Highlights
-
•
Our paper describes the development and adoption of a novel model of inpatient diabetes care, expanding the role of diabetes educators to include case management, and establishment of a Diabetes Resource Nurse program aimed at increasing the knowledge of staff nurses in caring for patients with diabetes.
-
•
Retrospective analysis of readmission data was performed, showing significant reductions in readmission rates for patients exposed to this program. This program is relatively easy to adopt and was well accepted by nurses.
-
•
We believe that our paper provides data that are relevant for both clinicians and administrators examining the models of inpatient diabetes care.
Keywords: Readmissions, Inpatient diabetes management, Nursing education, Case management
Abstract
Aims
Patients with diabetes have higher readmission rates than those without diabetes, yet limited data on efforts to reduce their readmissions are available. We describe a novel model of inpatient diabetes care, expanding the role of diabetes educators to include case management, and establishment of a Diabetes Resource Nurse program, aimed at increasing the knowledge of staff nurses, and evaluate the impact of this program on readmission rates.
Methods
We performed retrospective analysis of 30-day readmission rates of patients with diabetes before (July 2010–December 2011), and after (January 2012–June 2013) starting the implementation of this tiered inpatient diabetes care delivery model.
Results
We analyzed 34,472 discharged patient records from the 18-month pre-intervention period, and 32,046 records from the 18-month post-intervention period. The overall 30-day readmission rate for patients with diabetes decreased significantly from 20.1% (pre) to 17.6% (post) intervention (p < 0.0001). Patients seen by diabetes educators had the lowest 30-day readmission rates (∼15% during the whole study), a rate approaching the overall hospital readmission rates in those without diabetes in our institution.
Conclusion
The Diabetes Resource Nurse program is effective in decreasing readmission rates. Patients seen by the diabetes educators have the lowest rates of readmission.
Introduction
Unplanned hospital readmissions are recognized to be significant contributors to overall health care costs and may also suggest suboptimal quality of care [1], [2]. Therefore, policy makers have charged healthcare organizations to reduce readmissions in order to lower cost and improve outcomes. Hospital readmission rates in general are classified as early (30 day readmission rates), or late (90 day readmission rates). Overall, readmission rates for all Medicare patients are approximately 20% at 30 days and 34% at 90 days [3] but vary according to region and admission diagnosis and range anywhere from 11 to 32% for patients with CHF and 8 to 27% for pneumonia [4].
Hence, efforts have focused on identifying factors that increase the risk of readmission. Risks described to date include the severity of illness, presence of coexisting conditions (including diabetes), age, low socioeconomic status, previous hospitalization, as well as suboptimal care at hospital discharge and thereafter [3], [5], [6], [7], [8]. Efforts to reduce re-admission were developed by focusing on these risk factors including improvement in discharge planning, ensuring timely follow up, and improving transitional care. However, most to date have shown limited efficacy [9], [10].
Diabetes is an increasingly prevalent condition among patients hospitalized for other medical problems. It is estimated that about 25% of all hospitalized patients have diabetes [6], [11] and this can be a contributing factor which increases the risk of readmissions [12]. Overall readmission rates for patients with diabetes are higher than those for patients without diabetes, and have been reported at 14–30%, averaging at ∼20% in most studies [3], [4], [6], [13], [14], [15]. Similar to the general population, predictors of readmission among the inpatient diabetes cohort include racial and socioeconomic factors, non-diabetes related co-morbidities, and failure to acknowledge diabetes at discharge [14], [15]. Rubin et al. identified poor health literacy, failure of the discharge process, social determinants, and loss of control over illness as contributors to readmissions [16] and recently developed a tool to predict a hospital readmission risk among patients with diabetes [17].
