Highlights
-
•
Interdisciplinary teams (IDTs) should aim to implement a patient-centred approach.
-
•
IDTs can enable improved glycaemic control and reduced cardiometabolic risk.
-
•
Successful IDTs require strong leadership, good communication and shared goals.
Keywords: Diabetes mellitus, Type 2, Interdisciplinary team, Glycaemic control, Multidisciplinary, Integrated care
Abstract
The Global Partnership for Effective Diabetes Management has previously recommended the implementation of an interdisciplinary team (IDT) approach to type 2 diabetes (T2DM) management as one of 10 practical steps for health care professionals to help more people achieve their glycaemic goal. This article discusses some of the key contributors to success and also the challenges faced when applying IDT care, by examining case studies and examples from around the world. The real-world practices discussed show that implementing successful interdisciplinary care in diabetes is possible despite significant barriers such as established hierarchal structures and financial resource constraints. Instituting collaborative, integrated working relationships among multiple disciplines under strong leadership, together with enhanced and active communication and improved patient access to appropriate specialties is essential. Patients have a crucial role in the management of their own disease and including them as part of the treatment team is also critical. IDTs in diabetes care improve patient outcomes in terms of control of glycaemia and cardiometabolic risk factors, and decreased risk of diabetes complications. Ensuring access to an appropriate IDT, in whatever form, is paramount to enable the best care to be delivered.
Introduction
In 2007, the Global Partnership for Effective Diabetes Management recommended the implementation of an interdisciplinary team (IDT) approach to type 2 diabetes (T2DM) management [1] as one of 10 practical steps for health care professionals (HCPs) to help more people achieve their glycaemic goal [2]. IDT approaches to diabetes care provision have previously been reported to provide the greatest positive impact on glycaemic control in people with T2DM [3]. In this article, the Global Partnership discusses some of the key contributors to success and also the challenges faced when implementing IDT care, by examining case studies and examples from around the world reflecting circumstances that have varying degrees of resource availability or other constraints.
Real-world experiences of IDTs in practice
Effective IDT models in the real-world setting offer examples of best practice and effective frameworks that can be applied to provide innovative solutions to the challenges of establishing team-based diabetes care. Examples of such frameworks from different locations and in environments with widely varying resources are outlined here to illustrate how IDT approaches can be established in practice, and highlight common themes that arise.
USA: An IDT approach in an integrated health care delivery system
The Ochsner Medical Center’s ‘Diabetes Empowerment Clinic’ is a pilot initiative aimed at improving patient access to specialist care at Ochsner Health System primary care clinics in South East Louisiana. This initiative creates clinical teams with shared goals that deliver parallel and coordinated management strategies in a patient-centred format. The predecessor to the Diabetes Empowerment Clinic was Boot Camp, which was conducted within the primary care department and involved a primary care trained nurse practitioner, endocrinology-certified diabetes educator (CDE) and a pharmacist. However, the scope of this programme was limited to a one-time intensive visit designed to initiate treatment, which was then followed-up by a primary care physician (PCP). The success of Boot Camp led to the creation of the Diabetes Empowerment Clinic where initial and 3 to 6-month follow-up care is provided by an integrated IDT comprised of a diabetes trained nurse practitioner, a CDE, endocrinologists and at times a pharmacist.
Patients are initially referred by a PCP for an assessment with a CDE who then triages them to the Diabetes Empowerment Clinic unless they met criteria to have their care assumed by a diabetes nurse practitioner in the Endocrinology Department. The criteria include type 1 diabetes (T1DM), T2DM with poor glycaemic control on multiple daily injection therapy or an insulin pump, patients requiring U 500 insulin, or urgent or marked hyperglycaemia. The Diabetes Empowerment Clinic provides patients with individualized diabetes education and a management plan delivered through an IDT, until the patient’s HbA1c improves to their individualized target (typically 2–3 visits). Participation in the Diabetes Empowerment Clinic also provides patients with the option of seeing, or obtaining referrals to, other Ochsner Medical Centre specialists. At the conclusion of the Diabetes Empowerment Clinic, patients are transitioned back to the care of their PCPs along with clear communication of their individual goals, results and barriers to care. Some patients, when deemed appropriate, will be referred to the Endocrinology Department for longer term diabetes care.
