Abstract
Introduction
Knee pain may preclude participation in higher intensity physical activity in people with knee osteoarthritis and benefits of light activity are unclear. The effect of replacing sedentary time with light intensity activity on incident functional limitation 2 years later was investigated.
Methods
Included were people with or at high risk of knee osteoarthritis without baseline functional limitation using data from the Osteoarthritis Initiative collected between August 2008 and July 2010. Data was analyzed between May 2016 and August 2016 for time in sedentary, light, and moderate to vigorous physical activity from accelerometer monitoring. Incident functional limitation was defined as (1) slow gait speed <1.0 meters/sec during a 20-meter walk, (2) Western Ontario and McMasters University Osteoarthritis Index physical function >28, or (3) Short Form 12 Physical Component scale <40.
Results
Inclusion criteria was met by 1,873 people (mean age=65.0 [SD=9.0] years, mean BMI=28.4 [SD=4.7] kg/m2). Replacing 60 minutes/day of sedentary time with 60 minutes/day of light activity was associated with a 17% reduced risk for incident slow gait speed 2 years later (Hazard Ratio=0.83, 95% CI=0.70, 0.99) after adjustment. Approximately 5 minutes/day of moderate to vigorous physical activity would be necessary to receive the equivalent benefit of 60 minutes/day of light activity. Effects in secondary patient-reported outcomes did not reach statistical significance.
Conclusions
Replacing sedentary time with light activity may reduce the risk of performance-based functional limitation. As expected, moderate to vigorous physical activity rather than light provided stronger risk reduction. When moderate to vigorous physical activity is not an option, pursuing light activity may be a beneficial alternative to being sedentary.
INTRODUCTION
Knee osteoarthritis (OA) is the 11th highest contributor to global disability1 and the leading cause of functional limitation in older adults.2,3 Because knee OA has no known cure, the prevention of functional limitation is paramount. Engaging in physical activity is known to protect against functional limitation. For instance, structured exercise programs, such as resistance training4 and aerobic walking,5 and unstructured physical activity, such as increasing steps/day6 protect against functional limitation among people with knee OA. Less is known about the potential beneficial effects of specific intensities of physical activity on function in people with knee OA.
First, little empirical evidence exists to support whether light intensity activity benefits physical function for people with knee OA. This is a major gap because people with knee OA often have knee pain that precludes higher intensity activity, such as aerobic walking or hiking, and may subsequently need to rely on light intensity activities, such as light household cleaning or gardening, as sources of physical activity. Second, presuming light intensity activity benefits people with knee OA, it is unclear how much moderate to vigorous intensity physical activity (MVPA) may be needed to equal the benefit of light activity. Understanding these associations are important to inform patients and health providers of the potential implications of participating in different intensities of physical activity, (i.e., gauge the “return on the investment” of being physically active).
The purpose of this study is to investigate the protective association of replacing sedentary time with light intensity physical activity on the development of functional limitation 2 years later in people with or at high risk of knee OA. Also examined is how much light activity was needed to equal the benefit of MVPA in instances where both were associated with study outcomes. An isotemporal substitution model was employed to estimate the relative benefit of replacing a fixed time of sedentary activity with light intensity or with MVPA, a methodology previously employed in physical activity studies.7,8
METHODS
Study Sample
The Osteoarthritis Initiative (OAI) is a longitudinal cohort study of the risk factors and natural history of OA. Men and women aged 45 to 79 years were recruited from four clinical sites: Baltimore, Maryland; Pittsburgh, Pennsylvania; Pawtucket, Rhode Island; and Columbus, Ohio. OAI enrolled participants with or at elevated risk of developing symptomatic knee OA. Complete inclusion and exclusion criteria and study rationale can be found at www.oai.ucsf.edu/datarelease/About.asp. Participants included in the study were assessed annually. IRB approval was obtained from all OAI sites.
A subgroup of 2,098 OAI participants free of functional limitation participated in a study that objectively measured physical activity at the 48-month clinic visit from August 2008 to July 2010, which represents the study’s baseline.9 For the present analysis conducted from May 2016 to August 2016, OAI publically released clinical data were used from this subgroup collected from the baseline (OAI 48-month), 2-year (OAI 72-month), and 4-year (OAI 96-month) followup visits. Figure 1 provides a summary of the number of accelerometer records at each stage of study. Of the 1,954 OAI participants who wore the accelerometer for >4 valid days at baseline, 5% (n=81) were lost to follow-up, resulting in an analytic sample size of n=1,873. In general, participants included in the analytic sample (n=1,873) were more likely to be white, had at least a college degree, and had no depressive symptoms compared with those who were lost to follow-up (n=81) not included in the analysis (Appendix Table 1).
Figure 1.
