Abstract
Similar to same-age peers, perinatally HIV-infected (PHIV+) youth in the US are engaging in sex, including condomless sex. Understanding decisions about serostatus disclosure to sexual partners is important to domestic and global HIV prevention efforts, since large numbers of PHIV+ children are entering adolescence and becoming sexually active. Using Social Action Theory (SAT) to inform variable selection, we examined correlates of disclosure among 98 PHIV+ adolescents/young adults in New York City. Over half of these youth reported not disclosing to any casual partners (59%) and to any partners when using condoms (55%). In simple regression analyses, increased disclosure was associated with older age; being female; earlier age of learning one’s serostatus; and increased STD knowledge, disclosure intentions, and parent-child communication. Multiple regression analyses revealed a strong fit with the SAT model. As with adults, disclosure to sexual partners is difficult for PHIV+ youth and challenges prevention efforts. Effective interventions that help youth with disclosure decisions are needed to curb the epidemic.
Keywords: Perinatal HIV, disclosure, sexual partners, adolescence, young adulthood
INTRODUCTION
With advances in antiretroviral treatment (ART) and medical care, new perinatal HIV infections are increasingly rare in the United States (US). However, infants who acquired perinatal HIV-infection (PHIV+) earlier in the US epidemic are surviving into adolescence and young adulthood and becoming sexually active. Although some studies suggest that PHIV+ youth may have delayed onset of sexual activity compared to the general population (1), others indicate that some youth may have early onset of sexual intercourse (2). In addition, as they become older, PHIV+ youth engage in sexual risk behaviors similar to their peers, including having sex without a condom and sex with multiple partners (2–5). Moreover, adolescents and young adults have particular difficulty with consistent adherence to medication regimens (6–10). Thus, for PHIV+ youth – who struggle with adherence in the context of life-long HIV infection – engaging in condomless sex may be associated with a significant risk of transmitting HIV, including drug resistant strains of the virus (5, 11).
Understanding determinants of sexual risk behaviors in populations living with HIV has been key to creating specialized health programs and prevention interventions (12–14). Among adults, disclosure of HIV status to partners is an important component of prevention (15, 16). It represents a critical moment in a romantic and/or sexual relationship that can foster further communication about safer sex and avoidance of risk behaviors. Disclosure by a person living with HIV (PLWHIV) may encourage a partner to undergo testing, use prevention strategies such as condoms and pre-exposure prophylaxis (PrEP), and engage in care/treatment if needed.
However, disclosure is also risky and carries a threat of rejection, humiliation, and even violence (17, 18). Given the individual and societal attitudes towards HIV and the potential negative social repercussions of disclosure, particularly within the context of a sexual relationship (19), it is a difficult and sensitive subject for PLWHIV. Young people, who are often focused on “being normal” and “fitting in,” may avoid disclosure altogether (20, 21). Studies published to date have not systematically investigated how often, to whom, and in what situations PHIV+ youth disclose their status to sexual partners, nor have they explored theoretically informed correlates of disclosure in this population. Three small (N=12–55) existing investigations indicate that a number of PHIV+ youth choose to not disclose. Proportions of youth reporting disclosing to at least one partner ranged from 68% (22) to only 21% (23). Proportions reporting disclosing to first sexual partner (5) and to current partner (22) were low, 33% and 40%, respectively. The finding that PHIV+ youth were less than half as likely as behaviorally infected youth to have disclosed to someone (partners, as well as friends and family) (24) is particularly concerning given the higher likelihood of PHIV+ youth having unsuppressed viral load (7).
In the broader disclosure literature, a number of factors have been associated with disclosure. Sexual situation is one variable that has consistently been shown to affect disclosure to partners. For instance, behaviorally infected youth are less likely to disclose to casual than to steady partners (25, 26) and more likely to disclose when engaging in condomless sex (25). Among both behaviorally infected young adults and adult men who have sex with men, having fewer sexual partners is associated with more serostatus disclosure (20, 27). Stigma has also been shown to strongly influence disclosure (28). For instance, fear of stigma-related violence has been shown to be a major deterrent to disclosure among HIV+ women in the US (17, 18). Related, PHIV+ teenagers and young adults have cited fear of rejection and misunderstanding of the cause of infection as reasons for nondisclosure (22, 29). In a small qualitative study, some PHIV+ teens reported that their HIV+ caregivers encouraged them to keep their status a secret, perpetuating fears of stigmatization (30). Studies both of behaviorally infected youth and of adults have found that disclosure increases with length of time since diagnosis (26, 27), and learning one’s status at an older age has been associated with an increased sense of secrecy and fear of rejection (22). Finally, at the individual level, low self-efficacy and emotional distress predict nondisclosure in HIV+ adults (31). Conversely, in one study, guilt about possible transmission was the most commonly reported reason for eventual disclosure among PHIV+ adolescents (30).
An evidence-based understanding of the scope of nondisclosure and the barriers to and facilitators of disclosure can inform both the ways practitioners work with PHIV+ youth and interventions for this population. Yet, detailed quantitative explorations of these factors among PHIV+ youth are missing from the literature. Using data from a large cohort study of PHIV+ youth in New York City, Project CASAH, we examined a) detailed individual reports of disclosure to sexual partners, including disclosure in various sexual situations and in relation to overall sexual history; and b) potential correlates of disclosure among PHIV+ youth. We used Social Action Theory (SAT), a theoretical model of health behavior (32) to determine potential correlates of disclosure for analyses.
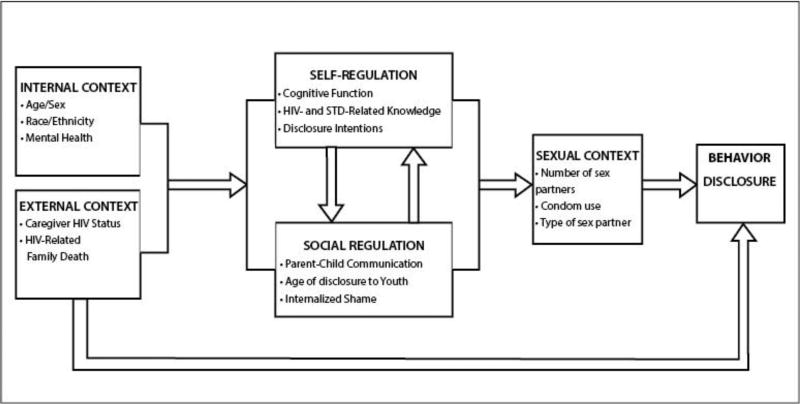
Theoretical models are helpful in understanding behavior. SAT posits that behavioral health outcomes are determined by three domains of influence. The Context in which behavior occurs can include internal contexts (e.g., age, gender, health and mental health status) and external contexts (e.g., culture, poverty, family illness/loss). Social-Regulation Processes, such as stigma and social support, inform decision-making, goal attainment, and attitudes and opinions and influence behaviors. Self-Regulation Processes include individual capabilities and motivations such as cognitive function, knowledge of health outcomes, intentions to engage in behaviors, and future aspirations.