Exposure to Boot Camp resulted in a substantial reduction in HbA1c levels in patients with poorly-controlled diabetes (HbA1c declined from 11.02% to 8.24% [96.94 mmol/mol to 66.56 mmol/mol] for Boot Camp participants vs. 10.89% to 10.16% [95.53 mmol/mol–87.55 mmol/mol] for those not enrolled in Boot Camp). In the Diabetes Empowerment Clinic pilot of 124 patients completing the programme, the mean HbA1c at entry was 9.74% (82.96 mmol/mol; SD 1.92) and at completion the mean HbA1c was 6.75% (50.28 mmol/mol; SD 0.75). 94% of the patients that completed the programme met the Healthcare Effectiveness Data and Information Set (HEDIS) goal of HbA1c <8% (63.94 mmol/mol) and 68% achieved a HbA1c of <7% (53.01 mmol/mol). These initiatives, including the less complex Boot Camp, show that improved integrated care can provide real benefits for patients, including improved glycaemic control.
Hong Kong: Structured IDT approach implemented on a large scale in the public sector
Hong Kong has a heavily-subsidized health care system, with most chronic care provided in public hospitals and clinics. In 1995, the Chinese University of Hong Kong and Prince of Wales Hospital jointly initiated a quality improvement programme for diabetes care. This comprised a nurse-coordinated comprehensive assessment programme that used structured protocols to establish the Hong Kong Diabetes Registry, followed by group empowerment and IDT care.
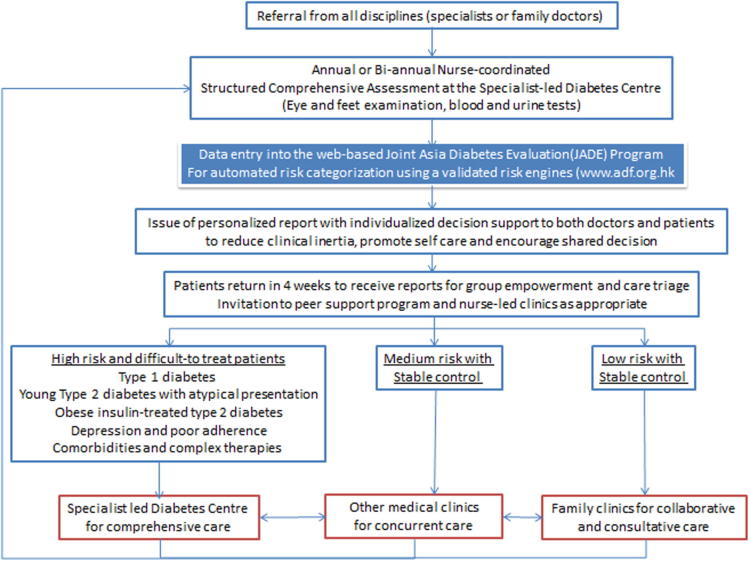
The implementation of this diabetes complications screening programme led to the creation of the diabetes nurse specialist role and hospital-based Diabetes Centres, which coordinate diabetes care and the empowerment programme. The documentation of risk factors, complications and clinical outcomes enabled the IDT to develop and validate a series of risk equations, and in 2007 the integrated care model was digitalized to form the web-based Joint Asia Diabetes Evaluation (JADE) Programme [4] (Fig. 1).
Fig. 1.
The integrated diabetes care model at the Chinese University of Hong Kong and Prince of Wales Hospital using the web-based Joint Asia Diabetes Evaluation (JADE) Programme. *The JADE Programme provided the premise for the implementation of the territory-wide Risk Assessment Management Progamme in diabetes mellitus (RAMP-DM) in the community-based clinics coordinated by nurse specialists and general practitioners.
In 2009, the model was adapted and widely implemented to become the Multidisciplinary Risk Assessment and Management programme for people with diabetes mellitus (‘RAMP-DM’). This programme, which operates in public general out-patient clinics (GOPCs) in Hong Kong, involves patients undergoing a comprehensive risk assessment by a specialist nurse, followed by risk stratification and education provided by an IDT [5]. Low-risk patients continue with the usual follow-up provided by the GOPC, medium-risk patients are given additional intervention by an advanced practice nurse (APN), and high-risk/very high risk patients are given additional intervention by an APN and an associate consultant, who is a specialist family physician [5].
