Abstract
Magnetic resonance imaging (MRI) is the workhorse modality in pediatric neuroimaging because it provides excellent soft-tissue contrast without ionizing radiation. Until recently, studies were uninterpretable without sedation; however, given development of shorter sequences, sequences that correct for motion, and studies showing the potentially deleterious effects of sedation on immature laboratory animals, it is prudent to minimize sedation when possible. This manuscript provides basic guidelines for performing pediatric neuro MRI without sedation by both modifying technical factors to reduce scan time and noise, and using a multi-disciplinary team to coordinate imaging with the patient’s biorhythms.
Keywords: Anesthesia, Children, Magnetic resonance imaging, Neuroradiology, Sedation
Introduction
Early in the history of pediatric MRI, children were routinely sedated for scans, using a variety of oral (e.g., chloral hydrate) and intravenous (e.g., pentobarbital) agents. Sedation had no known contraindications, sequences were long, and studies were often uninterpretable without sedation as a result of severe motion degradation. However, given the development of shorter sequences and the publication of animal studies showing potentially deleterious effects of sedation and anesthesia on central nervous system development in immature laboratory animals [1–5], it is prudent to minimize sedation, when possible, while performing pediatric MRI.
The easiest and simplest method to reduce the need for sedation during the imaging of pediatric patients is reducing scan time. The key to this time reduction is to tailor the examination to the clinical question, eliminate sequences that provide minimal information, and obtain the necessary sequences as early and quickly as possible without compromising diagnostic quality. Other strategies for minimizing sedation vary depending on the age of the child, who can be placed in one of four categories: neonate (first several weeks of age), infant (week to 1 year of age), young child (1–6 years) or older child (older than 6 years). It should be noted that when patients are sick or unstable, it is best to perform imaging in a hospital under supervision of a clinician or anesthesiologist with experience in MRI sedation.
Clarify clinical question
Determining the clinical indication for the MRI request can be challenging depending on the institution and accessibility of the ordering pediatrician. Many ordering pediatricians are unaware that the MRI protocol varies with the clinical history and physical/laboratory findings. The protocol for a “head MRI” ordered to evaluate a firm lump on the head differs from that for a soft bluish head mass, while an MRI ordered after a seizure is even further distinct. A conversation with the referring physician and the child’s parents can provide additional information that was not included on the requisition. This information can reduce both the number of sequences acquired and scan time. The ideal protocol for the unsedated child provides the minimum amount of information necessary to answer the clinical question.
Preventing motion degradation
Patient age and the subtlety of anticipated findings determine the best imaging sequences for reducing patient motion during an MRI exam while simultaneously minimizing the use of anesthesia and sedation. Limited fast MRI with single shot-fast spin echo or half-Fourier acquisition single-shot turbo spin-echo (SSFSE or HASTE; Table 1) is often adequate to evaluate ventricular size in children with known hydrocephalus [6], although ultrasound can be used for the first several months [7]. When evaluating for readily apparent abnormalities such as a large infarct or hemorrhage, sequences that correct for motion but offer relatively low spatial resolution can be used. Evaluation for subtle pathology such as small infarcts, hemorrhages or subtle demyelination might require more numerous and time-intensive sequences, which are usually more susceptible to motion degradation (diffusion-weighted imaging, fast spin echo T2, magnetic resonance angiography, and magnetic resonance venography). When more time-intensive sequences are necessary, two-dimensional acquisitions can be obtained more quickly than volumetric acquisitions, reducing the likelihood of motion degradation (although limiting the number of planes in which the brain is evaluated). Scheduling the scan during nap time and having a quiet room for the parents to soothe the child prior to the study can also reduce motion artifact. Older children can be entertained and distracted with movies and music played in the scanner, allowing them to tolerate longer scans [8].
Table 1.
