Abstract
Background
Vaginal brachytherapy (VBT), a common treatment for endometrial cancer (EC), is associated with high rates of vaginal stenosis. Recommendations for vaginal dilator use to minimize stenosis generally include 3 times per week for about 10 minutes per use. However, adherence rates range widely and are generally well below 50%.
Objectives
To assess feasibility of recruitment to a study of dilator use and test a theoretically driven enhanced educational program (EEP) to increase adherence.
Methods
Eligibility included women treated with post-operative VBT for stage I-IIIc EC. Patients were randomized to either nurse delivered standard institutional instruction (SII) or EEP.
Results
Of eligible patients, 76% consented, 42 were randomized and 69% completed the 6 month assessment. Mean age was 58.2 years; 48% were sexually active. There was no difference in adherence between arms. Overall, 20% and 8.3% were adherent to the prescribed 3 times per week use; and 64% and 16% were adherent to use at least once per week at 6 weeks and 6 months, respectively. Adherence was greater among those motivated by vaginal health and having lower body mass index. Non-adherence was significantly higher among college educated, EEP group, and with higher weight.
Conclusion
Feasibility of recruitment into a study of vaginal dilator use was high. Adherence was low and there was no difference between groups. Adherence to vaginal dilator use requires novel interventions to test.
Implications for Practice
Nursing education that includes how dilators may maintain vaginal health may improve use as it was a motivator for adherence in this study.
Keywords: Endometrial cancer, vaginal brachytherapy, vaginal dilator, vaginal stenosis, adherence, compliance
INTRODUCTION
Endometrial cancer is the number one gynecologic malignancy affecting women in the United States with an estimated 60,050 new cases diagnosed in 2016, and is most frequently diagnosed among women aged 45–74 with the medican age at diagnosis of 62 years.1 Most cases present in early stage (I–II) heralded by post-menopausal vaginal bleeding.2 Endometrial cancer is expected to increase in incidence due to the high and rising prevalence of obesity, one of the most common risk factors for the disease.3,4
The current approach to therapy for early-stage endometrial disease consists of surgery with adjuvant radiotherapy (RT) in selected cases to reduce locoregional recurrences.5,6,7 Adjuvant RT is usually delivered by vaginal brachytherapy (VBT), which is the insertion of a radioactive source directly into the vagina. Among patients treated with VBT, approximately 83% with Stage II and 68% with Stage III survive 5-years.8,9 VBT lead to symptoms of vaginal fibrosis, vaginal atrophy, lack of lubrication, vaginal dryness, and dyspareunia. These symptoms are associated with painful clinical examinations and sexual dysfunction including diminished desire, frequency of intercourse, arousal, ability to achieve orgasm, and sexual satisfaction.10–14 Despite advances in the treatment of endometrial cancer, little research has been done to understand the underlying mechanisms of exactly how RT affects the vagina and sexual function. The few older studies that exist indicate that vaginal RT denudes the vaginal epithelium by direct effect on the basal layer of the mucosa and on the fibroblasts of the connective tissue in the submucosa. Indirectly, vaginal mucosa is thought to be further devitalized by narrowing and obliteration of the small vessels and circumferential fibrosis (simultaneous decrease in vaginal length and width) clinically referred to as vaginal stenosis.15
The scarce research conducted in this underserved area has focused on clinical observations of the vagina and associations with patient reports of vaginal penetration, such as a vaginal dilator and/or penis, which are thought to prevent loss of vaginal length and impairment of sexual functioning following VBT. However, there is little empiric data to support this common wisdom. One retrospective chart review of 100 women treated for gynecologic malignancies with VBT found that dilator use two to three times per week was associated with a small but statistically significant decrease in clinical observations of vaginal stenosis.16
Thus, most clinical recommendations include insertion of a rigid dilator approximately 2–3 times per week to mechanically break up adhesions that begin as vaginal tissue starts to agglutinate at the apex.17,18 The recommendation is made regardless of sexual activity as maintaining a patent vagina is necessary for thorough and comfortable vaginal examinations. Yet, there are no reported prospective studies which assess whether vaginal dilators maintain vaginal length as assumed, what dose of dilator use is required to maintain vaginal length, nor the association among dilator use, vaginal length and sexual function.
The conduct of such studies are predicated on womens’ willingness to participate in sexual function research and to adhere with dilator use as prescribed. However, adherence rates vary widely across studies and non-adherence has been reported from 40% to 95%, with the frequency of dilator use for those who are compliant ranging from 1 to 4 times per week.18,19 According to the information-motivation-behavioral skills model, poor adherence may be related to the three main factors for which the model is named.20 Yet few published studies address information or education interventions to improve vaginal dilator use after cancer and only one published study addressed all three factors in this population. As would be predicted by the model, interventions addressing information without attending to motivation and behavioral skills have small or no effect on vaginal dilator adherence.21 The single study addressing all three factors, using a small groups psychoeducational intervention of two 2-hour group sessions over 1 or 2 weeks, delivered by a clinical psychologist and oncology nurse, showed statistically significant improvements in dilator adherence with the time and labor intensive experimental intervention over a standard education intervention. However, clinical significance was questionable given that by six months, only three women in the experimental group and one in the control group were dilating to prescription of three times per week; only five women were still dilating at least once per week by 12 months; and all had stopped by 18-month follow up.19
Thus, prior to design of a larger trial of vaginal dilator use and impact on vaginal length and sexual function, this pilot study sought to assess feasibility of recruitment into a study, and test a nurse led, one-on-one, enhanced education program, to improve adherence with vaginal dilator use 6 months post VBT for endometrial cancer.
METHODS
This study was designed as a pilot randomized trial to assess feasibility of recruitment into a trial testing vaginal dilator education methods and subsequent adherence with use. The primary aim was to establish feasibility of recruiting patients into a trial of vaginal dilator use and the secondary aim was assess preliminary efficacy of an enhanced educational program to improve adherence with vaginal dilator use. A tertiary aim is to assess sexual function using the validated Female Sexual Function Index22 and will be reported elsewhere. Feasibility of recruitment and adherence to vaginal dilators are required for future trials to assess maintenance of vaginal length and sexual function in larger trials.
This study received IRB approval at all participating sites and all patients enrolled provided informed consent. Participants were recruited from the practices of three radiation oncologists at two institutions (two at Northwestern University (NU) and one at the University of Pennsylvania (UP)). The study opened to accrual June 15, 2010 and closed April 30, 2013, with a 12 month hold on accrual from August 2011 to August 2012 due to relocation of the PI. One IRB mandated that all patients be re-consented because of the PIs move.
