Abstract
Purpose
To determine the effects of a home-based reflexology intervention delivered by a friend/family caregiver compared to attention control on health-related quality of life of women with advanced breast cancer undergoing chemotherapy, targeted and/or hormonal therapy.
Methods
Patient-caregiver dyads (N=256) were randomized to 4 weekly reflexology sessions or attention control. Caregivers in the intervention group were trained in a 30-minute protocol. During the 4 weeks, both groups had telephone symptom assessments, and intervention group had fidelity assessments. The intervention effects were assessed using linear mixed effects models at weeks 5 and 11 for symptom severity and interference with daily activities, functioning, social support, quality of patient-caregiver relationship, and satisfaction with life.
Results
Significant reductions in average symptom severity (p=.02) and interference (p<.01) over 11 weeks were found in the reflexology group compared to control, with no group differences in functioning, social support, quality of relationship or satisfaction with life at weeks 5 and 11. Stronger quality of relationship was associated with lower symptom interference in the entire sample (p=.02), but controlling for it did not diminish the effect of intervention on symptoms. Significant reductions in symptom severity in the reflexology group compared to attention control were seen during weeks 2–5, but were reduced at week 11.
Discussion
Efficacy findings of caregiver-delivered reflexology with respect to symptom reduction open a new evidence-based avenue for home-based symptom management.
Keywords: symptom management, breast cancer, home-based, intervention, lay caregivers, reflexology
Introduction
An estimated 1.7 million people are expected to be diagnosed with cancer in the United States (U.S.) during 2016 [1], and breast cancer accounts for more than 25% of cancers diagnosed in U.S. women [2]. The burden of unmanaged symptoms resulting from cancer and its treatment [3–6] leads to reduced health-related quality of life (HRQOL) [7,8].
While conventional medicine provides standard symptom care, more than 80% of women with breast cancer turn to complementary and integrative health (CIH) therapies for symptom management [9]. Among CIH therapies, foot or hand reflexology is one of the most common choices [10]. Foot reflexology involves applying pressure to specific areas of the feet called reflexes and is based on the premise that reflexes in the feet correspond to organs, glands, and systems of the body [11].
A growing body of evidence indicates the potential efficacy of reflexology for the management of symptoms [12–14]. Reflexology studies with cancer patients have had a variety of results, including reports of a significant decrease in anxiety among breast and lung cancer patients (n=23) [15], improvement in HRQOL among cancer patients in palliative care (n=12) [16], no change in depression or anxiety in a cancer palliative care sample (n=17) [17], lower anxiety (n=30) [18] and pain in two samples of patients with various cancer types (n= 23, n= 42, respectively) [19,20] decreased pain among gastric and liver cancer patients (n=30) [21]; and promotion of relaxation among post-surgical early-stage breast cancer patients (n=60) [22]. Only one large-scale study randomized study of reflexology (n=385) supported its efficacy for management of cancer-related symptoms and improving physical functioning among advanced breast cancer patients in treatment [23].
Receiving regular reflexology from a professional provider may not be feasible or sustainable during cancer treatment due to the need to travel to the provider’s office and pay out of pocket for services. The involvement of unpaid lay caregivers in the home may be a significant avenue for the delivery of supportive care [24–28], especially since symptom management is needed over an extended time during the cancer treatment. Lay caregiver is defined as someone who provides unpaid assistance to a patient with a chronic or disabling condition such as cancer [25,26], and is identified by the patient as their caregiver [24,27]. Lay caregivers are often friends or family members, and the number of caregivers supporting patients with cancer continues to grow with an estimated 2.8 million in the United states in 2015 [29].
Due to the involvement of home-based lay caregivers in the assistance with symptom management, the purpose of this work was to determine the effects of a home-based reflexology intervention delivered by a friend/family caregiver compared to attention control among women with advanced breast cancer undergoing medical treatment. Prior work has established the feasibility of training a lay person in reflexology [30–33]. In addition, clinically significant symptom improvements among cancer patients have been reported in association with reflexology-type therapies delivered by lay caregivers [20,34]. In a three-arm randomized trial, Wyatt et al. [23] compared reflexology delivered by a practicing reflexologist, a foot manipulation delivered by research staff who were naive to reflexology, and conventional care among advanced breast cancer patients. They found positive effects for both practicing reflexologists and lay provider-delivered reflexology compared to controls. Building upon these somewhat unexpected results of the success of lay providers who were members of the research staff, the present randomized controlled trial (RCT) asked friend or family caregivers of advanced breast cancer patients to deliver reflexology in the home-based setting.
Aims
The aims of this study were:
To determine the effects of a 4-week, home-based reflexology intervention delivered by a friend/family caregiver compared to attention control on: a) patient symptom severity and interference with daily activities at study weeks 1–4, 5 and 11 (primary outcome); b) functioning and satisfaction with life (secondary outcomes) at study weeks 5 and 11; c) perceived social support and quality of patient-caregiver relationship at study weeks 5 and 11 (potential mediators).
To determine if the effects of the reflexology intervention on symptoms, functioning, and satisfaction with life are mediated by the perceived social support and quality of relationship with the caregiver.
Methods
Design
This RCT enrolled 256 patient-caregiver dyads that were randomized to either 4 weeks of reflexology or attention control. The intervention effects were assessed during the 4-week intervention, immediately post-intervention at study week 5 and at week 11 follow-up.
Participants
Patient inclusion criteria were: 1) age ≥ 21; 2) stage III or IV breast cancer; 3) able to perform basic activities of daily living; 4) undergoing chemotherapy, targeted or hormonal therapy at the time of enrollment; 5) able to speak and understand English; 6) having access to a telephone; 7) able to hear normal conversation; and 8) cognitively oriented to time, place, and person (determined via recruiter). Patient exclusion criteria were: 1) diagnosis of major mental illness in the medical record and verified by the recruiter; 2) residing in a nursing home; 3) bedridden; 4) currently receiving regular reflexology; or 5) diagnoses of symptoms of deep vein thrombosis or painful foot neuropathy.
