Highlights
-
•
A five-factor theoretical model is proposed.
-
•
The SEM model evaluated relationships among three endogenous and two exogenous variables.
-
•
Higher levels of medication adherence had a significant direct effect on diabetes distress.
-
•
Self-care activities had significant direct effect on diabetes distress and HRQoL.
-
•
Diabetes-specific QoL had a significant effect on HRQoL.
Keywords: Health-related quality of life, Type 2 diabetes mellitus, Structural equation modeling, Self-care activities, Diabetes distress, Medication adherence
Abstract
Aims
Health-Related Quality of Life (HRQoL) has been increasing attention in health outcome studies. Factors that individually influence HRQoL, diabetes self-care behaviors, and medication adherence have been widely investigated; however, most previous studies have not tested an integrated association between multiple health outcomes. The purpose of this study was to formulate a hypothetical structural equation model linking HRQoL, diabetes distress, diabetes self-care activities, medication adherence and diabetes-dependent QoL in patients with Type 2 Diabetes Mellitus (T2DM).
Methods
A cross-sectional study design was employed, and 497 patients with T2DM were recruited from outpatient clinics in three public hospitals and one government clinic. The patients completed a series of questionnaires. The hypothetical model was tested using Structural Equation Modeling (SEM) analysis.
Results
The values of the multiple fit indices indicated that the proposed model provided a good fit to the data. SEM results showed that medication adherence (MMAS) had a significant direct effect on diabetes distress (PAID) (Beta = −0.20). The self-care activities (SDSCA) construct was significantly related to PAID (Beta = −0.24). SDSCA was found to have a significant relationship with HRQoL (SF-36) (Beta = 0.11). Additionally, diabetes distress had a significant effect (Beta = −0.11) on HRQoL of patients. Finally, ADDQoL had a significant effect on HRQoL (Beta = 0.12).
Conclusions
The various health outcome indicators such as self-care behaviors, diabetes distress, medication adherence and diabetes-dependent QoL need to be considered in clinical practice for enhancing HRQoL in those patients.
Introduction
Diabetes Mellitus (DM) is one of the most important public health concerns. The prevalence of DM has increased dramatically in most countries in the world. Recently, it is estimated that the number of DM patients will increase from 171 million to 366 million between the years 2000 and 2030 [46]. As Malaysia continues its progress as a nation both socially and economically, disease patterns and burdens are changing due to changes in lifestyle and dietary patterns of its population. According to the National Health and Morbidity Survey, the prevalence of DM among Malaysian adults aged older than 30 years had increased from 6.3% in 1986, 8.3% in 1996 and 14.9% in 2006 to finally hitting 15.2% in 2011 [17]. By the year 2030, Malaysia is expected to rank tenth with the highest rate of diabetes worldwide. This increase in the number of people with Type 2 Diabetes Mellitus (T2DM) will be synonymous to huge human burden. T2DM has thus been found to have unfavorable effects on the Heath-Related Quality of Life (HRQoL) of patients [2], [28].
To assess HRQoL and diabetes-specific factors, many instruments have been developed over time to obtain the perceived behavior of patients. Some are intended for general use, irrespective of the illness and condition of the patient. The generic instruments are often applicable to even healthy people. Some of the earliest ones were developed initially with population surveys in mind, but later were extended to include clinical trial settings. These instruments are commonly described as QoL scales and they are measures of health status since the focus is mainly physical symptoms. Some generic HRQoL measures, such as the SF-36, contain the essential elements of HRQoL and they are also easily cross-culturally validated [8]. The generic scale instruments allow for HRQoL comparisons among different group of patients. On the other hand, the disease-specific instrument attempts to capture only the specific impact of a disease on the patient’s functioning and well-being [8], [14]. The disease-specific instrument renders it more difficult to assess HRQoL for patients having multiple diseases while the HRQoL instrument is based on the specific health condition of a patient. Therefore, a combination of generic and disease-specific instruments may be more appropriate in measuring the patient’s health status [4]. However Herdman et al. [15] proposed for the validation of the diabetes-specific QoL instruments in Asian countries. This is due to the increase in implementation of patient reported outcomes in large clinical trials. Thus, Asia must de facto be included since it is one of the most densely populated continents in the world [43]. Among all the diabetes-specific QoL measures, the Audit of Diabetes Dependent QoL instrument is one of the most widely translated and validated in more than 20 languages as well as the Problem Areas in Diabetes Scale (PAID) [11], [13], [31], [35].
The major objective in the treatment of T2DM is to lower the blood glucose levels in the normal and/or near normal range [29]. A set of indicators for diabetes care has been recommended, such as measuring the control of blood sugar [23]. HRQoL has been posited to be another important health outcome measure. T2DM is a lifelong health condition which can affect the patients’ condition significantly. The Quality of Life (QoL) of T2DM patients has been shown to be affected with disease progression and response to medication therapy [2]. Health behaviours are commonly suggested as proximal health outcomes of HRQoL. Self-care in diabetes has been defined as an evolutionary process of development of knowledge or awareness by learning to survive with the complex nature of T2DM in a social context [30]. Since the vast majority of day-to-day care in diabetes is handled by patients and/or families [2], there is an important need for reliable and valid measures for self-management of T2DM [18]. Individuals with diabetes need to perform specific multifaceted activities in their daily lives, such as having an appropriate diet, regular exercising, monitoring their blood glucose levels, foot care and medication self-administration [28]. Patients with low adherence to self-care activities such as exercise and medication were found to have lower HRQoL [28]. On the other hand, diabetes self-care activities are reported to be positively related to HRQoL for adhering patients [16], [25].