At 12 months into the programme, a random sample of 1248 people with T2DM enrolled to RAMP-DM was selected and 1248 people with diabetes under usual primary care were matched by age, sex, and HbA1c level at baseline [6]. Compared with the usual care group, the RAMP-DM group with risk-stratification and IDT had a lower incidence of cardiovascular events (1.21% vs. 2.89%, p = 0.003), and a net decrease in HbA1c (−0.20%, p < 0.01), systolic blood pressure (−3.62 mmHg, p < 0.01) and 10-year estimated risks of cardiovascular disease (CVD) (total CVD risk, −2.06%, p < 0.01; coronary heart disease risk, −1.43%, p < 0.01; and stroke risk, −0.71%, p < 0.01) [6]. A significant increase in the proportion of patients reaching treatment targets of HbA1c and blood pressure was also observed in the RAMP-DM group [6]. In a subsequent 3-year analysis, the RAMP-DM group had lower incidences of individual and total cardiovascular complications, as well as all-cause mortality, compared with the usual care group [7].
RAMP-DM is an example of a programme run on a large scale in a public sector where variations between clinics occur. Its success lies in ensuring that clinics maintain the core operation framework with minimal modifications to the protocol [5]. Frequent site visits to the clinics by the governing body also enables issues to be identified and addressed appropriately [5].
UK: The role of primary care in an integrated diabetes management model
A model implemented in the UK transitions people with less complex diabetes to primary care while specialists manage the treatment of six categories of patients termed the ‘super six’ – patients on insulin pumps, those with antenatal diabetes, patients requiring diabetic foot care or with low estimated glomerular filtration rate who need dialysis, patients with uncontrolled T1DM/adolescent diabetes, and people with diabetes who are inpatients [8]. However, some aspects of diabetes care still require cooperation between specialists and PCPs [8], and as a result a collaborative relationship was established whereby specialists and PCPs maintained regular communication. Specialists also undertook annual/biannual visits to the primary care clinic to discuss complex cases with their primary care colleagues.
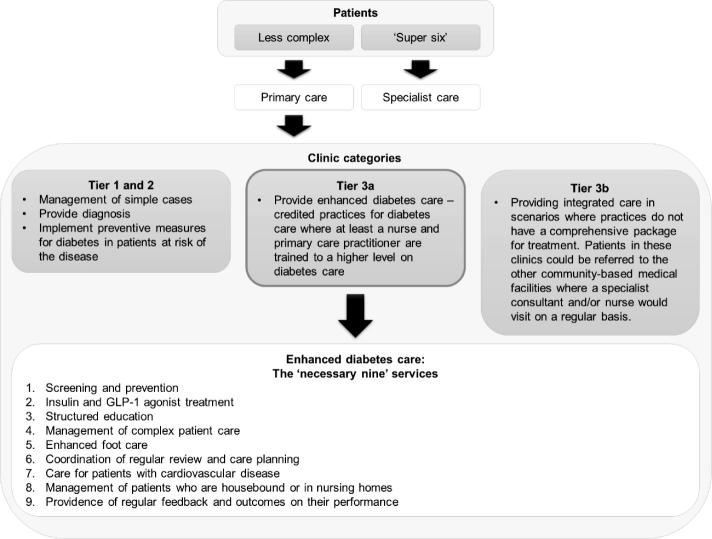
In the city of Leicester, this model was expanded further within the primary care setting by dividing clinics into different tiers to provide enhanced services where applicable (Fig. 2). A patient education programme (DESMOND, Diabetes Education and Self-Management for Ongoing and Newly Diagnosed) was incorporated in clinics within Tiers 1 and 2, while Tiers 3a and 3b were underpinned by more integrated care with additional team members or services. Tier 3a clinics provide the ‘necessary nine’ services (Fig. 2), which enabled them to manage even more complex patients. To date, this system has proven to be cost-effective, with no increase in the death rate or hospitalizations.
Fig. 2.
The ‘Leicester model’ – primary care clinic categories. ‘Super six’ – patients on insulin pumps, those with antenatal diabetes, patients requiring diabetic foot care or with low estimated glomerular filtration rate who need dialysis, patients with uncontrolled type 1 diabetes/adolescent diabetes, and people with diabetes who are inpatients [9].
Mexico: IDT diabetes care in a resource-poor environment
With ∼75% of people with diabetes living in low- and middle income countries [8], there is a pressing need for innovative cost-effective methods to enable the best possible diabetes care. In Mexico, government health centres are overcrowded and limited to non-specialist care, while private care is expensive with fragmented access to services. The Clínicas del Azúcar was created to provide a community-based medical service for diabetes patients, facilitated by an IDT composed of physicians, nurse practitioners, dietitians, psychologists, physical trainers, sociologists and laboratory technicians.