Data on efforts to reduce readmissions by interventions specifically targeting patients with diabetes are very limited. An association between high admission A1c and readmissions has been described [18], [19], [20], it is unclear whether improving hospital glycemic control would decrease re-admission rates. A randomized study of 179 participants showed that involvement of an inpatient diabetes team (endocrinologist and nurse educator) significantly reduced readmission rates [21]. More recently, glucose therapy intensification during hospitalization was associated with a decreased 30-day readmission risk among patients with elevated A1c [22]. Healy et al. retrospectively analyzed single-center readmission data and found that formal inpatient diabetes education for patients with poorly controlled diabetes (those with A1c >9%) is associated with 34% reduced odds of all cause readmissions at 30 days and 20% reduced odds of readmissions at 180 days [23]. Since, this study was limited to hospitalized patients with poor glycemic control, we do not know if patients with better baseline glucose control would benefit from the same intervention. In addition, many hospitals have a limited number of inpatient diabetes educators and only a small fraction of patients can be evaluated during their hospital stay. Therefore, if inpatient diabetes education can make an impact on patient care outcomes, it needs to be expanded to a larger portion of the patient population.
To that point, we have developed an innovative model to improve inpatient diabetes care at the bedside in our 600-bed tertiary care hospital. We expanded the role of our inpatient certified diabetes educators (CDE) to incorporate case management principles and renamed them as Diabetes Case Managers (DCM). In addition, we expanded the education of unit-based nurses and implemented a comprehensive curriculum to increase their knowledge in caring for hospitalized patients with diabetes and named them the Diabetes Resource Nurses (DRN). We hypothesized that DRNs will be a resource to other unit nurses as well as patients leading to improved patient care that in turn would translate to improved outcomes and reduced readmissions.
Study questions
This project examined the expansion of the role of the inpatient CDE to incorporate case management principles. It also evaluated the efficacy of implementation of the Diabetes Resource Nurse (DRN) program designed to increase the knowledge of staff nurses on medical-surgical units in diabetes management in the hospital setting. Specifically the project aimed answering the following questions:
-
1.
Do hospitalized patients with diabetes who receive case management services from CDEs have a lower readmission rate than those patients with diabetes who did not receive such services ?
-
2.
Does the rate of re-admission decrease among hospitalized patients with diabetes after the implementation of the DRN program?
Subjects