Although SAT has been used in multiple studies of behavioral health in both PLWHIV (33–35) and HIV-affected youth (1), prior studies on disclosure have not typically used a theoretical framework. We modified SAT to guide the larger CASAH study (36), and we now show how it can inform our understanding of disclosure and development of intervention programs. SAT was used to identify a range of contextual, social-regulatory, and self-regulatory variables measured in Project CASAH that we predicted would positively influence serostatus disclosure to sexual partners. We hypothesized that the following variables would be associated with more disclosure to sexual partners:
Contextual factors: the internal context of (a) fewer mental health issues, and the external contextual factors of (b) having an HIV-negative caregiver and (c) lacking a family history of HIV-related death. Internal contexts of age, sex, race, and ethnicity were also examined.
Social regulatory factors: (a) more extensive parent-child communication about dating and sex, (b) earlier disclosure of youth’s serostatus to youth by parents/clinicians, and (c) stigma, both fewer stigma-related fears, and less stigma-based social rejection.
Self-regulatory factors: (a) stronger cognitive function, (b) greater HIV- and STD-related knowledge, and (c) stronger disclosure intentions,
METHODS
Participants
Data come from Project CASAH (37), a longitudinal study investigating the mental health and risk behaviors of PHIV+ and perinatally exposed but uninfected (PHIV-) youth as they age through adolescence and into young adulthood. Youth and their caregivers were originally recruited between 2003 and 2008 from four major medical centers providing primary and tertiary care to HIV-affected families in New York City, an epicenter of the US HIV epidemic, including the pediatric/adolescent epidemic (38), and were both interviewed at regular intervals at 5 distinct time points. Institutional Review Board approval was obtained from all sites and the lead investigator’s home institution. Initial enrollment inclusion criteria were youth age (9–16 years), perinatal exposure to HIV, cognitive capacity to complete an interview, residential status with a legal guardian who could provide consent (foster care parents cannot provide consent for psychosocial studies in NYC), and fluency in English or (for caregivers only) Spanish. The vast majority of youth in the participating clinics spoke English and came from English and/or Spanish-speaking households. Caregivers provided written informed consent for themselves and permission for youth <18 years of age. Youth <18 years old provided written assent, and youth ≥18 years old provided written informed consent.
Data Collection
Data sources included 1) caregiver and youth quantitative interviews and 2) medical charts. Caregivers and youth were interviewed separately but simultaneously by trained bachelor-level interviewers. Interviews ranged from approximately 1.5 hours to 3 hours, depending on the time point and individual-level factors (e.g the third follow-up interview omitted a large psychological screener and was thus half the length of other interviews).Youth interviews also contained a number of brief, self-administered surveys on sensitive topics, primarily concerning sexual behaviors. After the interview, HIV+ youths’ medical charts were abstracted through the participating clinics, with the summaries including information on CD4+ cell count, HIV RNA viral load, and antiretroviral regimens. Monetary compensation for time (forty dollars per individual, per interview) and transportation (reimbursement according to transportation method) was provided.
Measures
Behavioral Health Outcomes
Youth Disclosure of HIV status to sexual partners (Primary Outcome) was assessed via the self-administered CASAH Social Disclosure Interview. Participants answered questions about previous disclosure of HIV serostatus to sexual partners in each of four distinct situations: 1) to steady girlfriends/boyfriends, 2) to casual sexual partners (i.e., “someone besides your steady girl/ or boyfriend”), 3) when using condoms, and 4) when not using condoms. For each of these four sexual situations, youth were asked if they disclosed to none, some, most, or all of their past partners, scored as 0, 1, 2, and 3, respectively. They were also presented with the option to answer “I haven’t had sex.” Only participants who answered at least one disclosure question with a response other than “I haven’t had sex” were included in this analysis. We verified that all participants reported sexual activity by referencing separate responses on an audio computer-assisted self-interview (ACASI) sexual behavior survey. Disclosure in each of the four situations is presented separately for descriptive results (percentage of youth endorsing each category in each situation). For all subsequent statistical analyses (correlations, t-tests, and multiple regression), a composite score was calculated as the mean of the four individual disclosure items. The score had a theoretical range of 0–3, with a high score indicating higher levels of HIV disclosure. Cronbach’s alpha for this scale was .938.
Number of Sexual Partners was derived from questions from the Adolescent Sexual Behavior Assessment (39), self-administered via ACASI. Youth reported a specific value for lifetime number of sexual partners, including vaginal, anal, and oral sex. Number of lifetime vaginal sex partners was used in these analyses as very few participants reported only oral or anal sex; the vast majority who endorsed oral or anal sex also endorsed vaginal sex. While slightly over half of these youth had four or fewer partners, many had dozens (17 reported having 12 or more partners), and three reported over 100 partners (250, 300, & 800). A log-transformation was applied to reduce the variability and skewness of the data as has been done in previous studies of sexual behavior (40).
Self-Regulatory Factors
Cognitive Function was assessed using the interviewer-administered Peabody Picture Vocabulary Test (PPVT-IV), a well-validated test measuring receptive language skills and word recognition (41). The PPVT has also been validated as a proxy for overall cognitive function (41, 42). Based on participant age and the raw score, standard scores are calculated and were the focus for these analyses.
HIV and STD-Related Knowledge was assessed using two interviewer-administered scales. The HIV knowledge scale, from a healthcare provider guide for helping HIV+ youth transition to adulthood (43) comprised 23 items about HIV transmission and treatment knowledge, with “True,” “False,” or “Unsure” response choices for each item. Questions included “You can tell if a person has HIV by looking at him or her;” “If I stop taking one HIV medication, I should stop all of my HIV medication;” and “If my viral load is undetectable, I am cured of HIV.” STD knowledge was assessed using a similarly structured measure used for treating adolescents with HIV (44). It consisted of 19 items with the same response options as the HIV knowledge scale. Items were more generally focused on STDs and pregnancy, with three items specifically mentioning HIV (“Condoms prevent HIV;” “You can get an STD and HIV at the same time;” and “A douche after sex is a good method to prevent HIV”). Other questions included “Condoms help prevent STDs;” “If the male pulls out before he cums, he cannot make the girl pregnant;” and “You can get an STD from having oral sex.” Participants received a score of 1 for correct and 0 for incorrect responses. Thus, possible scores ranged from 0–23 (HIV treatment knowledge) and 0–19 (STD knowledge). Both measures were piloted with youth prior to use.
Intentions to Disclose were assessed with four questions as part of the self-administered CASAH Social Disclosure Interview. Participants were asked to select the response that “describes the people you might talk to about your HIV” across different sexual situations: with a casual partner, with a steady partner, when using condoms, and when not using condoms (example: “If you were going to have sex with someone with a condom would you tell him or her that you were HIV-positive?”). There were four answer options, scored 0–3, ranging from “Definitely Wouldn’t,” to “Definitely Would.” Scores were calculated as the mean of the four items, with a possible range of 0–3. Alpha for this scale was .895.
Social Regulatory Factors
Parent-Child Communication was assessed using an adapted version of Miller’s scale on sexuality and risk discussions (45). Interviewers presented youth with 12 potential topics, including “when to start dating” and “how to talk to a partner about using condoms.” Youth reported whether (yes/no) they had ever discussed these facets of sexuality with their caregivers. A score was calculated as the count of the number of topics discussed (possible range 0–12). Note 7/10 of the original scale items were retained and five additional items were developed to more accurately reflect the needs and experiences of the PHIV+ adolescents, including discussion of HIV with sexual partners.