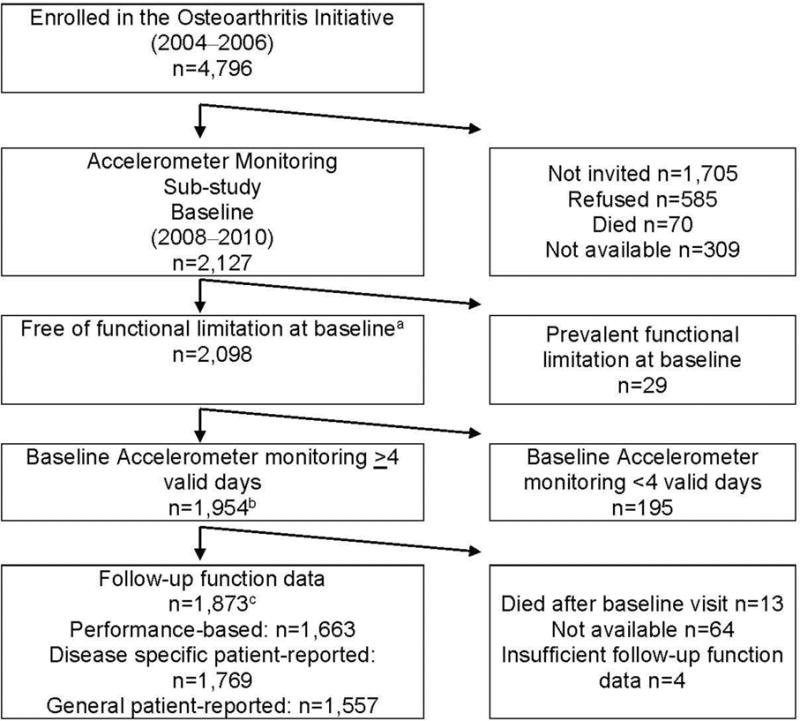
Flow chart for sample size.
aFunctional limitation is defined as a gait speed <1 meter/second, WOMAC <28, or SF-12 <40.
bFor n=51 participants baseline monitoring occurred at the OAI 72-month visit.
cFunctional outcomes included those taken at the 72- and/or 96-month OAI visits.
WOMAC, Western Ontario and McMasters University Osteoarthritis Index; SF-12, 12-item Short Form health survey; OAI, Osteoarthritis Initiative
Measures
Physical activity was monitored at baseline and the 2-year follow-up visits using an ActiGraph GT1M accelerometer. Briefly, the Actigraph GT1M is a small uniaxial accelerometer that measures acceleration and deceleration along a vertical axis,10 and is a valid measure of energy expenditure11 with high test–retest reliability when measured over >4 days.12 Study subjects were asked to continuously wear the accelerometer for 7 consecutive days from getting up the morning until going to bed in the evening, with the exception of water activities. Procedures for the placement, instructions, and data management for accelerometers in the OAI have been previously described.9
Accelerometer data were processed using established validated methodologies.13,14 Accelerometer data were first filtered to identify non-wear periods, (i.e., when the study subject may have removed the monitor), during a day. Potential wear time was first calculated from daily log diaries. Next non-wear was subtracted from potential diary wear time, which was defined as >90 consecutive minutes with activity counts=0 (allowing for 2 consecutive interrupted minutes with activity counts <100), consistent with previously published methods.9,13 Included were participants who had >4 valid days of wear time (i.e., >10 hours in a 24-hour period) in order to provide reliable estimates of physical activity.15
National Cancer Institute intensity thresholds were applied to classify accelerometer counts into three intensity levels: sedentary (0 to 99 counts), light (100 to 2019 counts), and moderate to vigorous (>2,020 counts) on a minute-by-minute basis.15 Total time in minutes/day was summed for each intensity level of physical activity.
The functional limitation was defined using both performance-based and patient-reported measures because both provide distinct information about the underlying construct of physical function.16 The primary outcome was incident functional limitation over 2 years for each study outcome among study participants free of functional limitation at baseline for the baseline to 2-year interval. Similarly, those free of functional limitation at the 2-year visit contributed outcome data from the 2- to 4-year interval. Baseline data for 51 participants came from OAI 72-month visit as they did not have data from OAI 48-month visit.
Functional limitation was defined as walking with a gait speed <1.0 meters/second, (i.e., a slow gait speed). Walking below this speed is a risk factor for hospitalization and mortality in older adults.17,18 Gait speed was determined from the average of two trials at a usual pace >20 meters.
The Western Ontario and McMasters University Osteoarthritis Index (WOMAC) physical function subscale (0–68, higher scores are worse) was used as a patient-reported measure of physical function.19,20 The physical function subscale includes 17 items measuring difficulty with mobility, activities of daily living, and heavy and light domestic duties. Functional limitation was defined as a score of >28 using the WOMAC.21,22 Those with a score of >28 report having at least slight to moderate difficulty in all 17 tasks from the WOMAC physical function scale, or severe to extreme difficulty in 7 to 9 tasks. OAI study participants rated each knee separately and worse knee was used in analyses.
The Short Form 12 (SF-12) Physical Component Scale is a global measure of patient-reported physical function.23,24 Scores of the SF-12 range from 0 to 100 with lower scores being worse, and are standardized to a population mean of 50 with a 10-point SD. Function limitation was defined as a score <40, representing one SD below the population average.
