Highlights
-
•
Nurse-led models of initiating injectable therapy in primary care are successful.
-
•
Education to GPs and nurses can assist initiation of injectable therapy.
-
•
Nurse-led patient group education can support initiating injectable therapy.
Keywords: Injectable therapy, Type two diabetes, Insulin initiation, Nurse-led models of care, Primary care
Abstract
Aims
To systematically identify and describe models of injectable therapy initiation for people with type 2 diabetes mellitus (T2DM) in primary care.
Methods
Eight electronic databases and the grey literature were searched. Studies examining models of injectable therapy initiation for adults with T2DM in primary care settings were included.
Results
Successful models included: 1) Nurse-led one-to-one approach; 2) Nurse-led group sessions; and 3) Providing education to GPs and nurses.
Conclusions
Few robust studies were found. Studied models were mainly in general practices, with limited evidence documented about starting people with T2DM on an injectable in the home setting.
Introduction
Type 2 diabetes mellitus (T2DM) affects approximately one million Australians [18] and 422 million people worldwide [33]. Sub-optimal glycaemic management is associated with an increased risk of developing diabetes-related complications and increased longer-term health costs. Across the population of people with type 2 diabetes, a 1% reduction in HbA1c over a five year period would result in reductions in the cumulative incidence of end-stage kidney disease by 40%, in amputations by 20%, in advanced eye disease by 42% and in myocardial infarction by 15% [29]. Optimal glycaemic management, that is established early and maintained throughout the disease duration, is essential for delaying and preventing long-term complications [7], [23], [36], [28].
Insulin is effective in optimising glycaemic levels, and the timely use of insulin for treatment of people with T2DM is clearly supported by American and European guidelines [21]. Despite this, the initiation of insulin is often delayed due to various client, General Practitioner (GP), or system level barriers. Patient barriers can include a fear of injections, negative perceptions of insulin, social stigma, lifestyle adaptations, restrictions required by insulin use and the fear of side effects and complications from use [14], [4]. GP barriers can include a physician’s lack of familiarity with insulin, time constraints, a lack of confidence in initiation, lack of resources (including having practice nurses), and clinical inertia [26], [30], [25], amongst others. Barriers associated with the health system have been infrequently reported, but are also important and have been shown to contribute to the delay in insulin initiation in primary care [2].
In Australia, almost two-thirds of all people with T2DM have their insulin therapy initiated by a specialist rather than in primary care; with GPs initiating an injectable therapy for less than 20% of cases [3]. This is despite the 2016–2018 “General practice management of type 2 diabetes” clinical practice guidelines [37] providing clear protocols for the initiation and titration of injectable therapies in the primary care setting. Insulin initiation by specialists is also common in international settings. For example it has been shown that Diabetes Specialist Nurses (DSNs) mostly in secondary care, rather than practice nurses in primary care, initiate injectable therapy [6]. This can lead to delays in insulin initiation due to limited availability of specialist resources. A move to manage people with T2DM in primary care rather than secondary care has the potential to result in increases in insulin commencement [6], reductions in the use of more costly secondary care [12], and positive impacts on long-term outcomes for people with T2DM if it meant that insulin was started earlier [15].
For insulin initiation and titration to become successfully adopted in primary care (including general practice, community settings and domiciliary settings), there is a need for making changes in service delivery to improve diabetes management. In particular, a model of care is required that is feasible, practical and sustainable in practice. This systematic review aims to identify and assess current models of initiating injectable therapy for people with T2DM in primary care that are present in the literature. In doing so, the characteristics of these models and successful attributes can be described and reported on. Through this, an understanding of current practices for initiating injectable therapy in primary care can be gained, whether these practices are working, and whether any gaps in knowledge need to be addressed.
Method
Search strategy
A comprehensive search of the literature was conducted and included the retrieval of electronic documents and hand searching of reference lists for relevant articles. The databases that were searched included Medline, CINAHL, ProQuest, PubMed, Web of Science, and Cochrane Central register of Controlled Trials (CENTRAL). The key words used were: insulin initiation, diabetes injectable therapy initiation, insulin stabilisation, insulin titration, insulin administration and dosage, and injections subcutaneous. Searches were limited from 2000 to 2016, to capture the recent literature relevant to current clinical practice. The first author screened and assessed all titles and abstracts for inclusion, while the second author also assessed the identified articles. Any discrepancies in assessment were resolved through discussion with all authors. The reference lists of included studies were also searched for additional articles.