Age of Disclosure to Youth was reported by caregivers and/or youth during the pre-interview screening process at every interview point prior to and including the investigated time point, depending on the youth’s age and living situation. During each interview, both caregivers and youth who had been disclosed to were asked how long it had been since the youth found out about his/her own status; caregiver answers were preferred when available. Age of disclosure was then calculated based on age at interview. This variable was dichotomized using two different ages, 10 and 13. A recent review of disclosure of HIV status to youth reported that medical providers recommended a median of age 10 for initiating HIV-centered discussions of health; it also concluded that various organizations recommend disclosing HIV to youth within the age range of 10–13 (46). As there is no clear consensus regarding the ideal age of disclosure, we chose to look at the extremes of this range.
Stigma was assessed using the Social Impact Scale, a well validated stigma measure in adults (47). On a 4-point Likert scale, participants reported to interviewers how much they agreed with statements regarding secrecy and fear related to their status (“I fear someone telling others about my HIV without my permission;” “I feel I need to keep my HIV a secret;” and “I do not feel I can be open with others about my HIV.”). For these analyses, we examined the two scales that have been validated with adults as young as 18, Internalized Shame and Social Rejection. Scores were calculated as the mean of the items for each scale, (possible range: 1–4). Although the entirety of the Internalized Shame scale was administered, we modified it in analysis given poor item-total correlations in 2/5 items. The three remaining items (listed above) reflect secrecy and fear related to HIV status; as such, we have renamed the subscale “Stigma-Related Fear.” Cronbach’s alpha was .617. We refer to the Social Rejection scale (which was used as is) as Stigma-Based Social Rejection for clarity; Cronbach’s alpha was .934.
Contextual Factors
Caregiver HIV Status was collected from current and past caregiver interviews. Enrolled caregivers reported on HIV testing and results.
HIV/AIDS-Related Family Death was reported by caregivers. Interviewers asked questions about all of the child’s family members by type of relation (e.g., birth mother, birth father, non-birth parent, other different types of relatives). If a caregiver indicated that a family member had died, s/he was asked if the death was HIV/AIDS related. A dichotomous variable was calculated indicating whether there was a history of an HIV/AIDS-related family death. At the time point used for analysis, many youth were over age 18 years, and caregivers did not come in for the interview. Thus, we are missing data on 48 youth.
Mental Health was measured using the interviewer-administered Youth Self Report (YSR, 11–18 years) and Adult Behavior Checklist (ABCL, ≥19 years) – Achenbach’s older-age counterparts to the Child Behavior Checklist (CBCL) – which are well validated and widely used symptom checklists of emotional and behavioral problems (48). On a 3-point scale, youth rate how “true” the items are in describing their behavior. Psychometric properties have been established for internalizing behavior (e.g., anxiety, withdrawal, depression) and externalizing behavior (e.g., aggression, delinquency) (48), using standardized scores based on age and gender; for this analysis, both the internalizing and externalizing subscales were used and analyzed independently.
Age and Gender were ascertained, with age calculated according to date of birth and date of interview.
Race and Ethnicity were reported to the interviewer by the youth, who selected from a list of racial and ethnic identities. The majority of youth were African American and/or Latino reflecting the majority makeup of the pediatric HIV epidemic in the NYC. For the purposes of analyses, race was coded as African American (yes or no), and ethnicity was coded as Hispanic/Latino (yes or no), given the small sample sizes for more specific ethnic categories (e.g., Puerto Rican, Dominican, Cuban, Mexican, etc.).
HIV RNA Viral Load (VL) was obtained from medical charts. Physicians and supporting staff were asked to report the three VL values collected closest to the interview date, and the value closest to and preceding the interview date was selected for analysis. Scores were dichotomized as either detectable or undetectable using <400 copies/mL as undetectable (the most consistent value during the time of the study across sites). VL data is presented to describe participants’ health, but not included in analyses because we could not match it to times of disclosure or to sexual events.
Analysis
Data for descriptive analyses included frequencies/percentages and means/standard deviations for each of the investigated SAT variables, as well as frequencies/percentages for behavioral health outcomes – i.e., number of sexual partners and all four disclosure items (when using a condom, when not using a condom, with steady partners, and with casual partners). Using the mean disclosure summary scores across the four disclosure items, Pearson correlations were calculated to assess relationships between disclosure and continuous variables; T-tests were used to determine the relationship between disclosure and dichotomous variables. Multiple regression analyses were conducted to determine which independent variables had the strongest association with disclosure in a multivariable model and to determine the amount of variance explained by the model. All variables with a significant bivariate association with disclosure (p < .05) were included in the model. Analyses of variables with missing data simply excluded the missing participants from the particular analyses; these participants were included in other analyses involving variables for which they had valid data.
RESULTS
Participant Characteristics
Data for this analysis come from the third Follow-Up interview (FU3; 2009–2014) with PHIV+ youth who were aware of their status (97% of PHIV+ youth at FU3), had engaged in sexual behavior, and had completed the questionnaire on disclosure of serostatus to sexual partners. FU3 was the chosen time point primarily because of the older age range of the participants at the interview − 14.5 to 25.7 years (M = 20.2, SD = 2.1), thus including more participants likely to be sexually active. Data collection for FU3 was the most recent FU completed, with data cleaned. Of the 206 PHIV+ youth enrolled in the study, 148 (72%) completed the FU3 interview an average of 5–6 years after enrollment. Among these, 98 (66%) were sexually active and provided responses to at least one of the disclosure questions. The 98 participants included in these analyses were significantly older at baseline than the 108 PHIV+ participants who either were not sexually active at the time of interview or did not complete the interview (13.4 vs. 12.0; t = −4.86, df = 204, p < .001), but they were comparable in terms of gender, race, and ethnicity. Data were available from 52 caregivers of the included youth.
The 98 youth included in these analyses were evenly split between males and females; 63% identified as African American, and 48% identified as Latino. At study enrollment, the participants who contributed to these analyses had caregivers that were predominantly female (85%) with a mean age of 50.3 (SD = 12.0) and some college education (56%). Their race/ethnicity was similar to that of the youth (36% Hispanic/Latino; 55% Black/African American). Approximately a third (37%) of the caregivers were the youth's biological parent, and 31% were HIV+. Group characteristics (means and frequencies) for each of the investigated domains are presented in Table I.
Table I.