Friend/family caregiver inclusion criteria were: 1) age ≥18; 2) able and willing to provide at least one 30-minute protocol session per week for 4 consecutive weeks; 3) able to speak and understand English; 4) access to a telephone; 5) able to hear normal conversation; and 6) cognitively oriented to time, place, and person (determined via recruiter). Exclusion criterion was: 1) unwilling to perform a return demonstration of the protocol according to training procedures.
Procedures
Dyads were recruited from nine community-based oncology clinics and two comprehensive cancer centers in the Midwest. Patients identified a friend or family member (caregiver) willing to be instructed in the 30-minute reflexology protocol, and provide at least one weekly session over four consecutive weeks. Informed consent was obtained from both members of the dyad, patient and caregiver. The investigators’ university granted Institutional Review Board (IRB) approval, and subsequently from all recruitment sites. Outcome data were collected at baseline, week 5 (immediately post-intervention) and week 11. Telephone interviews were administered by trained interviewers who were blinded to dyad group assignment. Patients’ medical records were abstracted for the 11-week study participation period by clinic personnel.
Randomization
Following the baseline interview, randomization to either caregiver-delivered reflexology or attention control was implemented from the central study office using a minimization procedure. Balancing variables were recruitment location, presence of metastasis, type of treatment (hormonal therapy only versus other combinations of chemotherapy, targeted and hormonal therapies) and the level of fatigue at baseline (<7 versus 7+ according to an established cut-off) [35].
Intervention protocol
Intervention fidelity was assured through established methods outlined by the NIH Treatment Fidelity Workgroup for consistency in dose, provider training, delivery, receipt and enactment of the intervention [36].
Reflexology protocol
Training and Delivery
Dyads randomized to the reflexology group were contacted by a study reflexologist to schedule friend/family caregiver training in the home. The cancer-specific protocol includes 9 reflexes on the foot as validated in previous work [23]. This protocol requires a thumb-walking pressure over each reflex, with a duration of 15 minutes per foot, totaling a 30-minute session. Caregiver training consisted of two home visits by a study reflexologist. The first visit was used to demonstrate the specific study protocol and train the caregiver to perform the stimulation of 9 reflexes, until a return-demonstration on the reflexologist by the caregiver was performed with 90% accuracy. Session one was then performed on the patient by the caregiver, while the reflexologist observed and coached. During the caregiver delivery of session two to the patient, the study reflexologist observed and offered adjustments in technique as needed. Two additional weeks of one or more sessions per week were delivered by the caregiver to the patient without the reflexologist being present. Illustrated directions and a contact number were left with the dyad to support their independent delivery of sessions during weeks 3 and 4 of the intervention timeframe.
Data Collection During Intervention
Weekly symptom assessment calls were made to all patients during weeks 1–4; these calls also queried the number of reflexology sessions they received in the past week. At least one weekly session was required, but the total number of sessions was not otherwise restricted. As needed and desired by the dyad, additional reflexology sessions could be conducted, and their number was tracked during each of weeks 1–4. In the attention control group, the weekly symptom calls provided social interaction and attention, but no interventions were administered. Caregivers in the reflexology group were also called weekly to remind them to deliver at least one session per week. After the week 5 interview, weekly calls were not made, but the dyads could continue conducting reflexology sessions. Data on the number of sessions delivered between weeks 5 and 11 were obtained during the week 11 interview.
Incentives
Following all data collection, the attention control group was offered a reflexology session for the patient or protocol training for their friend or family caregiver.
Measures
Demographic information collected in the baseline interview included patient’s age, race, ethnicity, level of education, employment, income, and relationship to the caregiver. The number of comorbid conditions was assessed using the Bayliss tool that queries 20 conditions [37], omitting the cancer item since all patients had breast cancer. Data on cancer stage, recurrence, metastasis, medical treatments administered during the study were obtained from the medical records. The number of CIH therapies used at baseline was determined using a checklist of 25 therapies.
The M.D. Anderson Symptom Inventory (MDASI) [35] was administered at baseline, weeks 1–4, 5 and 11. It evaluates severity of 13 symptoms (i.e., pain, fatigue, nausea, disturbed sleep, distress, shortness of breath, difficulty remembering, decreased appetite, drowsiness, dry mouth, sadness, vomiting, numbness/tingling) on a scale from 0=not present to 10=as bad as you can imagine, and the interference of these symptoms with daily life on a scale from 0=does not interfere to 10=completely interferes. Reliability and validity of the instrument are established [35]. Summed symptom severity and interference scores were derived from this instrument.
Physical functioning and satisfaction with participation in social roles were measured using Patient Reported Outcomes Measurement Information System (PROMIS) tools, which have good evidence of reliability and validity [38,39]. Four-item short forms were administered at baseline, weeks 5 and 11. Higher scores indicate more of the construct being measured. The T-score rescales the raw score into a standardized score with a mean of 50 and a standard deviation 10 for the general population.
Quality of Life Index (QLI) [40] measured satisfaction with life at baseline, weeks 5 and 11. The QLI reflects both satisfaction and importance regarding various aspects of life, using 30 items for each. Importance ratings are used to weight satisfaction responses, so that scores reflect satisfaction with the aspects of life that are valued by the individual. The total QLI score summarizes four domains: health and functioning, psychological/spiritual domain, social and economic.
Multidimensional Scale of Perceived Social Support (MSPSS) Tool [41] was administered at baseline, weeks 5 and 11. The two four-item subscales measuring perceived social support from friends and family were utilized in this study. Items are rated on a 7-point scale, with higher scores reflecting higher perceived social support. The MSPSS has exhibited concurrent, construct, and discriminant validity; as well as internal consistency and test-retest reliability, and a sound factor structure [42].