The critical aspect of Clínicas del Azúcar was providing access to specialized diabetes care for large numbers of people regardless of an individual’s economic status. This was achieved through offering a single fixed-fee annual payment (approximately US $250) that provided coverage for unlimited medical consultation, nutritional management, counseling, diabetes education, physical activity counseling, laboratory tests, and screening/examinations for detection of chronic complications. Through the work of the clinics, treatment outcomes have improved, and significant reductions in costs have been achieved.
The impact of an IDT in T2DM
The IDT approach can be effective in delivering care to people who have chronic conditions, such as T2DM, that require both self-management and major lifestyle alterations. In the case of T2DM, the complexity of the disease and its associated multiple comorbidities also raises particular diverse challenges that individual clinicians may find difficult to manage. Integrated team-based care has been associated with improved glycaemic control and reduced HbA1c levels in people with diabetes [10], [11], [12], [13], [14]. For example, a 6-month, randomized, controlled trial of individuals with poorly controlled diabetes showed that a management programme delivered by a nurse-led IDT (including a diabetes nurse educator, psychologist, pharmacist and nutritionist) significantly reduced HbA1c levels compared with usual diabetes care provided by PCPs (−1.3% vs. −0.2%, respectively, p < 0.0001) [14].
An IDT approach also has further benefits in terms of blood pressure [10], [15] and lipid level reductions [10], as well as improvements in quality of life [12], [13]. In addition, IDT care involving a variety of HCPs, such as nurses, podiatrists and endocrinologists, has been shown to reduce the risk of amputation at the lower extremity by 34–47% [16], [17], [18], [19]. Furthermore, IDT care is associated with a significantly reduced risk of end-stage renal disease in patients with T2DM nephropathy [20], [21], and significantly reduces the risk of mortality compared with non-integrated care [22].
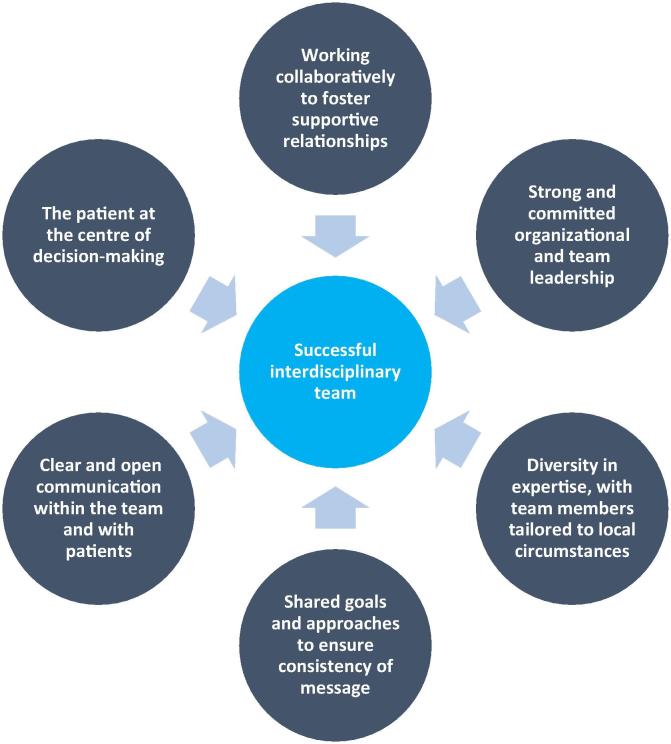
Key contributors to an effective IDT
Although the IDT approach has gained presence globally in T2DM management, the factors that contribute to its effective implementation are not widely understood, and differ depending on available resources and local working practices. There are, however, some key contributors to establishing a successful IDT approach to diabetes care delivery, which are outlined here (Fig. 3).
Fig. 3.
Key contributors to a successful IDT in diabetes care.
A key function of an IDT is providing continuous, accessible, consistent and effective care focused on an individual patient’s needs and goals. Within the team itself, a fundamental principle of an IDT is equality and interdependence between team members [1]. In particular, the focus is on how various specialists in the team function together in an integrated manner (interdisciplinary) rather than alongside each other (multidisciplinary), and how flexibility is needed with respect to professional boundaries [1]. It is critical to identify shared core roles and responsibilities while differentiating these from the unique contribution of each specialty. Working as a team requires members to be willing and committed to working collaboratively to create an environment that fosters trust and cultivates supportive relationships. A work setting that encourages mentoring, and ensures achievements and contributions are recognized further facilitates a successful partnership between team members.