Rapid brain protocol
| Sequence | Coverage | Slice/gap (mm) | Notes |
|---|---|---|---|
| Ax SSFSE | WB | 4/1 | |
| Cor SSFSE | WB | 4/1 | |
| Options | |||
| Ax DWI | WB | 3 T–2/0, 1.5 T–3/0 | b=1,000, try PROPELLER if motion |
| Cor DWI | WB | 3 T–2/0, 1.5 T–3/0 | b=1,000 |
| Sag SSFSE | WB | 4/1 | |
Ax axial, Cor coronal, DWI diffusion-weighted imaging, PROPELLER periodically rotated overlapping parallel lines with enhanced reconstruction, Sag sagittal, SSFSE single-shot fast spin echo, T tesla, WB whole brain
Motion correction
In certain circumstances patient motion is unavoidable, and sequences that either prospectively correct for motion or are less sensitive to motion artifact can be used. PROPELLER (periodically rotated overlapping parallel lines with enhanced reconstruction) and BLADE imaging, where k-space is sampled in a Cartesian fashion in multiple radially oriented blades, can reduce motion artifact at the expense of spatial resolution and increased scan time; radial acquisition of k-space can reduce motion artifacts and decrease scan time [9]. Both of these techniques are restricted by image blurring and other artifacts. Newer methods such as PROMO (prospective motion correction) can prospectively compensate some image degradation by monitoring the motion of the child during the scan [10].
Reducing scan time
Checking the images after each sequence can reduce scan time for certain indications if sequences are done in an order that maximizes the chance of acquiring the necessary information with the earlier sequences. It also allows a second (or third) attempt when the sequence has been degraded by motion. When a study is performed for new signs and symptoms, the exam can be ended as soon as the diagnosis is established, even if not all of the originally protocolled sequences are obtained. Other indications, such as brain tumor follow-up, require a set number of sequences and cannot be shortened by checking sequences mid-exam. Occasionally, unexpected findings (an abnormal blood vessel or an unexpected mass) require adding sequences (or an additional scan) for a full evaluation.
Numerous technical factors can be modified to reduce image acquisition time, but these modifications might produce artifacts or sacrifice image quality. Sequences should be shortened only after careful consideration of such consequences. If acquiring images with a rectangular field of view, one can reduce the duration of the phase-encoding gradient by making the shorter direction the phase-encoding direction. Again, 2-D acquisitions are usually acquired more quickly than volumetric acquisitions. However, 3-D acquisitions allow reconstruction in any plane and are, therefore, equivalent to acquiring 2-D images in multiple planes and can ultimately be faster in certain clinical scenarios. Techniques that under-sample k-space by taking advantage of k-space symmetry, such as SSFSE/HASTE, can also reduce acquisition time, albeit with decreased sensitivity for small lesions [11]. Likewise, spiral acquisition of k-space can reduce motion artifacts and decrease scan time but can result in image blurring [9]. Parallel imaging with high channel count phased-array coils can also be used reduce scan time while retaining sensitivity [12] or to increase sensitivity instead of reducing scan time.
In a child with known shunted hydrocephalus and clinical concern for shunt dysfunction, a rapid non-sedated MRI with only SSFSE images is sufficient to compare ventricular size to the prior scan [6]. It is insufficient to identify any but the most obvious parenchymal abnormalities [11], but new parenchymal findings are unlikely in this setting. In contradistinction, an infant with macrocephaly and concern for hitherto undiagnosed hydrocephalus would require a more complete scan (Table 2), likely with sedation, because other etiologies of macrocephaly must be ruled out and the cause of the presumed hydrocephalus must be elucidated. In this situation, a steady-state imaging sequence (CISS, FIESTA) may be useful to evaluate for causes of cerebrospinal fluid flow obstruction (e.g., aqueductal stenosis [13]) and volumetric T1- or T2-weighted sequences might be necessary to identify an underlying malformation, tumor or metabolic disease, all of which could account for macrocephaly. In a child with hydrocephalus known to be secondary to a tumor or infection, a complete evaluation of the brain is always necessary when evaluating a change in clinical status to ensure the change is not from progression of the inciting pathology rather than simply worsening hydrocephalus.
Table 2.