Both gait speed and WOMAC physical function have high test–retest reliability in people with knee OA19,25 and older adults.26 The SF-12 has high test–retest reliability in the general U.S. population.23
The following baseline factors were considered as potential confounders based on their association with physical activity and functional limitation21,27,28: age, sex, race (white, African American, other), education (high school graduate or less versus some college or more), and health factors including BMI, comorbidity, depressive symptoms, lower body pain, and the presence of radiographic knee OA. Knee pain in the last 30 days (0–100) was reported using a Visual Analogue Scale. Self-reported comorbidities were based on the modified Charlson comorbidity index29 (>1 vs none). Depressive symptoms were measured using the Center for Epidemiologic Studies Depression Scale30 (>16 as having major depressive symptoms vs <16 as not having major depressive symptoms). Lower body pain includes symptoms in the hips, ankles, or feet (present versus absent). Radiographic evidence of osteoarthritis (ROA) was identified by a Kellgren–Lawrence grade score of >2 in one or both knees assessed from “fixed-flexion” knee radiography protocol at or before the baseline clinic visit.31
Statistical Analysis
Descriptive statistics of time spent in different intensities of physical activity and the proportion of the sample with incident functional limitation are presented. An isotemporal substitution model was employed to evaluate the effect of replacing sedentary time with time spent in light activity.7 If the observed effect met statistical significance, what duration of time replacing sedentary time with MVPA approximated the same effect on functional limitation as replacing sedentary time for light activity was evaluated. The “substitution effect” is examined by replacing activity from one intensity category with an equal amount of time in a different category, while also adjusting for total daily wear time and the independent effects of other activities simultaneously.
Discrete time hazards models were used for the incidence of functional limitation, which accounted for multiple interval records from the same participant, (i.e., those who contributed data from the baseline to 2-year and 2- to 4-year intervals).32 This method estimated the discrete hazard rate, which is the probability of developing functional limitation in each subsequent 2-year interval given the participant’s functional limitation free status at the previous interval. Hazard ratios (HRs) and 95% CIs for developing functional limitation were adjusted for potential confounders from the starting point of each interval. HRs <1.0 indicate a protective effect of replacing light activity or MVPA for the same amount of sedentary time.
To examine the consistency of replacing light and MVPA for sedentary time with incident functional limitation by OA status, all analyses were repeated by restricting the sample to those with knee ROA followed by further restricting to those with symptomatic knee ROA. The standard definition for symptomatic knee OA from the OAI was applied, which includes both ROA, and the presence of symptoms, defined as pain, aching, or stiffness on most days of a month during the previous year.
RESULTS
The mean (SD) age and BMI of the current study sample was 65.0 (SD=9.0) years and 28.4 (SD=4.7) kg/m2, respectively. A majority of the participants were women (54.7%) and white (84%). Table 1 summarizes participant characteristics of the analytic sample.
Table 1.
Participant Characteristics at the Study Baseline Visit
| Characteristics | Entire sample included in analysis n=1,873 |
Sample with ROA included in analysis n=1,123 |
Sample with Sx ROAa included in analysis n=480 |
|---|---|---|---|
|
|
|||
| Mean±SD (range) or % | |||
| Age, years | 65.0±9.0 (49.0–83.0) |
65.9±8.8 (49.0–83.0) |
65.4±8.8 (49.0–83.0) |
| Sex, women | 54.7 | 54.2 | 52.03 |
| BMI, kg/m2 | 28.4±4.7 (17.2–49.7) |
29.0±4.7 (18.2–49.7) |
29.6±4.8 (18.2–49.7) |
| Education, college degree or higher | 87.1 | 85.6 | 85.6 |
| Race, white | 84.0 | 81.1 | 78.3 |
| ROA, present | 59.9 | 100.0 | 100.00 |
| Presence of knee pain in the last 30 days | 73.2 | 78.5 | 97.5 |
| Knee pain (0–10) | 3.0±2.7 (0.0–10.0) |
3.4±2.8 (0.0–10.0) |
5.0±2.5 (0.0–10.0) |
| Comorbidity, >1 | 28.8 | 30.3 | 34.3 |
| Lower body pain | 58.8 | 57.0 | 65.8 |
| Depressive symptoms, CES-D ≥16 | 11.2 | 10.3 | 13.5 |
| Physical activityb | |||
| Wear time, minutes | 890.3±80.9 (635.0–1,167.8) |
887.9±83.1 (657.0–1,167.8) |
887.6±85.4 (657.0–1,167.8) |
| Sedentary time, minutes | 590.1±88.8 (222.0–842.1) |
590.4±89.2 (237.7–841.7) |
590.5±93.4 (237.7–838.1) |
| Light PA time, minutes | 281.7±77.5 (65.0–647.0) |
280.3±79.0 (65.0–647.0) |
278.7±81.4 (65.0–647.0) |
| MVPA time, minutes | 18.4±19.6 (0.0–162.8) |
16.6±18.0 (0.0–136.1) |
15.6±16.8 (0.0–136.1) |
Symptomatic knee OA was defined as a knee with KL grade >2 and had pain, aching, or stiffness in or around the same knee on most days for >1 month during the past 12 months.