Quality of Relationship Tool [43] was administered at baseline, weeks 5 and 11. It consists of six items designed to assess the quality of a specific relationship and has established reliability with a sample of married couples. It is modified to capture patients’ perception of the quality of relationship with their friend/family caregiver. Items are rated on a 5-point scale with lower scores indicating better quality of relationship.
Analysis
Baseline characteristics were summarized by study group for outcome values and potential covariates. Attrition rates and reasons were compared by study group. The main analysis followed the intent-to-treat approach and included all participants who completed at least one post-baseline assessment regardless of their adherence to the intervention protocol. Linear mixed effects (LME) models were used to relate repeated measures of primary and secondary outcomes and potential mediators to study group, while controlling for outcome values at baseline. The main (time-averaged) group effect was of interest as reflected by the coefficient of the study group variable, and its significance was tested. For six repeated measures of symptom severity and interference, the group by time interaction was added to the LME model to further evaluate the process of change in symptoms. The least square (LS) means by study group at each week were output from the model, and differences between them were tested to assess potentially changing intervention effect as time progressed.
To test for mediation, perceived social support or quality of relationship (one at a time) was entered as a time-varying covariate into the LME models for primary and secondary outcomes that were significantly different by study group. The change in the significance of the study group variable after controlling for social support was used to determine whether mediation had occurred.
All statistical tests were two-sided. Since the primary and secondary outcomes were specified a priori, .05 level of significance was used. All analyses were conducted in SAS 9.4 [44].
Results
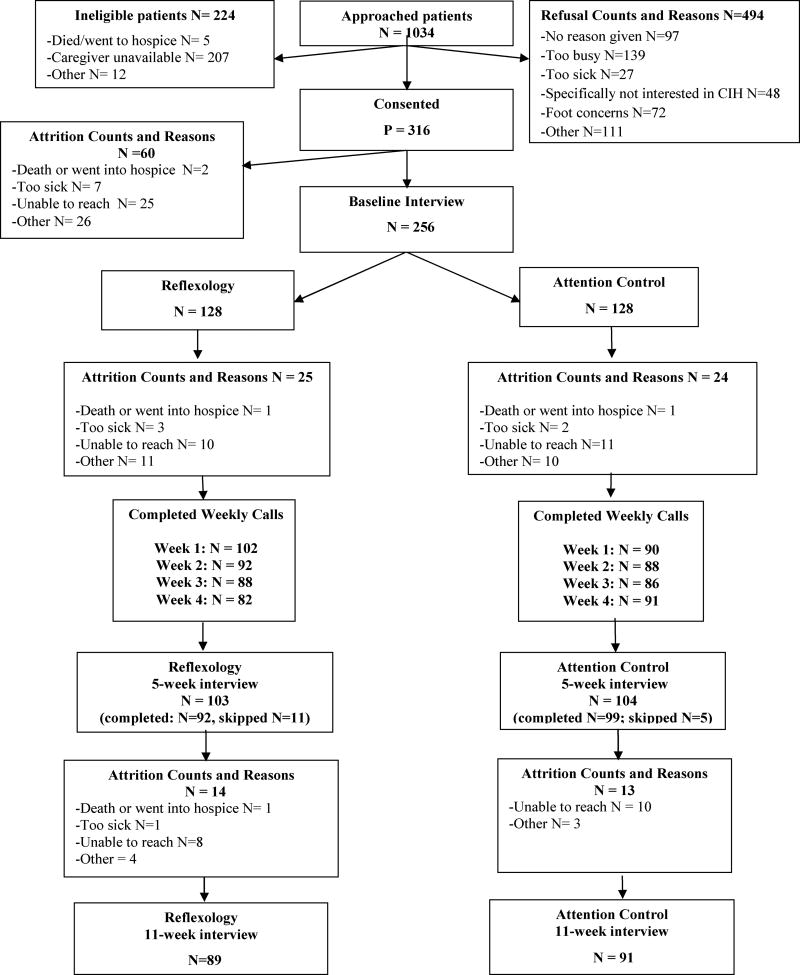
The flow of participants through the study is depicted in Figure 1. The consent rate for the dyad, i.e., patients and caregiver, was 37%. Distributions of symptom and other outcomes did not differ at baseline by study group (Table 1). The reflexology group had a mean age of 58 years, while the attention control group had a mean of 55 years, (p=.02). Because age could be a prognostic factor for symptom severity, it was controlled for in all later analyses.
Figure 1.
CONSORT Chart Home-Based Symptom Management via Reflexology for Breast Cancer Patients
Table 1.