Inclusion criteria
For the study selection criteria, the review was restricted to English-language studies focusing on adults with T2DM, aged 18 years and older, for whom injectable therapy for T2DM (i.e. insulins or GLP-1 mimetics/agonists) had been recommended. The review included randomised-controlled trials (RCT), quasi-RCT, uncontrolled evaluations, cross-sectional studies and qualitative research in order to gain a more complete picture of the models of injectable initiation being used. Papers excluded from the review were: studies focusing on secondary care, abstracts alone, articles that lacked sufficient information about study design, methods of analysis and findings to be able to provide adequate assessment, conceptual/methodological or advocacy papers and review articles.
Data extraction and risk of bias
Two reviewers worked independently to extract data relevant to the review and assess the risk of bias of the studies. Data extraction forms were developed prior to the review. Information on the study purpose, setting, method, participants, sample size and main findings were extracted. Any discrepancies on data extraction and assessment of risk of bias were resolved via discussion. Two checklists developed by Kmet et al. [24] were used to assess the risk of bias for both quantitative (observational studies, cross sectional, and descriptive) and qualitative articles included in the review. These checklists addressed a range of characteristics, including study design, measures, methodology, analysis, and reporting. The risk of bias for randomised control trials (RCTs) was assessed using the Cochrane Collaboration Criteria [5].
Data synthesis and analysis
Given the heterogeneity of the studies included, and as the systematic review aimed to identify and describe current models of initiating injectable therapy for people with T2DM, the data synthesis is largely descriptive. The findings are presented according to the strategies identified for initiating injectable therapy for people with T2DM.
Results
Search results
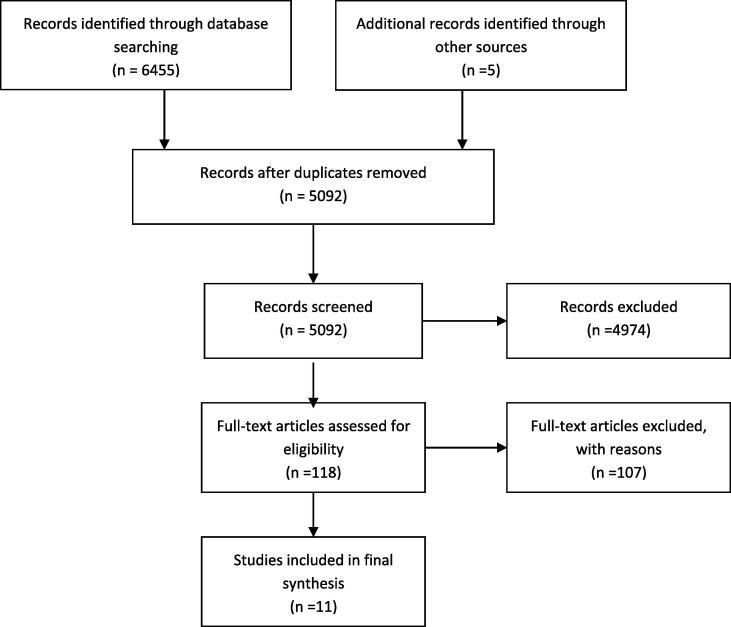
An initial search strategy retrieved 6455 articles which fitted the inclusion criteria. After eliminating duplicates and screening titles for relevance, 118 abstracts remained for assessment. Of the 118 abstracts reviewed, 10 met all of the eligibility criteria for the systematic review. Fig. 1 shows the selection and reviewing process in greater detail.
Fig. 1.
Flow diagram showing the process of study selection to be included in the review.
A total of 10 articles were included in this review, of which 9 were quantitative studies and one was a qualitative study. Table 1 displays the study summaries and methodology quality.
Table 1.
Study summaries and methodology quality.