Demographic and Study Characteristics of PHIV+ Adolescents and Young Adults in New York City, 2009–2014, According to Social Action Theory Domains (N=98)
| Social Action Theory Domains/Behavior (Minima-Maxima/Total N) | ||||
|---|---|---|---|---|
| N | % | M | SD | |
| Contextual | ||||
| Female | 49 | 50% | ||
| African American | 62 | 63% | ||
| Latino | 47 | 48% | ||
| Age at Interview | 20.21 | 2.06 | ||
| HIV+ Caregiver (Total N=94) | 29 | 31% | ||
| ndetectable Viral Load (Total N = 84) | 41 | 49% | ||
| History of HIV-Related Family Death (Total N = 52) | 20 | 39% | ||
| Youth Mental Health- Internalizing Behavioral Issues (23–100) | 49.69 | 10.30 | ||
| Youth Mental Health-Externalizing Behavioral Issues (23–100) | 52.44 | 8.39 | ||
| Self-Regulatory | ||||
| HIV Treatment Knowledge (0–23) | 19.33 | 2.69 | ||
| STD-Related Knowledge (0–19) | 13.54 | 3.41 | ||
| Cognitive Function (20–160) | 83.32 | 11.48 | ||
| Disclosure Intentions (0–3) | 1.66 | 0.92 | ||
| Social Regulatory | ||||
| Stigma-Related Fear (1–4) | 2.67 | 0.78 | ||
| Stigma-Based Social Rejection (1–4) | 3.44 | 1.58 | ||
| Parent-Child Communication (0–12) | 7.04 | 3.93 | ||
| Disclosed to before age 13 | 68 | 69% | ||
| Disclosed to before age 10 | 42 | 43% | ||
| Behavior | Median | Range | ||
| Number of Lifetime Vaginal Sex Partners | 4 | 0–800 | ||
Overall, youth demonstrated below-average cognitive function (PPVT M = 83.32, SD = 11.48), but reported internalizing and externalizing behavioral problems in the normative range (T-scores < 65 or 70) (M = 49.69, SD = 10.30 and M = 52.44, SD = 8.39, respectively). Although all participants included in these analyses were sexually active, their sexual experience varied widely (reported lifetime vaginal sex partners range: 0–800, median: 4). Only 3 boys and 8 girls in this subset reported any kind of sex with same-sex partners. Among all youth reporting anal or oral sex, all but 4 reported vaginal sex. Although they were all aware of their status, participants had been told at ages ranging from 3.4 to 16 years (M = 10.7, SD = 2.9). VL data were available at FU3 for 73 out of 98 youth (74%). Data were missing because the youth were not engaged in care in the past year, had begun seeing a physician at a different clinic, or had charts that were unavailable. Of participants with VL data, 51% had a detectable viral load around the time of the interview (M = 3.40 months before day of interview, SD = 6.06 months).
Patterns of Disclosure to Partners (Table II)
Table II.
Reported Disclosure of HIV Status to Sexual Partners by PHIV+ Adolescents and Young Adults in New York City across Four Scenarios, 2009–2014 (N=98*)
| Partners Disclosed to |
When having sex with condoms (N=98) |
When having sex without condoms (N = 84) |
When having sex with steady partners (N = 96) |
When having sex with casual partners (N = 92) |
|---|---|---|---|---|
|
| ||||
| % | % | % | % | |
| None | 55 | 45 | 37 | 59 |
| Some | 16 | 14 | 25 | 13 |
| Most | 4 | 8 | 5 | 9 |
| All | 25 | 32 | 33 | 20 |
Ns for each scenario do not equal 98 due to “not applicable” responses
Disclosure to past sexual partners varied significantly by partner type and by whether or not a condom was used. A higher proportion of respondents (59%) reported disclosing to none of their casual sex partners than to none of their steady partners (37%; McNemar test p= < .001) and to none of their partners when a condom was used (55%) than when sex was condomless (45%, p=.007). Similarly, more participants reported disclosing to all or most of their partners when having sex without a condom (40%) than when having sex with a condom (29%, p=.001) and when having sex with steady partners (38%) than when having sex with casual partners (29%, p=.021). Although we did not ask about disclosure with or without a condom for each partner type, condom use was less common with a boy/girlfriend than with other partners at last reported vaginal sex occasion (82% vs. 94%); however, the difference was not statistically different (p = .115).
Associations of Social Action Theory Domains with Disclosure
Other Behavioral Health Outcomes
Number of lifetime vaginal sexual partners was not associated with disclosure in bivariate analyses (Table III).
Table III.
Correlations between Reported Disclosure of HIV Status to Sexual Partners and Self-Regulatory, Social Regulatory, and Contextual Factors (N= 98)
| Behavior/Social Action Theory Domains |
Disclosure | |
|---|---|---|
| r | p | |
| Behavior | ||
| Number of Sex Partners | −.17 | .103 |
| Self-Regulatory | ||
| HIV Treatment Knowledge | .16 | .113 |
| STD-Related Knowledge | .21 | .041 |
| Disclosure Intentions | .75 | <.001 |
| Cognitive Function | .02 | .886 |
| Social Regulatory | ||
| Stigma-Related Fear | −.13 | .191 |
| Stigma-Social Rejection | .04 | .718 |
| Parent-Child Sex-Related Communication | .23 | .022 |
| Contextual | ||
| Age at interview | .24 | .020 |
| Internalizing Behavioral Issues | .12 | .226 |
| Externalizing Behavioral Issues | .14 | .173 |
Self-Regulatory Factors (Table III)
Two self-regulatory factors were significantly and positively correlated with disclosure to more partners. Intentions to disclose to future partners was the factor most strongly correlated with previous disclosure practices (r = .75, p<.001). Youth who had higher scores in STD-related knowledge were also more likely to have disclosed, (r = .21, p =.041). Neither HIV-related knowledge nor youth cognitive function was significantly correlated with disclosure.
Social Regulatory Factors
Several of the social regulatory factors appear to be related to disclosure. More extensive parent-child communication about sex and dating (Table III) positively correlated with youth disclosure to more partners. In terms of age of learning one’s serostatus (Table IV), a significant mean difference was found using the age cutoff of 13 years, t(96) = 2.64, p =.01, with those told when younger than age 13 reporting disclosure to more partners. Those who were told their status before age 10 did not have significantly different disclosure rates to partners from those who were told at 10 years or older. Neither stigma-related fear nor stigma-based social rejection was associated with disclosure to partners (Table III).
Table IV.
T-Tests Comparing Reported Disclosure with Social Regulatory and Contextual Factors
| Domains | Disclosure | ||||||
|---|---|---|---|---|---|---|---|
|
| |||||||
| N | M | SD | t | df | p | ||
|
| |||||||
| Social Regulatory | |||||||
| Age of Disclosure (10 cutoff) | <10 | 42 | 1.33 | 1.14 | 1.44 | 96 | .154 |
| ≥10 | 56 | 0.99 | 1.19 | ||||
| Age of Disclosure (13 cutoff) | <13 | 68 | 1.34 | 1.17 | 2.64 | 96 | .010 |
| ≥13 | 30 | 0.68 | 1.09 | ||||
| Contextual | |||||||
| Sex | Male | 49 | 0.88 | 1.05 | −2.24 | 93 | .028 |
| Female | 49 | 1.40 | 1.25 | ||||
| Race (African American, yes/no) | Yes | 62 | 1.03 | 1.14 | 1.23 | 96 | .221 |
| No | 36 | 1.33 | 1.23 | ||||
| Ethnicity (Latino, yes/no) | Yes | 47 | 1.38 | 1.56 | −1.96 | 96 | .053 |
| No | 51 | 0.92 | 1.17 | ||||
| Caregiver HIV Status | Positive | 29 | 1.12 | 1.19 | 2.33 | 92 | .816 |
| Negative | 65 | 1.19 | 1.20 | ||||
| HIV- related Family Death | Yes | 20 | 1.67 | 1.31 | −1.84 | 50 | .071 |
| No | 32 | 1.04 | 1.14 | ||||
Contextual Factors
Age and sex were each associated with disclosure practices. Older participants were more likely to disclose to more sexual partners, r = .24, p = .02 (Table III), and females disclosed to more of their partners than did males, t(93) = −2.24, p = .03 (Table IV). While race was not significantly associated with disclosure (Table IV), Latino ethnicity approached significance, with Latino youth reporting disclosure to more sexual partners than non-Latino youth, t(96) = −1.96, p = .053. Internalizing and externalizing behavioral problems, caregiver HIV status, and a family history of AIDS-related death were not associated with disclosure rates (Table IV).
