Highlights
-
•
We report an interesting case with ascending colon cancer and situs inversus totalis (SIT) who underwent laparoscopic hemicolectomy.
-
•
SIT is a rare congenital anomaly with an incidence rate of 1 per 5000–10,000 adults.
-
•
In cases of SIT, the left and right aspects of the thoracic and intra-abdominal organs are inverted, like a mirror image.
Keywords: Situs inversus totalis, Colorectal cancer, Laparoscopic surgery
Abstract
Introduction
Situs inversus totalis (SIT) is a rare congenital anomaly in which the left and right aspects of the thoracic and intra-abdominal organs are inverted, like a mirror image. Surgical procedures in a patients with SIT is difficult as their anatomy is abnormal. In particular, laparoscopic procedures are considered more difficult in patients with SIT because of the mirror-image anatomy.
Presentation of case
The patient was a 75-year-old woman with ascending colon cancer. Laparoscopic hemicolectomy with radical lymphadenectomy was performed. After surgery, no specific complications developed. On the ninth postoperative day, the patient was discharged from our hospital. Recognition of the inverted anatomy by the surgeon using preoperative imaging permitted safe operation using techniques not otherwise differing from those used in ordinary cases.
Discussion and conclusions
Laparoscopic colectomy is considered to be a safe and feasible option for patients with colorectal cancer and SIT.
1. Introduction
Situs inversus totalis (SIT) is a rare congenital anomaly with an incidence rate of 1 per 5000–10,000 adults [1]. In cases of SIT, the left and right aspects of the thoracic and intra-abdominal organs are inverted, like a mirror image [2]. Due to the different anatomical positions of the organs, surgical procedures in patients with SIT are considered more difficult than those in others, particularly laparoscopic surgery. While, laparoscopic colorectal surgery (LCS) is currently the standard procedure for colorectal cancers (CRC), including the present case, only eight cases of LCS for colorectal cancer in patients with SIT have been reported [3], [4], [5], [6], [7], [8], [9].
We herein report the case of a 75-year-old patient with ascending colon cancer and SIT who underwent laparoscopic hemicolectomy with radical lymphadenectomy. The technical differences between this case and cases with normal anatomy are described.
The work in this case has been reported in line with the SCARE criteria [10].
2. Presentation of case