Macrocephaly protocol
| Sequence | Coverage | Slice/gap (mm) | Notes |
|---|---|---|---|
| Sag T1 3-D | WB | 1/0 | Reformat Ax/Cor 1.5/1.5 mm |
| Cor 3-D FLAIR CUBE | WB | 1.2/0 | Reformat Ax/Sag 1.5/1.5 mm |
| Options | |||
| Ax T2 dual echo | WB | 4/2 | If leukoencephalopathy, TR=3,000 ms, TE=60/120 ms |
| MRS 2-D CSI | If leukoencephalopathy, 2-D box at level of BG to include posterior white matter | ||
| Gad 3-D T1 | WB | If new hydrocephalus, reformat Ax/Cor 1.5/1.5 mm | |
Ax axial, BG basal ganglia, Cor coronal, FLAIR fluid-attenuated inversion recovery, MRS magnetic resonance spectroscopy, Sag sagittal, TE echo time, TR repetition time, WB whole brain
Noise reduction
Noise is the most important modifiable determinant of the need for sedation in neonates and infants. Certain technical factors can reduce noise, including the use of diminished gradient slew rate and slow ramps for k-space readout [14], commonly used in combination with an ultrashort echo time (TE). Insulation of the inner bore of the magnet can further reduce the noise experienced by the child [15]. Inserting ear plugs and covering the ears with noise attenuators (Fig. 1) can reduce noise experienced by the child.
Fig. 1.
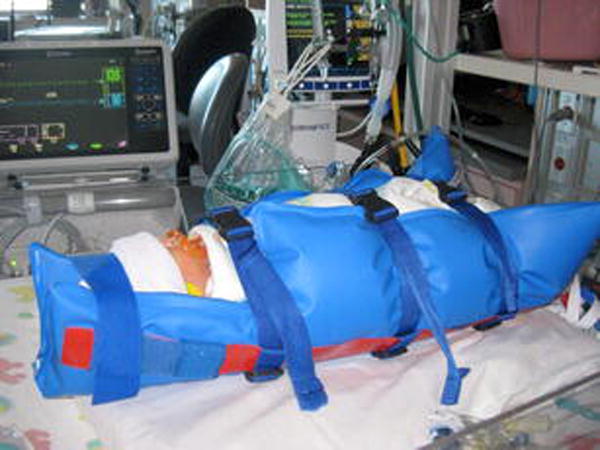
Photo shows a neonate wrapped in vacuum bean bag with noise attenuators in place, ready for transport to scanner suite
Special considerations in imaging neonates
The first-line method for minimizing neonatal motion during scans is the feed-and-swaddle technique; the second line is sedation using morphine or pentobarbital when feed and swaddle is unsuccessful. Successful feed and swaddle requires preparation and the scan time must be scheduled in advance, preferably coordinated with the neonate’s feeding schedule. Discussion with the parents and bedside nurse can help determine the ideal amount of time to allot for feeding, as the time required for a particular infant to feed determines how long before the scan the feeding should begin. Methods for soothing infants include frequent diaper changes, music and an oral sucrose solution. The bedside nurse and parents often know which works best for an individual infant.
One hour prior to scan, the infant should be partly wrapped in a blanket (inner layer), and a vacuum bean bag (outer layer), and given a head covering, swimmer’s ear plugs and ear muffs (Fig. 1). The neonate should be fitted with MRI-compatible ECG leads, an O2 saturation probe, a temperature probe and intravenous tubing. The vacuum bean bag should be tightened immediately prior to transport to the scanner (Fig. 2), which is kept on hold for the child. Preparing the infant prior to leaving the unit significantly reduces time in the scanner and reduces the chance of waking the child in the MRI suite. Try feed and swaddle first for short scans, recognizing that the technique is usually less successful with increasing scan time and increasing age. Successful feed and swaddle depends on a dedicated and communicative team approach to scanning infants, involving the parents, technologists and nursing staff.
Fig. 2.

Photo shows a neonate on the scanner table immediately prior to commencing feed-and-swaddle scan
When attempting to scan neonates using feed and swaddle, noise reduction is crucial. Insert ear plugs and cover ears with noise attenuators, and perform the noisiest sequences at the end of the scan. Additional technical methods to reduce noise, as mentioned previously, include diminished gradient slew rate and slow ramps for k-space readout [14], and even insulation of the inner wall of the magnet’s bore [15]. Even the longer-duration neonatal encephalopathy protocol (Table 3), with its greater number of noisier sequences, can be performed with feed and swaddle; motion-degraded sequences are simply repeated until they are of diagnostic quality. In rare situations when severe motion degradation precludes a diagnostic examination, quick consultation with the ordering clinicians during the study to develop a plan for a scan under sedation or repeat feed and swaddle scan can help minimize unproductive time in the scanner.