Multivariable Associations with Disclosure
Table V shows the results of a multiple regression analysis including all independent variables with a significant bivariate association with disclosure. Two variables were significant in this model: disclosure intentions (b = .86, SE = .09, p < .001) and learning one’s status before age 13 (b = −.37, SE = .18, p = .044). The total R2 for the model was .609, indicating that 60.9% of the variance of disclosure was explained by the above model.
Table V.
Linear Regression Comparing Disclosure with Social Action Theory Domains
| Social Action Theory Domains |
b | SE | p |
|---|---|---|---|
| Self-Regulatory | |||
| STD-Related Knowledge | .02 | .02 | .472 |
| Disclosure Intentions | .86 | .09 | < .001 |
| Social Regulatory | |||
| Parent-Child Communication | .02 | .02 | .480 |
| Disclosure Before or After Age 13 | −.37 | .18 | .044 |
| Contextual | |||
| Age | .07 | .04 | .062 |
| Sex | .15 | .17 | .363 |
DISCUSSION
Disclosure Patterns
In one of the first quantitative analyses of patterns and correlates of HIV serostatus disclosure by PHIV+ adolescents and young adults to their sexual partners, we uncovered a number of important findings, many of which have also been described among behaviorally infected youth and adults (25–28, 49). Similar to same-age peers (3), PHIV+ youth are having sex with and without condoms and both within and outside of committed relationships. As predicted, we found that many of these sexually active adolescents and young adults are not disclosing their status to any of their partners, especially when those partners are casual – i.e. not a steady girl/boyfriend. Although disclosure is more common when condoms are not being used, it is noteworthy that only 40% of participants reported disclosing to all or most of their partners and almost half (45%) report disclosing to no partners when having unprotected sex. As more than half of the youth in our sample had detectable viremia around the time of the interview, these findings point to the need for interventions to help youth navigate decisions about disclosure, promote open discussions of sexual health, and, thus, prevent further HIV transmission. To our knowledge there are few if any evidence based disclosure interventions that have been published for this population (50).
Some explanations for our findings on disclosure patterns emerge from previous qualitative work among PHIV+ youths (22, 30) as well as behaviorally infected adolescents and adults (25, 26, 49). With a steady partner, established dynamics of closeness and trust may reduce fears of rejection (22) and, thus, lead to disclosure. Discussing sensitive issues with a close partner may be facilitated by expectations of empathy, commitment, and more in-depth communication, leading to opportunities for questions and support. The observed higher rates of disclosure during sex without condoms may stem from a sense of responsibility related to the heightened risk of transmission. Indeed, in a qualitative study, youth cited their “conscience” as leading them to disclose more in the situation of condomless sex (30). Our findings support the premise that youth are considering the consequences of risky behavior, even if they are not always able to engage in sex with a condom. Guilt may also contribute to disclosure to steady partners, as the infected youth might feel a stronger bond and sense of responsibility in a committed relationship. However, the higher disclosure rates in these two situations (unprotected sex and steady partnership) may also be explained in part by the possibility that monogamous partners refrain from condom use more frequently, resulting in overlap between these two categories. More in-depth investigation of this intersection could be beneficial.
Sexual situations in which participants disclosed to fewer partners – sex with a condom and sex with a casual partner – might be explained by these same dynamics. For sex with a condom, there is less risk of transmission and responsibility or guilt may not be as pressing a factor, leading to non-disclosure. Also, fear of rejection and lack of trust might be much stronger with a casual partner whom the youth does not know well. In fact, in qualitative interviews, PHIV+ youth have categorized disclosure to casual partners as more emotionally/socially risky (22). In our analyses, however, social rejection and stigma-related fear were not significantly correlated with disclosure. Moreover, our participants did not report high rates of social rejection, which might account for the lack of association. However, Project CASAH participants routinely expressed difficulty with the social rejection questions, explaining that they had not disclosed their status to any of the people cited in the questions (teachers, friends, etc.) and, therefore, had not experienced the social rejection. Yet, that did not mean they were not afraid of being rejected. In varying degrees, there were still youth in this study who reported fear of others knowing their status. Further exploration of how to best measure perceptions and experiences of stigma in this population and others who have kept their HIV a secret is warranted.
Although scenarios in which disclosure is lowest pose the greatest prevention challenges, it is important to help young people make decisions about disclosure in a range of sexual situations in order to promote sexual health and prevent further HIV transmission. Providing youth with fundamental knowledge of disclosure and its potential benefits and possible negative consequences in a range of sexual situations may be critical in helping them think through decisions prior to the moment of sex. Youth’s relationships may not be well planned and may change frequently, as might their use of condoms within a particular relationship (for example, condoms are initially used and then abandoned). In one qualitative study of Canadian PHIV+ adolescents, participants described transitioning into condomless sex unexpectedly, in “the heat of the moment,” and worrying about the resulting risk of transmission (29). Waiting to disclose until this moment or turning point in a relationship could potentially have damaging emotional consequences for the infected individual as well as his or her partner.
SAT and Disclosure
To our knowledge, this is the first theoretically informed study to investigate systematically the theoretically-informed factors (self-regulatory, social regulatory, and contextual) associated with disclosure/nondisclosure in older PHIV+ youth. Multiple regression analyses revealed a strong model fit, suggesting that SAT is an effective mode through which to study and explain disclosure. As all three SAT domains yielded significance in bivariate analyses, and two domains contributed to significance in the multiple regression analysis, a holistic approach to future work concerning disclosure is warranted.
We found a number of significant relationships across the SAT domains that have bearing on clinical approaches to working with this population. First, the self-regulatory factors of strong intentions to disclose and better STD and pregnancy-related knowledge were significantly correlated with increased disclosure to partners. Disclosure intention was the most strongly correlated of these variables, revealing a consistency of planned action (e.g., those who had already disclosed strongly intended to do so with future partners) and a strong relationship between intentionality and behavior. Although our data do not speak to causation, those who better understood the health consequences of risky sexual behavior (most importantly, modes of transmission) were also more likely to disclose their HIV status to their partners. The success of numerous sexual health-based HIV educational interventions around the world in lowering sexual risk behaviors (51) suggests that understanding the consequences of various actions, as well as protective options to reduce poor health outcomes, can facilitate safer sexual choices in the perinatally-infected population, which could include disclosing to sexual partners. For PHIV+ youth, a focus on general sexual health education might be just as important as HIV education.
Our finding that those with fewer partners disclosed to a higher proportion of those partners is supported by the literature on disclosure in other HIV+ populations (20, 27). This result makes particular sense when considering this population’s unique entry into sexual activity (i.e., having sex for the first time as an already-infected individual); for those who intend to disclose, the very prospect of disclosing to all future partners might have a limiting effect on the number of sexual relationships, with fewer partners potentially reflecting sexual selectivity. Additionally, as one adds partners to his/her sexual history, one also adds opportunities to refrain from disclosing, especially if a higher number of sexual partners means more casual partners. Longitudinal research is needed to examine the causal priority of these variables and how addressing these relationships could be incorporated into interventions.