| Author | Purpose | Setting | Method | Participants | Sample size (response rate) | Outcome measures | Main findings |
|---|---|---|---|---|---|---|---|
| Blackberry et al. [2] (1) | To evaluate the impact of a new model of care for insulin initiation in primary care, that features GPs and PNs working in an expanded role with CDE-RN support | General practices, Victoria, Australia | RCT | Patients with T2DM | 92 (50%) | SF-36v2 ADDQoL User Evaluation survey HbA1c levels |
|
| Coates et al. [6] (2) | To describe insulin initiation practices across the United Kingdom (UK) and identify factors influencing current practice |
National register of diabetes care staff and general practices, UK | Cross-sectional | DSNs and PNs | 1245 DSNs and PNs (37.7%) | Survey collecting data on job title, industry (primary or secondary care), starting individuals on insulin, insulin regimens, insulin products, devices used in insulin administration, starting dose, experience, qualifications |
|
| Dale et al. [9] (3) | To evaluate the impact of the initiation of insulin on glycaemic control and weight gain in patients with poorly controlled T2DM, registered with practices that volunteered to participate in an insulin initiation training programme | General Practices, UK | Longitudinal observational | Healthcare professionals (HCPs) | 94 HCPs (71.2%) and data on 835 patients | - Eight time points of data on HbA1c, weight, insulin regime, oral hypoglycaemic therapy. - Details on adverse events |
|
| Downey [13] (4) | To describe how practices successfully adapted a module to help people with T2DM to start insulin therapy and provide educational workshops for their staff | General Practices, UK | Cross-sectional evaluation | HCPs | 20 (95%) | Survey rating satisfaction with the course | The educational model was perceived well and there was demand for the course |
| Furler et al. [17] (5) | To develop a model of care for insulin initiation to be part of routine diabetes care in Australian general practice. To evaluate the model for feasibility of integration within routine general practice care |
General practices, Victoria, Australia | Qualitative evaluation | GPS, PNs and patients with T2DM | 24 HCPS and patients (response rate not applicable) | Exploring how GPs and PNs participated and engaged with a new model of care for initiating injectable therapy |
|
| Greenslade et al. [15] (6) | To describe a hybrid educational model for commencing insulin and to describe patient characteristics and metabolic changes before and during the first year on insulin for a group of 50 patients undertaking the educational program | Referrals from primary and secondary care, New Zealand | Longitudinal observational | Patients with T2 DM | 24 (49%) | Weight, BMI, HbA1c measured at three, six and 12 months |
|
| Harris et al. [20] (7) | To determine the effectiveness of an insulin initiation strategy utilising diabetes specialist and community retail pharmacy support to increase family physician insulin prescribing rates |
Family physician clinics and community pharmacies across Canada | RCT | Family physicians, community pharmacists, people with T2DM | 151 physicians (11%) response rate), 107 community pharmacists (no response rate provided), 11380 patient data (49.6%) | Physician’s insulin prescribing rate, the number of insulin starts per 12-month intervention of insulin-eligible patients, HbA1c, fasting plasma glucose, OAD prescription and score, insulin prescription and dosage, proportion of patients at HbA1c target, and proportion of patients with intensification of diabetes management |
|
| Shepherd et al. [35] (8) | Describes a course development for insulin initiation, attendance and evaluation, over a 34-month period | Three unspecified locations in South West UK | Cross-sectional evaluation | Course was delivered by local diabetes professionals and educational experts to healthcare professionals | 165 participants in training, 80 practice teams responded to survey (37.5%) | Survey to determine whether an insulin initiation course had changed practice of healthcare professionals and whether people with T2DM were subsequently started on insulin |
|
| Verges et al. [38], [39] (9) | To explore insulin initiation strategies and outcomes for patients using insulin plus oral anti-diabetes drugs. | General Practices, France | Longitudinal, observational | Physicians (GP & Specialists)/Patients with T2DM | 678 (36%) | Prescribing decisions of dose, injection frequency, maintenance or removal of OAD, glycaemic control, weight, treatment satisfaction |
|
| Yki-Jarvinen et al. [40] (10) | To compare initiation of insulin individually and in groups with respect to change in HbA1c and several other parameters in T2DM patients. | People with T2DM in Finland, Sweden, U.K., and the Netherlands |
RCT | People with T2DM | 121 (63:58) - no response rate provided | Glycaemic control, hypoglycaemia, insulin dose, body weight, treatment satisfaction and time spent of patient education |
|
Study characteristics
The study characteristics are discussed separately for quantitative studies and the qualitative study.
Quantitative study
Three of the studies were cross-sectional and self-report (2, 4, and 8), three were Randomised Controlled Trials (RCT) (1, 7, and 10) and three were longitudinal observational studies (3, 6 and 9). Sample size ranges from 20 to 20,493 participants. Response rates ranged from 11% to 95%, with one study not providing a response rate (10) because the study used purposive sampling. The outcomes assessed in the included quantitative studies varied widely, from changes in HbA1c levels with new models of care, to healthcare professionals’ satisfaction with the models. Four of the studies were conducted in the United Kingdom (UK) (2, 3, 4, and 8), one in Australia (1), one each in New Zealand (6), France (9), and Canada (7) and one across four countries (Finland, Sweden, UK and Netherlands) (10). Four of the studies were conducted in general practices (1, 3, 4, and 9), one in both a general practice and using a national register of diabetes care staff (2), one in both general practices and community pharmacies (7), and two that did not specify a setting (8 and 10). Three studies involved people with T2DM (6, 9, and 10), two studies mentioned the involvement of healthcare professionals generally (4 and 8), two studies involved General Practitioners (GPs), Practice Nurses (PNs), Diabetes Specialist Nurses (DSNs) and patients with T2DM (1, 3), one study involved DSNs and PNs (2), and one involved GPs, community pharmacists and people with T2DM (7).