A strong and supportive organizational leadership is required that is committed to the IDT approach [23]. This is also necessary at a team level, in which leadership, whether by physicians, pharmacists or specialist nurses, has been recognized as an essential element in successful IDT delivery [24]. Individuals who are leading the team should be clear on when and how to be a team player. Creativity and adaptability within the team should be encouraged given that an IDT approach can vary depending on factors such as number of patients involved and resource constraints. It is also important that all members of the team have a voice, no matter how junior or inexperienced. While seniority should be respected, junior members of staff often have innovative and creative ideas that deserve to be heard. In this way, inclusivity within the team is encouraged and job satisfaction improved.
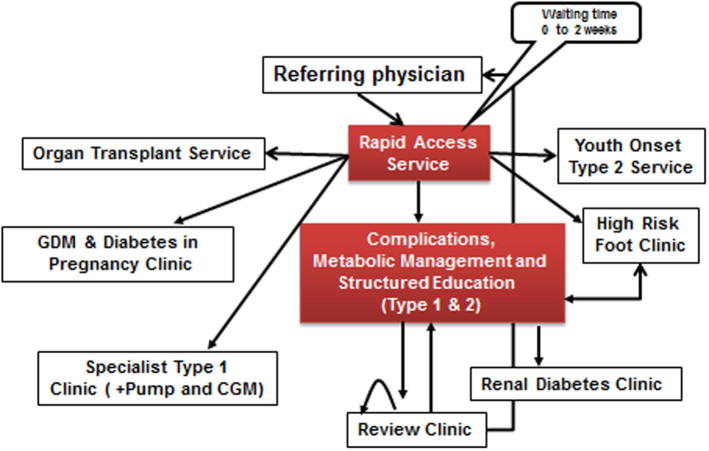
A diverse team of HCPs with complementary expertise is consistently recommended across IDT practical guidelines [1], [23] and such an approach can be seen in practice (see Fig. 4 for an example of an inter-disciplinary diabetes centre at Royal Prince Alfred Hospital, Sydney, Australia). The Global Partnership has previously suggested team composition should be tailored to local needs, available resources and clinical setting [1], [23], and also suggests that a ‘team’ can be composed of an individual patient and a HCP as long as best practice principles are applied.
Fig. 4.
Royal Prince Alfred Hospital: an inter-disciplinary diabetes centre∗ (education is integrated with clinical service and care is shared with primary care.). *Established in 1985. CGM, continuous glucose monitoring; GDM, gestational diabetes mellitus.
Having a shared goal and approach within the IDT is critical [1], [23] and such alignment within the team facilitates the delivery of clear and consistent messages to people with diabetes. This also contributes to the process of developing coordinated management plans that have the patient as the focus of decision-making [1], [25]. Part of ensuring adequate implementation of shared approaches is clear and open communication [1]. Embedding communication strategies into the team’s routine helps to create the framework and opportunity for effective and timely team interactions [23]. For example, regular and structured review meetings designed to develop an agreed approach, and daily team case conferences where patient’s medical records are reviewed.
As with all health care providers, continued professional training is essential for all IDT members who should possess at least a competent level of knowledge of diabetes and diabetes therapies, and keep up-to-date with advances in the field that might affect day-to-day patient management. The ability to impart knowledge of diabetes and its complications, and inform patients of how best to self-manage is a fundamental function of a diabetes IDT. Moreover, team members with different skill sets tend to educate and inform each other, which leads to a broader understanding of diabetes management that can further enhance patient care.
Given the pluralistic needs of an individual with T2DM – and that those needs vary during the clinical course of a few decades – a structured, coordinated and integrated care programme will help to ensure that the appropriate treatment (e.g. specialist, primary, paramedical care) or intervention (e.g. education, peer support) is provided at the right time and in the correct setting [4]. In areas with limited resources or capacity, diabetologists are often required to take on the combined role of being a manager, a mentor and a monitor to enable their expertise to benefit patients through other team members.
A further consideration is the silent nature of many diabetes risk factors and complications. Most professional bodies recommend regular comprehensive assessment to enable early detection and personalized intervention (taking risks and benefits into consideration) [26], [27]. Using protocols and through task delegation, effective implementation of comprehensive assessment programmes, followed by data management for risk stratification and care triage, is one possible way to deliver personalized care effectively and efficiently with quality assurance [28], [29]. In the chronic care model, documentation is a fundamental aspect of care provision; in the absence of patient records being kept or maintained, continuity of care becomes almost impossible.