All admitted patients to University Of Nebraska Medical Center were included in analysis of readmission rates. Patients with admission diagnosis of diabetes were analyzed separately from those without diabetes.
Materials and methods
This is a retrospective analysis of 30-day readmission rates for patients with diabetes before and after implementation of our novel diabetes care delivery model as described above.
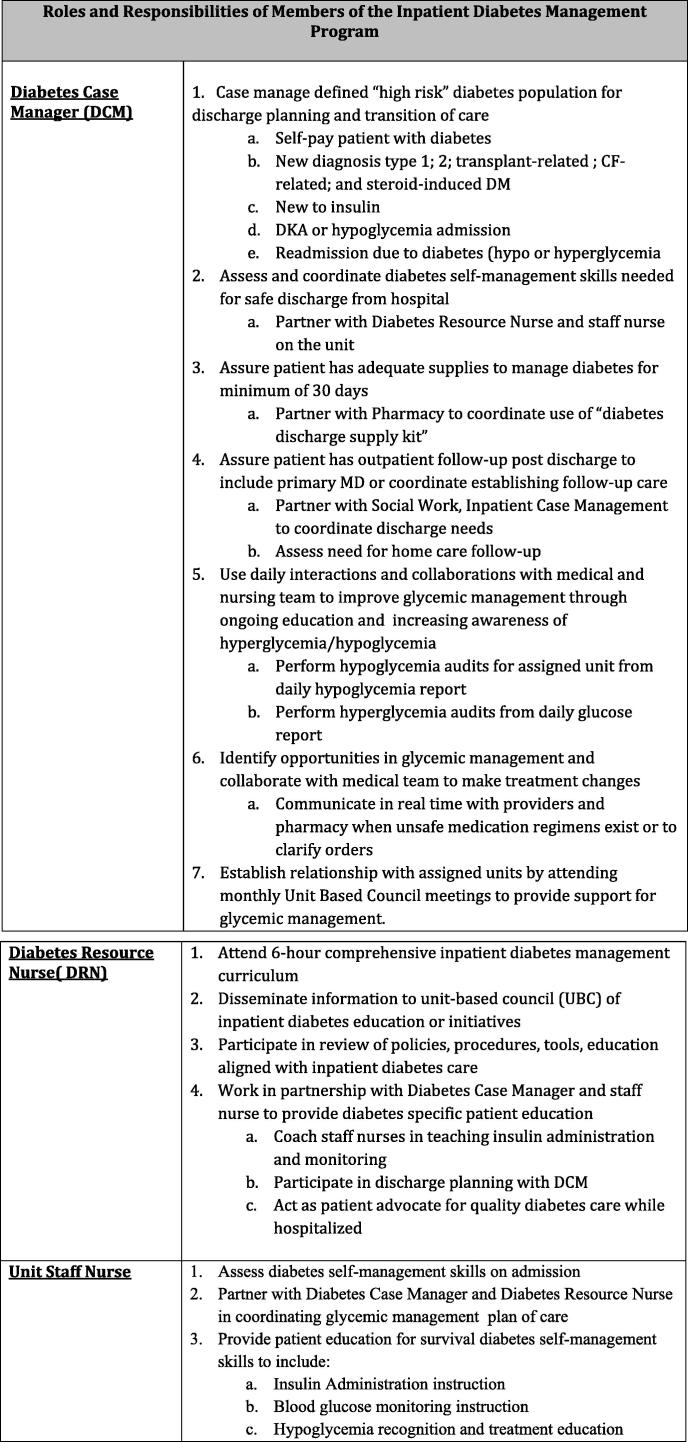
DCM model of care
Starting January 2012, the role of the CDE was expanded from providing diabetes self-management education to now include case management services (DCM) (Fig. 1). Both CDEs and DCMs were consulted on individuals deemed to be “high risk patients”, but DCMs also focused on daily interactions and collaborations with medical and nursing team to improve glycemic management in the whole hospital. They performed hypoglycemia and hyperglycemia audits, facilitating intervention in care of patients throughout the hospital that were not formally assigned to their individual care.
Fig. 1.
DRN model of care
Starting January 2012, a model was developed to increase the involvement and knowledge level of unit nurses from medical-surgical units who were interested in expanding their diabetes knowledge base. The DRN program goals were to improve the care of the patient with diabetes or hyperglycemia during hospital stay, improve transitions of care, and empower the nurse to be able to make educated decisions for patients with diabetes at the bedside. They all underwent a 6-h Diabetes Resource Nurse training. The DRNs then became the “go to” person on each unit for diabetes care (Fig. 1).
Readmission data were evaluated during the total period from July 1st 2010 to June 30th 2013. The data were divided into “pre-intervention” period from July 1st 2010–Dec 31st 2011, encompassing eighteen months prior to the implementation of the DRN model, and “post-intervention” period from January 1st 2012–June 30th 2013, eighteen months after implementation of the DRN model started. The tiered implementation of the new nursing model was ongoing during the whole 18 months of the “post-intervention” period.
In the pre-intervention period, thirty-day readmissions of patients with diabetes who received care by CDE were compared to patients with diabetes who received care provided by unit nurses. In the post-intervention period, we compared thirty-day readmissions of patients with diabetes who received care provided by DCM vs that provided by DRN.
Statistical analysis
Data were analyzed using descriptive and inferential statistics. Total 30-day readmission rate of the hospital and 30-day readmission rate of patients with a diagnosis of diabetes, are expressed in percentage of frequency of all patient discharges; percentage of frequency of all patients with a diagnosis of diabetes; and percentage of diabetes readmissions (number of diabetes readmissions/all readmissions). Chi-Square test was used for all comparisons on SAS ® 9.4. The calculated p-values were without adjustment for multiple comparisons. Level of significance was defined as p < 0.05.