For n=51 participants baseline physical activity monitoring occurred at OAI 72 month visit. Daily minutes averaged over 7 days.
ROA, radiographic knee osteoarthritis; Sx ROA, symptomatic knee osteoarthritis; MVPA, moderate to vigorous intensity physical activity; CES-D, Center for Epidemiologic Studies Depression Scale; VAS, Visual Analogue Scale of the average knee pain in the past 30 days
Of the 1,663 participants without slow gait speed at baseline (>1.0 meters/second), 127 developed a slow gait speed over the follow-up. In general, those with an incident slow gait speed spent more time being sedentary and less time in light activity and MVPA compared with those without incident slow gait speed (Table 2).
Table 2.
Baseline Physical Function and Physical Activity for Study Subjects Without Functional Limitation at Baseline and With and Without Incident Functional Limitation at Follow-up
| Baseline physical function and physical activity | Incident performance-based measure of functional limitation (Slow gait speed, <1.0 m/s) N=1,663 |
Incident disease specific patient-reported functional limitation (WOMAC, >28/68) N=1,769 |
Incident general patient-reported functional limitation (SF-12, <40/100) N=1,557 |
|||
|---|---|---|---|---|---|---|
|
|
||||||
| Yes n=127 |
No n=1536 |
Yes n=195 |
No n=1574 |
Yes n=278 |
No n=1279 |
|
| Physical function, m/s | 1.13±0.10 | 1.37±0.18 | 14.0±8.8 | 4.9±6.8 | 48.1±5.0 | 52.7±5.3 |
| Sedentary, minutes | 605.3±88.4 | 586.8±88.6 | 588.5±92.5 | 591.4±87.3 | 587.2±88.7 | 591.8±87.3 |
| Light intensity, minutes | 246.9±69.5 | 288.5±76.9 | 279.3±87.7 | 282.2±75.3 | 273.4±83.9 | 286.4±74.3 |
| Moderate-to-vigorous intensity, minutes | 6.7±10.4 | 20.4±20.2 | 13.3±14.9 | 19.4±20.1 | 14.1±17.8 | 21.3±20.4 |
Notes: Presented as mean±SD.
WOMAC, Western Ontario and McMasters University Osteoarthritis Index Physical Function Scale; m/s, meters per second; SF-12, 12-item Short From health survey
Replacing 60 minutes/day of sedentary time with 60 minutes/day of light intensity physical activity reduced the risk of developing a slow gait speed by 17% after adjustment for potential confounders (Adjusted HR=0.83, 95% CI=0.70, 0.99). Reducing the replacement to 30 minutes/day attenuated the protective effect to 9% (Figure 2). One would have to replace 5 minutes/day of sedentary time with 5 minutes/day of MVPA to receive the equivalent benefit of replacing 60 minutes/day of light for sedentary time, (i.e., a 17% reduction in risk of developing a slow gait speed).
Figure 2.
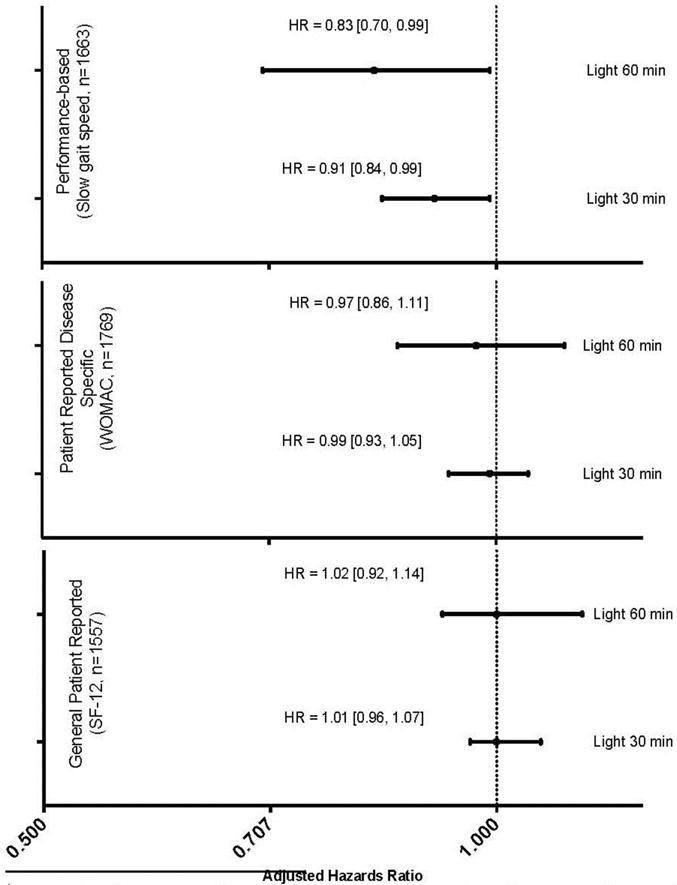
Adjusteda hazard’s ratio of replacing sedentary time for the same fixed time in light intensity physical activity with incident functional limitation. Time is defined as average minutes/day.
aHazard ratios were adjusted for age, sex, race, education, BMI, knee pain in the last 30 days, comorbidities, depressive symptoms, lower body pain in the hips, ankles, or feet, and radiographic evidence of OA.