Patients were randomized to one of two nurse-delivered educational conditions: (1) standard institutional instruction (SII) for the use of a vaginal dilator; or (2) a theoretically guided, nurse led, one-on-one enhanced educational program (EEP) for vaginal dilator use with telephone follow-up. Group assignment was blinded to evaluating physicians, but not to the nurses. Block randomization was used to generate an a priori randomization sequence using a computer algorithm and sequential assignments.
Eligibility included women who underwent a hysterectomy and oophorectomy with/without lymphadenectomy for treatment of stage I-IIIc endometroid endometrial cancer. In addition, participants were required to have post-operative VBT and no prior history of external beam pelvic RT or chemotherapy.
Intervention
The EEP was developed in collaboration with a clinical psychologist (LH) based on the information-motivation-behavioral skills model of enhancing adherence with behavioral change related to risky sexual behaviors and adherence with therapy for HIV/AIDS.23–26 This model is an extension of the transtheoretical model of behavior change27 used in hundreds of studies of behavior change across chronic diseases and life style changes including sexual related activities. The information, motivation and behavioral skills were adapted to focus the intervention on reasons for, and practical use of, the vaginal dilator. In addition, cognitive behavioral techniques were employed to address potential barriers to use.
Professional training in the delivery of this educational component was done as one-on-one education between the principal investigator (PI) and the intervention-nurses at each site. EEP nurses were asked not to discuss the education session or any issues related to the education during the course of the study with the physician or the nurse providing the SII. Intervention nurse training included review of the EEP and the telephone intervention to discuss concerns and solutions to barriers interfering with vaginal dilator adherence. To assist with fidelity to the intervention a detailed instruction manual along with a script for phone calls and flip chart of pictures, and handouts for patients were provided to the intervention nurses. Additionally, monthly nurse phone and email contact with the PI and/or study coordinator focused on debriefings, concerns related to recruitment, intervention delivery, and solutions to barriers interfering with vaginal dilator adherence.
The study protocol made use of vaginal dilators which are standard of care, non-significant risk, non-FDA regulated devices used for the maintenance of vaginal patency after VBT for the treatment of endometrial, cervical, anal and rectal cancers. The vaginal dilators were all size small as manufactured by Syracuse Medical Devices, Inc, and were purchased by each institution and given to patients free of charge on both the standard of care and EEP arms.
Subjects randomized to the SII arm received instruction in vaginal dilator use according to the institution’s standard of practice. For NU standard care consisted of recommended dilator use beginning 4 weeks following VBT to be used 3–5 times per week for 10 minutes each use, for the rest of the patient’s life. For UP standard of care was similar with the following differences: recommended dilator use beginning 2–4 weeks following VBT, to be used 10–15 minutes 2 to 4 times in week 1, 5 times per week for weeks 2–24, and 2–3 times per week thereafter for life.
The EEP arm recommended dilator use starting 2 weeks following VBT for 10 minutes each use for the 6 month duration of the study and to continue with institutional standard care thereafter. Patients were instructed that penile penetration counts as one vaginal dilation and could supplement or replace dilator use in a given day. Instruction in dilator use was delivered during the patient’s scheduled VBT treatment visits. Sexual function questionnaires were completed at the time of each visit or mailed within 1–2 weeks of each study time point. Reminder telephone calls were made 5–7 days and again at 12 days after each visit if the questionnaires were not received. The EEP included nurse led follow-up phone calls at four time points: weeks 1, 4, 12, and 18 to assess adherence with dilator use and discuss concerns or questions. Patients on the SII arm received attention control calls at the same time points and were asked about two other side-effects of RT, diarrhea and bladder irritation.
Measures
Sociodemographic, sexual history and treatment factors at baseline were obtained from the medical record and supplemented by intervew. Sociodemographic factors included age, race, marital/co-habitation status, and education. Sexual history information related to sexual intercourse activity prior to diagnosis, vaginal dilation, and estrogen replacement use. BMI, alcohol use and smoking history were also documented as all have been associated with increased vaginal atrophy or interference with sexual function.28,29 Treatment factors include stage of disease, number, dose and method of delivery of VBT.
Feasibility of recruitment was calculated as the number of patients who consented to participate in the study divided by the number of eligible patients. Adherence was defined in two ways: (1) an indicator variable representing retention (remaining in the study for the full six months), and (2) a repeated indicator measure of adherence to protocol (any penetration ±3 times per week).
At the end of the SII or EEP, and again at 6 weeks and 6 months, the nurse obtained information via a brief, open ended interview related to the following broad categories: patient’s concerns, what would personally motivate them to comply with dilator use and what barriers they anticipated with adherence.
Statistical Analysis
Descriptive statistics were used to characterize continuous and categorical sociodemographic and clinical characteristics by intervention group. Sociodemographic, clinical characteristics, and attitudes (concerns, barriers, and motivators) were compared by retention using Fisher’s Exact tests and two sample t-tests for categorical and continuous variables, respectively.
Bivariate logistic regression models were used to assess the individual impact of intervention group, socio-demographic and clinical variables and attitudes expressed by at least 20% of the subjects to attrition. Similarly, bivariate generalized linear models were used to model weekly non-adherence (logistic distribution for dichotomous indicator for <3 times per week, any penetration) and activity use (Poisson distribution for number of times per week, any penetration) by intervention group, sociodemographic and clinical variables, and attitudes expressed by at least 20% of the subjects. Correlated outcomes at the site and subject level were modeled using an exchangeable covariance structure.
Targeted sample size was 58 patients based on Hertzog’s30 recommendations for feasibility aims which suggests a threshold of 25 participants per group for pilot studies involving direct estimation of a between-group effect size, with an additional 8 patients to account for 15% estimated attrition. Inferential analyses were performed acknowledging their limited power and ability to detect only large effects.
RESULTS
Patients screened, consented and analyzed are presented in the Figure. Fifty-eight patients were consented, however, one IRB mandated that all patients be re-consented because of the PIs move, and when this was done, 7 patients were then unable to be reached after multiple attempts to re-consent. Thus, in terms of feasibility of recruiting women to a study to improve adherence to vaginal dilators, forty-two patients were randomized and included in the analysis: twenty-four on the SII arm and eighteen to the EEP arm. At 6 months, twenty-one (88%) patients remained on the SII arm and eight (44%) on the EEP arm. Taking into account the study closure periods, an average of 3 and 2.76 patients were screened and consented per month, respectively, for an overall 76% consent rate of those eligible and an overall 69% of participants completing the 6 month primary endpoint.
Figure.