Results
Recruitment of DRN
The original goal was to recruit four to five nurses from each unit to participate. The interest exceeded this goal and the curriculum was opened to any interested nurses, with a minimum of five nurses from each unit representing both 12-h work shifts. During the post- intervention period (Jan 2012–June 2013) a total of 126 nurses were trained, and the program was expanded from focusing primarily on medical-surgical units to any interested unit nurse. This included nurses from critical care units and ancillary support units, such as the medical call center who interact with patients after discharge with diabetes.
Overall admission and readmission rates
Analysis of 34,472 discharged patient records were completed from the 18-month pre-intervention period, and 32,046 discharged patient records from the 18-month post-intervention period (see Table 1). More women were admitted than men (51.75% vs 48.25% 0; p = 0.0014). Mean age was 54 yrs in the entire group, but discharged patients with diabetes were significantly older than those without diabetes (60.2 vs 52.0 yrs; p < 0.001). Overall hospital readmission rates were 13.87% during the entire study period. Men had higher (15.3%) overall 30 day readmission rates compared to women (12.97%) (p < 0.0001) and this was evident both in pre-intervention phase (M: 15.70% vs F: 13.77%; p < 0.001) as well as post-intervention phase (M: 14.33% vs F: 12.09%; p < 0.001).
Table 1.
Discharges and readmission rates pre- and post-intervention.
| Variables | 18 months Pre-intervention |
18 months Post-intervention |
||
|---|---|---|---|---|
| N = | % | N = | % | |
| All patients discharged | 34,472 | 32,046 | ||
| All patients with Non-DM discharged | 24,952 | 72.4% | 22,655 | 70.7% |
| All patients with DM discharged | 9520 | 27.6% | 9391 | 29.3% |
| All patients 30-day readmissions | 5030 | 14.6% | 4202 | 13.1% |
| All Non-DM patients 30-day readmissions | 3112 | 12.47% | 2547 | 11.25% |
| All DM patients 30-day readmissions | 1918 | 20.1% | 1653 | 17.6% |
| DM prevalence of all 30-day readmissions | 1918 | 38.1% | 1653 | 39.3% |
| DM patients seen by CDE Pre | 1817 | 19.1% | ||
| DM 30-day readmissions seen by CDE Pre | 275 | 15.1% | ||
| DM patients seen by DCM Post | 1718 | 18.3% | ||
| DM 30-day readmissions seen by DCM Post | 271 | 15.8% | ||
| Patients with usual care Pre | 7703 | 80.9% | ||
| DM 30-day readmissions with usual care Pre | 1643 | 21.3% | ||
| DM patients with DRN intervention Post | 7673 | 81.7% | ||
| DM 30-day readmissions with DRN intervention Post | 1382 | 18.0% | ||
Abbreviations: DM = Diabetes mellitus, CDE = Certified Diabetes educator, DCM = Diabetes Case Manager, DRN = Diabetes Resource Nurse.
Diabetes as a contributing factor to admissions and readmissions
Almost a third of all admitted patients had diabetes. There were 9520 (27.6%) discharged patients with diabetes in the pre-intervention group and 9391 (29.3%) in the post-intervention group. Patients with diabetes contributed even more to the readmitted group. In the pre-intervention group, 1918 (38.1%) of all patients readmitted within 30 days had diabetes. This rate remained high in the post-intervention group, where 1653 (39.3%) had diabetes.
Readmission rates for patients with diabetes
The overall 30-day readmission rate for patients with diabetes decreased significantly from 20.1% (pre) to 17.6% (post) intervention (p < 0.0001) (Table 1). However, the 30-day readmission rates for patients with diabetes (20.1%), was significantly higher than the overall hospital readmission rate (14.6%) in the pre-intervention period (p < 0.0001). Similarly, in the post-intervention period, the 30-day readmission rates for patients with diabetes (17.6%) remained higher than the 30-day readmission rate for all patients (13.1%) (p < 0.0001).
