social isolation of elderly caregivers. Int Psychogeriatr. 2012;24:472–483. doi: 10.1017/S1041610211001700. [DOI] [PubMed] [Google Scholar]
- 33.Thompson EH. What’s unique about men’s caregiving? Men as caregivers: Theory, research, and service implications. New York: Springer; 2002. pp. 20–47. [Google Scholar]
- 34.Barsky AJ, Peekna HM, Borus JF. Somatic symptom reports in women and men. J Gen Intern Med. 2001;16:266–275. doi: 10.1046/j.1525-1497.2001.00229.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Verbrugge L. Gender and health: An update on hypotheses and evidence. J Health Soc Behav. 1985;26:156–182. [PubMed] [Google Scholar]
- 36.Almeida DM, Neupert SD, Banks SR, et al. Do daily stress processes account for socioeconomic health disparities? J Gerontol B Psych Sci Soc Sci. 2005;60:34–39. doi: 10.1093/geronb/60.special_issue_2.s34. [DOI] [PubMed] [Google Scholar]
- 37.Almeida DM, Piazza JR, Stawski RS, et al. The Speedometer of life: Stress, health and aging. In: Schaie KW, Levey R, editors. The Handbook of the Psychology of Aging. New York: Elsevier; 2010. pp. 191–200. [Google Scholar]
- 38.Cutler DM, Lleras-Muney Understanding differences in health behaviors by education. J Health Econ. 2010;29:1–28. doi: 10.1016/j.jhealeco.2009.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Poulin MJ, Brown SL, Ubel PA, et al. Does a helping hand mean a heavy heart? Helping behavior and well-being among spouse caregivers. Psychol Aging. 2010;25:108–117. doi: 10.1037/a0018064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Rutledge T, Loh C. Effect sizes and statistical testing in the determination of clinical significance in behavioral medicine research. Ann Beh Med. 2004;27:138–145. doi: 10.1207/s15324796abm2702_9. [DOI] [PubMed] [Google Scholar]
- 41.Mausbach BT, Coon DW, Depp C, et al. Ethnicity and time to institutionalization of dementia patients: A comparison of Latina and Caucasian female family caregivers. J Am Geriatr Soc. 2004;52:1077–1084. doi: 10.1111/j.1532-5415.2004.52306.x. [DOI] [PubMed] [Google Scholar]
- 42.Schulz R, Eden J. Families caring for an aging America. The National Academies Press; 2016. Available at: http://www.nap.edu/23606. Accessed October 10, 2016. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