Qualitative study
The qualitative study (5) was conducted in a general practice in Australia with both GPs and patients with T2DM. A purposive sampling method was used and the data collected included interviews (24 healthcare professionals and patients) and focus groups (10 patients). A thematic analysis of the data was performed, however the study publication did not state a theoretical framework.
Narrative synthesis: initiation of injectable therapy for T2DM strategies
Injectable therapy initiation can be successfully managed in primary care
The majority of the studies demonstrated that injectable therapy initiation for people with T2DM can be successfully managed in primary care following the implementation of a model of care, or an education program to GPs and nurses (1, 3, 5 and 9). GPs and nurses reported feeling more confident to initiate and titrate insulin with education and support (4, 8), however the one study that objectively measured insulin prescribing rates following a program of specialist support showed no difference in insulin prescribing rates between intervention and control physicians (7).
GP and/or PNs working with support from specialists
Three models identified in this review included GPs and PNs working together with support from specialists (e.g. DSN, endocrinologist or pharmacist; 1, 5 and 7). In two of these models, healthcare professionals successfully initiated insulin in an effective manner measured by self-report (5) or reductions in HbA1c and increased time in target glucose range (1). The third model – assessed via RCT (7) – involved an intervention with two-tiered support as follows: 1) provision of active support by a CDE to GPs for two months and passive support for 10 months and; 2) a community retail pharmacist option for the GP for referral to initiate insulin. This intervention did not result in an enhancement of insulin initiation, as measured by objective insulin-prescribing rates, however (7). Two studies (1 and 5) involved the GP and PN working together in an enhanced role and being mentored by a Clinical Diabetes Educator (CDE) nurse and endocrinologist if required.
Nurse-led models of initiating injectable therapy
Four studies included nurse-led models of initiating injectable therapy for people with T2DM (1, 3, 5 and 6). In two studies (1 and 5) the GPs and PNs worked together, with the GPs identifying and making recommendations for starting insulin, while the PNs led care provision by starting the patient on an injectable therapy and having discussions about general diabetes management and education. In one study (3) an experienced DSN supported PNs to undertake their first insulin initiations, until PNs were confident to perform this role. In another study (6) education and initiation of injectable therapy was successfully provided by a nurse using both individual and group sessions.
Group initiation of injectable therapy
Two studies (6 and 10) involved the initiation of injectable therapy for people with T2DM in a group setting. One study (6) found an improvement in HbA1c levels over a 12-month period following the group initiation, and the other study found no differences in glycaemic management levels and treatment satisfaction between those who had insulin initiated individually and those who had received support to commence insulin in a group setting.
Insulin initiation training programs to GPs and PNs
Six of the identified studies involved training for GPs and/or PNs to initiate injectable therapy for people with T2DM. Training involved insulin types, delivery devices, insulin regimes, injection techniques through interactive workshops. Amount of training ranged from three hours (5) to two full days (4). In three studies, training was provided to both GPs and PNs (1, 3, 5) which resulted in reductions in HbA1c levels (1 and 3), increased time in a target glucose range (1 and 3). Greater engagement with GPs and PNs was also reported as a result of healthcare provider training programs (5 and 8).
Injectable therapy initiation models mainly occur in general practices
Eight of the studies investigated models of injectable therapy initiation that involved general practice settings (1–7, and 9). Two studies did not specify where the injectable therapy initiation was occurring (8 and 10).
Risk of bias within studies
For the purpose of our review, we included qualitative, cross sectional, longitudinal observational, and RCT study designs. For the qualitative study, criteria on the Qualsyst that were not met were: 1) a thorough description of the data collection methods (e.g. no discussion about data saturation); and 2) mention of reflexivity (e.g. the influence of the researcher on the study results). For the cross sectional studies, the rigour of methodology was compromised by a low response rate or lack of information about the response rate, and a lack of a clear description about subject groups’ selection and characteristics hence limiting the ability to generalise findings. For longitudinal observational studies the study validity was compromised by a lack of detail regarding the control of confounding variables [19]. The risk of bias for cross-sectional design, observational and descriptive studies are reported in table two. The risk of bias for the qualitative study is reported in table three and the risk of bias for RCTs are reported in table four (Tables Table 2, Table 3, Table 4).