HR, Hazards Ratio; WOMAC, Western Ontario and McMasters University Osteoarthritis Index Physical Function Scale; SF-12, 12-item Short Form health survey
Of the 1,769 without functional limitation at baseline as measured by WOMAC, 195 developed functional limitation over the follow-up. Those who developed functional limitation spent similar time being sedentary and in light activity, and less time in MVPA compared with those without incident functional limitation (Table 2).
Replacing 60 minutes/day of sedentary time with 60 minutes/day with light activity was associated with a 3% protective effect from incident knee-specific functional limitation as measured by WOMAC, which did not meet statistical significance after adjustment for potential confounders (Adjusted HR=0.97, 95% CI=0.96, 1.11). Replacing 30 minutes/day was not associated with a protective effect as measured by WOMAC (Figure 2).
Of the 1,557 free of functional limitation at baseline as measured by SF-12, 278 developed functional limitation over the follow-up. Those who developed functional limitation spent similar time being sedentary and in light activity, and less time in MVPA compared with those without incident functional limitation (Table 2). Replacing 60 and 30 minutes/day of sedentary time with light activity was not associated with functional limitation (Adjusted HR=1.02, 95% CI=0.92, 1.14, 1.01, 95% CI=0.96, 1.07, respectively; Figure 2).
Similar results for all the study outcomes were found when restricting the sample to those with ROA (Appendix Figure 1) and symptomatic knee OA (Appendix Figure 2). Replacing 60 minutes/day of sedentary time with light activity was associated with a 15% protective effect from slow gait speed for the sample with ROA, and an 11% protective effect from slow gait speed for the sample with symptomatic knee OA. However, these effects did not reach statistical significance when adjusted for potential confounders.
DISCUSSION
Replacing sedentary time with light intensity activity had a modest but statistically significant reduction in risk of developing performance-based functional limitation 2 years later in this large prospective cohort study of people with or at elevated risk for knee OA. Light intensity activity was not protective for patient-reported functional limitation. About 60 minutes/day of light activity was equivalent to about 5 minutes/day of MVPA to convey the same 17% reduced risk for slow walking. Replacing sedentary time with light activity remained protective, but did not meet statistical significance when restricted to people with knee ROA or symptomatic knee OA because of smaller sample sizes. Thus, light intensity physical activity may be beneficial to preserve the performance of function regardless of OA status for people with or at risk of knee OA.
Light intensity physical activity was protective against incident functional limitation as defined by slow walking, which is consistent with previous work with outcomes in disability33 and mortality.34 This finding is important because light activity may be the only intensity of physical activity available to people with knee OA who find higher intensity activities to be difficult due to pain. Importantly, this protective effect was significant to reduce the development of slow gait speed, which is a known risk factor for death,18 persistent lower extremity limitation, and hospitalization in older adults.17
Previously, it was unclear how much light activity would equate to the benefits of MVPA. As expected, stronger protective effects of MVPA rather than light intensity physical activity was found with incident performance-based functional limitation. An average of 60 minutes/day of light activity is needed to convey the same benefit as 5 minutes/day of MVPA to prevent slow walking. A possible reason why replacing MVPA is more efficient than light intensity is because MVPA necessitates greater lower body muscle strength than light intensity activity.35 In fact, MVPA taxes all body systems, such as the cardiovascular, neural, and somatosensory components greater than light intensity activity likely preserving the ability of these underlying systems to support physical function.
Physical activity was more protective against developing functional limitation assessed by performance than for patient-reported outcomes, (i.e., WOMAC or SF-12). This may have occurred for several reasons. First, it is possible that those who were more active simply walked more,36–38 and consequently there was a strong association between physical activity and preservation of gait speed. Second, the patient-reported outcomes included a wide variety of activities in addition to walking, which may capture variability of response and contribute to less precision. Lastly, estimates of physical function obtained from patient reported outcomes are known to differ from that obtained from performance-based instruments.16
Limitations
There are limitations to the study to acknowledge. The accelerometer the OAI employed recorded movement in units of activity counts, thus the exact types of activities employed to attain light activity and MVPA cannot be reported. In addition, there is a possibility of confounding because of unmeasured factors. Hence, the results should be interpreted with caution. Ideally a clinical trial with randomization should be conducted to more definitively establish the protective association between light intensity physical activity and future functional limitation. However, until a clinical trial is conducted, the study provides preliminary guidance with the magnitude of functional benefit that may occur with participation in light and MVPA. Three outcome definitions of limitation were employed, however because there is no gold standard definition for functional limitation, the outcomes do not represent an exhaustive list of such limitation. Lastly, the study had smaller sample sizes for analyses restricted to ROA and symptomatic OA, hence there was less power to show statistical significance. The study has valuable strengths including the analysis of longitudinal prospective data and objective accelerometer physical activity monitoring. Importantly, the relative benefit of replacing light activity for sedentary time on functional limitation in knee OA was investigated; a paucity of studies currently exist to show the benefit of light intensity physical activity in knee OA.