Psychological factors such as diabetes-related emotional distress were found to be associated with lesser adherence to diet, exercise, frequent blood glucose testing and medication regimens [9], [26], [27], [33]. Previous studies have also found that health-related quality of life were inversely related to diabetes self-care activities and they reported that the EuroQoL-5 dimensions (EQ-5D) index was significantly associated with non-adherence to foot care, exercise duration and smoking [28]. The diabetes-dependent quality of life is also an important indicator of HRQoL. Wee et al. [43] reported that respondents who scored a better EQ-5D index have better Audit of Diabetes Dependent QoL (ADDQoL) Average Weighted Index scores (Spearman correlation = 0.54, p-value < 0.01). Diabetes distress was also found to be significantly related to medication adherence. Patients who are non-adherent to their daily medication intake had a higher level of diabetes-specific emotional distress [26].
The aim of this study is to test a structural model that links diabetes distress, medication adherence, self-care activities, diabetes-specific QoL and HRQoL using a sample of T2DM patients in Malaysia. This is the first study in Malaysia that extensively investigates the relationships among a number of physiological, psychological, behavioral predictors and adaptive outcomes using psychometrically validated instruments via Structural Equation Modeling (SEM). Literature on diabetes studies has demonstrated that various factors can individually influence HRQoL, diabetes self-care activities, medication adherence, and diabetes-dependent QoL and diabetes distress. However, most of the previous studies are yet to test a model regarding the multiple associations among these variables. The remainder of this paper is organised as follows: The methodology is explained in Section 2. The SEM results are then presented in Section 3 while Section 4 discusses the findings.
Material and methods
Study design and sample
This study involves a cross-sectional design. The patients were recruited from three hospitals namely Hospital Tuanku Ampuan Rahimah, Hospital Sungai Buloh and Hospital Serdang and a government public health clinic; Klinik Kesihatan Botanic. The three hospitals and the clinic were located in the state of Selangor, Malaysia. The inclusion criteria for the patients who participated was: 1. They were aged above 18 years 2. They were diagnosed with T2DM for at least one year 3. They were taking T2DM diabetes medications and 4. They were able to speak, read and write either in English or Malay language. On the other hand the exclusion criteria was: 1. Participants with gestational diabetes or mental disorders and 2. Those who were not able to read in Malay/English language. Sample size was calculated based on the need to conduct the Structural Equation Modeling (SEM) analysis which means that minimum of 200 subjects was necessary for adequate model specification [7]. The Medical Research Ethics Committee in Kuala Lumpur, Malaysia, through the National Medical Research Register (NMRR) granted the permission for this research.
Instrumentation
For this study, the self-reported questionnaire consisted of socio-demographic questions such as age and duration of diabetes. Participants were also asked to complete five questionnaires: (1) Problem Areas in Diabetes Scale (PAID); (2) Audit of Diabetes-Dependent Quality of Life-19 item (ADDQoL-19); (3) Morisky Medication Adherence Scale (MMAS); (4) Summary of Diabetes Self-Care Activities (SDSCA), and (5) Short-Form 36 (SF-36).
The five instruments used in this paper are either generic or diabetes-specific and were chosen on the basis of the number of items, time taken to complete the questionnaire and their purpose. The ADDQoL and PAID instruments were firstly chosen since they were the most popular and have high internal consistency reliabilities in comparison to the other diabetes-specific instruments [32], [44]. Moreover, to study diabetes-related QoL, the ADDQoL was the most suitable since it allows the subject to judge the relevance or importance of each item and to eliminate non-relevant or non-important items from consideration before calculating the final weighted score [6]. This study also aimed at looking into the psychological aspect of diabetes and thus PAID instrument was chosen since it is the most commonly used to measure diabetes-specific emotional distress [26]. Since self-care behaviours are a very important aspect of diabetes, the SDSCA was chosen. The SDSCA takes into consideration various important domains such as diet, exercise, blood sugar testing and foot examination (Toobert, Hampson, & Glasgow, 2000). Lastly to look into the medication aspect, the Morisky Medication Adherence Scale was picked since it is the most concise and easiest to administer among patients [20] in contrast to other diabetes-specific medication instruments. The five chosen instruments are discussed as follows:
Problem Areas in Diabetes Scale (PAID)
The PAID instrument comprises of 20 statements identified as the common diabetes emotional distress reported in both T1DM and T2DM patients [26]. The PAID consists of 20 items that the patient rates on a 5-point Likert scale (0: Not a problem, 1: Minor problem, 2: Moderated problem, 3: Somewhat serious problem and 4: Serious problem). The total score ranges from 0 to 100 with higher scores indicating greater emotional distress. The total score is achieved by adding the 0–4 responses given for the 20 items and by multiplying this sum by 1.25 [45]. This instrument has been reported to have adequate validity and reliability [26], [33], [44], [45]. The Cronbach’s Alpha values ranged between 0.93 and 0.95 [42], [44] hence supporting high internal consistency and reliability.
Audit of Diabetes-Dependent QoL (ADDQoL)
The ADDQoL comprises of 19 items and it is the third version after the 13-item and the 18-item ADDQoL measures [6]. The ADDQoL assesses the impact of diabetes on 19 life domains specifically. The first two items assesses the present Quality of Life (QoL) and diabetes-related QoL. The remaining items ask the respondents to rate how particular aspects of their life would be affected if they did not have diabetes and this particular rating is a five-point Likert scale ranging from −3 to 1 (impact). Thereafter, the second part of the question requires the patients to answer the importance of these domains of their life using a four-point Likert scale from 0 to 3 (importance). For five of the items, if the participants selected the ‘Not Applicable’, it will be counted as a missing data and is generally not included in the calculation of the average impact score. The two ratings (impact and importance) are then multiplied and summed to calculate the Average Weighted Score (AWI) whereby more negative scores indicate a negative impact on QoL [36], [43]. Good reliability and internal consistency were reported in the 18-item version [5] and with the latest 19-item version [9].