Effectiveness of diabetes educators as CDEs and DCMs
In the pre-intervention period, the 30-day readmission rate of patients with diabetes seen by the CDE was 15.1%, compared to 21.3% for those who received usual diabetes care by unit nurses (p < 0.0001) (Table 1, Table 2). In the post-intervention period, patients with diabetes seen by DCM had a 30-day readmission rate of 15.8%, compared to 18.0% for patients with diabetes who were exposed to the DRN model (p < 0.0001) (Table 1, Table 3).
Table 2.
Readmission rates of patients seen by CDE during 18 months Pre-intervention (Pre-I) vs. DCM during 18 months Post Intervention (Post-I).
| Comparison of Variables | N= | % | N= | % | p value |
|---|---|---|---|---|---|
| All patients with DM readmitted Pre-I/to all patients seen by CDE readmitted Pre-I | 1918 | 20.1% | 275 | 15.1% | p < 0.0001 |
| All patients with DM readmitted Post- I/to all patients seen by DCM Post-I | 1653 | 17.6% | 271 | 15.8% | p = 0.0657 |
Abbreviations: DM = Diabetes mellitus, CDE = Certified Diabetes educator, DCM = Diabetes Case Manager.
Table 3.
Statistical comparison of readmission rates during 18 months of usual care (Pre – intervention: Pre-I) vs 18 months of DRN/DCM (Post – Intervention: Post I).
| Comparisons of Variables | N= | % | N= | % | p value |
|---|---|---|---|---|---|
| Patients with DM readmitted receiving usual care Pre-I/to DM patients readmitted seen by DRN Post-I | 1643 | 21.3% | 1382 | 18.0% | p < 0.0001 |
| Patients with DM readmitted seen by CDE Pre-I/to patients receiving usual care Pre-I | 275 | 15.1% | 1643 | 21.3% | p < 0.0001 |
| Patients seen by DCM Post-I readmitted/to DM patients readmitted seen by DRN Post-I | 271 | 15.8% | 1382 | 18.0% | p = 0.0278 |
Abbreviations: DM = Diabetes mellitus, CDE = Certified Diabetes educator, DCM = Diabetes Case Manager, DRN = Diabetes Resource Nurse.
Effectiveness of Diabetes Resource Nurse (DRN) program
Thirty-day readmission rates for patients with diabetes who were exposed to the DRN (18%) program were significantly lower compared to readmission rates for patients who received usual diabetes care from unit nurses prior to implementation of the DRN program (21.3%), (p < 0.0001). The reduction of readmissions seen with the DRN program remained statistically significant when those results were evaluated within the larger scope of reduced readmission rates for all the patients in the hospital during the 36 months of observation. Readmission rates for patients without diabetes decreased from 12.47% to 11.25% during this study (Table 1), but reduction in readmissions for patients with diabetes after the implementation of the DRN program were overall a larger reduction. The estimated difference of the readmission rate reduction for pre and post intervention between patients with diabetes and those without diabetes is 1.325%, which is statistically significant (p = 0.039;96% CI 0.068–2.58%).
Discussion
This study examined the development and implementation of an innovative inpatient model to improve the care of patients with diabetes, and demonstrated decreases in the rates of hospital readmission for patients with diabetes with the implementation of a DCM and DRN care mode. The readmission rates of patients with diabetes are consistent with what has been described in the literature supporting evidence that suggests diabetes is a major contributor to the patient population readmitted within 30 days. Studies have validated the lack of knowledge for healthcare nurses regarding diabetes management in the hospital, and have also shown interventions aimed at improving nurses’ knowledge in caring for patients with diabetes are effective [24], [25], [26]. There is limited research that has looked at readmission rates following a nursing model intervention.