The study findings support recommendations by health professionals for light physical activity in addition to MVPA for people with or at high risk of knee OA. Advice to increase moderate activity often focuses on brisk walking. But, this intensity may be difficult for people with knee pain or other lower body pain. These results indicate replacing sedentary time with enjoyable light activities, such as taking a casual stroll, could also be beneficial. Examples of other enjoyable and practical types of light intensity activities may include grocery shopping with a cart, light effort household cleaning, and watering the lawn or garden.
CONCLUSIONS
In summary, replacing sedentary time with light intensity activity may reduce the risk of incident performance-based functional limitation 2 years later in people with or at high risk of knee OA. Replacing an hour per day of sedentary time with light activity equates the same benefit of replacing 5 minutes/day of sedentary time with MVPA. Health professionals may consider recommending activity to people with knee OA, even if only light activity is possible, in order to minimize the risk of developing future functional limitation.
Supplementary Material
Acknowledgments
Funding for DKW was provided by NIH U54 GM104941 and K12 HD055931. Funding for DD, JL, and JS was provided by NIH 2R01-AR054155 and P60-AR064464. None of the funders of this manuscript had any role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; and preparation, review, or approval of the manuscript.
The Osteoarthritis Initiative (OAI) is a public-private partnership comprised of five contracts (N01-AR-2-2258, N01-AR-2-2259, N01-AR-2-2260, N01-AR-2-2261, N01-AR-2-2262) funded by NIH, a branch of the DHHS, and conducted by the OAI Study Investigators. Private funding partners include Merck Research Laboratories; Novartis Pharmaceuticals Corporation, GlaxoSmithKline; and Pfizer, Inc. Private sector funding for the OAI is managed by the Foundation for the National Institutes of Health. This manuscript was prepared using an OAI public use data set and does not necessarily reflect the opinions or views of the OAI investigators, NIH, or the private funding partners.
DKW and DD were involved in conception and design of the study and in analysis and interpretation of the data. DD, JL, and JS were involved in collection of data. All authors were involved in the interpretation of data. DKW drafted the manuscript. All authors were involved in revision and final approval of the manuscript. All authors had full access to all of the data in the study. DKW and DD are the guarantors.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Dr. White and Dr. Dunlop had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. No author has any potential conflict of interest as related to this manuscript.
All authors have completed the ICMJE uniform disclosure form at www.icmje.org/coi_disclosure.pdf and declare: no support from any organization for the submitted work, no financial relationships with any organizations that might have an interest in the submitted work in the previous 3 years, and no other relationships or activities that could appear to have influenced the submitted work.
References
- 1.Cross M, Smith E, Hoy D, et al. The global burden of hip and knee osteoarthritis: estimates from the global burden of disease 2010 study. Ann Rheum Dis. 2014;73(7):1323–1330. doi: 10.1136/annrheumdis-2013-204763. https://doi.org/10.1136/annrheumdis-2013-204763. [DOI] [PubMed] [Google Scholar]
- 2.Guccione AA, Felson DT, Anderson JJ, et al. The effects of specific medical conditions on the functional limitations of elders in the Framingham Study. Am J Public Health. 1994;84(3):351–358. doi: 10.2105/ajph.84.3.351. https://doi.org/10.2105/AJPH.84.3.351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Murray CJ, Richards MA, Newton JN, et al. UK health performance: findings of the Global Burden of Disease Study 2010. Lancet. 2013;381(9871):997–1020. doi: 10.1016/S0140-6736(13)60355-4. https://doi.org/10.1016/S0140-6736(13)60355-4. [DOI] [PubMed] [Google Scholar]
- 4.Fransen M, McConnell S, Harmer AR, Van der Esch M, Simic M, Bennell KL. Exercise for osteoarthritis of the knee. Cochrane Database Syst Rev. 2015(1):CD004376. doi: 10.1002/14651858.CD004376.pub3. https://doi.org/10.1002/14651858.cd004376.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Loew L, Brosseau L, Wells GA, et al. Ottawa panel evidence-based clinical practice guidelines for aerobic walking programs in the management of osteoarthritis. Arch Phys Med Rehabil. 2012;93(7):1269–1285. doi: 10.1016/j.apmr.2012.01.024. https://doi.org/10.1016/j.apmr.2012.01.024. [DOI] [PubMed] [Google Scholar]