Table 2.
Risk of bias for cross-sectional design, observational and descriptive studies.
| Question or objective sufficiently described? | Design evident and appropriate to answer study question? | Method of subject selection or source of information/input variables is described and appropriate. | Subject characteristics or input variables/information sufficiently described? | Outcome measure(s) well defined and robust to measurement/misclassification bias? Means of assessment reported? | Sample size appropriate? | |
|---|---|---|---|---|---|---|
| Coates et al. [6] | ++ | ++ | ++ | ++ | ++ | ++ |
| Dale et al. [8] | ++ | ++ | + | + | ++ | ++ |
| Downey [13] | + | – | + | – | + | ++ |
| Greenslade et al. [17] | + | + | + | – | ++ | ++ |
| Shepherd et al. [35] | ++ | ++ | + | – | – | – |
| Verges et al. [38], [39] | ++ | ++ | ++ | ++ | ++ | ++ |
| Analysis described and appropriate? | Some estimate of variance is reported for the main results/outcomes? | Controlled for confounding? | Results reported in sufficient detail? | Do the results support the conclusions? | |
|---|---|---|---|---|---|
| Coates et al. [6] | ++ | + | + | ++ | ++ |
| Dale et al. [8] | – | ++ | n/a | + | + |
| Downey [13] | – | n/a | n/a | – | + |
| Greenslade et al. [17] | ++ | – | n/a | – | + |
| Shepherd et al. [35] | – | – | n/a | – | – |
| Verges et al. [38], [39] | ++ | ++ | + | ++ | ++ |
Note: Yes (++); Partial (+); No (–); Not applicable (n/a).
Criteria adapted from Kmet et al. [24].
Table 3.
Risk of bias for the qualitative study.
| Objective clearly described? | Design evident and appropriate to answer study question? | Context for the study is clear? | Connection to a theoretical framework/wider body of knowledge? | Sampling strategy described, relevant and justified? | |
|---|---|---|---|---|---|
| Furler et al. [16] | ++ | ++ | + | ++ | ++ |
| Data collection methods clearly described and systematic? | Data analysis clearly described, complete and systematic? | Use of verification procedure(s) to establish credibility of the study? | Conclusions supported by the results? | Reflexivity of the account? | |
|---|---|---|---|---|---|
| Furler et al. [16] | ++ | + | ++ | ++ | ++ |
Note: Yes (++); Partial (+); No (–); Not applicable (n/a).
Criteria adapted from Kmet et al. [24].
Table 4.
Risk of bias for Randomised Control Trials.
| Author | Selection bias |
Performance bias | Detection bias | Attrition bias | |
|---|---|---|---|---|---|
| Random sequence generation | Allocation concealment | ||||
| [2] | Unclear | Unclear | Unclear | Low | Low |
| [20] | Low | Low | Unclear | Low | Low |
| [40] | High | Low | Unclear | Low | Low |
Criteria adapted from Clarke and Oxman [5].
Discussion
This systematic review explored existing models for the initiation of injectable therapy for people with T2DM in primary care, through the examination of both quantitative and qualitative studies. A range of models were identified, with successful elements of such models summarised to allow for the initiation of injectable therapy in primary care settings to be more readily and frequently adopted.
The studies included in this review have provided some evidence that the initiation of injectable therapy can be successfully managed in primary care (e.g. [2], [9], [16]. Strategies identified in the literature to assist people with T2DM to commence on an injectable therapy have included the provision of training programs to nurses and GPs (e.g. [2], [9], [34]) and introducing nurse-led models of care (e.g. [16], [17]) with specialist support available. Education programs for the initiation of injectable therapies have shown to also boost the confidence of GPs and nurses in undertaking this task [9]. In addition, having specialist support, such as a CDE or endocrinologist, available to nurses and GPs can assist with the timely, safe and effective initiation of injectable therapy [2]. Initiating injectable therapy in the primary care setting using nurse-led models of care with specialist support available was shown to be effective in both qualitative and quantitative studies [9], [2], [16].