Table 3.
Neonatal encephalopathy protocol
| Sequence | Coverage | Slice/gap (mm) | Notes |
|---|---|---|---|
| Ax DWI | WB | 3 T–2/0, 1.5 T–3/0 | b=700 |
| Sag 3-D T1 | WB | 1.5/0 | Reformat Ax/Cor 1.5/1.5 mm |
| Ax T2 dual echo | WB | 4/2 | TR=3,000 ms, TE=60/120 ms |
| Cor 3-D T2 | WB | Reformat Ax/Sag 1.5/1.5 mm | |
| Ax 3-D ISI | WB | SWAN (GE), VEN BOLD (Philips), SWI (Siemens) Reformat Ax 2/6 mm |
|
| Ax 3-D TOF MRA | COW-C2 | b=1,000 | |
| Cor MRV INHANCE | WB | Use correct venc | |
| MRS SV BG, short and long TE | BG | TE=35 ms and TE=258 ms Over BG/thalamus |
|
| Options | |||
| Ax T1 | WB | 4/1 | If gad to be given, acquire pre-gad T1 |
| Gad Ax T1 | WB | 4/1 | |
| Gad Cor T1 | WB | 4/1 | |
Ax axial, BG basal ganglia, Cor coronal, COW circle of Willis, DWI diffusion-weighted imaging, Gad gadolinium, ISI iron-sensitive imaging, MRA magnetic resonance angiography, MRS magnetic resonance spectroscopy, MRV magnetic resonance venography, Sag sagittal, SV single voxel, SWAN T2-star weighted angiography, SWI susceptibility-weighted imaging, TE echo time, TR repetition time, VEN BOLD venous blood oxygen level dependent, WB whole brain
Special considerations in imaging infants
For infants 3 months and younger, the feed-and-swaddle method is useful for relatively short protocols, but with increasing age and scan time this technique is less successful. The next line for these younger infants is sedation with pentobarbital (1 mg/kg/dose) and morphine (0.05 mg/kg/dose). For infants older than 3–6 months, fast scans for hydrocephalus can still be done without sedation using a fast MRI protocol (Table 1). For higher-quality scans, such as those needed for tumor or refractory epilepsy (Table 4) with a high likelihood of subsequent surgery, general anesthesia with propofol is often necessary. In these cases, speed is secondary to the goal of acquiring high-quality diagnostic images in order to avoid the need for repeated anesthesia. The fundamental principles for maintaining high signal-to-noise ratio include avoiding a (too) small field of view, (too) thin sections and (too) small voxels when possible. Thicker sections and larger voxels are completely adequate for infarcts, encephalopathy and large masses. Using a rectangular field of view can decrease imaging time while maintaining signal to noise. These protocol modifications can produce good image quality while minimizing sedation time; for any sedated scan, however, the overriding objective must be answering the clinical question. Other options (usually used for follow-up or research studies) include bringing the children in at night (a little past bedtime), having them fall asleep and then putting them in the scanner.
Table 4.