Demographic characteristics and baseline values of the outcomes by study group
| Reflexology N=128 |
Attention Control N=128 |
P-value | |
|---|---|---|---|
|
| |||
| N (%) | N (%) | ||
|
| |||
| Metastatic cancer | |||
| Yes | 80 (62) | 81 (63) | .89 |
| No | 48 (38) | 47 (37) | |
|
| |||
| Recurrent cancer | |||
| Yes | 41 (32) | 35 (27) | .41 |
| No | 87 (68) | 93 (73) | |
|
| |||
| Treatment type | |||
| Chemotherapy or targeted therapy (with or w/o hormonal) | 105 (82) | 105 (82) | .99 |
| Hormonal therapy only | 23 (18) | 23 (18) | |
|
| |||
| Race | |||
| White | 105 (83) | 107 (84) | |
| Black or African American | 13 (10) | 13 (10) | .87 |
| Other | 9 (7) | 7 (6) | |
|
| |||
| Ethnicity | |||
| Hispanic or Latino | 5 (4) | 6 (5) | .76 |
| Not Hispanic or Latino | 123 (96) | 122 (95) | |
|
| |||
| Relationship to caregiver | |||
| Spouse or partner | 70 (55) | 71 (56) | |
| Child or stepchild | 21 (16) | 21 (16) | .49 |
| Friend | 11 (9) | 17 (13) | |
| Other | 26 (20) | 19 (15) | |
|
| |||
| Caregiver sex | |||
| Male | 76 (61) | 73 (57) | .59 |
| Female | 49 (39) | 54 (43) | |
|
| |||
| Employment | |||
| Full time | 28 (22) | 38 (30) | |
| Part time | 10 (8) | 12 (9) | .32 |
| Other | 50 (39) | 48 (38) | |
| Retired | 40 (31) | 29 (23) | |
|
| |||
| Education | |||
| High school graduate (or GED) or some high school | 29 (23) | 29 (22) | |
| Some college or 2-year degree | 35 (27) | 38 (30) | .88 |
| 4-year college graduate | 30 (24) | 33 (26) | |
| More than a 4-year college degree | 33 (26) | 28 (22) | |
|
| |||
| Marital status | |||
| Never Married | 14 (11) | 13 (10) | |
| Married or Living with Partner | 89 (70) | 87 (68) | .88 |
| Divorced/Separated | 19 (15) | 19 (15) | |
| Widowed | 6 (4) | 9 (7) | |
|
| |||
| Mean (SD) | Mean (SD) | ||
|
| |||
| Age in years | 58.09 (11.62) | 54.80 (10.30) | .02 |
|
| |||
| Number of comorbid conditions | 4.00 (2.54) | 3.35 (2.62) | .28 |
|
| |||
| Number of CIH therapies used | 2.61 (2.52) | 2.45 (2.47) | .62 |
|
| |||
| MDASI summed symptom severity | 44.49 (24.40) | 42.51 (22.59) | .50 |
|
| |||
| MDASI summed symptom interference | 22.33 (16.05) | 22.55 (15.67) | .91 |
|
| |||
| Severity of fatigue | 5.96 (2.67) | 5.70 (2.80) | .45 |
|
| |||
| Severity of pain | 3.56 (3.09) | 3.57 (3.24) | .98 |
|
| |||
| PROMIS physical function | 41.18 (7.57) | 41.17 (8.12) | .99 |
|
| |||
| PROMIS satisfaction with participation in social roles | 45.61 (8.47) | 44.66 (8.33) | .37 |
|
| |||
| Quality of Life Index (QLI) | 21.71 (4.31) | 21.13 (4.69) | .31 |
|
| |||
| Social support (MSPSS) | 6.54 (1.66) | 6.50 (0.83) | .81 |
|
| |||
| Quality of Relationship | 1.29 (0.61) | 1.22 (0.38) | .30 |
The characteristics of the drop-outs did not differ by study group (data not in Tables). The attrition rates after randomization were 30% in the reflexology group, and 29% in the attention control group (Figure 1). Most frequently, attrition occurred due to inability to reach the participant over the telephone for data collection. A total of 7 women (5 in the reflexology group and 2 in the attention control) dropped out for the reasons of being too sick, going into hospice or death during the 11-week study. In the reflexology group, an average of 4.4 sessions (standard deviation 3.3) were delivered by the caregivers over the 4-week intervention period (1.1 per week), while during the following 6 weeks, the mean was 3.6 (standard deviation 6.1), corresponding to 0.6 sessions per week on average.
The primary analysis of the main (time-averaged) intervention effect on primary and secondary outcomes revealed significant reductions in summed symptom severity in the reflexology group compared to attention control (mean difference −4.34, standard error (SE) 1.85, p=.02) and interference (mean difference −3.69, SE= 1.39, p<.01, Table 2). No statistically significant differences between study groups were observed for the physical function or satisfaction with life. Satisfaction with participation in social roles was on average better in the reflexology group, but the difference did not reach statistical significance (p=.06; Table 2).
Table 2.
Differences between reflexology and attention control groups averaged over weeks 5 and 11 (main effects): study group coefficients, their standard errors, test statistics, and p-values
| Outcome | Coefficient (SE) | T | P-value |
|---|---|---|---|
| MDASI summed symptom severity | −4.34 (1.85) | −2.34 | .02 |
| MDASI summed symptom interference | −3.69 (1.39) | −2.66 | <.01 |
| PROMIS physical function | 0.195 (0.67) | 0.29 | .77 |
| PROMIS satisfaction with participation in social roles | 1.659 (0.88) | 1.88 | .06 |
| Quality of Life Index | 0.599 (0.36) | 1.67 | .10 |
| Quality of Relationship | 0.000725 (0.07) | 0.01 | .99 |
| Social support | −0.26 (0.15) | −1.76 | .08 |
There were also no differences between study groups in quality of patient-caregiver relationship at weeks 5 and 11. The perceived social support was higher in the attention control group but the difference was not statistically significant (p=.08; Table 2). Since there was no intervention effect on potential mediators, further mediation analyses were not warranted. Controlling for the social support and quality of patient-caregiver relationship did not attenuate the effects of study group on symptom outcomes; stronger quality of relationship was associated with lower symptom interference (coefficient=2.46, SE=1.07, p=.02).