The challenges
Implementation of an IDT approach is not without its challenges, and due to the increasing prevalence of T2DM, new models of care need to be analyzed and tested [30], [31]. With equality and interdependence as a key principle, the traditional hierarchal structure that exists in many institutions can act as a barrier to effective IDT care. Other major challenges include a lack of resources to establish an IDT, inadequate access to appropriate specialties, time-poor working environments, and poor communication within the team and with patients [25], [32]. Organizational factors, such as individual work schedules, can prevent regular communication among team members [25], resulting in misalignment of treatment goals and poorer patient outcomes [25].
In many countries/areas, acute hospital and episodic primary care are the traditional modes of care delivery. However, for people with diabetes who need education, empowerment and engagement to understand the nature of the disease and the ‘what, why and how’ of diabetes self-management, changes of setting and workflow are required to enable trustworthy relationships to develop between the patient and the IDT. The establishment of centres to facilitate IDT care can often achieve these aims and is also highly conducive to team-building, which promotes mutual learning and quality improvement.
Conclusions
The real-world examples outlined here show that implementing successful interdisciplinary care in diabetes is possible despite significant barriers. Overcoming an established hierarchal structure is challenging and financial resource constraints are perhaps one of the greatest impediments to the delivery of adequate IDT care. Moreover, establishing collaborative, integrated working relationships among multiple disciplines under the direction of strong leadership (including enhanced and active communication) and improving patient access to appropriate specialties is essential. The role of patients in their own disease management is crucial and it is therefore critical to include them as part of the treatment team to enable regular communication and share management goals.
As shown, IDTs in diabetes care contribute to improvements in treatment outcomes for patients and ensuring access to an appropriate IDT, in whatever form, is paramount. Putting in place the key contributors to an effective IDT within a framework that suits regional or country-specific circumstances, as highlighted by the examples provided here, allows the best care to be delivered to people with diabetes.
Funding
The literature search was supported by an unrestricted educational grant from AstraZeneca.
Contribution statements
All authors contributed to the conception and design of the paper and were involved in the drafting and/or revision of the article and had final approval of the version to be published.
Conflicts of interest
The authors Margaret McGill, Lawrence Blonde, Kamlesh Khunti, Juliana CN Chan and Clifford J Bailey are members of the Global Partnership for Effective Diabetes Management, an independent multidisciplinary task force with no conflicts of interest to report. Fernando J Lavalle also has no conflicts of interest to report.
Acknowledgement
The authors would like to thank Duncan Pennington of International Medical Press for editorial assistance with drafting and revision of the manuscript.
References
- 1.McGill M., Felton A.M. New global recommendations: a multidisciplinary approach to improving outcomes in diabetes. Prim Care Diabetes. 2007;1:49–55. doi: 10.1016/j.pcd.2006.07.004. [DOI] [PubMed] [Google Scholar]
- 2.Bailey C.J., Aschner P., Del Prato S., LaSalle J., Ji L., Matthaei S. Global Partnership for Effective Diabetes Management. Individualized glycaemic targets and pharmacotherapy in type 2 diabetes. Diab Vasc Dis Res. 2013;10:397–409. doi: 10.1177/1479164113490765. [DOI] [PubMed] [Google Scholar]
- 3.Shojania K.G., Ranji S.R., McDonald K.M., Grimshaw J.M., Sundaram V., Rushakoff R.J. Effects of quality improvement strategies for type 2 diabetes on glycaemic control: a meta-regression analysis. JAMA. 2006;296:427–440. doi: 10.1001/jama.296.4.427. [DOI] [PubMed] [Google Scholar]
- 4.Chan J.C., Sui Y., Oldenburg B., Zhang Y., Chung H.H., Goggins W. Effects of telephone-based peer support in patients with type 2 diabetes mellitus receiving integrated care: a randomized clinical trial. JAMA Intern Med. 2014;174:972–981. doi: 10.1001/jamainternmed.2014.655. [DOI] [PubMed] [Google Scholar]
- 5.Fung C.S., Chin W.Y., Dai D.S., Kwok R.L., Tsui E.L., Wan Y.F. Evaluation of the quality of care of a multi-disciplinary risk factor assessment and management programme (RAMP) for diabetic patients. BMC Fam Pract. 2012;13:116. doi: 10.1186/1471-2296-13-116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Jiao F.F., Fung C.S., Wong C.K., Wan Y.F., Dai D., Kwok R. Effects of the Multidisciplinary Risk Assessment and Management Program for Patients with Diabetes Mellitus (RAMP-DM) on biomedical outcomes, observed cardiovascular events and cardiovascular risks in primary care: a longitudinal comparative study. Cardiovasc Diabetol. 2014;13:127. doi: 10.1186/s12933-014-0127-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Jiao F., Fung C.S., Wan Y.F., McGhee S.M., Wong C.K., Dai D. Long-term effects of the multidisciplinary risk assessment and management program for patients with diabetes mellitus (RAMP-DM): a population-based cohort study. Cardiovasc Diabetol. 2015;14:105. doi: 10.1186/s12933-015-0267-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kar P. The ‘super six’ for the acute trust; all else under primary care? Pract Diab. 2011;28:308–309. [Google Scholar]
- 9.International Diabetes Federation. IDF Diabetes Atlas – Seventh Edition. <http://www.diabetesatlas.org/> [Last accessed March 2016].