Pediatric seizure protocol
| Sequence | Coverage | Slice/gap (mm) | Notes |
|---|---|---|---|
| Sag T1 3-D | WB | 1/0 | Reformat Ax/Cor 1.5/1.5 mm |
| Ax T2 single echo | WB | 4/2 | Long TE, not CUBE |
| Cor 3-D FLAIR CUBE | WB | 1.2/0 | Reformat Ax/Sag 1.5/1.5 mm |
| Cor 3-D T2 | WB | 1.5/0 | Scan if child is 3–9 months Reformat Ax/Sag 1.5/1.5 mm |
| Ax 3-D ISI | WB | 4/1 | SWAN (GE), VEN BOLD (Philips), SWI (Siemens) |
| Ax & Cor DWI | WB | 3 T–2/0, 1.5 T–3/0 | b=1,000 |
| Options | |||
|
Cor FMPIR T2 Cor |
3/0 | TI=120 ms Temporal lobes |
|
| MRS 2-D CSI | 2-D box at level of BG to include posterior white matter; check for developmental delay or suspected metabolic disorder | ||
| Ax T1 | WB | 4/1 | |
| Gad Ax T1 | WB | 4/1 | |
| Gad Cor T1 | WB | 4/1 | |
| Gad 3-D T1 | WB | Reformat Ax/Cor 1.5/1.5 mm for small lesions | |
Ax axial, BG basal ganglia, Cor coronal, DWI diffusion-weighted imaging, FLAIR fluid-attenuated inversion recovery, FMPIR fast multiplanar inversion recovery, Gad gadolinium, ISI iron-sensitive imaging, MRS magnetic resonance spectroscopy, Sag sagittal, SWAN T2-star weighted angiography, SWI susceptibility-weighted imaging, T tesla, TE echo time, TI inversion time, VEN BOLD venous blood oxygen level dependent, WB whole brain
Special considerations in imaging young children
Young children, ages 1–5 years, are the most difficult to scan without sedation. The likelihood of success is greatest when the scan is coordinated with child’s biorhythms. A dedicated child life team can help reduce need for sedation in young children in some circumstances [16]. Schedule the scan at the child’s nap time, whenever possible, and have a quiet room for the parents to sooth the child before the scan, and perform the most quiet sequences first. Modifying technical parameters, as previously discussed, can help reduce scan time, but when the study indication requires fine anatomical detail, signal to noise cannot be sacrificed to reduce scan time. With 5- to 6-year-old children, who can sometimes stay still for about 20 min, scan for as long as the child is comfortable, give the child a 15- to 30-min break (enough to perform a quick MRI such as for hearing loss), and then resume scanning. If higher-quality, longer scans are necessary given the study indication, general anesthesia is still required.
Special considerations in imaging of older children
Older children are more able to cooperate with an MRI exam, especially when the process is explained in advance and they have an idea of what to expect. An initial visit the day before the exam, or earlier on the day of the exam, and involvement of a dedicated child life team [16] can help make the experience less intimidating for the child and parents. Including the parents helps to reduce both the child’s and the parents’ anxiety. Using pictures, comics and videos to explain the test, and simulating the exam reduces the number of steps that are new or frightening. A mock MRI scanner can be used to further familiarize the child with the imaging process on the day prior to the exam [17]. Children of these ages can be distracted during the scan with videos and music [8]. A treasure box with toys can provide positive reinforcement and give the child a sense of accomplishment. Again, reducing scan time and noise when possible is always beneficial, although this is less critical in this age group than in younger children.
Conclusion
Sedation for pediatric brain MRI is unavoidable in certain clinical and diagnostic scenarios, but given the growing concern regarding the risks of sedation, each case should be evaluated individually, with the goal of minimizing the use of sedation while still addressing the clinical indication. Neonates should be scanned without sedation if possible, using a combination of feed and swaddle, noise reduction and optimization of sequences to avoid motion. Infants can be scanned without sedation in some cases using feed and swaddle, but longer and more complex scans in older infants might require sedation. Young children (ages 1–6 years) usually require sedation for studies other than rapid ventricle checks. Many older children can cooperate with MR scans without sedation when the process is explained in advance, when they have the opportunity to take a break during the exam, and when videos and music are available for entertainment. Tailoring each protocol to the clinical indication and study can both reduce the need for sedation and maximize the yield of sedated studies.
Acknowledgments
Dr. A. J. Barkovich receives funding from the National Institute of Neurological Disorders and Stroke for grant R01NS046432.