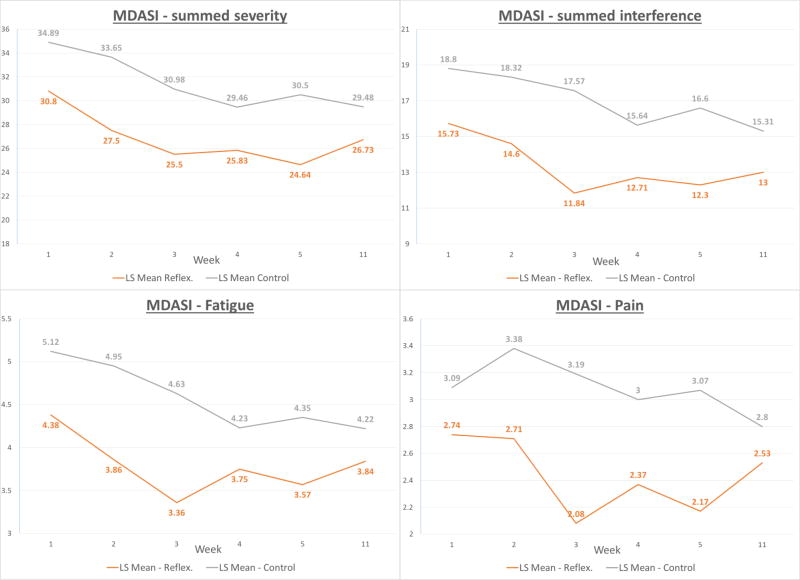
Finally, further examination of the process of change in symptoms revealed that significant reductions in symptom severity in the reflexology group compared to attention control began at week 2 (p<.01) and continued at weeks 3–5 (Table 3). The differences were smaller at week 11 follow-up; however, the overall longitudinal pattern depicted in Figure 2 was consistent with the main time-averaged group effect presented in Table 2. A similar longitudinal pattern was seen for the summed symptom interference (Table 3 and Figure 2). When individual symptoms comprising the MDASI were examined, substantial significant differences seen for the summed indices were observed for the symptoms of fatigue and pain, indicating that these two symptoms were most responsive to the reflexology intervention.
Table 3.
Least square (LS) means and their standard errors for symptom outcomes at weeks 1–4, 5, and 11
| MDASI summed symptom severity |
MDASI summed symptom interference |
Severity of fatigue | Severity of pain | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Week | Reflex. LS Mean (SE) |
Control LS Mean (SE) |
P- value |
Reflex. LS Mean (SE) |
Control LS Mean (SE) |
P- value |
Reflex. LS Mean (SE) |
Control LS Mean (SE) |
P- value |
Reflex. LS Mean (SE) |
Control LS Mean (SE) |
P- value |
| 1 | 30.80 (1.47) | 34.89 (1.54) | .06 | 15.73 (1.12) | 18.80 (1.16) | .06 | 4.38 (0.23) | 5.12 (0.24) | .02 | 2.74 (0.22) | 3.09 (0.23) | .28 |
| 2 | 27.50 (1.53) | 33.65 (1.55) | <.01 | 14.60 (1.15) | 18.32 (1.17) | .02 | 3.86 (0.24) | 4.95 (0.24) | <.01 | 2.71 (0.23) | 3.38 (0.24) | .04 |
| 3 | 25.50 (1.55) | 30.98 (1.55) | .01 | 11.84 (1.17) | 17.57 (1.17) | <.01 | 3.36 (0.24) | 4.63 (0.24) | <.01 | 2.08 (0.24) | 3.19 (0.24) | <.01 |
| 4 | 25.83 (1.57) | 29.46 (1.52) | .10 | 12.71 (1.19) | 15.64 (1.15) | .08 | 3.75 (0.24) | 4.23 (0.24) | .15 | 2.37 (0.24) | 3.00 (0.23) | .06 |
| 5 | 24.64 (1.52) | 30.50 (1.48) | <.01 | 12.30 (1.15) | 16.60 (1.12) | <.01 | 3.57 (0.24) | 4.35 (0.23) | .02 | 2.17 (0.23) | 3.07 (0.22) | <.01 |
| 11 | 26.73 (1.54) | 29.48 (1.52) | .21 | 13.00 (1.16) | 15.31 (1.15) | .16 | 3.84 (0.24) | 4.22 (0.24) | .26 | 2.53 (0.23) | 2.80 (0.23) | .42 |
Figure 2.
Discussion
As earlier mentioned, this RCT grew out of previous work that demonstrated the efficacy of reflexology delivered by not only trained reflexology practitioners but also by study staff lay providers who were naïve to reflexology [23]. Due to this unexpected finding, it became important to evaluate friend or family caregivers as home providers. The present study trained lay caregivers in reflexology delivery to determine if symptom benefits were possible, and indeed, the symptoms improved.
Due to the demonstrated efficacy for symptom management from trained caregivers, promoting the availability of such care would be beneficial to patients. While the literature most often described caregiver training in psychosocial interventions, few caregivers are trained in comprehensive psychomotor symptom management interventions such as reflexology [32,45,46]. The potential of such home-based interventions should be seen as an important adjunct to formal care. Friend and family caregivers can provide home-based interventions when needed for symptom management as opposed to scheduling appointments for some time in the future with practitioners. In addition, home-based delivery minimizes the financial expenses and potential exposure to outside contaminants for immunocompromised patients with advanced disease. The findings from this research demonstrate the possibility of an accessible and efficacious caregiver-delivered home-based intervention.
In terms of sustainability of study outcomes, a reduced effect was noted at week 11. This could be explained by lower adherence to the conduct of regular weekly sessions once weekly calls with reminders from research staff were discontinued. These findings are consistent with the literature that suggests the importance for continued caregiver support to sustain patient outcomes [47–49]. The Institute of Medicine also recommended that healthcare professionals establish programs to assist informal caregivers in management of their caregiving role [50].
An important factor that must be considered is the impact of this intervention on the dyad relationship. It is conceivable that a successful intervention for the patient might not derive benefits for the dyadic relationship. The HRQOL of both members must be considered and preserved. In a meta-analysis, Waldron et al. reported that among 84 cancer caregiver studies, spouses and women were the most distressed categories of caregivers [45]. In the present study, the vast majority of male caregivers were spouses, not allowing a further investigation of caregiver sex versus spousal relationship. Burridge et al. found that caregivers are caught in a paradox whereby their health needs may become subsumed by the patient’s [51]. In contrast to these reports, from a social standpoint, the dyadic relationships in the present study were not different in quality when compared to dyads in the control group. Specifically, the involvement of friend or family caregivers in the delivery of reflexology to patients was not associated with strains on the patient-caregiver relationship or social support from the patient’s perspective. The finding of no impact on dyadic relationships in the present study may be due to the majority of male caregivers in this study as opposed to the study by Waldron et al. [45].