In line with the findings of this systematic review, the literature has shown that training provided to health professionals can result in large changes in professional practice, not just for diabetes care management [27]. Abramczyk et al. [1] suggest that training for nurses who are involved in diabetes care is essential to support diabetes prevention and diagnosis, and to help in the treatment and care processes when managing a person with diabetes. The literature has also shown the effectiveness of nurse-led models of care in other disease areas. For example, a study that compared the effectiveness of a nurse-led hypertension clinic with conventional community care in general practice for the management of uncontrolled hypertension in patients with T2DM found that compared with conventional care, this type of model is more effective [11].
Nonetheless, it is evident through this systematic review that studies investigating strategies for the initiation of injectable therapy for people with T2DM in primary care are few, with only ten studies in total identified. This is despite the need for more insulin initiation to occur in primary care to ease the burden on secondary care, reduce the amount of time that people spend with sub-optimal blood glucose levels, and reduce the risk of long term complications developing [6], [31]. In addition, the quality of the majority of identified publications was relatively poor, with little evidence of planning for a rigorous program evaluation in newly implemented programs, with the exception of Blackberry et al. [2] and Furler et al. [16]. This resulted in high risks of bias across the remaining programs and relatively low generalisability, or opportunity to replicate findings.
The majority of the research conducted in the area has also focused on general practice settings, with no study investigating insulin initiation in other areas of primary care, such as in the home environment. Home nurses play a pivotal role in assisting with the management of diabetes and therefore may be well placed to help with the initiation of injectable therapies and provide the education and care needed [10]. Working in the home environment provides rich information on what interventions may be more effective, as health providers can ascertain the world within which their patients live [32]. Despite the obvious potential for such a model, no research has formally evaluated the initiation of injectable therapy in the home setting by home nurses or diabetes educators [22]. With the growing older population and advances in telehealth, the usefulness and success of this type of home-based model clearly warrants further investigation.
In conclusion, the reviewed studies show that initiating injectable therapy can successfully occur in primary care by providing education and specialist support to GPs and nurses, but such strategies have not consistently led to positive changes in insulin prescribing patterns. Overall however, studies that evaluate models of injectable therapy initiation in primary care are few, and have been of average quality. High quality studies with methodological rigour in the evaluation of models of care for T2DM are needed in order to make specific recommendations for the uptake of these models. There is an urgent need to reform current practices for the timely initiation of insulin, which can reduce risks of developing diabetes-related complications and reduce longer-term health costs. This systematic review of the literature has demonstrated that current studies trialling and evaluating alternate models of care are not sufficient in quantity or quality to adequately inform practice, with more research of high rigour in this area being necessary.
References
- 1.Abramczyk A., Lewoc J., Izworski A. Nurse training case study: e-training of nurses in diabetes problems. Nurse Educ Pract. 2005;5(2):70–77. doi: 10.1016/j.nepr.2004.01.007. [DOI] [PubMed] [Google Scholar]
- 2.Blackberry I.D., Furler J.S., Ginnivan L.E., Derraz H., Jenkins A., Cohen N. An exploratory trial of insulin initiation and titration among patients with type 2 diabetes in the primary care setting with retrospective continuous glucose monitoring as an adjunct: INITIATION study protocol. Bmc Family Practice. 2014;15 doi: 10.1186/1471-2296-15-82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Britt H., Miller G.C., Charles J., Henderson J., Bayram C., Pan Y. Australian Institute of Health and Welfare, and, University of Sydney; 2009. General practice activity in Australia 2008–09. [Google Scholar]
- 4.Brod M., Alolga S.L., Meneghini L. Barriers to initiating insulin in type 2 diabetes patients: development of a new patient education tool to address myths, misconceptions and clinical realities. Patient-Patient-Centered Outcomes Res. 2014;7(4):437–450. doi: 10.1007/s40271-014-0068-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Clarke M, Oxman A. Cochrane Reviews' Handbook 4.0, Oxford. UK., The Cochrane Collaboration, 2000.