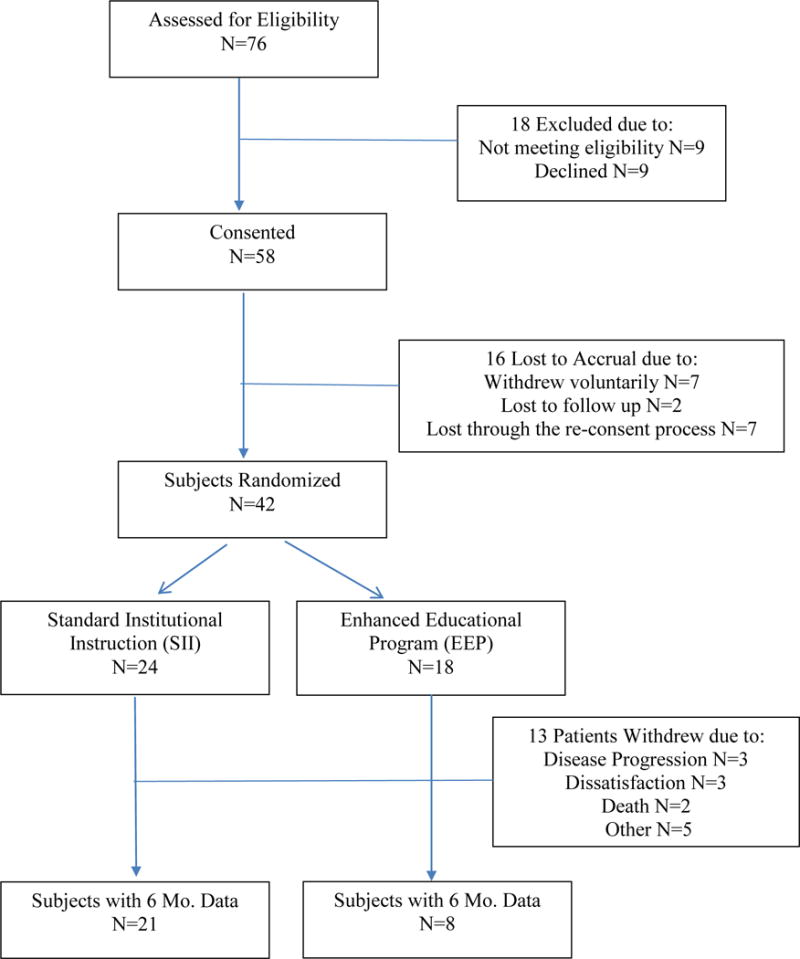
Flow Diagram of Study Recruitment and Retention
The mean age and BMI of the 42 patients randomized was 58.2 years and 31.4, respectively. The majority of patients were college educated (78.6%), white (76.2%), and non-smokers (85.7%). Nearly half (45.2%) of the patients were married, sexually inactive (50.0%), and 23.8% reported using a vaginal vibrator or dilator prior to their cancer diagnosis. The majority of patients (83.3%) were not on estrogen replacement therapy prior to cancer diagnosis, and 26.2% reported having a current or previous chronic illness. Over 95% of the patients presented with stage I disease and received VBT with either 3 fractions at 700 cGy or 4 fractions at 550 cGy. VBT was delivered with a vaginal cylinder and a standard technique.17 All patients underwent high-dose-rate (HDR) fractionated treatment based on the American Brachytherapy Society recommendations.31
Nurse led standard vaginal dilator education (SII Arm) took on average 18 minutes (minimum 10 minutes: maximum 25 minutes; median 15 minutes) whereas the enhanced education (EEP Arm) took on average 37 minutes (minimum 20 minutes: maximum 60 minutes; median 40 minutes). Nurses had difficulities reaching patients at four time points - weeks 1, 4, 12, and 18 and the mean number of follow-up calls where the patient was reached was 1.8 phone calls. Only 1% of subjects received all four follow-up calls and 1.4% were unable to be reached at any follow-up point. Forty-nine percent had a week 1 call, 49% had a week 4 call, 37% had a week 12 call, and 54% had a week 18 call.
There were no statistically significant differences between the arms for patient sociodemographic characteristics (Table 1). Although not statistically significant, patients randomized to the EEP intervention had a higher BMI than those randomized to SII (mean 29.5 vs. 34.0, p=.159).
Table 1.
Socio-Demographics, Clinical Characteristics, and Attitudes by Intervention (n=42)
| SII (n=24) n(%) |
EEP (n=18) n(%) |
Overall | ||
|---|---|---|---|---|
| Education | High School or lower | 5 (20.8) | 4 (22.2) | 9 (21.4) |
| College/Grad School | 19 (79.2) | 14 (77.8) | 33 (78.6) | |
| Race | White | 16 (66.7) | 16 (88.9) | 32 (76.2) |
| Black (African, Caribbean) | 6 (25.0) | 2 (11.1) | 8 (19.0) | |
| Asian | 2 (8.3) | 0 | 2 (4.8) | |
| Marital status | Never married | 6 (25.0) | 1 (5.5) | 7 (16.7) |
| Married/living with partner | 9 (37.5) | 10 (55.6) | 19 (45.2) | |
| Divorced/Separated | 7 (29.2) | 3 (16.7) | 10 (23.8) | |
| Widowed | 2 (8.3) | 4 (22.2) | 6 (14.3) | |
| Alcohol use over the past 30 days | None/Rarely | 20 (83.3) | 11 (61.1) | 31 (73.8) |
| 0–1 per day | 3 (12.5) | 5 (27.8) | 8 (19.0) | |
| 2 per day | 1 (4.2) | 2 (11.1) | 3 (7.1) | |
| Smoking (currently) | No | 20 (83.3) | 16 (88.9) | 36 (85.7) |
| Yes | 4 (16.7) | 2 (11.1) | 6 (14.3) | |
| Sexual activity prior to cancer diagnosis 1 | No | 12 (50.0) | 9 (50.0) | 21 (50.0) |
| Yes | 11 (45.8) | 9 (50.0) | 20 (47.6) | |
| No answer | 1 (4.2) | 0 | 1 (2.4) | |
| Vaginal dilation use prior to cancer diagnosis | No | 16 (66.7) | 15 (83.3) | 31 (73.8) |
| Yes | 7 (29.2) | 3 (16.7) | 10 (23.8) | |
| No answer | 1 (4.2) | 0 | 1 (2.4) | |
| Estrogen replacement therapy prior to cancer diagnosis | No | 20 (83.3) | 15 (83.3) | 35 (83.3) |
| Yes | 4 (16.7) | 3 (16.7) | 7 (16.7) | |
| Chronic Illness (current or previous) | No | 19 (79.2) | 12 (66.7) | 31 (73.8) |
| Yes | 5 (20.8) | 6 (33.3) | 11 (26.2) | |
| Stage | I | 22 (91.7) | 18 (100) | 40 (95.2) |
| II | 1 (4.2) | 0 | 1 (2.4) | |
| Radiation | 3 fractions × 400 cGy | 2 (8.3) | 0 | 2 (4.8) |
|
| ||||