The finding of the stable social relationship in this study points to the need to consider other potential mechanisms of action of reflexology, such as underlying biology. To date, the potential physiologic mechanisms suggested in the literature include: activation of receptors to release oxytocin for its positive effects on well-being [52]; facilitation of optimum circulation, which in turn eliminates toxins and supports immune, nervous, and glandular systems [53]; activation of the relaxation response [22,54]; and complex inputs and processing via neuromatrices in the central nervous system [20,55]. These theoretical mechanisms may or may not be the active ingredient in reflexology, and further research is needed on the pathways that may explain symptom reduction due to reflexology.
Limitations
The consent rate was lower than other studies enrolling advanced cancer patients [3,4,13]. This was due to the need to enroll both the patient and their friend or family caregiver. Obtaining two consent forms rather than one presented an additional challenge. The demographic characteristics of the sample reflected those of populations served by the participating sites and may not be generalizable to other populations. Diverse oncological treatments may have caused a variety of drug-induced toxicities. Due to a large number of drugs and their combinations [56], it was not possible to control for specific toxicities, but due to randomization, it is unlikely that these toxicities impacted estimates of intervention effects.
Conclusions
This research has identified that caregiver-delivered reflexology is efficacious in reducing cancer symptom severity and interference with daily activities. It has further established that the social relationship between patient and friend or family caregiver is not influenced by this structured home-based symptom management intervention. This combination of findings leads to the exciting next steps with research on reflexology and perhaps other complementary therapies – the exploration of a physiologic mechanism underlying their efficacy.
Acknowledgments
The research team would like to thank our dedicated participants who made this study possible.
Funded by NCI: grant R01 CA157459 Home-Based Symptom Management via Reflexology for Advanced Breast Cancer Patients. Principal Investigator: G. Wyatt.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of Interest: The authors declare that they have no conflict of interest.
References
- 1.American Cancer Society. Cancer Facts and Figures 2016. [Accessed Nov 18 2016];2016 http://www.cancer.org/acs/groups/content/@research/documents/document/acspc-047079.pdf.
- 2.Jemal A, Siegel R, Ward E, et al. Cancer statistics. CA Cancer J Clin. 2007;57(1):43–66. doi: 10.3322/canjclin.57.1.43. [DOI] [PubMed] [Google Scholar]
- 3.Butt Z, Rosenbloom SK, Abernethy AP, et al. Fatigue is the most important symptom for advanced cancer patients who have had chemotherapy. Journal of the National Comprehensive Cancer Network. 2008;6(5):448–455. doi: 10.6004/jnccn.2008.0036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Grabsch B, Clarke D, Love A, et al. Psycological morbidity and quality of life in women with advanced breast cancer: A cross-sectional survey. Palliative and Supportive Care. 2006;4:47–56. doi: 10.1017/s1478951506060068. [DOI] [PubMed] [Google Scholar]
- 5.National Cancer Institute. Definitions, statistics, and graphs: Survivorship Definitions. [Accessed Nov 03 2016];2014 http://cancercontrol.cancer.gov/ocs/statistics/definitions.html.
- 6.Kangas M, Bovbjerg DA, Montgomery GH. Cancer-related fatigue: A systematic and meta-analytic review of non-pharmacological therapies for cancer patients. Psychol Bull. 2008;134(5):700–741. doi: 10.1037/a0012825. [DOI] [PubMed] [Google Scholar]
- 7.McMillan SC, Small BJ. Symptom distress and quality of life in patients with cancer of newly admitted to hospice home care. Oncol Nurs Forum. 2002;29(10):1421–1428. doi: 10.1188/02.ONF.1421-1428. [DOI] [PubMed] [Google Scholar]
- 8.Cella DF, Wagner L, Cashy J, et al. Should health-related quality of life be measured in cancer symptom management clinical trials? Lessons learned using the functional assessment of cancer therapy. Journal of the National Cancer Institute Monographs. 2007;37:53–60. doi: 10.1093/jncimonographs/lgm009. [DOI] [PubMed] [Google Scholar]
- 9.Boon HS, Olatunde F, Zick SM. Trends in complementary/alternative medicine use by breast cancer survivors: comparing survey data from 1998 and 2005. BMC Womens Health. 2007;7:4. doi: 10.1186/1472-6874-7-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lengacher C, Bennett M, Kip K, et al. Frequency of use of complementary and alternative medicine in women with breast cancer. Oncol Nurs Forum. 2002;29(10):1445–1452. doi: 10.1188/02.ONF.1445-1452. [DOI] [PubMed] [Google Scholar]
- 11.Byers DC. Better Health with Foot Reflexology: The Original Ingham Method. Ingham Publishing, Inc.; St. Petersburg, FL: 1996. [Google Scholar]
- 12.Ernst E. Is reflexology an effective intervention: A systematic review of randomized controlled trials. Med J Australia. 2009;191:263–266. doi: 10.5694/j.1326-5377.2009.tb02780.x. [DOI] [PubMed] [Google Scholar]
- 13.Wang MY, Tsai PS, Lee PH, Chang WY, Yang CM. The efficacy of reflexology: Systematic review. J Adv Nurs. 2008;62(5):512–520. doi: 10.1111/j.1365-2648.2008.04606.x. [DOI] [PubMed] [Google Scholar]
- 14.Ernst E, Posadzki P, Lee MS. Reflexology: An update of a systematic review of randomized clinical trials. Maturitas. 2011;68(2):116–120. doi: 10.1016/j.maturitas.2010.10.011. [DOI] [PubMed] [Google Scholar]
- 15.Stephenson N, Weinrich S, Tavakoli A. The effects of foot reflexology on anxiety and pain inpatients with breast and lung cancer. Oncol Nurs Forum. 2000;27:67–72. [PubMed] [Google Scholar]