A similar model to the DRN program developed at The Nebraska Medical Center was described by Newton and Young in 2006 [27] which showed financial feasibility and significant clinical outcome improvements, but did not look at readmission rates. The results of our study address the efficacy of the model related to 30-day readmission rates. The results have shown that patients seen by a CDE in their initial educator role, or in their expanded role as managers (DCM) had the lowest risk of readmission, both in the pre-intervention and post-intervention period. The observation that there was no improvement in readmission rates after expanding the CDE role to DCM is likely related to the fact that the readmission rates for patients seen by CDEs were already very low (15.1%), approaching the overall readmission rates in our hospital (14.6%), and much lower than readmission rates for all patients with diabetes (20.1%). Furthermore, DCMs indirectly influenced the care of all patients in the hospital through their interaction with care teams, hypo and hyperglycemia audits and other activities as listed in Fig. 1. Thus we believe that high risk patients with diabetes benefit from the expertise and availability of a DCM who are an important resource to hospitals in coordinating care, especially during transition to outpatient settings. The results have also shown the implementation of the DRN program significantly decreased the readmission rates of patients not seen by the DCM indicating the effectiveness of providing a comprehensive education curriculum to improve nurses’ knowledge of providing diabetes care in the hospital. This reduction of readmissions for patients seen by DRN is closing the gap in readmission rates for patients exposed to DRNs to those of DCMs (18% vs 15.8%, p = 0.0278) in the post-intervention phase (Table 3). In addition, the effect of DRN on readmission rates could have been underestimated since the DRN education started at the January 2012, and continued throughout June 2013, thus intervention itself lasted throughout the so called “post-intervention” implementation phase.
The DRN education program has been very well received by 126 participating nurses, as evidenced by survey results administered after the completion of the program. This survey evaluated nursing attitudes towards roles and responsibilities they have in caring for patients with diabetes. Seventy-one surveys were available for evaluation and 70/71 agreed or strongly agreed that their diabetes core knowledge improved and that they will use it in daily practice. In addition, 69/71 felt that they had a positive educational experience. Our data compliments a study by Haas showing that the development of tools to improve diabetes knowledge and care can be well accepted by nurses, and implemented effectively [28]. Similarly, the adoption of the DRN program has been well accepted by our nurses. Although financial analysis for the program was not an aim of this project, it has been a feasible program for the hospital to implement, with no significant barriers identified to implementation.
Limitations
This study looked solely at readmission rates for patients with diabetes and not at other clinical outcomes linked with improving diabetes care. Additional analysis of clinical outcomes such as rates of hypoglycemia and hyperglycemia has not yet been performed to evaluate if the program improved glucometrics. The accuracy of the readmission data is dependent upon the ability to accurately capture all patients with a diagnosis of diabetes, which is dependent upon physician documentation. The prevalence of inpatient hyperglycemia in people without preexisting diabetes is often not captured in retrospective studies like this. This study only accounts for those patients with a diagnosis of diabetes. Patients with stress induced hyperglycemia who also have increased risk of mortality and morbidity [29], were not examined in this project. Readmissions are tracked for all causes and are not necessarily related directly to diabetes. Furthermore, due to the way we obtained the data, the analysis did not account for possible differences in various nondiabetes related risk factors including age, polypharmacy and other medical co-morbidities. However, as the DRN program influenced all patients in the hospital, we do not believe that differences in non-diabetes related risk factors for readmission impacted our results since those are likely similar before and after the intervention.
Further analysis of the readmission data could provide information for additional quality improvement interventions targeting readmissions related to diabetes. In addition, we cannot separate the effect of DRN from that of DCM because both education interventions were implemented at the same time and a patient could technically be exposed to both. However, <20% of all hospitalized patients with diabetes are seen by DCM (Table 1), thus we think that DCM intervention could not account for all of the readmission risk reduction seen with implementation of DRN program. Lastly, during the study period there were other initiatives occurring to reduce hospital readmissions. However, as outlined above the decrease in readmission rates seen after the implementation of DRN program remained significant even after the overall reduction in readmission was taken into account. While the difference is small, it is not only statistically but clinically significant as well given the high cost or readmission and a very small cost of nursing education.
Conclusions
The implementation of DRN program has been shown to be an effective intervention in improving care for the patient with diabetes as shown by the decrease in rates of readmissions. Patients seen by the CDE in the pre-intervention period and the DCM in the post-intervention period had the lowest readmission of all readmitted patients with diabetes, approaching the overall hospital readmission rates in those without diabetes. Due to lack of resources, it is not feasible to have the all patients with diabetes seen by a these specialized diabetes experts. The DRN program is an effective option to increase the knowledge level of staff nurses on medical-surgical units, extend the expertise of the DCM, and decrease rates of readmission for all patients with diabetes.