| 3 fractions × 700 cGy | 6 (25.0) | 4 (22.2) | 10 (23.8) | |
| 4–5 fractions × 550 cGy | 16 (66.7) | 14 (77.8) | 30 (71.4) | |
|
| ||||
| Mean (SD) | Mean (SD) | Mean (SD) | ||
| Median (IQR) | Median (IQR) | Median IQR) | ||
| Age2 | 59.0 (10.3) | 57.1 (12.3) | 58.2 (11.0) | |
| 60 (12.0) | 59 (20.0) | 60 (16.0) | ||
| Weight | 171.0 (39.1) | 196.1 (67.4) | 181.8 (53.8) | |
| 177 (50.5) | 182.5 (67.0) | 180 (61.0) | ||
| Height | 64.4 (2.7) | 63.4 (4.3) | 64.0 (3.5) | |
| 65 (2.0) | 64 (2.0) | 64 (3.0) | ||
| BMI | 29.5 (7.7) | 34.0 (11.8) | 31.4 (9.8) | |
| 28.8 (9.7) | 34.8 (10.1) | 29.9 (11.2) | ||
|
| ||||
|
SII (n=24) N (%) |
EEP (n=18) N (%) |
|||
|
| ||||
| Concerns | Discomfort or pain | 1 (4.2) | 4 (22.2) | 5 (11.9) |
| Other | 1 (4.2) | 0 | 1 (2.4) | |
| Not specified | 1 (4.2) | 1 (5.6) | 2 (4.8) | |
| No concerns | 19 (79.2) | 12 (66.7) | 31 (73.8) | |
| Motivation | Vaginal health | 7 (29.2) | 4 (22.2) | 11 (26.2) |
| Prevent stenosis and scarring | 9 (37.5) | 8 (44.4) | 17 (40.5) | |
| Pain free | 1 (4.2) | 1 (5.6) | 2 (4.8) | |
| Other | 4 (16.7) | 4 (22.2) | 8 (19.0) | |
| No answer | 1 (4.2) | 0 | 1 (2.4) | |
| Barrier1 | Pain | 0 | 3 (16.7) | 3 (7.1) |
| Other | 0 | 1 (10.0) | 1 (2.4) | |
| No barriers | 22 (91.7) | 13 (72.2) | 35 (83.3) | |
| Institution | NU | 16 (66.7) | 14 (77.8) | 30(71.4) |
| Penn | 8 (33.3) | 4 (22.2) | 12 (28.6) | |
1 patient missing data in SII only;
3 patients missing data, 1 in SII, 2 in EEP.
A marginal difference between groups was observed for BMI p=.1596; a significant difference was observed for barriers to dilator use p=.0289. Abbreviations: EEP, Enhanced Educational Program; SII, Standard Institutional Instruction
In terms of adherence, there were no statistically significant differences between arms to prescribed 3 times per week or any dilator use at either the 6 week or 6 month timepoints. At 6 weeks, overall 20% of patients (both arms combined) were adherent to the prescribed 3 times per week vaginal dilator use; 15.8% of patients on SII arm and 33.3% of patients on the EEP arm. At 6 months, overall 8.3% of patients were adherent to the prescribed 3 times per week vaginal dilator use; 11.1% of patients on SII arm and 0 patients on the EEP arm, p =0.99). Adherence to any vaginal dilator use (at least once per week) at 6 weeks and 6 months was 64% (p=0.14) and 16% (p=0.99), respectively.
In general, patients did not express concerns about using the vaginal dilator. Motivators for use were maintenance of vaginal health (26.2%) and prevention of vaginal stenosis and scarring (40.5%). Only 3 patients reported pain as a barrier to use. Concerns and motivators for dilator use did not differ significantly by intervention (Table 1). Four patients expressed barriers to using the vaginal dilator (3 for pain), all of which were in the EEP group (p=.03).
Table 2 presents distributions of sociodemographic variables, clinical characteristics, and attitudes by retention. Sexual activity prior to diagnosis was the only clinical variable that approached statistical significance (p=.08), with 58.6% being sexually active in the retention group and 23.1% being sexually active among those that dropped out. Table 3 summarizes bivariate logistic regression model results for attrition. The odds of attrition are significantly higher among those with a college education [OR: 4.51; 95% CI: (1.93–10.53)], black [OR: 1.47; 95% CI: (1.37–1.58)], not married [OR: 1.45; 95% CI: (1.35–1.55)], sexually inactive [OR: 4.08; 95% CI: (1.08–15.38)], chronically ill [OR: 1.40; 95% CI: (1.18–1.66)], those with higher BMI [OR: 1.06; 95% CI: (1.04–1.09)] and receiving the EEP intervention [OR: 8.78; 95% CI: (7.80–9.89)].
Table 2.