Footnotes
Compliance with ethical standards
Conflicts of interest None
References
- 1.Ikonomidou C, Bosch F, Miksa M, et al. Blockade of NMDA receptors and apoptotic neurodegeneration in the developing brain. Science. 1999;283:70–74. doi: 10.1126/science.283.5398.70. [DOI] [PubMed] [Google Scholar]
- 2.Jevtovic-Todorovic V, Hartman RE, Izumi Y, et al. Early exposure to common anesthetic agents causes widespread neurodegeneration in the developing rat brain and persistent learning deficits. J Neurosci. 2003;23:876–882. doi: 10.1523/JNEUROSCI.23-03-00876.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bercker S, Bert B, Bittigau P, et al. Neurodegeneration in newborn rats following propofol and sevoflurane anesthesia. Neurotox Res. 2009;16:140–147. doi: 10.1007/s12640-009-9063-8. [DOI] [PubMed] [Google Scholar]
- 4.Bajic D, Commons KG, Soriano SG. Morphine-enhanced apoptosis in selective brain regions of neonatal rats. Int J Dev Neurosci. 2013;31:258–266. doi: 10.1016/j.ijdevneu.2013.02.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Olney JW, Wozniak DF, Jevtovic-Todorovic V, et al. Drug-induced apoptotic neurodegeneration in the developing brain. Brain Pathol. 2002;12:488–498. doi: 10.1111/j.1750-3639.2002.tb00467.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Patel DM, Tubbs RS, Pate G, et al. Fast-sequence MRI studies for surveillance imaging in pediatric hydrocephalus. J Neurosurg Pediatr. 2014;13:440–447. doi: 10.3171/2014.1.PEDS13447. [DOI] [PubMed] [Google Scholar]
- 7.Gupta P, Sodhi KS, Saxena AK, et al. Neonatal cranial sonography: a concise review for clinicians. J Pediatr Neurosci. 2016;11:7–13. doi: 10.4103/1817-1745.181261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Courtier J, Cardenas A, Tan C, et al. Nonanesthesia magnetic resonance enterography in young children: feasibility, technique, and performance. J Pediatr Gastroenterol Nutr. 2015;60:754–761. doi: 10.1097/MPG.0000000000000712. [DOI] [PubMed] [Google Scholar]
- 9.Forbes KP, Pipe JG, Karis JP, et al. Brain imaging in the unsedated pediatric patient: comparison of periodically rotated overlapping parallel lines with enhanced reconstruction and single-shot fast spin-echo sequences. AJNR Am J Neuroradiol. 2003;24:794–798. [PMC free article] [PubMed] [Google Scholar]
- 10.White N, Roddey C, Shankaranarayanan A, et al. PROMO: real-time prospective motion correction in MRI using image-based tracking. Magn Reson Med. 2010;63:91–105. doi: 10.1002/mrm.22176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Patel MR, Klufas RA, Alberico RA, Edelman RR. Half-fourier acquisition single-shot turbo spin-echo (HASTE) MR: comparison with fast spin-echo MR in diseases of the brain. AJNR Am J Neuroradiol. 1997;18:1635–1640. [PMC free article] [PubMed] [Google Scholar]
- 12.Pruessmann KP, Weiger M, Scheidegger MB, Boesiger P. SENSE: sensitivity encoding for fast MRI. Magn Reson Med. 1999;42:952–962. [PubMed] [Google Scholar]
- 13.Algin O, Hakyemez B, Parlak M. Phase-contrast MRI and 3D-CISS versus contrast-enhanced MR cisternography on the evaluation of the aqueductal stenosis. Neuroradiol. 2010;52:99–108. doi: 10.1007/s00234-009-0592-x. [DOI] [PubMed] [Google Scholar]
- 14.de Zwart JA, van Gelderen P, Kellman P, Duyn JH. Reduction of gradient acoustic noise in MRI using SENSE-EPI. Neuroimage. 2002;16:1151–1155. doi: 10.1006/nimg.2002.1119. [DOI] [PubMed] [Google Scholar]
- 15.Dean DC, 3rd, Dirks H, O’Muircheartaigh J, et al. Pediatric neuroimaging using magnetic resonance imaging during non-sedated sleep. Pediatr Radiol. 2014;44:64–72. doi: 10.1007/s00247-013-2752-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.McGuirt D. Alternatives to sedation and general anesthesia in pediatric magnetic resonance imaging: a literature review. Radiol Technol. 2016;88:18–26. [PubMed] [Google Scholar]
- 17.de Bie HM, Boersma M, Wattjes MP, et al. Preparing children with a mock scanner training protocol results in high quality structural and functional MRI scans. Eur J Pediatr. 2010;169:1079–1085. doi: 10.1007/s00431-010-1181-z. [DOI] [PMC free article] [PubMed] [Google Scholar]