Author contribution
A.D researched data, wrote manuscript; B.P. researched data, Contributed to discussion; J.L. performed statistical data analysis; W.G. reviewed/edited manuscript.
Acknowledgements
We thank Cyrus Desouza, MBBS, for his review of this manuscript and editorial suggestions.
References
- 1.Fisher C., Lingsma H.F., Marang-van de Mheen P.J. Is the readmission rate a valid quality indicator? A review of the evidence. PLoS ONE. 2014;9(11) doi: 10.1371/journal.pone.0112282. e112282-e112282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Rumball, Smith J., Hider P. The validity of readmission rate as a marker of the quality of hospital care ad a recommendation for its definition. N Z Med J. 2009;122(1289):63–70. [PubMed] [Google Scholar]
- 3.Jencks S.F., Williams M.V., Coleman E.A. Rehospitalizations among patients in the Medicare fee-for-service program. N Engl J Med. 2009;360:1418–1428. doi: 10.1056/NEJMsa0803563. [DOI] [PubMed] [Google Scholar]
- 4.Dharmmarjan K., Hseih A.F., Lin Z. Diagnoses and timing of 30-day readmissions after hospitalization for heart failure, acute myocardial infarction, or pneumonia. JAMA. 2013;309:355–363. doi: 10.1001/jama.2012.216476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Epstein A.M., Ashish K.J., Orav E.J. The relationship between Hospital Admission Rates and rehospitalizations. N Engl J Med. 2011;365:2287–2295. doi: 10.1056/NEJMsa1101942. [DOI] [PubMed] [Google Scholar]
- 6.Donze J., Lipsitz S., Bates D., Schnipper J.L. Causes and patterns of readmissions in patients with common comorbidities:retrospective cohort study. BMJ. 2013;347:f7171. doi: 10.1136/bmj.f7171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hernandez A.F., Greiner M.A., Fonarow G.C. Relationship between early physician followup and 30 day readmission among Medicare beneficiaries hospitalized for heart failure. JAMA. 2010;303:1716–1722. doi: 10.1001/jama.2010.533. [DOI] [PubMed] [Google Scholar]
- 8.Joynt K.E., Orav E.J., Jha A.K. Thirty day readmission rates for Medicare beneficiaries by race and site of care. JAMA. 2011;305:675–681. doi: 10.1001/jama.2011.123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bodenheimer T. Coordinating care – a perilous journey through the healthcare system. N Engl J Med. 2008;358:1064–1071. doi: 10.1056/NEJMhpr0706165. [DOI] [PubMed] [Google Scholar]
- 10.Peikes D., Chen A., Schlore J., Brown R. Effects of care coordination on hospitalization, quality of care, and health care expenditures among Medicare beneficiaries: 15 randomized trials. JAMA. 2009;301:603–618. doi: 10.1001/jama.2009.126. [DOI] [PubMed] [Google Scholar]
- 11.Jha A.K., Orav I.J., Epstein A.M. Public reporting of discharge planning and rates of readmissions. N Engl J Med. 2009;361 doi: 10.1056/NEJMsa0904859. 2637-1645. [DOI] [PubMed] [Google Scholar]
- 12.Whitston M., Chung S., Henderson J., Young B. What can be learned about the impact of diabetes on hospital admissions from routinely recorded data? Diabet Med. 2012;29:1199–1205. doi: 10.1111/j.1464-5491.2011.03535.x. [DOI] [PubMed] [Google Scholar]
- 13.Jiang H.J., Stryer D., Friedman B., Andrews R. Multiple hospitalizations for patients with diabetes. Diabetes Care. 2003;26(5):1421–1426. doi: 10.2337/diacare.26.5.1421. [DOI] [PubMed] [Google Scholar]