- 16.Hodgson H. Does reflexology impact on cancer patients' quality of life? Nurs Stand. 2000;14(31):33. doi: 10.7748/ns2000.04.14.31.33.c2817. [DOI] [PubMed] [Google Scholar]
- 17.Ross CS, Hamilton J, Macrae G, et al. A pilot study to evaluate the effect of reflexology on mood and symptom rating of advanced cancer patients. Palliat Med. 2002;16(6):544–545. doi: 10.1191/0269216302pm597xx. [DOI] [PubMed] [Google Scholar]
- 18.Quattrin R, Zanini A, Buchini S, et al. Use of reflexology foot massage to reduce anxiety in hospitalized cancer patients in chemotherapy treatment: Methodology and outcomes. Journal of Nursing Management. 2006;14(2):96–105. doi: 10.1111/j.1365-2934.2006.00557.x. [DOI] [PubMed] [Google Scholar]
- 19.Stephenson N, Dalton JA, Carlson J. The effect of foot reflexology on pain in patients with metastatic cancer. Appl Nurs Res. 2003;16(4):284–286. doi: 10.1016/j.apnr.2003.08.003. [DOI] [PubMed] [Google Scholar]
- 20.Stephenson N, Swanson M, Dalton J, Keefe FJ, Engelke M. Partner-delivered reflexology: Effects on cancer pain and anxiety. Oncol Nurs Forum. 2007;34(1):127–132. doi: 10.1188/07.ONF.127-132. [DOI] [PubMed] [Google Scholar]
- 21.Tsay S, Chen H, Chen S, Lin H, Lin K. Effects of reflexotherapy on acute postoperative pain and anxiety among patients with digestive cancer. Cancer Nurs. 2008;31(2):109–115. doi: 10.1097/01.NCC.0000305694.74754.7b. [DOI] [PubMed] [Google Scholar]
- 22.Sharp DM, Walker MB, Chaturvedi A, et al. A randomized, controlled trial of the psychological effects of reflexology in early breast cancer. Eur J Cancer. 2010;46(2):312–322. doi: 10.1016/j.ejca.2009.10.006. [DOI] [PubMed] [Google Scholar]
- 23.Wyatt G, Sikorskii A, Rahbar M, Victorson D, You M. Health-related quality of life outcomes: A reflexology trial with patients with advanced-stage breast cancer. Oncol Nurs Forum. 2012;39(6):568–577. doi: 10.1188/12.ONF.568-577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Stenberg U, Ruland CM, Miaskowski C. Review of the literature on the effects of caring for a patient with cancer. Psycho-oncol. 2010;19:1013–1025. doi: 10.1002/pon.1670. [DOI] [PubMed] [Google Scholar]
- 25.Family Caregiver Alliance. Caregiver Assessment: Principles, Guidelines and Strategies for Change. [Accessed Nov 18 2016];Report from a National Consensus Development Conference. 2006 I https://www.caregiver.org/sites/caregiver.org/files/pdfs/v1_consensus.pdf. [Google Scholar]
- 26.Family Caregiver Alliance. Caregiver Assessment: Voices and views from the Field. [Accessed Nov 18 2016];Report from a National Consensus Development Conference. 2006 II https://www.caregiver.org/sites/caregiver.org/files/pdfs/v2_consensus.pdf. [Google Scholar]
- 27.Kissane D, Bloch S. Family focused grief therapy. Oxford University Press; 2002. [Google Scholar]
- 28.Reinhard S, Levine C, Samis S. Home alone: Family caregivers providing complex chronic care. [Accessed Nov 03 2016];American Association of Retired Persons. 2012 http://www.aarp.org/content/dam/aarp/research/public_policy_institute/health/home-alone-family-caregivers-providing-complex-chronic-care-rev-AARP-ppi-health.pdf.
- 29.National Alliance for Caregiving, American Association of Retired Persons Public Policy Institute. Caregiving in the U.S. 2015. National Alliance of Caregiving and American Association of Retired Persons; Bethesda, MD: 2015. [Google Scholar]
- 30.Given CW, Wyatt GK, Given BA. A complementary therapy intervention for supportive care of cancer patients: West Michigan Cancer Center, Michigan State University, and the Mary Margaret Walther Program 1998–2002 [Google Scholar]
- 31.Wyatt G, Sikorskii A, Siddiqi A. Feasibility of a reflexology and guided imagery intervention during chemotherapy: Results of a quasi-experimental study. Oncol Nurs Forum. 2007;34(3):635–642. doi: 10.1188/07.ONF.635-642. [DOI] [PubMed] [Google Scholar]
- 32.Kozachik S, Wyatt GK, Given CW, Given B. Patterns of Use of Complementary Therapies Among Cancer Patients and Their Family Caregivers. Cancer Nurs. 2006;29(2):84–94. doi: 10.1097/00002820-200603000-00002. [DOI] [PubMed] [Google Scholar]
- 33.Wyatt GK, Sikorskii A, Rahbar H. Reflexology: An Intervention for Advanced Breast Cancer. Michigan State University funded by the National Cancer Institute; 2005–2010. [Google Scholar]
- 34.Kohara H, Miyauchi T, Suehiro Y, et al. Combined modality treatment of aromatherapy, footsoak, and reflexology relieves fatigue in patients with cancer. J Palliat Med. 2004;7(6):791–796. doi: 10.1089/jpm.2004.7.791. [DOI] [PubMed] [Google Scholar]
- 35.Cleeland CS, Mendoza T, Wang XS, et al. Assessing symptom distress in cancer patients: The M.D. Anderson symptom inventory. Cancer. 2000;89(7):1634–1646. doi: 10.1002/1097-0142(20001001)89:7<1634::aid-cncr29>3.0.co;2-v. [DOI] [PubMed] [Google Scholar]
- 36.Badger T, Segrin C, Dorros SM, Meek P, Lopez AM. Depression and anxiety in women with breast cancer and their partners. Nurs Res. 2007;56(1):44–53. doi: 10.1097/00006199-200701000-00006. [DOI] [PubMed] [Google Scholar]
- 37.Bayliss EA, Ellis JL, Steiner JF. Seniors’ self-reported multimorbidity captured biopsychosocial factors not incorporated into two other data-based morbidity measures. J Clin Epidemiol. 2009;62(5):550–557. doi: 10.1016/j.jclinepi.2008.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Cella D, Riley W, Stone A, et al. Initial item banks and first wave testing of the Patient-Reported Outcomes Measurement Information System (PROMIS) network: 2005–2008. J Clin Epidemiol. 2010;63:1179–1194. doi: 10.1016/j.jclinepi.2010.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.PROMIS. [Accessed Nov 03 2016];Patient-Reported Outcomes Measurment Information System, Version 1.0. 2010 www.nihpromis.org.