- 6.Coates V.E., Dromgoole P., Turner E. Insulin initiation in adults: evidence based or context driven? J Nurs Healthcare Chronic Illness. 2009;1(1):105–112. [Google Scholar]
- 7.Control D., C. T. R. Group The effect of intensive treatment of diabetes on the development and progression of long-term complications in insulin-dependent diabetes mellitus. N Engl J Med. 1993;329(14):977–986. doi: 10.1056/NEJM199309303291401. [DOI] [PubMed] [Google Scholar]
- 8.Dale J., Gadsby R., Shepherd J. Insulin initiation in primary care for patients with type 2 diabetes: six month follow-up audit. Br J Diabetes Vasc Dis. 2008;8(1):28–31. [Google Scholar]
- 9.Dale J., Martin S., Gadsby R. Insulin initiation in primary care for patients with type 2 diabetes: 3-Year follow-up study. Primary Care Diabetes. 2010;4(2):85–89. doi: 10.1016/j.pcd.2010.03.001. [DOI] [PubMed] [Google Scholar]
- 10.Davis W.A., Lewin G., Davis T.M., Bruce D.G. Determinants and costs of community nursing in patients with type 2 diabetes from a community-based observational study: The Fremantle Diabetes Study. Int J Nurs Stud. 2013;50(9):1166–1171. doi: 10.1016/j.ijnurstu.2012.11.013. [DOI] [PubMed] [Google Scholar]
- 11.Denver E.A., Barnard M., Woolfson R.G., Earle K.A. Management of uncontrolled hypertension in a nurse-led clinic compared with conventional care for patients with type 2 diabetes. Diabetes Care. 2003;26(8):2256–2260. doi: 10.2337/diacare.26.8.2256. [DOI] [PubMed] [Google Scholar]
- 12.Department of Health and Ageing . Commonwealth of Australia; Canberra, Australia: 2008. Towards a National Primary Health Care Strategy: A discussion Paper from the Australian Government. [Google Scholar]
- 13.Downey J. Providing education to enable healthcare professionals to safely initiate insulin in primary care. Diabetes Primary Care. 2007;9(5) S2-S2. [Google Scholar]
- 14.Funnell M.M. Overcoming barriers to the initiation of insulin therapy. Clin Diabetes. 2007;25(1):36–38. [Google Scholar]
- 15.Furler J., Spitzer O., Young D., Best J. Insulin in general practice barriers and enablers for timely initiation. Aust Fam Physician. 2011;40(8):617–621. [PubMed] [Google Scholar]
- 16.Furler J.S., Blackberry I.D., Walker C., Manski-Nankervis J.A., Anderson J., O'Neal D. Stepping up: a nurse-led model of care for insulin initiation for people with type 2 diabetes. Fam Pract. 2014;31(3):349–356. doi: 10.1093/fampra/cmt085. [DOI] [PubMed] [Google Scholar]
- 17.Greenslade M., Lunt H., Kendall D., Frampton C. ‘Introduction to Insulin’classes: flexible approach to insulin initiation. Pract Diabetes Int. 2009;26(4):142–144. [Google Scholar]
- 18.Guariguata L., Whiting D., Hambleton I., Beagley J., Linnenkamp U., Shaw J. Global estimates of diabetes prevalence for 2013 and projections for 2035. Diabetes Res Clin Pract. 2014;103(2):137–149. doi: 10.1016/j.diabres.2013.11.002. [DOI] [PubMed] [Google Scholar]
- 19.Guyatt G.H., Oxman A.D., Vist G., Kunz R., Brozek J., Alonso-Coello P. GRADE guidelines: 4. Rating the quality of evidence—study limitations (risk of bias) J Clin Epidemiol. 2011;64(4):407–415. doi: 10.1016/j.jclinepi.2010.07.017. [DOI] [PubMed] [Google Scholar]
- 20.Harris S.B., Gerstein H.C., Yale J.F., Berard L., Stewart J., Webster-Bogaert S. Can community retail pharmacist and diabetes expert support facilitate insulin initiation by family physicians? Results of the AIM@GP randomized controlled trial. Bmc Health Services Res. 2013;13 doi: 10.1186/1472-6963-13-71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Inzucchi S.E., Bergenstal R.M., Buse J.B., Diamant M., Ferrannini E., Nauck M. Management of hyperglycemia in type 2 diabetes: a patient-centered approach position statement of the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD) Diabetes Care. 2012;35(6):1364–1379. doi: 10.2337/dc12-0413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kennedy M.J., Davis D.A., Smith N., Gaedigk A., Pearce R.E., Kearns G.L. Six-month, prospective, longitudinal, open-label caffeine and dextromethorphan phenotyping study in children with growth hormone deficiency receiving recombinant human growth hormone replacement. Clin Ther. 2008;30(9):1687–1699. doi: 10.1016/j.clinthera.2008.09.012. [DOI] [PubMed] [Google Scholar]