Morisky Medication Adherence Scale (MMAS)
Morisky et al. [20] originally developed a four-item medication adherence scale. The four-item scale exhibits poor psychometric properties but it is still widely used in self-reporting medication adherence. Recently, Morisky et al. [19] developed an eight-item scale known as the Morisky Medication Adherence Scale (MMAS). The questions were formulated in such a way so that the respondents avoid a “yes-saying” bias. The response choices consist of yes/no for questions 1 to 7 and a 5-point Likert scale for the last item (Item 8). The scoring is such that each “no” response is rated as “1” and the “yes” response as “0” except for question 5 (Did you take your diabetic medicine yesterday?) which is the reverse, i.e. “yes” is rated as 1 and “no” as 0. For item 8 (How many times do you have difficulty remembering to take all your medications?), if the patient responds “0 (Never/Rarely)”, the score is “1” and if response “4 (All the time)” is chosen, the score is “0”. Responses to the item 1 is rated as 0.25, item 2 as 0.75 and finally item 3 as 0.75 respectively based on the scoring method from the original developer. The total score for the MMAS-8 ranges from 0 to 8. The scores are then categorized as low (less than 6), medium (6 to less than 8) and high (8) medication adherence subsequently.
Summary of Diabetes Self-Care Activities (SDSCA)
The SDSCA measures the diabetes self-care behavior. The SDSCA is a popular and well-known instrument which has been applied widely in the diabetes management studies. The SDSCA is a valid and reliable instrument having moderate inter-item reliability (r = 0.59 – 0.74) [38]. Furthermore, the SDSCA is a self-report measure consisting of 12 items: 10 items to measure four components of diabetes self-management namely diet, exercise, blood sugar testing, foot care and two questions on tobacco use. The respondents are asked to rate how many days during the past 7 days they performed a specific self-care behavior. The scale ranges from 0 to 7, and the higher scores correspond to higher diabetes management activities [45]. The two items on smoking were ‘Have you smoked a cigarette-even one puff-during the past seven days? 0. No, 1. Yes (Number of cigarettes).’ A mean score is calculated for each of the five domains (diet, exercise, blood glucose testing, foot care, and smoking) whereby higher scores indicate better diabetes self-management. Adequate internal and test-retest reliability, validity and sensitivity to change were demonstrated by the normative data from seven studies [37]. For the purpose of this study, only 10 questions from the SDSCA were used excluding the question on smoking.
Short Form 36 (SF-36)
The SF-36 Health Survey version 2.0 comprises 36 questions which measure self-reported outcomes on eight HRQoL domains. The domains are as follows: physical functioning (PF), social functioning (SF), role limitation due to physical problems (PF), role limitation due to emotional problems (RE), mental health (MH), energy and vitality (VT), bodily pain (BP), and the general health perception (GH). The SF-36 also includes an item to assess the change in respondent’s health status during the past year [12]. The SF-36 scores range from 0 to 100, 0 indicating the poorest health related quality of life and 100 being the highest. For each quality of life domain tested, the item scores were coded, summed and transformed into a scale from 0 (worst) to 100 (best) using the available algorithm described by the SF-36 developers [40]. The Physical Component Score (PCS) and the Mental Component Score (MCS) were both calculated by using standard weights in order to interpret the summary scales comprehensively. The SF-36 version 2 was scored based on the scoring algorithm developed by [41]. The Quality Metric organization provided the scoring algorithm software under the SF-36 license.
Statistical analysis
Data were analyzed using IBM SPSS STATISTICS 22.0 and IBM SPSS AMOS 18.0. Descriptive statistics were used for the participants' characteristics and measured variables. Cronbach’s alpha was computed for the variables. The percentage response rates were 75.4%, 91.6%, 94.0% and 91.7% for Hospital Tuanku Ampuan Rahimah, Hospital Sungai Buloh, Hospital Serdang and Klinik Kesihatan Botanic respectively. The overall response rate for this study was 82.8% with 497 usable questionnaires. Structural Equation Modelling (SEM) technique was used to analyse the data. Confirmatory Factor Analysis (CFA) was employed to test the measurement model. The structural equation model was determined to examine the relationship between the exogenous and endogenous constructs. The model was evaluate using multiple criteria: χ2 test, Goodness-of-Fit Index (GFI) greater than 0.90, Comparative-Fit Index (CFI) greater than 0.90, Normed-Fit Index (NFI) greater 0.90, and Root Mean Square Error of Approximation (RMSEA) less than 0.08 [3]. Hypotheses regarding the structural relationships of the constructs in the final model were evaluated using the magnitude of path coefficients (standardized coefficient) and their significance. Prior to SEM, the data was checked for normality, outliers and multicollinearity.