- 40.Ferrans CE. Development of a quality of life index for patients with cancer. Oncol Nurs Forum. 1990;17(3):15–21. [PubMed] [Google Scholar]
- 41.Uchino BN. What a lifespan approach might tell us about why distinct measures of social support have differential links to physical health. J Soc Pers Relat. 2009;26:53–62. doi: 10.1177/0265407509105521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Zimet GD, Powell SS, Farley GK, Werkman S, Berkhoff KA. Psychometric characteristics of the multidimensional scale of perceived social support. J Pers Assess. 1990;55:610–617. doi: 10.1080/00223891.1990.9674095. [DOI] [PubMed] [Google Scholar]
- 43.Bradbury TN, Fincham FD, Beach SRH. Research on the nature and determinants of marital satisfaction: A decade in review. J Marriage Fam. 2000;62:964–980. [Google Scholar]
- 44.Software S. Version 9.4 of the SAS System for Windows. Cary, NC: Copyright 2013–2016 SAS Institute Inc. SAS and all other SAS Institute Inc. product or service names are registered trademarks or trademarks of SAS Institute Inc.; 2013–2016. [Google Scholar]
- 45.Waldron EA, Janke EA, Bechtel CF, Ramirez M, Cohen A. A systematic review of psychosocial interventions to improve cancer caregiver quality of life. Psycho-Oncol. 2013;22(6):1200–1207. doi: 10.1002/pon.3118. [DOI] [PubMed] [Google Scholar]
- 46.Rexilius SJ, Mundt C, Erickson Megel M. Therapeutic effects of massage therapy and handling touch on caregivers of patients undergoing autologous hematopoetic stem cell transplant. Oncol Nurs Forum. 2002;29:E35–44. doi: 10.1188/02.ONF.E35-E44. [DOI] [PubMed] [Google Scholar]
- 47.Cartledge Hoff A, Haaga DAF. Effects of an Education Program on Radiation Oncology Patients and Families. J Psychsoc Oncol. 2006;23(4):61–79. doi: 10.1300/j077v23n04_04. [DOI] [PubMed] [Google Scholar]
- 48.Cohen M, Kuten A. Cognitive–behavior group intervention for relatives of cancer patients: a controlled study. J Psychosom Res. 2006;61(2):187–196. doi: 10.1016/j.jpsychores.2005.08.014. [DOI] [PubMed] [Google Scholar]
- 49.Kurtz ME, Kurtz JC, Given CW, Given BA. Depression and physical health among family caregivers of geriatric patients with cancer - a longitudinal view. Med Sci Monitor. 2004;10(8):447–456. [PubMed] [Google Scholar]
- 50.Institute of Medicine. Retooling for an Aging America : Building the Health Care Workforce. National Academies Press; Washington, D.C.: 2008. [PubMed] [Google Scholar]
- 51.Burridge LH, Mitchell GK, Jiwa M, Girgis A. Consultation etiquette in general practice: a qualitative study of what makes it different for lay cancer caregivers. BMC Fam Pract. 2011;12(1):110–110. doi: 10.1186/1471-2296-12-110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Cronfalk BS, Strang P, Ternestedt BM. Inner power, physical strength and existential well-being in daily life: Relatives' experiences of receiving soft tissue massage in palliative home care. J Clin Nurs. 2009;18(15):2225–2233. doi: 10.1111/j.1365-2702.2008.02517.x. [DOI] [PubMed] [Google Scholar]
- 53.Wilkinson S, Lockhart K, Gambles M, Storey L. Reflexology for symptom relief in patients with cancer. Cancer Nurs. 2008;31(5):354–360. doi: 10.1097/01.NCC.0000305756.58615.81. [DOI] [PubMed] [Google Scholar]
- 54.McVicar AJ, Greenwood CR, Fewell F, et al. Evaluation of anxiety, salivary cortisol and melatonin secretion following reflexology treatment: A pilot study in healthy individuals. Complement Ther Clin Pract. 2007;13(3):137–145. doi: 10.1016/j.ctcp.2006.11.001. [DOI] [PubMed] [Google Scholar]
- 55.Stephenson N, Dalton J. Using reflexology for pain management. J Holist Nurs. 2003;21(4):179–191. doi: 10.1177/0898010103021002007. [DOI] [PubMed] [Google Scholar]
- 56.Wyatt G, Sikorskii A, Tesnjak I, Victorson D, Srkalovic G. Chemotherapy interruptions in relation to symptom severity in advanced breast cancer. Supportive Care in Cancer. 2015 Nov;23(11):3183–91. doi: 10.1007/s00520-015-2698-5. Epub 2015 Mar 25. [DOI] [PMC free article] [PubMed] [Google Scholar]