Helping to shape and reinforce these self-regulatory factors are the significant social regulatory factors of parent-child communication regarding sex/dating and serostatus disclosure to the youth. Parental communication is associated with reduced youth sexual risk behavior as well as increased condom use and discussions of safer sex with partners (52–54). Parent-youth communication about these topics may introduce the youth to the idea of having intimate, sensitive, or even uncomfortable conversations about sex and HIV status. Therefore, PHIV+ youth who communicate with their parents about sex and dating may be at an advantage in terms of future disclosure to sexual partners. Our findings also suggest that open discussions about a child’s HIV should occur sooner rather than later, as those youth who were told of their own status earlier disclosed it to more sexual partners, perhaps reflecting greater comfort in talking about their own HIV. In a prior analysis from CASAH when the youth were younger, PHIV+ youth who knew their status for longer reported stronger disclosure intentions (55), and our current results suggest that reports of intentions and behavior are strongly correlated. This holds great clinical significance for PHIV+ youth under 13 years of age, particularly in countries where there are still high rates of perinatal infection and, therefore, younger perinatally infected populations (56). Furthermore, those who were told their HIV status at an older age may benefit from targeted help in combating the emotional effects of having had their diagnosis kept from them for so long.
Two internal contextual factors were significantly associated with disclosure. Males and younger youth appeared to be at higher risk for less disclosure. A meta-analysis of over 200 studies on self-disclosure found that, overall, women are more likely than men to self-disclose to others (57). This is particularly interesting in the context of HIV, given women’s perceived risk of violence and aggression in response to disclosure. The aforementioned meta-analysis speculated that men may conform to gender-based sexual identities that emphasize strength and de-emphasize vulnerability (57). We attribute the age-related finding to maturity level and perhaps increased comfort surrounding sexual relationships in general, though this warrants further investigation. Overall, our findings suggest that discussions about disclosure that begin in or prior to early adolescence may be critical, and boys may need special focus.
Limitations
This study has a number of limitations. First, our analysis was cross-sectional, limiting statements about causal priority of study variables. Second, disclosure is a dynamic process that changes over time and context, and research is needed on how disclosure to partners changes over time, in particular as it relates to the SAT factors we found to be important. Third, we were not able to examine disclosure by partner type and condom use simultaneously, and a more nuanced and relevant understanding of disclosure to a given partner type in the context of protected or unprotected sex will be important for interventions. Same-sex partnerships were also excluded from our analyses given how few were reported at this age period and will deserve further attention in the future. Although our sample was larger than those of many other PHIV+ disclosure studies, a larger sample size could also add more weight to our findings. In addition, our age range was quite large (14–26), and a larger sample would allow us to further investigate how age might be related to disclosure to partners. The age range at Project CASAH’s baseline interview was large in order to obtain a sufficient sample size at baseline. The ideal sample used for analysis arguably would have been slightly older; as previously explained, due to data collection timing and sample size, FU3 data was the most appropriate choice. Finally, our sample was clinic based as well as exclusively from New York City and, therefore, might not reflect all PHIV+ adolescents and young adults in the US. In turn, PHIV+ youth in the US may differ in important ways from PHIV+ youth in other countries and from behaviorally infected youth. Thus, studies examining these variables in other populations of infected young people are warranted.
Conclusion
Nonetheless, our data indicate that disclosure of HIV status to sexual partners may be difficult for young people who have grown up with HIV. Developing effective strategies to help young people make decisions about how, when, and to whom to disclose their HIV status is important for prevention of further HIV transmission as well as for sexual health more generally. For example, creating interventions that a) provide youth with information about sexual relationships, communication, HIV and STI transmission, and pregnancy as well as b) help them think about and plan how to navigate disclosure decisions in advance (e.g. by supporting intentions to disclose to partners, while evaluating issues around safety and emotional wellbeing) may be important areas for future research with PHIV+ youth and young adults. With a more nuanced understanding of disclosure to sexual partners, we can help PHIV+ youth engage in healthy, communicative sexual relationships, giving all parties involved the tools to make safe and thoughtful choices regarding their own health and the health of others.
Figure 1.
Social Action Theory Model and selected variables
References
- 1.Elkington KS, Bauermeister JA, Robbins RN, Gromadzka O, Abrams EJ, Wiznia A, et al. Individual and contextual factors of sexual risk behavior in youth perinatally infected with HIV. AIDS Patient Care STDS. 2012;26(7):411–22. doi: 10.1089/apc.2012.0005. Epub 2012/06/15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Elkington KS, Bauermeister JA, Brackis-Cott E, Dolezal C, Mellins CA. Substance use and sexual risk behaviors in perinatally human immunodeficiency virus-exposed youth: Roles of caregivers, peers and HIV status. The Journal of adolescent health : official publication of the Society for Adolescent Medicine. 2009;45(2):133–41. doi: 10.1016/j.jadohealth.2009.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Elkington KS, Bauermeister JA, Santamaria EK, Dolezal C, Mellins CA. Substance use and the development of sexual risk behaviors in youth perinatally exposed to HIV. J Pediatr Psychol. 2014 doi: 10.1093/jpepsy/jsu103. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ezeanolue EE, Wodi AP, Patel R, Dieudonne A, Oleske JM. Sexual behaviors and procreational intentions of adolescents and young adults with perinatally acquired human immunodeficiency virus infection: Experience of an urban tertiary center. The Journal of adolescent health : official publication of the Society for Adolescent Medicine. 2006;38(6):719–25. doi: 10.1016/j.jadohealth.2005.06.015. [DOI] [PubMed] [Google Scholar]