Socio-Demographics, Clinical Characteristics, and Attitudes by Retention
| Retained (n=29)† n(%) | Dropped Out (n=13) n(%) | Overall (n=42) n(%) | ||
|---|---|---|---|---|
| Age mean (SD) median (IQR)2 |
59.2 (10.6) 62 (14.0) |
55.4 (12.4) 55 (19.0) |
58.2 (11.0) 60 (16.0) |
|
| Education | High School or lower | 8 (27.6) | 1 (7.7) | 9 (21.4) |
| College/Grad School | 21 (72.4) | 12 (92.3) | 33 (78.6) | |
| Race | White | 22 (75.9) | 10 (76.9) | 32 (76.2) |
| Black /Asian | 7 (24.1) | 3 (23.1) | 10 (23.8) | |
| Marital status | Married/living with partner | 14 (48.3) | 5(38.5) | 19 (45.2) |
| divorced/separated/widowed/never married | 15 (51.7) | 8 (61.5) | 23 (54.8) | |
| Alcohol use over the past 30 days | None/Rarely | 21 (72.4) | 10 (76.9) | 31 (73.8) |
| 0–2 per day | 8 (27.6) | 3 (23.1) | 11 (26.2) | |
| Smoking (currently) | No | 25 (86.2) | 11 (84.6) | 36 (85.7) |
| Yes | 4 (13.8) | 2 (15.4) | 6 (14.3) ( | |
| Sexual activity prior to cancer diagnosis3,4 | No | 12 (41.4) | 9 (69.2) | 21 (50.0) |
| Yes | 17 (58.6) | 3 (23.1) | 20 (47.6) | |
| Vaginal dilation use prior to cancer diagnosis1 | No | 22 (75.9) | 9 (69.2) | 31 (73.8) |
| Yes | 6 (20.7) | 4 (30.8) | 10 (23.8) | |
| Estrogen replacement therapy prior to cancer diagnosis | No | 24 (82.8) | 11 (84.6) | 35 (83.3) |
| Yes | 5 (17.2) | 2 (15.4) | 7 (16.7) | |
| Chronic Illness (current or previous) | No | 22 (75.9) | 9 (69.2) | 31 (73.8) |
| Yes | 7 (24.1) | 4 (30.8) | 11 (26.2) | |
| Stage | I | 28 (96.6) | 12 (92.3) | 40 (95.2) |
| II | 1 (3.4) | 0 | 1 (2.4) | |
| Radiation | 3 fractions × 400 cGy | 1 (3.4) | 1 (7.7) | 2 (4.8) |
| 3 fractions × 700 cGy | 8 (27.6) | 2 (15.4) | 10 (23.8) | |
| 4 fractions × 550 cGy | 20 (69.0) | 10 (76.9) | 30 (71.4) | |
| BMI mean (SD) median (IQR) |
29.7 (7.0) 29.3 (8.5) |
35.3 (13. 8) 36.1 (16.5) |
31.4 (9.8) 29.9 (11.2) |
|
| Concerns | Discomfort or pain | 4 (13.8) | 1 (7.7) | 5 (11.9) |
| Other | 1 (3.5) | 0 | 1 (2.4) | |
| Not specified | 0 | 2 (15.4) | 2 (4.8) | |
| No concerns | 22 (75.9) | 9 (69.2) | 31 (73.8) | |
| Motivation | Vaginal health | 7 (24.1) | 4 (30.8) | 11 (26.2) |
| Prevent sclerosis and scarring | 13 (44.8) | 4 (30.8) | 17 (40.5) | |
| Pain free | 2 (6.9) | 0 | 2 (4.8) | |
| Other | 5 (17.2) | 3 (23.1) | 8 (19.0) | |
| Barrier | Pain | 2 (6.9) | 1 (7.7) | 3 (7.1) |
| Other | 0 | 1 (7.7) | 1 (2.4) | |
| No barriers | 25 (86.2) | 10 (76.9) | 35 (83.3) | |
| Institution | NU | 20 (69.0) | 10 (76.9) | 30 (71.4) |
| Penn | 9 (31.0) | 3 (23.1) | 12 (28.6) |
1 patient missing data in SII only;
3 patients missing data, 1 in SII, 2 in EEP.
A significant difference was observed for sexual activity prior to diagnosis p=.0855.
n(%) presented for categorical variables, mean (SD) and median (IQR) presented for continuous variables age and BMI. Abbreviations: IQR, Interquartile range; SD, standard deviation
Table 3.
Bivariate Logistic Regression Model Results for Attrition1 (N=42)
| Variables | OR (95% CI) | p |
|---|---|---|
| Education (reference: No college) | ||
| Attend college | 4.51 (1.93–10.53) | 0.0005 |
| Race (reference: White) | ||
| Black | 1.47 (1.37–1.58) | <.0001 |
| Marital Status (reference: Married) | ||
| Not married currently | 1.45 (1.35–1.55) | <.0001 |
| Alcohol (reference: No) | ||
| Yes | 0.72 (0.42–1.22) | 0.2212 |
| Smoke (reference: No) | ||
| Yes | 1.21 (0.85–1.72) | 0.2882 |
| Sexual activity (reference: Yes) | ||
| No | 4.08 (1.08–15.38) | 0.0376 |
| Vaginal Dilation (reference: No) | ||
| Yes | 1.48 (0.68–3.23) | 0.3214 |
| Estrogen Use (reference: No) | ||
| Yes | 0.88 (0.26–2.92) | 0.8285 |
| Chronic illness (reference: No) | ||
| Yes | 1.40 (1.18–1.66) | 0.0001 |
| Group (reference: SII) | ||
| EEP | 8.78 (7.80–9.89) | <.0001 |
| Motivation for ‘Vaginal health’ Pre-interview (reference: No) |
||
| Yes | 1.47 (0.54–3.97) | 0.4517 |
| Motivation for Prevent stenosis and scarring Pre-interview (reference: No) | ||
| Yes | 0.64 (0.20–2.02) | 0.4420 |
| Age | 0.97 (0.92–1.02) | 0.2926 |
| Weight | 1.01 (1.00–1.01) | <.0001 |
| Height | 0.93 (0.91–0.95) | <.0001 |
| BMI | 1.06 (1.04–1.09) | <.0001 |
Note: OR=Exp(β)
Attrition = dropout or not retained through 6 months, n=13 subjects dropped out. Stage and of method of VBT were not considered in regression models because of limited variability (ie, more than 90% of the patients were in a single category).
Table 4 summarizes bivariate GEE logistic regression model results for non-adherence as defined by a dichotomous indicator variable for weekly penetration of less than three times per week. Among the 29 patients completing the study, the odds of non-adherence were significantly less among those using estrogen [OR: 0.35; 95% CI: (0.13–0.96)] and significantly higher among those with higher weight [OR: 1.02; 95% CI: (1.01–1.03)]. Among all 42 patients enrolled, the odds of non-adherence were significantly higher among those in the EEP intervention group [OR: 3.21; 95% CI: (1.12–9.17)] and those with higher weight [OR: 1.01; 95% CI: (1.00–1.03)].
Table 4.
Bivariate GEE Model Results for Non-Adherence (N=29)
| Variables | Patients Retained (N=29) | All Randomized Patients (N=42) | ||
|---|---|---|---|---|
| OR (95% CI) | p | OR (95% CI) | p | |
| Education (reference: No college) | ||||
| Attend college | 1.61 (0.53–4.87) | 0.4017 | 2.55 (0.84–7.78) | 0.1003 |
| Race (reference: White) | ||||
| Black | 2.43 (0.76–7.84) | 0.1364 | 2.35 (0.68–8.09) | 0.1758 |
| Marital Status (reference: Married) | ||||
| Not married currently | 0.62 (0.24–1.56) | 0.3069 | 0.83 (0.32–2.11) | 0.6880 |
| Alcohol (reference: No) | ||||
| Yes | 1.34 (0.55–3.23) | 0.5174 | 1.13 (0.43–2.92) | 0.8078 |
| Smoke (reference: No) | ||||
| Yes | 2.59 (0.94–7.16) | 0.0658 | 2.31 (0.72–7.38) | 0.1577 |
| Sexual activity (reference: Yes) | ||||
| No | 1.47 (0.56–3.85) | 0.4382 | 2.47 (0.94–6.48) | 0.0670 |
| Vaginal Dilation (reference: No) | ||||
| Yes | 0.85 (0.25–2.94) | 0.8013 | 1.13 (0.34–3.77) | 0.8394 |
| Estrogen Use (reference: No) | ||||
| Yes | 0.35 (0.13–0.96) | 0.0407 | 0.45 (0.14–1.49) | 0.1934 |
| Chronic illness (reference: No) | ||||
| Yes | 1.28 (0.43–3.84) | 0.6579 | 1.41 (0.47–4.29) | 0.5412 |
| Group (reference: SII) | ||||
| EEP | 1.21 (0.42–3.48) | 0.7209 | 3.21 (1.12–9.17) | 0.0296 |
| Motivation for ‘Vaginal health’ Pre-interview (reference: No) |
||||
| Yes | 0.70 (0.34–1.43) | 0.3310 | 0.96 (0.37–2.50) | 0.9373 |
| Motivation for Prevent stenosis and scarring Pre-interview (reference: No) | ||||
| Yes | 1.05 (0.40–2.78) | 0.9170 | 0.65 (0.32–2.29) | 0.7494 |
| Age | 1.01 (0.96–1.05) | 0.8097 | 0.99 (0.94–1.04) | 0.7159 |
| Weight | 1.02 (1.01–1.03) | 0.0012 | 1.01 (1.00–1.03) | 0.0145 |
| Height | 1.14 (0.99–1.31) | 0.0741 | 1.03 (0.89–1.19) | 0.6866 |
| BMI | 1.07 (0.99–1.16) | 0.0872 | 1.07 (1.00–1.14) | 0.0422 |
Note: OR=Exp(β). Stage and of method of VBT were not considered in regression models because of limited variability (ie, more than 90% of the patients were in a single category).