- 23.King P., Peacock I., Donnelly R. The UK Prospective Diabetes Study (UKPDS): clinical and therapeutic implications for type 2 diabetes. Br J Clin Pharmacol. 1999;48(5):643–648. doi: 10.1046/j.1365-2125.1999.00092.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kmet L.M., Lee R.C., Cook L.S. Alberta Heritage Foundation for Medical Research Edmonton; 2004. Standard quality assessment criteria for evaluating primary research papers from a variety of fields. [Google Scholar]
- 25.Kunt T., Snoek F. Barriers to insulin initiation and intensification and how to overcome them. Int J Clin Pract. 2009;63(s164):6–10. doi: 10.1111/j.1742-1241.2009.02176.x. [DOI] [PubMed] [Google Scholar]
- 26.Leivesley K. Barriers to insulin initiation in primary care. Practice Nurs. 2005;16(9):434–441. [Google Scholar]
- 27.O'Brien M., Freemantle N., Oxman A., Wolfe F., Davis D., Herrin J. “Continuing education meetings and workshops: effects on professional practice and health care outcomes. The Cochrane Library. 2009;1 doi: 10.1002/14651858.CD003030. [DOI] [PubMed] [Google Scholar]
- 28.Owens D.R. Clinical evidence for the earlier initiation of insulin therapy in type 2 diabetes. Diabetes Technol Ther. 2013;15 doi: 10.1089/dia.2013.0081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Palmera A.J., Rozea S., Valentinea W.J., Minshallb M.E., Foosa V., Luratia F.M. Validation of the CORE Diabetes Model against epidemiological and clinical studies. Curr Med Res Opin. 2004;20(sup1):S27–S40. doi: 10.1185/030079904X2006. [DOI] [PubMed] [Google Scholar]
- 30.Parchman M.L., Pugh J.A., Romero R.L., Bowers K.W. Competing demands or clinical inertia: the case of elevated glycosylated hemoglobin. Ann Family Med. 2007;5(3):196–201. doi: 10.1370/afm.679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Paul S.K., Klein K., Thorsted B.L., Wolden M.L., Khunti K. Delay in treatment intensification increases the risks of cardiovascular events in patients with type 2 diabetes. Cardiovasc Diabetol. 2015;14 doi: 10.1186/s12933-015-0260-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Rosa M.A., Lapides S., Hayden C., Santangelo R. The interdisciplinary approach to the implementation of a diabetes home care disease management program. Home Healthcare Now. 2014;32(2):108–116. doi: 10.1097/NHH.0000000000000022. [DOI] [PubMed] [Google Scholar]
- 33.Seuring T., Archangelidi O., Suhrcke M. The economic costs of type 2 diabetes: a global systematic review. Pharmacoeconomics. 2015;33(8):811–831. doi: 10.1007/s40273-015-0268-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Shepherd M., Frost J., Jones J., Soper C., Macleod K. Insulin initiation in primary care: Helping it happen. Diabetes Primary Care. 2007;9(3) [Google Scholar]
- 35.Shepherd M., Frost J., Jones J., Soper C., MacLeod K. Insulin initiation in primary care: helping it happen. Diabetes Primary Care. 2007;9(3):152–157. [Google Scholar]
- 36.Stratton I.M., Adler A.I., Neil H.A.W., Matthews D.R., Manley S.E., Cull C.A. Association of glycaemia with macrovascular and microvascular complications of type 2 diabetes (UKPDS 35): prospective observational study. BMJ. 2000;321(7258):405–412. doi: 10.1136/bmj.321.7258.405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.The Royal Australian College of General Practitioners . VIC, RACGP; East Melbourne: 2016. General practice management of type 2 diabetes:2016–18. [Google Scholar]
- 38.Verges B., Brun J.M., Tawil C., Alexandre B., Kerlan V. Strategies for insulin initiation: insights from the French LIGHT observational study. Diabetes-Metab Res Rev. 2012;28(1):97–105. doi: 10.1002/dmrr.1288. [DOI] [PubMed] [Google Scholar]
- 39.Verges B., Brun J.M., Tawil C., Alexandre B., Kerlan V. Strategies for insulin initiation: insights from the French LIGHT observational study. Diabetes Metab Res Rev. 2012;28(1):97–105. doi: 10.1002/dmrr.1288. [DOI] [PubMed] [Google Scholar]
- 40.Yki-Jarvinen H., Juurinen L., Alvarsson M., Bystedt T., Caldwell I., Davies M. Initiate insulin by aggressive titration and education (INITIATE) - a randomized study to compare initiation of insulin combination therapy in type 2 diabetic patients individually and in groups. Diabetes Care. 2007;30(6):1364–1369. doi: 10.2337/dc06-1357. [DOI] [PubMed] [Google Scholar]