- 5.Tassiopoulos K, Moscicki AB, Mellins C, Kacanek D, Malee K, Allison S, et al. Sexual risk behavior among youth with perinatal HIV infection in the United States: Predictors and implications for intervention development. Clin Infect Dis. 2013;56(2):283–90. doi: 10.1093/cid/cis816. Epub 2012/11/10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mellins CA, Brackis-Cott E, Dolezal C, Abrams EJ. The role of psychosocial and family factors in adherence to antiretroviral treatment in human immunodeficiency virus-infected children. Pediatr Infect Dis J. 2004;23(11):1035–41. doi: 10.1097/01.inf.0000143646.15240.ac. Epub 2004/11/17. [DOI] [PubMed] [Google Scholar]
- 7.Usitalo A, Leister E, Tassiopoulos K, Allison S, Malee K, Paul ME, et al. Relationship between viral load and self-report measures of medication adherence among youth with perinatal HIV infection. AIDS Care. 2014;26(1):107–15. doi: 10.1080/09540121.2013.802280. Epub 2013/06/27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Van Dyke RB, Lee S, Johnson GM, Wiznia A, Mohan K, Stanley K, et al. Reported adherence as a determinant of response to highly active antiretroviral therapy in children who have human immunodeficiency virus infection. Pediatrics. 2002;109(4):e61. doi: 10.1542/peds.109.4.e61. Epub 2002/04/03. [DOI] [PubMed] [Google Scholar]
- 9.Wiener L, Riekert K, Ryder C, Wood LV. Assessing medication adherence in adolescents with HIV when electronic monitoring is not feasible. AIDS Patient Care STDS. 2004;18(9):527–38. doi: 10.1089/apc.2004.18.527. Epub 2005/01/06. [DOI] [PubMed] [Google Scholar]
- 10.Williams PL, Storm D, Montepiedra G, Nichols S, Kammerer B, Sirois PA, et al. Predictors of adherence to antiretroviral medications in children and adolescents with HIV infection. Pediatrics. 2006;118(6):e1745–57. doi: 10.1542/peds.2006-0493. Epub 2006/11/15. [DOI] [PubMed] [Google Scholar]
- 11.Marks G, Burris S, Peterman TA. Reducing sexual transmission of HIV from those who know they are infected: the need for personal and collective responsibility. AIDS. 1999;13(3):297–306. doi: 10.1097/00002030-199902250-00001. Epub 1999/04/13. [DOI] [PubMed] [Google Scholar]
- 12.Fisher JD, Fisher WA. Changing AIDS-risk behavior. Psychological bulletin. 1992;111(3):455–74. doi: 10.1037/0033-2909.111.3.455. Epub 1992/05/01. [DOI] [PubMed] [Google Scholar]
- 13.Lyles CM, Kay LS, Crepaz N, Herbst JH, Passin WF, Kim AS, et al. Best-evidence interventions: Findings from a systematic review of HIV behavioral interventions for US populations at high risk, 2000–2004. Am J Public Health. 2007;97(1):133–43. doi: 10.2105/AJPH.2005.076182. Epub 2006/12/02. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Marks G, Crepaz N, Senterfitt JW, Janssen RS. Meta-analysis of high-risk sexual behavior in persons aware and unaware they are infected with HIV in the United States: Implications for HIV prevention programs. J Acquir Immune Defic Syndr. 2005;39(4):446–53. doi: 10.1097/01.qai.0000151079.33935.79. [DOI] [PubMed] [Google Scholar]
- 15.Crepaz N, Marks G. Serostatus disclosure, sexual communication and safer sex in HIV-positive men. AIDS Care. 2003;15(3):379–87. doi: 10.1080/0954012031000105432. [DOI] [PubMed] [Google Scholar]
- 16.De Rosa CJ, Marks G. Preventive counseling of HIV-positive men and self-disclosure of serostatus to sex partners: New opportunities for prevention. Health psychology : official journal of the Division of Health Psychology, American Psychological Association. 1998;17(3):224–31. doi: 10.1037//0278-6133.17.3.224. [DOI] [PubMed] [Google Scholar]
- 17.Gielen AC, Fogarty L, O'Campo P, Anderson J, Keller J, Faden R. Women living with HIV: Disclosure, violence, and social support. J Urban Health. 2000;77(3):480–91. doi: 10.1007/BF02386755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Gielen AC, O'Campo P, Faden RR, Eke A. Women's disclosure of HIV status: Experiences of mistreatment and violence in an urban setting. Women & health. 1997;25(3):19–31. doi: 10.1300/J013v25n03_02. Epub 1997/01/01. [DOI] [PubMed] [Google Scholar]
- 19.Obermeyer CM, Baijal P, Pegurri E. Facilitating HIV disclosure across diverse settings: A review. Am J Public Health. 2011;101(6):1011–23. doi: 10.2105/AJPH.2010.300102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Dempsey AG, MacDonell KE, Naar-King S, Lau CY. Adolescent Medicine Trials Network for HIVAI. Patterns of disclosure among youth who are HIV-positive: a multisite study. The Journal of adolescent health : official publication of the Society for Adolescent Medicine. 2012;50(3):315–7. doi: 10.1016/j.jadohealth.2011.06.003. Epub 2012/02/14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Havens JF, Mellins CA. Psychiatric aspects of HIV/AIDS in childhood and adolescence. In: Rutter M, Taylor E, editors. Child and Adolescent Psychiatry/Fifth Edition. Oxford, UK: Blackwell; 2008. [Google Scholar]
- 22.Fair C, Albright J. "Don't tell him you have HIV unless he's 'the one'": Romantic relationships among adolescents and young adults with perinatal HIV infection. AIDS Patient Care STDS. 2012;26(12):746–54. doi: 10.1089/apc.2012.0290. Epub 2012/12/04. [DOI] [PubMed] [Google Scholar]
- 23.Koenig LJ, Pals SL, Chandwani S, Hodge K, Abramowitz S, Barnes W, et al. Sexual transmission risk behavior of adolescents With HIV acquired perinatally or through risky behaviors. J Acquir Immune Defic Syndr. 2010;55(3):380–90. doi: 10.1097/QAI.0b013e3181f0ccb6. Epub 2010/08/31. [DOI] [PubMed] [Google Scholar]
- 24.Peele YL, D'Angelo LJ, Chandwani S, Abramowitz S, Koenig LJ. 164. Determinants Of HIV Serostatus Self-Disclosure Among Adolescents Participating in the Adolescent Impact Study. Abstract. The Journal of adolescent health : official publication of the Society for Adolescent Medicine. 2012;50(2):S91–S2. [Google Scholar]
- 25.D'Angelo LJ, Abdalian SE, Sarr M, Hoffman N, Belzer M, Network. AMHIVAR Disclosure of serostatus by HIV infected youth: The experience of the REACH study. Reaching for Excellence in Adolescent Care and Health. The Journal of adolescent health : official publication of the Society for Adolescent Medicine. 2001;29(Supplement 3):72–9. doi: 10.1016/s1054-139x(01)00285-3. Epub 2001/09/01. [DOI] [PubMed] [Google Scholar]
- 26.Batterham P, Rice E, Rotheram-Borus MJ. Predictors of serostatus disclosure to partners among young people living with HIV in the pre- and post-HAART eras. AIDS and behavior. 2005;9(3):281–7. doi: 10.1007/s10461-005-9002-5. Epub 2005/08/10. [DOI] [PubMed] [Google Scholar]
- 27.Simon Rosser BR, Horvath KJ, Hatfield LA, Peterson JL, Jacoby S, Stately A. Predictors of HIV disclosure to secondary partners and sexual risk behavior among a high-risk sample of HIV-positive MSM: Results from six epicenters in the US. AIDS Care. 2008;20(8):925–30. doi: 10.1080/09540120701767265. Epub 2008/09/09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Nachega JB, Morroni C, Zuniga JM, Sherer R, Beyrer C, Solomon S, et al. HIV-related stigma, isolation, discrimination, and serostatus disclosure: A global survey of 2035 HIV-infected adults. J Int Assoc Physicians AIDS Care. 2012;11(3):172–8. doi: 10.1177/1545109712436723. Epub 2012/03/21. [DOI] [PubMed] [Google Scholar]