In bivariate Poisson models (data not shown), weekly activity (count of any vaginal dilator or penile penetration) is significantly greater among those using estrogen, motivated by vaginal health, and having lower weight and BMI. The weekly profile of activity as defined by any penetration did not differ significantly by intervention group (data not shown).
DISCUSSION
Women treated for early to intermediate stage endometrial with VBT have high survival rates meaning they will be left to live with vaginal symptoms and sexual dysfunction. To minimize radiation related vaginal stenosis, standard practice is to prescribe vaginal dilators about three times per week. This is an invasive and intimate procedure that could be prescribed for years to life for which there is little empirical data. The data that does exist suggests possible decreased risk of stenosis for those who use dilators, however studies also report low rates of adherence with prescribed dilator use.
The current pilot study sought to assess feasibility of recruitment and to test an enhanced educational program to improve adherence with dilator use in preparation for a larger trial of vaginal dilators. Feasibility in terms of recruitment was high with 76% of eligible patients consenting to participate. However, despite attempts at telephone follow-up, attrition was also high with a higher than anticipated attrition rate of 31% of participants not completing the 6 month primary endpoint. Sexual activity prior to diagnosis was the only clinical variable that approached statistical significance for predicating retention, with those who were sexually active being two and half times more likely to complete the study.
The study also assessed preliminary efficacy of a theoretically guided EEP to improve patient adherence with vaginal dilators. Overall, adherence with as prescribed 3 times per week vaginal dilator use was lower than previous reports in the literature but any dilator use compared favorably to the literature.16,18,19 Overall 20% and 8.3% of patients (both arms combined) were adherent to the prescribed 3 times per week vaginal dilator use; and 64% and 16% were adherent to use at least once per week at 6 weeks and 6 months, respectively. However, there was no difference with adherence between nurse-led standard of care (a one page hand out provided by the nurse) and the multi-component enhanced educational intervention. There may be several reasons for this which also present limitations of the study including the small sample size and high dropout rate on the EEP arm. In addition, the current study eligibility included patients sexually active and sexually inactive, as dilator use is prescribed in both instances, but many previous studies only included sexually active patients. Further, while we sought to prevent contamination of the intervention by not sharing the intervention delivered by intervention nurses with the usual care nurses, there may have been enough overlap to prevent detection of significant differences. Future studies may seek to video tape usual nursing care and experimental interventions to assess/ensure significant differnces between methods.
Vaginal dilator non-adherence was significantly higher among those with a college education, with a higher weight, and in the EEP intervention group. Conversely, being motivated by vaginal health and having lower weight are independent predictors of higher dilator or penile penetration activity. Higher education as a predictor of non-adherence is difficult to explain, however, national surveys do show differences in sexual behaviors by education.32 On the other hand, increased weight or BMI is consistently documented as interfering with aspects of sexual activity.33–35 All patients in this study were over-weight (BMI ±25 kg/m2) and most were obese (BMI ±30 kg/m2) and a quarter had other chronic illnesses, all of which may be moderators of motivation and dilator use and attenuate the effects of educational method.
While it may seem scientifically sound to approach further interventions with more complex multi-faceted approaches to increase adherence, for example adding a weight loss intervention, it has been shown that there is a curvilinear relation between the number of behavioral recommendations and improvements in behavior, with a moderate number of recommendations producing the highest level of change.36 Yet, even the very singular recommendation in this study of dilation three times per week did not yield the desired results, possibly indicating adherence to something as intimate as dilator use, especially to sexually inactive patients, may add an additional layer of complexity for even theory driven interventions.
Overall, 73% of women in this study reported no concerns and 83% reported no barriers to adherence, yet adherence remained low. Two recent qualitative studies sought to shed light on barriers to dilator use. One study included 30 women prescribed vaginal dilators after radiotherapy for gynecologic cancer. Patients listed lack of time or privacy, forgetting, or feeling tired as reasons for nonadherence. Additionally, negative emotions such as dilator’s hard plastic design, anticipatory fear of pain or blood loss, and an association with the radiotherapy were deterents to use.37 Our EEP informational, motivational and behavioral skills component addressed each of these issues, yet did not increase adherence over SII. Alternatley, a study of ten women with a history of gynecologic cancer who were prescribed vaginal dilators found the overarching theme of the womens’ experiences was covered by what the authors labled, “from ‘sex toy’ to intrusive imposition.” There were five main categories under this theme that women reported as their feelings and attitudes toward vaginal dilators/dilatation: embarrassing sex toy; reliving the invasion of treatment; aversive “hands-on” experience; not at the forefront of my recovery; and minimizing the resistance.38 While it is possible these feelings played some role in the level of adhenrence in this study, over all women reported few similar concerns.
The main concern voiced by women in this study was pain or discomfort which was reported by only 12% of women, however it was not an independent predictor of non-adherence. Thus, while negative feelings may play a significant role in non-adherence for women, in this study it was not psychological factors that predicted adherence, possibly because they were addressed formally in the EEP, and, hypothetically, informally through good nursing care in the SII, although the later was not assessed in this study. Rather the physical characteristic of being overweight, which was not addressed in either the SII or the EEP, was the main factor that was both predictive of non-adherence and not addressed by the intervention.