Results
Participants
Overall, the sample comprised of 53.7% males and 46.3% females. The mean age was 55.5 (SD = 10.9) years and ranged from 25 to 85 years. The mean duration of diabetes was 9.97 (SD = 7.74) years ranging from 1 to 37 years. The mean Body Mass Index (BMI) was 28.56 (SD = 6.51) ranging from 24.84 to 72.62 kg/m2. The mean duration of oral medication intake was 9.25 years (SD = 7.75) to control their diabetes. In addition, the mean duration of insulin injection was 4.09 (SD = 4.53) years. From Table1, 47.7% were Malays (n = 237), 34.8% were Indians/Punjabis (n = 173), and 17.5% (n = 87) were Chinese respectively. The majority of the respondents was married (83.9%) and attended secondary school (54.3%). For those who were working, the most frequently reported income was less than RM1000 (42.9%). Most participants were living with spouse and children (59.6%) or spouse (16.3%) and only 2.8% were living alone. About 78.1% had medical conditions and it consisted of arthritis (13.5%), heart disease (21.5%), hypertension (54.5%), and high cholesterol (34.2%), and lung problems (3.6%).
Table 1.
Demographic characteristics (n = 497).
| Variable | n | % | |
|---|---|---|---|
| Gender | Male | 267 | 53.7 |
| Female | 230 | 46.3 | |
| School | No schooling | 21 | 4.2 |
| Primary school | 92 | 18.5 | |
| Secondary school | 270 | 54.3 | |
| University | 99 | 19.9 | |
| Others | 13 | 2.6 | |
| Ethnicity | Malay | 237 | 47.7 |
| Chinese | 87 | 17.5 | |
| Indian | 173 | 34.8 | |
| Marital status | Single | 26 | 5.2 |
| Married | 417 | 83.9 | |
| Divorced | 13 | 2.6 | |
| Widowed | 39 | 7.8 | |
| Working | Yes | 184 | 37.0 |
| No | 193 | 38.8 | |
| Retired | 119 | 23.9 | |
| Income | <RM1000 | 213 | 42.9 |
| RM 1000–3000 | 51 | 10.3 | |
| RM 3001–5000 | 127 | 25.6 | |
| RM 5001–8000 | 72 | 14.5 | |
| >RM8001 | 32 | 6.4 | |
| Living | With spouse | 81 | 16.3 |
| With spouse and children | 296 | 59.6 | |
| With children | 74 | 14.9 | |
| Alone | 14 | 2.8 | |
| Others | 29 | 5.8 | |
| Medical conditions | Yes | 388 | 78.1 |
| No | 109 | 21.9 | |
| Comorbidities | |||
| Arthritis | Yes | 67 | 13.5 |
| No | 417 | 83.9 | |
| Heart disease | Yes | 107 | 21.5 |
| No | 377 | 75.9 | |
| Hypertension | Yes | 271 | 54.5 |
| No | 212 | 42.7 | |
| High Cholesterol | Yes | 170 | 34.2 |
| No | 314 | 63.2 | |
| Lung problems | Yes | 18 | 3.6 |
| No | 466 | 93.8 |
Structural equation model
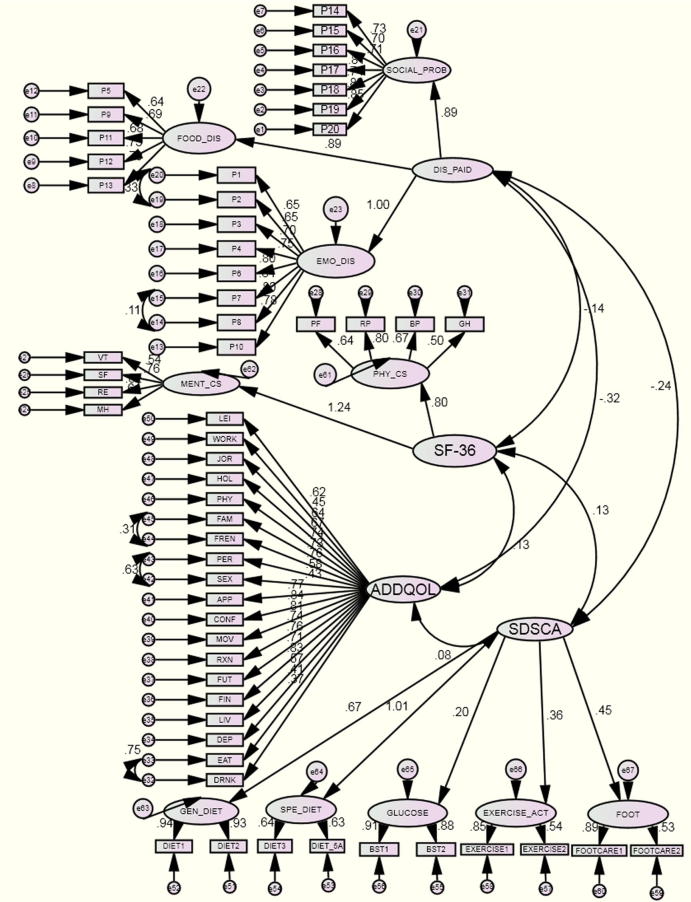
A four-factor measurement model (Model 1a) firstly examined whether the endogenous and exogenous variables fitted the data well using CFA. In this particular model, the PAID (diabetes distress) was a second-order construct with three factors or components (social support, food and emotional problems). The SF-36 was a second-order construct measured by two components (PCS and MCS), the ADDQoL (diabetes-specific QoL) was a first-order construct with 19 items and finally, the self-care construct was a second-order construct with five components, general diet, specific diet, blood glucose, exercise and foot care respectively. In this initial measurement model testing, the criteria for model fit indices were partially met, with a χ2 = 4024.5, χ2/df = 2.641, GFI = 0.774, CFI = 0.848 and RMSEA = 0.058 (0.055, 0.060). Then, the post-hoc modifications were used to improve the fit based on modification indices. The errors e42 (SEX) and e43 (PER) on the ADDQoL construct and the other pair of error terms such as e32 (DRNK) and e33 (EAT); and e45 (FAM) and e44 (FREN) were allowed to be correlated. The re-specification was undertaken based on the theoretical justification. For the PAID construct, e15 (P7) and e14 (P8); and e20 (P1) and e19 (P2) were also allowed to correlate. After which, the measurement model (see Fig. 1) results revealed that the model fitted the data adequately well: χ2 = 3266.4, χ2/df = 2.150, GFI = 0.804, CFI = 0.90 and RMSEA = 0.049 (0.046, 0.051) Fig. 2.