- 6.White DK, Tudor-Locke C, Zhang Y, et al. Daily walking and the risk of incident functional limitation in knee osteoarthritis: an observational study. Arthritis Care Res (Hoboken) 2014;66(9):1328–1336. doi: 10.1002/acr.22362. https://doi.org/10.1002/acr.22362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mekary RA, Willett WC, Hu FB, Ding EL. Isotemporal substitution paradigm for physical activity epidemiology and weight change. Am J Epidemiol. 2009;170(4):519–527. doi: 10.1093/aje/kwp163. https://doi.org/10.1093/aje/kwp163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Buman MP, Hekler EB, Haskell WL, et al. Objective light-intensity physical activity associations with rated health in older adults. Am J Epidemiol. 2010;172(10):1155–1165. doi: 10.1093/aje/kwq249. https://doi.org/10.1093/aje/kwq249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Dunlop DD, Song J, Semanik PA, et al. Objective physical activity measurement in the osteoarthritis initiative: Are guidelines being met? Arthritis Rheum. 2011;63(11):3372–3382. doi: 10.1002/art.30562. https://doi.org/10.1002/art.30562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Matthews CE, Ainsworth BE, Thompson RW, Bassett DR., Jr Sources of variance in daily physical activity levels as measured by an accelerometer. Med Sci Sports Exerc. 2002;34(8):1376–1381. doi: 10.1097/00005768-200208000-00021. https://doi.org/10.1097/00005768-200208000-00021. [DOI] [PubMed] [Google Scholar]
- 11.Kumahara H, Schutz Y, Ayabe M, et al. The use of uniaxial accelerometry for the assessment of physical-activity-related energy expenditure: a validation study against whole-body indirect calorimetry. Br J Nutr. 2004;91(2):235–243. doi: 10.1079/BJN20031033. https://doi.org/10.1079/BJN20031033. [DOI] [PubMed] [Google Scholar]
- 12.Farr JN, Going SB, Lohman TG, et al. Physical activity levels in patients with early knee osteoarthritis measured by accelerometry. Arthritis Rheum. 2008;59(9):1229–1236. doi: 10.1002/art.24007. https://doi.org/10.1002/art.24007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Song J, Semanik P, Sharma L, et al. Assessing physical activity in persons with knee osteoarthritis using accelerometers: data from the osteoarthritis initiative. Arthritis Care Res (Hoboken) 2010;62(12):1724–1732. doi: 10.1002/acr.20305. https://doi.org/10.1002/acr.20305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Semanik P, Song J, Chang RW, Manheim L, Ainsworth B, Dunlop D. Assessing physical activity in persons with rheumatoid arthritis using accelerometry. Med Sci Sports Exerc. 2010;42(8):1493–1501. doi: 10.1249/MSS.0b013e3181cfc9da. https://doi.org/10.1249/MSS.0b013e3181cfc9da. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Troiano RP, Berrigan D, Dodd KW, Masse LC, Tilert T, McDowell M. Physical activity in the United States measured by accelerometer. Med Sci Sports Exerc. 2008;40(1):181–188. doi: 10.1249/mss.0b013e31815a51b3. https://doi.org/10.1249/mss.0b013e31815a51b3. [DOI] [PubMed] [Google Scholar]
- 16.Latham NK, Mehta V, Nguyen AM, et al. Performance-based or self-report measures of physical function: which should be used in clinical trials of hip fracture patients? Arch Phys Med Rehabil. 2008;89(11):2146–2155. doi: 10.1016/j.apmr.2008.04.016. https://doi.org/10.1016/j.apmr.2008.04.016. [DOI] [PubMed] [Google Scholar]
- 17.Cesari M, Kritchevsky SB, Penninx BW, et al. Prognostic value of usual gait speed in well-functioning older people–results from the Health, Aging and Body Composition Study. J Am Geriatr Soc. 2005;53(10):1675–1680. doi: 10.1111/j.1532-5415.2005.53501.x. https://doi.org/10.1111/j.1532-5415.2005.53501.x. [DOI] [PubMed] [Google Scholar]
- 18.Studenski S, Perera S, Patel K, et al. Gait speed and survival in older adults. JAMA. 2011;305(1):50–58. doi: 10.1001/jama.2010.1923. https://doi.org/10.1001/jama.2010.1923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bellamy N, Buchanan WW, Goldsmith CH, Campbell J, Stitt LW. Validation study of WOMAC: a health status instrument for measuring clinically important patient relevant outcomes to antirheumatic drug therapy in patients with osteoarthritis of the hip or knee. J Rheumatol. 1988;15(12):1833–1840. [PubMed] [Google Scholar]
- 20.Bellamy N, Buchanan WW. A preliminary evaluation of the dimensionality and clinical importance of pain and disability in osteoarthritis of the hip and knee. Clin Rheumatol. 1986;5(2):231–241. doi: 10.1007/BF02032362. https://doi.org/10.1007/BF02032362. [DOI] [PubMed] [Google Scholar]
- 21.Sharma L, Cahue S, Song J, Hayes K, Pai YC, Dunlop D. Physical functioning over three years in knee osteoarthritis: role of psychosocial, local mechanical, and neuromuscular factors. Arthritis Rheum. 2003;48(12):3359–3370. doi: 10.1002/art.11420. https://doi.org/10.1002/art.11420. [DOI] [PubMed] [Google Scholar]