Conclusion/Implications for Practice
This pilot study suggests that recruiting women into a study of vaginal dilator use is feasible. The study also provides realistic estimates of attrition that may help guide future research sample size calculations. Since pre-VBT sexual activity is the only predictor of study retention, including this as eligibility criteria for future studies may be reasonable in terms of research, but would abandon assessments of ways to improve use in non-sexually active women in need of a patent vagina for vaginal examinations. This study also provides dilator adherence rates, which seem concordant with the literature across a number of standard of care chart reviews, psychoeducational or educational interventions for overall use, but lower for prescribed 3 times per week use. Patient eligibility, metrics for “as prescribed” and ranges of dilator use vary widely and no study in the literature to date reports improved adherence above 50% at timepoints less than one year. All this indicates a pressing need for novel methods to improve dilator use (and subsequent sexual function and quality of life) after VBT in endometrial cancer survivors.
Implications for clinical practice suggest that usual nursing care with written instructions and free provision of dilators may be equivalent to more intensive interventions as described in the literature and in the current study. However, while the study sought to formally include information-motivation and behavioral skills components, it is likely that good nursing care covers many of these issues, and should not be abandoned. However, neither option improves adherence to more optimal rates that may be required for maintaining vaginal patency or sexual function. Results suggest that optimizing nursing education to include how vaginal dilators may maintain vaginal health may improve use, as it was a predictive motivator for adherence in this study. Further, recommending healthy behaviors that promote weight loss for obese patients may improve a myriad of positive outcomes, including dilator adherence.
Acknowledgments
This study was supported by a grant from the National Cancer Institute 1R21CA140766-01
Footnotes
The authors have no conflicts of interest to disclose.
References
- 1.SEER Stat Fact Sheets: Endometrial Cancer. 2016 http://seer.cancer.gov/statfacts/html/corp.html. Accessed February 3, 2016.
- 2.Ries L, Melbert D, Krapcho M, et al. SEER cancer statistics review, 1975–2005. Vol. 2008. Bethesda, MD: National Cancer Institute; pp. 1975–2005. [Google Scholar]
- 3.Modesitt SC, van Nagell JR., Jr The impact of obesity on the incidence and treatment of gynecologic cancers: a review. Obstetrical & gynecological survey. 2005;60(10):683–692. doi: 10.1097/01.ogx.0000180866.62409.01. [DOI] [PubMed] [Google Scholar]
- 4.Rieck G, Fiander A. The effect of lifestyle factors on gynaecological cancer. Best Practice & Research Clinical Obstetrics & Gynaecology. 2006;20(2):227–251. doi: 10.1016/j.bpobgyn.2005.10.010. [DOI] [PubMed] [Google Scholar]
- 5.Kellas-Sléczka S, Wojcieszek P, Białas B. Adjuvant vaginal brachytherapy as a part of management in early endometrial cancer. Journal of contemporary brachytherapy. 2012;4(4):247–252. doi: 10.5114/jcb.2012.32560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Creutzberg CL, van Putten WL, Koper PC, et al. Surgery and postoperative radiotherapy versus surgery alone for patients with stage-1 endometrial carcinoma: multicentre randomised trial. PORTEC Study Group. Post Operative Radiation Therapy in Endometrial Carcinoma. Lancet. 2000;355(9213):1404–1411. doi: 10.1016/s0140-6736(00)02139-5. [DOI] [PubMed] [Google Scholar]
- 7.Keys HM, Roberts JA, Brunetto VL, et al. A phase III trial of surgery with or without adjunctive external pelvic radiation therapy in intermediate risk endometrial adenocarcinoma: a Gynecologic Oncology Group study. Gynecol Oncol. 2004;92(3):744–751. doi: 10.1016/j.ygyno.2003.11.048. [DOI] [PubMed] [Google Scholar]
- 8.Cozad SC. Stage II adenocarcinoma of the endometrium: adjuvant radiotherapy and recurrence patterns. International journal of radiation oncology, biology, physics. 2008;71(1):205–212. doi: 10.1016/j.ijrobp.2007.09.022. [DOI] [PubMed] [Google Scholar]
- 9.Patel S, Portelance L, Gilbert L, et al. Analysis of prognostic factors and patterns of recurrence in patients with pathologic stage III endometrial cancer. International journal of radiation oncology, biology, physics. 2007;68(5):1438–1445. doi: 10.1016/j.ijrobp.2007.02.003. [DOI] [PubMed] [Google Scholar]
- 10.Bergmark K, Åvall-Lundqvist E, Dickman PW, Henningsohn L, Steineck G. Vaginal changes and sexuality in women with a history of cervical cancer. New England Journal of Medicine. 1999;340(18):1383–1389. doi: 10.1056/NEJM199905063401802. [DOI] [PubMed] [Google Scholar]
- 11.Bruner DW, Lanciano R, Keegan M, Corn B, Martin E, Hanks GE. Vaginal stenosis and sexual function following intracavitary radiation for the treatment of cervical and endometrial carcinoma. International journal of radiation oncology, biology, physics. 1993;27(4):825–830. doi: 10.1016/0360-3016(93)90455-5. [DOI] [PubMed] [Google Scholar]
- 12.Flay LD, Matthews JH. The effects of radiotherapy and surgery on the sexual function of women treated for cervical cancer. International Journal of Radiation Oncology* Biology* Physics. 1995;31(2):399–404. doi: 10.1016/0360-3016(94)E0139-B. [DOI] [PubMed] [Google Scholar]
- 13.Jensen PT, Froeding LP. Pelvic radiotherapy and sexual function in women. Translational Andrology and Urology. 2015;4(2):186–205. doi: 10.3978/j.issn.2223-4683.2015.04.06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Seibel MM, Freeman MG, Graves WL. Carcinoma of the cervix and sexual function. Obstetrics and gynecology. 1980;55(4):484–487. [PubMed] [Google Scholar]
- 15.Abitbol MM, Davenport JH. The irradiated vagina. Obstetrics and gynecology. 1974;44(2):249–256. [PubMed] [Google Scholar]
- 16.Bahng AY, Dagan A, Bruner DW, Lin LL. Determination of prognostic factors for vaginal mucosal toxicity associated with intravaginal high-dose rate brachytherapy in patients with endometrial cancer. International Journal of Radiation Oncology* Biology* Physics. 2012;82(2):667–673. doi: 10.1016/j.ijrobp.2010.10.071. [DOI] [PubMed] [Google Scholar]