- 10.Bright D.R., Kroustos K.R., Thompson R.E., Swanson S.C., Terrell S.L., Dipietro N.A. Preliminary results from a multidisciplinary university-based disease state management program focused on hypertension, hyperlipidemia, and diabetes. J Pharm Pract. 2012;25:130–135. doi: 10.1177/0897190011420725. [DOI] [PubMed] [Google Scholar]
- 11.Pimazoni-Netto A., Rodbard D., Zanella M.T. Rapid improvement of glycemic control in type 2 diabetes using weekly intensive multifactorial interventions: structured glucose monitoring, patient education, and adjustment of therapy – a randomized controlled trial. Diabetes Technol Ther. 2011;13:997–1004. doi: 10.1089/dia.2011.0054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Rasekaba T.M., Graco M., Risteski C., Jasper A., Berlowitz D.J., Hawthorne G. Impact of a diabetes disease management program on diabetes control and patient quality of life. Popul Health Manag. 2012;15:12–19. doi: 10.1089/pop.2011.0002. [DOI] [PubMed] [Google Scholar]
- 13.Codispoti C., Douglas M.R., McCallister T., Zuniga A. The use of a multidisciplinary team care approach to improve glycemic control and quality of life by the prevention of complications among diabetic patients. J Okla State Med Assoc. 2004;97:201–204. [PubMed] [Google Scholar]
- 14.Sadur C.N., Moline N., Costa M., Michalik D., Mendlowitz D., Roller S. Diabetes management in a health maintenance organization. Efficacy of care management using cluster visits. Diabetes Care. 1999;22:2011–2017. doi: 10.2337/diacare.22.12.2011. [DOI] [PubMed] [Google Scholar]
- 15.Choe H.M., Bernstein S.J., Cooke D., Stutz D., Standiford C. Using a multidisciplinary team and clinical redesign to improve blood pressure control in patients with diabetes. Qual Manage Health Care. 2008;17:227–233. doi: 10.1097/01.QMH.0000326727.01203.99. [DOI] [PubMed] [Google Scholar]
- 16.Aydin K., Isildak M., Karakaya J., Gürlek A. Change in amputation predictors in diabetic foot disease: effect of multidisciplinary approach. Endocrine. 2010;38:87–92. doi: 10.1007/s12020-010-9355-z. [DOI] [PubMed] [Google Scholar]
- 17.Rubio J., Aragon-Sanchez J., Jimenez S., Guadalix G., Albarracín A., Salido C. Reducing major lower extremity amputations after the introduction of a multidisciplinary team for the diabetic foot. Int J Low Extremity Wounds. 2014;13:22–26. doi: 10.1177/1534734614521234. [DOI] [PubMed] [Google Scholar]
- 18.Yesil S., Akinci B., Bayraktar F., Havitcioglu H., Karabay O., Yapar N. Reduction of major amputations after starting a multidisciplinary diabetic foot care team: single centre experience from Turkey. Exp Clin Endocrinol Diabetes. 2009;117:345–349. doi: 10.1055/s-0028-1112149. [DOI] [PubMed] [Google Scholar]
- 19.Martinez-Gomez D.A., Moreno-Carrillo M.A., Campillo-Soto A., Carrillo-García A., Aguayo-Albasini J.L. Reduction in diabetic amputations over 15 years in a defined Spain population. Benefits of a critical pathway approach and multidisciplinary team work. Rev Esp Quimioter. 2014;27:170–179. [PubMed] [Google Scholar]
- 20.Leung W.Y., So W.Y., Tong P.C., Chan N.N., Chan J.C. Effects of structured care by a pharmacist-diabetes specialist team in patients with type 2 diabetic nephropathy. Am J Med. 2005;118:1414. doi: 10.1016/j.amjmed.2005.07.050. [DOI] [PubMed] [Google Scholar]