- 22.McHugh GA, Luker KA, Campbell M, Kay PR, Silman AJ. Pain, physical functioning and quality of life of individuals awaiting total joint replacement: a longitudinal study. J Eval Clin Pract. 2008;14(1):19–26. doi: 10.1111/j.1365-2753.2007.00777.x. https://doi.org/10.1111/j.1365-2753.2007.00777.x. [DOI] [PubMed] [Google Scholar]
- 23.Ware J, Jr, Kosinski M, Keller SD. A 12-Item Short-Form Health Survey: construction of scales and preliminary tests of reliability and validity. Med Care. 1996;34(3):220–233. doi: 10.1097/00005650-199603000-00003. https://doi.org/10.1097/00005650-199603000-00003. [DOI] [PubMed] [Google Scholar]
- 24.Ware JE, Jr, Sherbourne CD. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care. 1992;30(6):473–483. https://doi.org/10.1097/00005650-199206000-00002. [PubMed] [Google Scholar]
- 25.Fransen M, Crosbie J, Edmonds J. Reliability of gait measurements in people with osteoarthritis of the knee. Phys Ther. 1997;77(9):944–953. doi: 10.1093/ptj/77.9.944. https://doi.org/10.1093/ptj/77.9.944. [DOI] [PubMed] [Google Scholar]
- 26.Curb JD, Ceria-Ulep CD, Rodriguez BL, et al. Performance-based measures of physical function for high-function populations. J Am Geriatr Soc. 2006;54(5):737–742. doi: 10.1111/j.1532-5415.2006.00700.x. https://doi.org/10.1111/j.1532-5415.2006.00700.x. [DOI] [PubMed] [Google Scholar]
- 27.Guccione AA, Felson DT, Anderson JJ. Defining arthritis and measuring functional status in elders: methodological issues in the study of disease and physical disability. Am J Public Health. 1990;80(8):945–949. doi: 10.2105/ajph.80.8.945. https://doi.org/10.2105/AJPH.80.8.945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Jordan J, Luta G, Renner J, Dragomir A, Hochberg M, Fryer J. Knee pain and knee osteoarthritis severity in self-reported task specific disability: the Johnston County Osteoarthritis Project. J Rheumatol. 1997;24(7):1344–1349. [PubMed] [Google Scholar]
- 29.Katz JN, Chang LC, Sangha O, Fossel AH, Bates DW. Can comorbidity be measured by questionnaire rather than medical record review? Med Care. 1996;34(1):73–84. doi: 10.1097/00005650-199601000-00006. https://doi.org/10.1097/00005650-199601000-00006. [DOI] [PubMed] [Google Scholar]
- 30.Radloff L. The CES-D Scale: A Self-Report Depression Scale for Research in the General Population. Appl Psychol Meas. 1977;1(3):385–401. https://doi.org/10.1177/014662167700100306. [Google Scholar]
- 31.Peterfy C, Li J, Zaim S, et al. Comparison of fixed-flexion positioning with fluoroscopic semi-flexed positioning for quantifying radiographic joint-space width in the knee: test-retest reproducibility. Skeletal Radiol. 2003;32(3):128–132. doi: 10.1007/s00256-002-0603-z. https://doi.org/10.1007/s00256-002-0603-z. [DOI] [PubMed] [Google Scholar]
- 32.Prentice RL, Gloeckler LA. Regression analysis of grouped survival data with application to breast cancer data. Biometrics. 1978;34(1):57–67. https://doi.org/10.2307/2529588. [PubMed] [Google Scholar]
- 33.Dunlop DD, Song J, Semanik PA, et al. Relation of physical activity time to incident disability in community dwelling adults with or at risk of knee arthritis: prospective cohort study. BMJ. 2014;348:g2472. doi: 10.1136/bmj.g2472. https://doi.org/10.1136/bmj.g2472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Schmid D, Ricci C, Baumeister SE, Leitzmann MF. Replacing Sedentary Time with Physical Activity in Relation to Mortality. Med Sci Sports Exerc. 2016;48(7):1312–1319. doi: 10.1249/MSS.0000000000000913. https://doi.org/10.1249/MSS.0000000000000913. [DOI] [PubMed] [Google Scholar]
- 35.Fielding RA, Katula J, Miller ME, et al. Activity adherence and physical function in older adults with functional limitations. Med Sci Sports Exerc. 2007;39(11):1997–2004. doi: 10.1249/mss.0b013e318145348d. https://doi.org/10.1249/mss.0b013e318145348d. [DOI] [PubMed] [Google Scholar]
- 36.Yusuf HR, Croft JB, Giles WH, et al. Leisure-time physical activity among older adults. United States, 1990. Arch Intern Med. 1996;156(12):1321–1326. https://doi.org/10.1001/archinte.1996.00440110093012. [PubMed] [Google Scholar]
- 37.Rafferty A, Reeves M, McGee H, Pivarnik J. Compliance with physical activity recommendations by walking for exercise - Michigan, 1996 and 1998. MMWR Morb Mortal Wkly Rep. 2000;49:560–565. [PubMed] [Google Scholar]
- 38.Hootman JM, Macera CA, Ham SA, Helmick CG, Sniezek JE. Physical activity levels among the general U.S. adult population and in adults with and without arthritis. Arthritis Rheum. 2003;49(1):129–135. doi: 10.1002/art.10911. https://doi.org/10.1002/art.10911. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