- 17.Nag S, Erickson B, Parikh S, Gupta N, Varia M, Glasgow G. The American Brachytherapy Society recommendations for high-dose-rate brachytherapy for carcinoma of the endometrium. International journal of radiation oncology, biology, physics. 2000;48(3):779–790. doi: 10.1016/s0360-3016(00)00689-1. [DOI] [PubMed] [Google Scholar]
- 18.Robinson JW, Faris PD, Scott CB. Psychoeducational group increases vaginal dilation for younger women and reduces sexual fears for women of all ages with gynecological carcinoma treated with radiotherapy. International Journal of Radiation Oncology* Biology* Physics. 1999;44(3):497–506. doi: 10.1016/s0360-3016(99)00048-6. [DOI] [PubMed] [Google Scholar]
- 19.Jeffries SA, Robinson JW, Craighead PS, Keats MR. An effective group psychoeducational intervention for improving compliance with vaginal dilation: a randomized controlled trial. International journal of radiation oncology, biology, physics. 2006;65(2):404–411. doi: 10.1016/j.ijrobp.2005.12.009. [DOI] [PubMed] [Google Scholar]
- 20.Fisher JD, Fisher WD. The information-motivation behavioral skills model. In: DiClemente RJ, Crosby RA, Kegler MC, editors. Emerging Theories in Health Promotion Practice and Research: Strategies for Improving Public Health. Indianapolis, IN: Jossey-Bass, Inc.; 2002. [Google Scholar]
- 21.Brand AH, Do V, Stenlake A. Can an educational intervention improve compliance with vaginal dilator use in patients treated with radiation for a gynecological malignancy? Int J Gynecol Cancer. 2012;22(5):897–904. doi: 10.1097/IGC.0b013e31824d7243. [DOI] [PubMed] [Google Scholar]
- 22.Rosen R, Brown C, Heiman J, et al. The Female Sexual Function Index (FSFI): a multidimensional self-report instrument for the assessment of female sexual function. J Sex Marital Ther. 2000;26(2):191–208. doi: 10.1080/009262300278597. [DOI] [PubMed] [Google Scholar]
- 23.Bryan AD, Fisher JD, Fisher WA, Murray DM. Understanding condom use among heroin addicts in methadone maintenance using the information-motivation-behavioral skills model. Subst Use Misuse. 2000;35(4):451–471. doi: 10.3109/10826080009147468. [DOI] [PubMed] [Google Scholar]
- 24.Fisher JD, Fisher WA, Misovich SJ, Kimble DL, Malloy TE. Changing AIDS risk behavior: effects of an intervention emphasizing AIDS risk reduction information, motivation, and behavioral skills in a college student population. Health Psychology. 1996;15(2):114. doi: 10.1037//0278-6133.15.2.114. [DOI] [PubMed] [Google Scholar]
- 25.Fisher JD, Fisher WA, Williams SS, Malloy TE. Empirical tests of an information-motivation-behavioral skills model of AIDS-preventive behavior with gay men and heterosexual university students. Health Psychol. 1994;13(3):238–250. doi: 10.1037//0278-6133.13.3.238. [DOI] [PubMed] [Google Scholar]
- 26.Fisher JD, Fisher WA, Misovich SJ, Kimble DL, Malloy TE. Changing AIDS risk behavior: effects of an intervention emphasizing AIDS risk reduction information, motivation, and behavioral skills in a college student population. Health psychology : official journal of the Division of Health Psychology, American Psychological Association. 1996;15(2):114–123. doi: 10.1037//0278-6133.15.2.114. [DOI] [PubMed] [Google Scholar]
- 27.Prochaska JO, DiClemente CC. Toward a comprehensive model of change. Springer; 1986. [Google Scholar]
- 28.Addis IB, Ireland CC, Vittinghoff E, Lin F, Stuenkel CA, Hulley S. Sexual activity and function in postmenopausal women with heart disease. Obstetrics and gynecology. 2005;106(1):121–127. doi: 10.1097/01.AOG.0000165276.85777.fb. [DOI] [PubMed] [Google Scholar]
- 29.Kalogeraki A, Tamiolakis D, Relakis K, et al. Cigarette smoking and vaginal atrophy in postmenopausal women. In Vivo. 1996;10(6):597–600. [PubMed] [Google Scholar]
- 30.Hertzog MA. Considerations in determining sample size for pilot studies. Research in nursing & health. 2008;31(2):180–191. doi: 10.1002/nur.20247. [DOI] [PubMed] [Google Scholar]
- 31.Small W, Jr, Beriwal S, Demanes DJ, et al. American Brachytherapy Society consensus guidelines for adjuvant vaginal cuff brachytherapy after hysterectomy. Brachytherapy. 2012;11(1):58–67. doi: 10.1016/j.brachy.2011.08.005. [DOI] [PubMed] [Google Scholar]
- 32.Herbenick D, Reece M, Schick V, Sanders SA, Dodge B, Fortenberry JD. Sexual behavior in the United States: results from a national probability sample of men and women ages 14–94. The journal of sexual medicine. 2010;7(s5):255–265. doi: 10.1111/j.1743-6109.2010.02012.x. [DOI] [PubMed] [Google Scholar]
- 33.Bond DS, Vithiananthan S, Leahey TM, et al. Prevalence and degree of sexual dysfunction in a sample of women seeking bariatric surgery. Surgery for Obesity and Related Diseases. 2009;5(6):698–704. doi: 10.1016/j.soard.2009.07.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Poggiogalle E, Di Lazzaro L, Pinto A, Migliaccio S, Lenzi A, Donini LM. Health-related quality of life and quality of sexual life in obese subjects. International journal of endocrinology. 2014;2014 doi: 10.1155/2014/847871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Smits A, Lopes A, Bekkers R, Galaal K. Body mass index and the quality of life of endometrial cancer survivors—a systematic review and meta-analysis. Gynecologic oncology. 2015;137(1):180–187. doi: 10.1016/j.ygyno.2015.01.540. [DOI] [PubMed] [Google Scholar]
- 36.Wilson K, Senay I, Durantini M, et al. When it comes to lifestyle recommendations, more is sometimes less: A meta-analysis of theoretical assumptions underlying the effectiveness of interventions promoting multiple behavior domain change. Psychological bulletin. 2015;141(2):474. doi: 10.1037/a0038295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Bakker RM, Vermeer WM, Creutzberg CL, Mens JW, Nout RA, Ter Kuile MM. Qualitative accounts of patients’ determinants of vaginal dilator use after pelvic radiotherapy. J Sex Med. 2015;12(3):764–773. doi: 10.1111/jsm.12776. [DOI] [PubMed] [Google Scholar]
- 38.Cullen K, Fergus K, Dasgupta T, Fitch M, Doyle C, Adams L. From “sex toy” to intrusive imposition: a qualitative examination of women’s experiences with vaginal dilator use following treatment for gynecological cancer. J Sex Med. 2012;9(4):1162–1173. doi: 10.1111/j.1743-6109.2011.02639.x. [DOI] [PubMed] [Google Scholar]