- 14.Robbins J.M., Webb D.A. Diagnosing diabetes and preventing rehospitalizations: the urban diabetes study. Med Care. 2006;44:292–296. doi: 10.1097/01.mlr.0000199639.20342.87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Rubin D.J. Hospital readmissions of patients with diabetes. Curr Diab Rep. 2015;15(4):17. doi: 10.1007/s11892-015-0584-7. [DOI] [PubMed] [Google Scholar]
- 16.Rubin D., Donnell-Jackson K., Jhingan R., HillGolden S., Parnjape A. Early readmission among patients with diabetes: a qualitative assessment of contributing factors. J Diabetes Complications. 2014;28:869–873. doi: 10.1016/j.jdiacomp.2014.06.013. [DOI] [PubMed] [Google Scholar]
- 17.Rubin D.J., Handorf E.A., Golden S.H., Nelson D.B., McDoness M.E., Zhao H. Development and validation of a novel tool to predict hospital readmission risk among patients with diabetes. Endocr Pract. 2016 doi: 10.4158/E161391.OR. Jul 13.(Epub ahead of print) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Dungan K. Relationship between glycemic control and readmission rates in patients hospitalized with congestive heart failure during the implementation of hospital wide initiatives. Endocr Pract. 2010;16:945–951. doi: 10.4158/EP10093.OR. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Menzin J. Relationship between glycemia control and diabetes related hospital costs in patients with type 1 or type 2 diabetes mellitus. J Manag Care Pharm. 2010;16:264–275. doi: 10.18553/jmcp.2010.16.4.264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Dungan K. The effect of diabetes on hospital readmissions. J Diabetes Sci Technol. 2012;6:1045–1052. doi: 10.1177/193229681200600508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Koproski J., Pretto Z., Poretsly L. Effects of an intervention by a diabetes team in hospitalized patients with diabetes. Diabetes Care. 1997;20:1533–1555. doi: 10.2337/diacare.20.10.1553. [DOI] [PubMed] [Google Scholar]
- 22.Wei N.J., Wexler D., Nathan D.M., Grant R.W. Intensification of diabetes medication and risk for 30 day readmission. Diab Med. 2013;30:56–62. doi: 10.1111/dme.12061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Healy S et al. Inpatient diabetes education is associated with less frequent hospital readmission among patients with poor glycemic control. Diabetes Care 36: 2960–2967. [DOI] [PMC free article] [PubMed]
- 24.Kim H., Ross J., Meikus G., Zhanglin Z., Boockvar K. Scheduled and unscheduled hospital readmission among patients with diabetes. Am J Manage Care. 2010;16:760–767. [PMC free article] [PubMed] [Google Scholar]
- 25.Derr R.L., Mala S.S., Bronich-Hall L., Rodriguez A. Insulin-related knowledge among health care professionals in internal medicine. Diabetes Spectrum. 2007;20:177–185. [Google Scholar]
- 26.Trepp R., Wille T., Wieland T., Reinhart W. Diabetes-related knowledge among medical and nursing house staff. Swiss Med Weekly. 2010;140:370–375. doi: 10.4414/smw.2010.12974. [DOI] [PubMed] [Google Scholar]
- 27.Newton C., Young S. Financial implications of glycemic control: results of an inpatient diabetes management program. Endocr Pract. 2006;12 S:43–48. doi: 10.4158/EP.12.S3.43. [DOI] [PubMed] [Google Scholar]
- 28.Haas L. Improving inpatient diabetes care: nursing issues. Endocr Pract. 2006;12 S:56–60. doi: 10.4158/EP.12.S3.56. [DOI] [PubMed] [Google Scholar]
- 29.Moghissi E., Korytkowski M., DiNardo M., Einhorn D., Helleman R., Hirsch I. American Association of clinical Endocrinologists and American Diabetes Association Consensus Statement on Inpatient Glycemic Control. Diabetes Care. 2009;32:1119–1131. doi: 10.2337/dc09-9029. [DOI] [PMC free article] [PubMed] [Google Scholar]