Fig. 1.
Measurement Model.
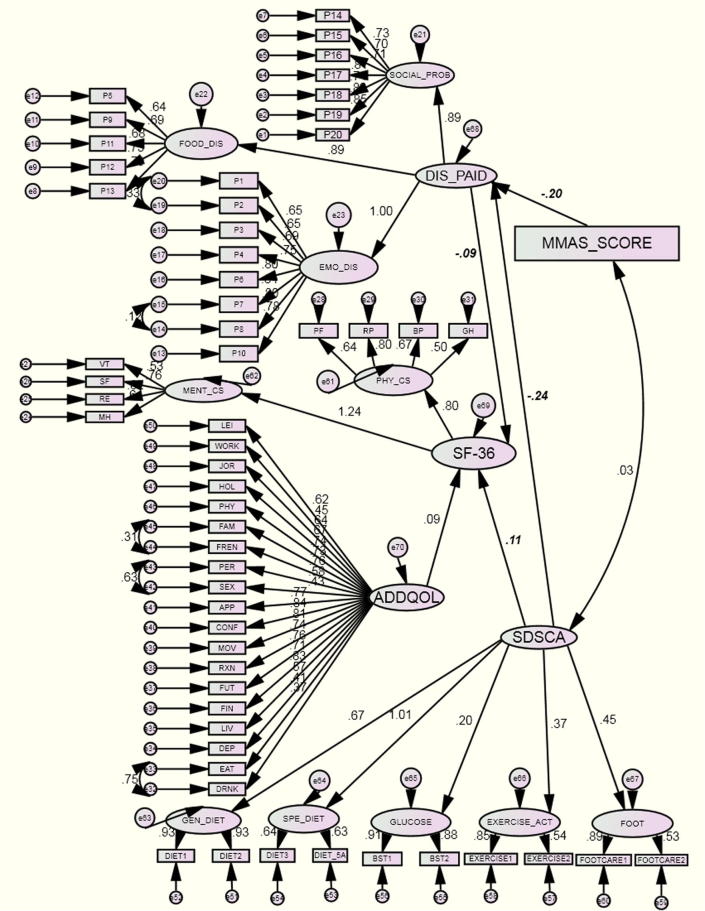
Fig. 2.
Structural Model.
The structural equation model (SEM) evaluated the directional analytic relationships among the three endogenous variables and the two exogenous variables which were formerly hypothesized. Three pairs of error terms on the ADDQoL construct; and two pairs of error terms were allowed to be correlated in the structural model which was similar to the measurement model. The overall goodness-of-fit statistics revealed that the structural regression model fitted the data well: the χ2 statistic was 3375.9 based on 1576 df, which was statistically significant (p-value = 0.000). The χ2/df ratio was 2.142, which was less than the recommended value of 5.0. The CFI (0.90), GFI (0.802) and TLI (0.885) showed satisfactory fit indices. The RMSEA was 0.048 (90% CI = 0.046, 0.050), which was desirably small indicating a well-fitted model. From the final model, medication adherence (MMAS) had a significant direct effect on diabetes distress ( = −0.20, p < 0.001). Results suggested that patients with higher levels of medication adherence had lower levels of diabetes-specific distress. The construct of self-care activities was significantly related to diabetes distress ( = −0.24, p = 0.001). Similarly, self-care activities were found to have a significant relationship with HRQoL ( = 0.11, p = 0.040). This result indicated that T2DM patients who had higher level of diabetes self-care activities reported higher health-related quality of life. Furthermore, diabetes distress had a significant effect on HRQoL ( = −0.11, p < 0.001) demonstrating that patients with higher level of diabetes-specific emotional distress has lower health-related quality of life on the SF-36 scale. Finally, as hypothesized, diabetes-specific QoL (ADDQoL) had a significant effect on HRQoL ( = 0.12, p < 0.001).
Discussion
The increase in the number of people with Type 2 Diabetes Mellitus (T2DM) contributes to human and economic burden as it causes other diseases such as cardiovascular disease, blindness, dementia or Alzheimer. Due to diabetes, many patients had to have their legs amputated [21], [29]. Medications for TDM can cause other serious problems (heart attack or death) [10].
The results of this study confirmed that patients with higher levels of medication adherence had lower levels of diabetes-specific distress. This result was in accordance with prior studies suggesting that medication adherence plays an important role in predicting diabetes-specific distress [9], [27]. Thus, medication-focused strategy among type 2 diabetes patients can be encouraged in clinical practice to help individuals cope better and reduce diabetes-specific distress. The results also showed that diabetes-specific distress was negatively associated with HRQoL which was consistent with the study by Morisky et al. [19] who reported that lower health related quality of life was associated with a higher level of emotional distress and this association showed a statistically moderate significant correlation. Wang et al. [39] reported that diabetes distress had a statistically indirect effect on impact HRQoL ( = −0.024) in their SEM model. Measurement of diabetes-specific distress in diabetes health care can help increase awareness and help healthcare professionals provide better treatment for the patients.