- 29.Fernet M, Wong K, Richard ME, Otis J, Levy JJ, Lapointe N, et al. Romantic relationships and sexual activities of the first generation of youth living with HIV since birth. AIDS Care. 2011;23(4):393–400. doi: 10.1080/09540121.2010.516332. Epub 2011/01/29. [DOI] [PubMed] [Google Scholar]
- 30.Michaud PA, Suris JC, Thomas LR, Kahlert C, Rudin C, Cheseaux JJ. To say or not to say: A qualitative study on the disclosure of their condition by human immunodeficiency virus-positive adolescents. The Journal of adolescent health : official publication of the Society for Adolescent Medicine. 2009;44(4):356–62. doi: 10.1016/j.jadohealth.2008.08.004. Epub 2009/03/25. [DOI] [PubMed] [Google Scholar]
- 31.Kalichman SC, Nachimson D. Self-efficacy and disclosure of HIV-positive serostatus to sex partners. Health psychology : official journal of the Division of Health Psychology, American Psychological Association. 1999;18(3):281–7. doi: 10.1037//0278-6133.18.3.281. Epub 1999/06/05. [DOI] [PubMed] [Google Scholar]
- 32.Ewart CK. Social action theory for a public health psychology. Am Psychol. 1991;46(9):931–46. doi: 10.1037//0003-066x.46.9.931. Epub 1991/09/01. [DOI] [PubMed] [Google Scholar]
- 33.Webel A, Phillips JC, Rose C, Holzemer WL, Chen W-T, Tyer-Viola L, et al. A cross-sectional description of social capital in an international sample of persons living with HIV/AIDS (PLWH) BMC Public Health. 2012;12(1):1–11. doi: 10.1186/1471-2458-12-188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Remien RH, Mellins CA, Robbins RN, Kelsey R, Rowe J, Warne P, et al. Masivukeni: Development of a multimedia based antiretroviral therapy adherence intervention for counselors and patients in South Africa. AIDS & Behavior. 2013;17(6):1979–91. doi: 10.1007/s10461-013-0438-8. Epub 2013/03/08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Traube DE, Holloway IW, Smith L. Theory development for HIV behavioral health: Empirical validation of behavior health models specific to HIV risk. AIDS Care. 2011;23(6):663–70. doi: 10.1080/09540121.2010.532532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Mellins CA, Dolezal C, Brackis-Cott E, Nicholson O, Warne P, Meyer-Bahlburg HFL. Predicting the onset of sexual and drug risk behaviors in HIV-negative youths with HIV-positive mothers: The role of contextual, self-regulation, and social-interaction factors. J Youth Adolescence. 2007;36(3):265–78. doi: 10.1007/s10964-006-9129-3. [DOI] [PubMed] [Google Scholar]
- 37.Mellins CA, Brackis-Cott E, Leu CS, Elkington KS, Dolezal C, Wiznia A, et al. Rates and types of psychiatric disorders in perinatally human immunodeficiency virus-infected youth and seroreverters. J Child Psychol Psychiatry. 2009;50(9):1131–8. doi: 10.1111/j.1469-7610.2009.02069.x. Epub 2009/03/21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Centers for Disease Control and Prevention. HIV Surveillance Report, Volume 25: Diagnoses of HIV Inflection in the United States and Dependent Areas, 2013. Atlanta, Georgia: CDC; Feb, 2015. [Google Scholar]
- 39.Dolezal C, Marhefka SL, Santamaria EK, Leu CS, Brackis-Cott E, Mellins CA. A comparison of audio computer-assisted self-interviews to face-to-face interviews of sexual behavior among perinatally HIV-exposed youth. Arch Sex Behav. 2012;41(2):401–10. doi: 10.1007/s10508-011-9769-6. Epub 2011/05/24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Tukey JW. Exploratory data analysis. Reading, MA: Addison-Wesley; 1977. [Google Scholar]
- 41.Dunn LM, Dunn DM. Peabody Picture Vocabulary Test, Fourth Edition. Minneapolis, MN: Pearson Education; 2007. [Google Scholar]
- 42.Campbell JM, Brown RT, Cavanagh SE, Vess SF, Segall MJ. Evidence-based assessment of cognitive functioning in pediatric psychology. J Pediatr Psychol. 2008;33(9):999–1014. doi: 10.1093/jpepsy/jsm138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Jacob S, Jearld S. Transitioning your HIV+ youth to healthy adulthood: A guide for health care providers. New York, NY: Children's Hope Foundation and the Partnership for Family Health; 2007. [Google Scholar]
- 44.hivcareforyouth.org. Treating adolescents with HIV: Tools for building skills in cultural competence, clinical care, and support. 2007 Available from: www.hivcareforyouth.org.
- 45.Miller KS, Kotchick BA, Dorsey S, Forehand R, Ham AY. Family communication about sex: What are parents saying and are their adolescents listening? Fam Plann Perspect. 1998;30(5):218–22. 35. Epub 1998/10/22. [PubMed] [Google Scholar]
- 46.Sahay S. Coming of age with HIV: A need for disclosure of HIV diagnosis among children/adolescents. J HIV AIDS Infect Dis. 2013;1:1–7. [Google Scholar]
- 47.Fife BL, Wright ER. The dimensionality of stigma: A comparison of its impact on the self of persons with HIV/AIDS and cancer. J Health Soc Behav. 2000;41(1):50–67. Epub 2000/04/06. [PubMed] [Google Scholar]
- 48.Achenbach TM. Integrative guide for the 1991 CBCL/4–18, YSR, and TRF profiles. Burlington, VT: University of Vermont, Department of Psychiatry; 1991. [Google Scholar]
- 49.Ciccarone DH, Kanouse DE, Collins RL, Miu A, Chen JL, Morton SC, et al. Sex without disclosure of positive HIV serostatus in a US probability sample of persons receiving medical care for HIV infection. Am J Public Health. 2003;93(6):949–54. doi: 10.2105/ajph.93.6.949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Evangeli M, Foster C. Who, then what? The need for interventions to help young people with perinatally acquired HIV disclose their HIV status to others. AIDS. 2014;28(Suppl 3):S343–6. doi: 10.1097/QAD.0000000000000334. Epub 2014/07/06. [DOI] [PubMed] [Google Scholar]
- 51.Kirby DB, Laris BA, Rolleri LA. Sex and HIV education programs: Their impact on sexual behaviors of young people throughout the world. J Adoles Health. 2007;40(3):206–17. doi: 10.1016/j.jadohealth.2006.11.143. [DOI] [PubMed] [Google Scholar]
- 52.Whitaker DJ, Miller KS. Parent-adolescent discussions about sex and condoms: Impact on peer influences of sexual risk behavior. J Adolesc Research. 2000;15(2):251–73. [Google Scholar]
- 53.Whitaker DJ, Miller KS, May DC, Levin ML. Teenage partners' communication about sexual risk and condom use: The importance of parent-teenager discussions. Fam Plann Perspect. 1999;31(3):117–21. Epub 1999/06/24. [PubMed] [Google Scholar]
- 54.Miller BC, Norton MC, Fan X, Christopherson CR. Pubertal Development, parental communication, and sexual values in relation to adolescent sexual behaviors. J Early Adolesc. 1998;18(1):27–52. [Google Scholar]
- 55.Santamaria EK, Dolezal C, Marhefka SL, Hoffman S, Ahmed Y, Elkington K, et al. Psychosocial implications of HIV serostatus disclosure to youth with perinatally acquired HIV. AIDS Patient Care STDS. 2011;25(4):257–64. doi: 10.1089/apc.2010.0161. Epub 2011/02/18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.UNAIDS. The Gap Report. Geneva, Switzerland: UNAIDS; 2014. [Google Scholar]
- 57.Dindia K, Allen M. Sex differences in self-disclosure: A meta-analysis. Psychological bulletin. 1992;112(1):106–24. doi: 10.1037/0033-2909.112.1.106. Epub 1992/07/01. [DOI] [PubMed] [Google Scholar]