- 21.Chan J.C., So W.Y., Yeung C.Y., Ko G.T., Lau I.T., Tsang M.W. Effects of structured versus usual care on renal endpoint in type 2 diabetes: the SURE study: a randomized multicenter translational study. Diabetes Care. 2009;32:977–982. doi: 10.2337/dc08-1908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.So W.Y., Tong P.C., Ko G.T., Leung W.Y., Chow C.C., Yeung V.T. Effects of protocol-driven care versus usual outpatient clinic care on survival rates in patients with type 2 diabetes. Am J Manage Care. 2003;9:606–615. [PubMed] [Google Scholar]
- 23.National Diabetes Education Program. Redesigning the health care team: diabetes prevention and lifelong management. <http://ndep.nih.gov/media/NDEP37_RedesignTeamCare_4c_508.pdf?redirect=true> [accessed March 2016].
- 24.Warrington L., Ayers P., Baldwin A.M., Wallace V., Riche K.D., Saulters R. Implementation of a pharmacist-led, multidisciplinary diabetes management team. Am J Health Syst Pharm. 2012;69:1240–1245. doi: 10.2146/ajhp110297. [DOI] [PubMed] [Google Scholar]
- 25.Ritholz M.D., Beverly E.A., Abrahamson M.J., Brooks K.M., Hultgren B.A., Weinger K. Physicians’ perceptions of the type 2 diabetes multi-disciplinary treatment team: a qualitative study. Diabetes Educ. 2011;37:794–800. doi: 10.1177/0145721711423320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Inzucchi S.E., Bergenstal R.M., Buse J.B., Diamant M., Ferrannini E., Nauck M. Management of hyperglycemia in type 2 diabetes: a patient-centered approach: Position statement of the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD) Diabetes Care. 2012;35:1364–1379. doi: 10.2337/dc12-0413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Raz I., Riddle M.C., Rosenstock J., Buse J.B., Inzucchi S.E., Home P.D. Personalized management of hyperglycemia in type 2 diabetes: reflections from a diabetes care editors’ expert forum. Diabetes Care. 2013;36:1779–1788. doi: 10.2337/dc13-0512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Chan J.C., Ozaki R., Luk A., Kong A.P., Ma R.C., Chow F.C. Delivery of integrated diabetes care using logistics and information technology – the Joint Asia Diabetes Evaluation (JADE) program. Diabetes Res Clin Pract. 2014;106(Suppl. 2):S295–S304. doi: 10.1016/S0168-8227(14)70733-8. [DOI] [PubMed] [Google Scholar]
- 29.Tricco A.C., Ivers N.M., Grimshaw J.M., Moher D., Turner L., Galipeau J. Effectiveness of quality improvement strategies on the management of diabetes: a systematic review and meta-analysis. Lancet. 2012;379:2252–2261. doi: 10.1016/S0140-6736(12)60480-2. [DOI] [PubMed] [Google Scholar]
- 30.Wilson A., O'Hare J.P., Hardy A., Raymond N., Szczepura A., Crossman R. Evaluation of the clinical and cost effectiveness of intermediate care clinics for diabetes (ICCD): a multicentre cluster randomised controlled trial. PLoS ONE. 2014;9:e93964. doi: 10.1371/journal.pone.0093964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Seidu S., Walker N.S., Bodicoat D.H., Davies M.J., Khunti K. A systematic review of interventions targeting primary care or community based professionals on cardio-metabolic risk factor control in people with diabetes. Diabetes Res Clin Pract. 2016;113:1–13. doi: 10.1016/j.diabres.2016.01.022. [DOI] [PubMed] [Google Scholar]
- 32.Cuddihy R.M., Philis-Tsimikas A., Nazeri A. Type 2 diabetes care and insulin intensification: is a more multidisciplinary approach needed? Results from the MODIFY survey. Diabetes Educ. 2011;37:111–123. doi: 10.1177/0145721710388426. [DOI] [PubMed] [Google Scholar]