Important therapies in the management of diabetes are an adjustment of diet, foot care, exercise and smoking quitting. Several studies have shown non-adherence to diet with a rate of 60–80% [37]. The non-adherence rate for foot care was around 20% in an Iranian study [1]. Exercise is another crucial part of diabetes management since it improves HbA1c levels, help reduce weight and decrease the occurrence of further complications. The non-adherence rate for exercise was 25% in India [22], 75% in Iran [1] and 67% in Hungary. However, daily activities are not considered as an exercise, though many patients report barriers to adhere to regular physical exercise. Thus, non-adhering T2DM patients might have a decrease level of HRQoL. In a German study [24], patients participating in a diabetes management program for T2DM showed better HRQoL when adhering to proper self-care activities. Furthermore, non-adherence parameters had a significant effect on HRQoL. Saleh et al. [28] reported that non-adhering patients to diabetes self-care activities generally had a lower HRQoL with a mean EQ-5D index of 0.55. The findings of the present study were consistent with past studies. It was also hypothesized that patients reporting better present AWI scores on ADDQoL would have a better HRQoL [9], [34].
The Structural Equation Modeling (SEM) methodology used in this study provides a comprehensive framework on how to develop a statistical model among multiple QoL constructs in T2DM patients. This study provides a theoretical framework of the relationships between MMAS and SDSCA with PAID, ADDQoL and SF-36. Hence, this study had enhanced the understanding of QoL issues among T2DM patients in several ways. This was the first study in Malaysia that extensively investigated the relationships among a number of physiological, psychological, behavioral predictors and adaptive outcomes using psychometrically validated instruments via SEM, thus showing practical applications of the SEM approach. Literature on diabetes studies had demonstrated that various factors can individually influence HRQoL, diabetes self-care activities, medication adherence, diabetes-dependent QoL and diabetes distress; however most of the previous models had not tested any integrated association between multiple variables. Therefore, findings from this study can be used as a potential starting point for examining multiple predictors and outcome variables in future diabetes QoL studies. This new evidence-based findings provides in-depth and important information to T2DM patients, doctors and relevant stakeholders in the healthcare management. The theoretical framework developed from this study can also be applied in a wide variety of other applications of SEM such as modeling the HRQoL of patients with hypertension using hypertension-specific and HRQoL instruments.
Conclusions
This study developed a structural model linking diabetes distress, medication adherence, self-care activities, diabetes-specific QoL and HRQoL of patients with T2DM. The Structural Equation Modeling (SEM) results showed that medication adherence is an important determinant of diabetes-specific distress. Patients should be advised and encouraged to have high medication adherence so that they would endure less distress and experience a better quality of life. Diabetes self-care activities should also be emphasised as it lowers diabetes distress and increases overall quality of life. As expected, a better diabetes-specific quality of life leads to better Health-Related Quality of Life. This study applies to other different chronic diseases and can be replicated to assess factors that may affect the health outcomes of the patients. It is recommended for clinicians to take an active role in guiding their patients to better medication adherence and self-care activities. Effective interventions by health care providers are important to encourage and help T2DM patients improve their quality of life while living and coping with this debilitating disease.
Acknowledgments
The authors would like to thank the Research Management Institute (RMI) of Universiti Teknologi MARA (UiTM), Malaysia, for funding this research under the RIF fund (600-RMI/DANA 5/3/RIF (218/2012). This study was also registered under the Medical Research and Ethics Committee, Malaysia (NMRR-13-640-15679). The authors would also like to thank Professor Dr. Joseph F. Hair, Kennesaw State University for his valuable comments on the structural equation model.
References
- 1.Aghamollaei T., Eftekhar H., Shojaeizadeh D., Mohammad K., Nakhjavani M., Pour F.G. Behavior, metabolic control and health-related quality of life in diabetic patients at bandar abbas diabetic clinic. Iran J Public Health. 2003;32(3):54–59. [Google Scholar]
- 2.Anderson B.J. Families and chronic illness research: targeting transitions and tools-Commentary on Trief et al. (2006) Families Syst Health. 2006;24(3):332–335. [Google Scholar]
- 3.Bentler P.M. Comparative Fit indexes in structural models. Psychol Bull. 1990;107(2):238–246. doi: 10.1037/0033-2909.107.2.238. [DOI] [PubMed] [Google Scholar]
- 4.Borrott N., Bush R. Measuring Quality of Life among those with type 2 diabetes in primary care. Australia 2008.
- 5.Bradley C., Speight J. Patient perceptions of diabetes and diabetes therapy: assessing quality of life. Diabetes/metabolism. Res Rev. 2002;18(Suppl 3):S64–9. doi: 10.1002/dmrr.279. (October 2001) [DOI] [PubMed] [Google Scholar]
- 6.Bradley C., Todd C., Gorton T., Symonds E., Martin a., Plowright R. The development of an individualized questionnaire measure of perceived impact of diabetes on quality of life: the ADDQoL. Qual Life Res. 1999;8(1–2):79–91. doi: 10.1023/a:1026485130100. [DOI] [PubMed] [Google Scholar]
- 7.Buhi E., Goodson P., Neilands T. Structural equation modeling: a primer for health behavior researchers. Am J Health Behav. 2007;31(1):74–85. doi: 10.5555/ajhb.2007.31.1.74. [DOI] [PubMed] [Google Scholar]
- 8.Chen T.-H., Li L., Kochen M.M. A systematic review: how to choose appropriate health-related quality of life (HRQOL) measures in routine general practice? J Zhejiang Univ Sci B. 2005;6(9):936–940. doi: 10.1631/jzus.2005.B0936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Delahanty L.M., Grant R.W., Wittenberg E., Bosch J.L., Wexler D.J., Cagliero E. Association of diabetes-related emotional distress with diabetes treatment in primary care patients with Type 2 diabetes. Diabet Med. 2007;24(1):48–54. doi: 10.1111/j.1464-5491.2007.02028.x. [DOI] [PubMed] [Google Scholar]
- 10.Eid M., Faridah A. Glycaemic control of Type 2 Diabetic patients on follow up at Hospital Universiti Sains Malaysia. Malaysian J Med Sci. 2003;10(2):40–49. [PMC free article] [PubMed] [Google Scholar]
- 11.El Achhab Y., Nejjari C., Chikri M., Lyoussi B. Disease-specific health-related quality of life instruments among adults diabetic: a systematic review. Diabetes Res Clin Pract. 2008;80(2):171–184. doi: 10.1016/j.diabres.2007.12.020. [DOI] [PubMed] [Google Scholar]
- 12.Gandek B., Ware J.E., Group P. Methods for validating and norming translations of health status questionnaires: the IQOLA project approach. J Clin Epidemiol. 1998;51(11):953–959. doi: 10.1016/s0895-4356(98)00086-9. [DOI] [PubMed] [Google Scholar]
- 13.Garratt A.M., Schmidt L., Fitzpatrick R. Patient-assessed health outcome measures for diabetes. Diabetes UK. 2002;19:1–11. doi: 10.1046/j.1464-5491.2002.00650.x. [DOI] [PubMed] [Google Scholar]
- 14.Guyatt G.H. The philosophy translation of health-related quality of life. Qual Life Res. 1993;2:461–465. doi: 10.1007/BF00422220. [DOI] [PubMed] [Google Scholar]
- 15.Herdman M., Fox-Rushby J., Badia X. A model of equivalence in the cultural adaptation of HRQoL instruments: the universalist approach. Qual Life Res. 1998;7(4):323–335. doi: 10.1023/a:1024985930536. [DOI] [PubMed] [Google Scholar]
- 16.Jermendy G., Erdesz D., Nagy L., Yin D., Phatak H., Karve S. Outcomes of adding second hypoglycemic drug after metformin monotherapy failure among type 2 diabetes in Hungary. Health Qual Life Outcomes. 2008;6(88):1–8. doi: 10.1186/1477-7525-6-88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Letchuman G.R., Nazaimoon W.M.W., Mohamad W.B.W., Chandran L.R., Tee G.H., Jamaiyah H. Prevalence of Diabetes in the Malaysian National Health Morbidity Survey III 2006 The Malaysian National Health Morbidity Survey III (NHMS) Med J Malaysia. 2010;65(3):173–179. [PubMed] [Google Scholar]
- 18.McNabb W.L. Adherence in diabetes: can we define it and can we measure it? Diabetes Care. 1997;20(2):215–218. doi: 10.2337/diacare.20.2.215. [DOI] [PubMed] [Google Scholar]
- 19.Morisky D.E., Ang A., Krousel-wood M. Predictive validity of a medication adherence measure in an outpatient setting. J Clin Hypertens. 2008;10(5):348–354. doi: 10.1111/j.1751-7176.2008.07572.x. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 20.Morisky D.E., Green L.W., Levine D. Concurrent and predictive validity of a self-reported measure of medication adherence. Med Care. 1986;24(1):67–74. doi: 10.1097/00005650-198601000-00007. [DOI] [PubMed] [Google Scholar]
- 21.Muller I., Grauw W.J., Gerwen W., Bartelink M., van den Hoogen H.J. Foot ulceration and lower limb amputation in Type 2 diabetic patients in dutch primary health care. Diabetes Care. 2001;25:570–574. doi: 10.2337/diacare.25.3.570. [DOI] [PubMed] [Google Scholar]
- 22.Mumu S.J., Saleh F., Ara F., Afnan F., Ali L. Non-adherence to life-style modification and its factors among type 2 diabetic patients. Indian J Public Health. 2014;58(1):40–44. doi: 10.4103/0019-557X.128165. [DOI] [PubMed] [Google Scholar]
- 23.Narayan K.M., Gregg E.W., Fagot-Campagna A., Engelgau M.M., Vinicor F. Diabetes–a common, growing, serious, costly, and potentially preventable public health problem. Diabetes Res Clin Pract. 2000;50(Suppl 2):S77–S84. doi: 10.1016/s0168-8227(00)00183-2. [DOI] [PubMed] [Google Scholar]
- 24.Ose D., Miksch A., Urban E., Natanzon I., Szecsenyi J., Kunz C.U. Health related quality of life and comorbidity. A descriptive analysis comparing EQ-5D dimensions of patients in the German disease management program for type 2 diabetes and patients in routine care. BMC Health Serv Res. 2011;11(1):179. doi: 10.1186/1472-6963-11-179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Özmen B., Boyvada S. The relationship between self-monitoring of blood glucose control and glycosylated haemoglobin in patients with type 2 diabetes with and without diabetic retinopathy. J Diabetes Complications. 2003;17(3):128–134. doi: 10.1016/s1056-8727(02)00200-3. [DOI] [PubMed] [Google Scholar]
- 26.Polonsky W.H., Anderson B.J., Lohrer P.a., Welch G., Jacobson a.M., Aponte J.E.. Assessment of diabetes-related distress. Diabetes Care. 1995;18(6):754–760. doi: 10.2337/diacare.18.6.754. [DOI] [PubMed] [Google Scholar]
- 27.Rubin R.R., Peyrot M. Quality of life and diabetes. Diabetes/Metab Res Rev. 1999;15(3):205–218. doi: 10.1002/(sici)1520-7560(199905/06)15:3<205::aid-dmrr29>3.0.co;2-o. [DOI] [PubMed] [Google Scholar]
- 28.Saleh F., Mumu S.J., Ara F., Hafez M.A., Ali L. Non-adherence to self-care practices & medication and health related quality of life among patients with type 2 diabetes: a cross-sectional study. BMC Public Health. 2014;14(1):431. doi: 10.1186/1471-2458-14-431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Shojaiefard A., Khorgami Z., Larijani B. Independent risk factors for amputation in diabetic foot. Int J Diabetes Dev Countries. 2008;28(2):32–37. doi: 10.4103/0973-3930.43096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Shrivastava S., Shrivastava P., Ramasamy J. Role of self-care in management of diabetes mellitus. J Diabetes Metabol Disord. 2013;12(1):14. doi: 10.1186/2251-6581-12-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Singh H., Bradley C. Assessing diabetes-specific knowledge in people with diabetes living in India. Diabet Med. 2006;23(Suppl 4):471. [Google Scholar]
- 32.Snoek FJ., Van der Ven NCW., Lubach C. Snoek et al. Diabetes Spectrum 1999; 12(3): 147.
- 33.Snoek F., Pouwer F., Welch W., Polonsky W. Diabetes-related emotional distress in. Diabetes Care. 2000;23(9):1305–1309. doi: 10.2337/diacare.23.9.1305. [DOI] [PubMed] [Google Scholar]
- 34.Soon S.S., Goh S.Y., Bee Y.M., Poon J.L., Li S.C., Thumboo J. Audit of diabetes-dependent quality of life (ADDQoL) [Chinese Version for Singapore ] questionnaire. Appl Health Econ Health Policy. 2010;8(4):239–249. doi: 10.2165/11313920-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 35.Speight J., Reaney M.D., Barnard K.D. Not all roads lead to Rome-a review of quality of life measurement in adults with diabetes. Diabetic Med J Br Diabetic Assoc. 2009;26(4):315–327. doi: 10.1111/j.1464-5491.2009.02682.x. [DOI] [PubMed] [Google Scholar]
- 36.Sundaram M., Kavookjian J., Patrick J.H., Miller L.-A., Madhavan S.S., Scott V.G. Quality of life, health status and clinical outcomes in Type 2 diabetes patients. Qual Life Res. 2007;16(2):165–177. doi: 10.1007/s11136-006-9105-0. [DOI] [PubMed] [Google Scholar]
- 37.Toobert D., Hampson S., Glasgow R.E. The summary of diabetes self-care. Diabetes Care. 2000;23(7):943–950. doi: 10.2337/diacare.23.7.943. [DOI] [PubMed] [Google Scholar]
- 38.Vincent D., McEwen M.M., Pasvogel A. The validity and reliability of a Spanish version of the summary of diabetes self-care activities questionnaire. Nurs Res. 2008;57(2):101–106. doi: 10.1097/01.NNR.0000313484.18670.ab. [DOI] [PubMed] [Google Scholar]
- 39.Wang R.-H., Wu L.-C., Hsu H.-Y. A path model of health-related quality of life in type 2 diabetic patients: a cross-sectional study in Taiwan. J Adv Nurs. 2011;67(12):2658–2667. doi: 10.1111/j.1365-2648.2011.05701.x. [DOI] [PubMed] [Google Scholar]
- 40.Ware J.E. SF-36 health survey update. Spine. 2000;25(24):3130–3139. doi: 10.1097/00007632-200012150-00008. [DOI] [PubMed] [Google Scholar]
- 41.Ware J.E., Kosinski M., Gandek B., Aaronson N.K. The factor structure of the SF-36 health survey in 10 countries : results from the IQOLA project. J Clin Epidemiol. 1998;51(11):1159–1165. doi: 10.1016/s0895-4356(98)00107-3. [DOI] [PubMed] [Google Scholar]
- 42.Watkins K., Connell C.M. Measurement of health-related QOL in diabetes mellitus. PharmacoEconomics. 2004;22(17):1109–1126. doi: 10.2165/00019053-200422170-00002. [DOI] [PubMed] [Google Scholar]
- 43.Wee H., Tan C., Goh S., Li S. Usefulness of the audit of (ADDQoL) questionnaire in patients with diabetes in a multi-ethnic asian country. Pharmacoeconomics. 2006;24(7):673–682. doi: 10.2165/00019053-200624070-00006. [DOI] [PubMed] [Google Scholar]
- 44.Welch G.W., Jacobson A.M., Polonsky W.H. The problem areas in diabetes scale. Diabetes Care. 1997;20(5):760–766. doi: 10.2337/diacare.20.5.760. [DOI] [PubMed] [Google Scholar]
- 45.Welch G., Weinger K., Anderson B., Polonsky W.H. Responsiveness of the Problem Areas In Diabetes (PAID) questionnaire. Diabetic Med J Br Diabetic Assoc. 2003;20(1):69–72. doi: 10.1046/j.1464-5491.2003.00832.x. [DOI] [PubMed] [Google Scholar]
- 46.Wild S., Roglic G., Green A., Richard S., King H. Estimates for the year 2000 and projections for 2030. World Health. 2004;27(5):1047–1053. doi: 10.2337/diacare.27.5.1047. [DOI] [PubMed] [Google Scholar]