A 75-year-old woman, known since early childhood to have SIT, was admitted to our hospital with a diagnosis of ascending colon cancer, according to colonoscopy, for further evaluation and surgical treatment. The patient had no medical history of abdominal surgery, and results from the general physical examination were normal. Laboratory examination confirmed no anemia or hepatic, renal, or electrolyte dysfunction. Serum carcinoembryonic antigen level and CA 19-9 level were not elevated.
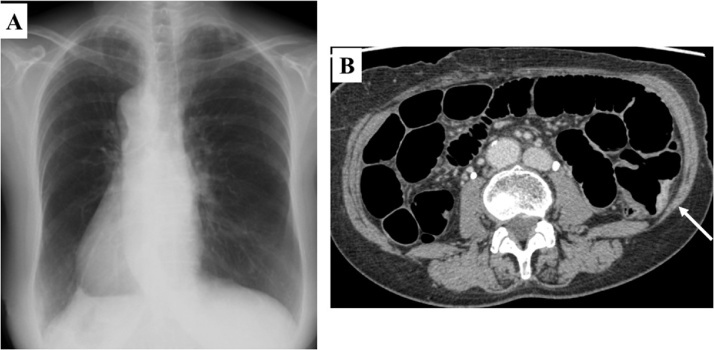
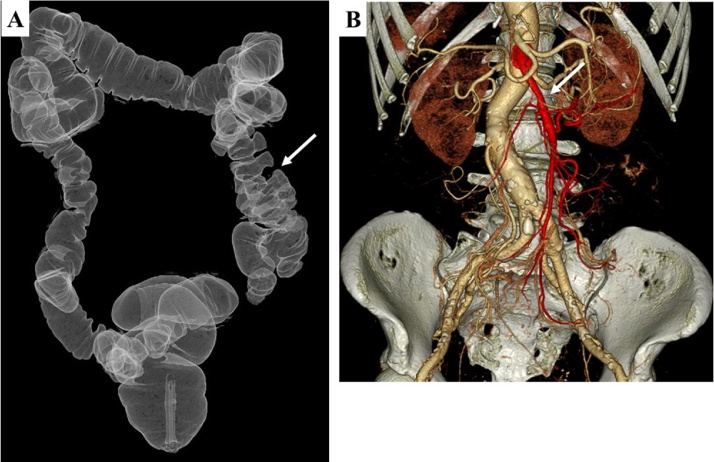
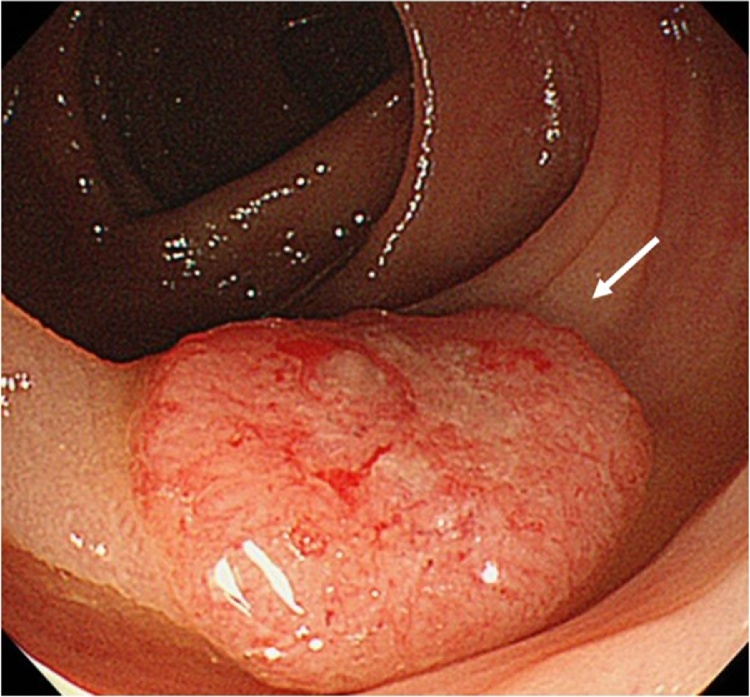
Chest radiography showed dextrocardia (Fig. 1A). Abdominal computed tomography (CT) revealed complete transposition of abdominal viscera, confirming SIT. CT and CT colonography showed a mass in the ascending colon and no evidence of distant metastasis (Figs. 1 B and 2 A ). CT angiography showed that the superior mesenteric artery was located on the left side (Fig. 2B). An ulcerated lesion in the ascending colon was observed by colonoscopy (Fig. 3). Biopsies from this lesion revealed moderately differentiated adenocarcinoma. Based on the above findings, laparoscopic hemicolectomy with radical lymphadenectomy was planned.
Fig. 1.
Chest radiography and abdominal computed tomography of the patient. (A) Chest radiography showing dextrocardia. (B) Abdominal computed tomography (CT) shows a mass in the ascending colon (arrow).
Fig. 2.
CT angiography and CT colonography. (A) Three-dimensional CT angiography shows the superior mesenteric artery, located on the right side (arrow). (B) CT-colonography shows a mass in the ascending colon.
Fig. 3.
Colonoscopy revealing an ulcerated lesion in the ascending colon (arrow).
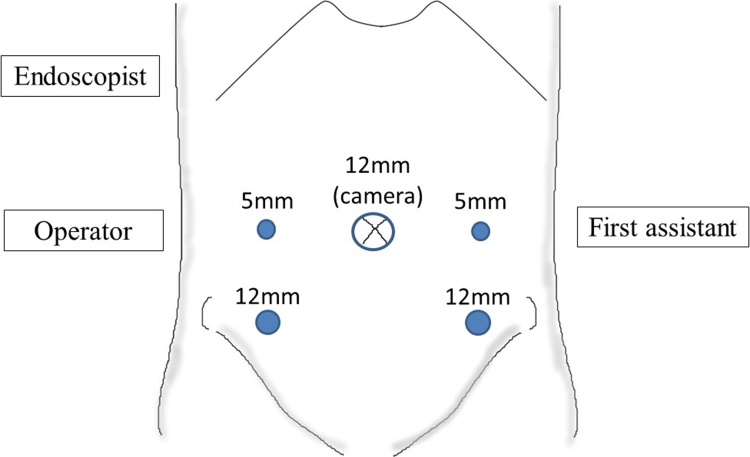
While under general anesthesia, the patient was placed in the lithotomy position with her head and right side down. The operating surgeon was situated on the right side of the patient (opposite to the usual for surgery), with the first assistant on the left, and the endoscopist on the right (Fig. 4). A camera was inserted into the abdomen through a 12-mm trocar at the umbilicus. Four additional trocars were placed. For the operating surgeon, a 12-mm trocar was placed in the right lower quadrant and a 5-mm trocar was placed in the right flank, and for the assistant, a 12-mm trocar was placed in the left lower quadrant and a 5-mm trocar was placed in the left flank (Fig. 4).
Fig. 4.
Location of surgeons and trocar placement in this patient with situs inversus totalis.
Upon commencement of the laparoscopy, the liver, the cecum and ascending colon were situated at the left, and the spleen on the right. The tumor was located in the ascending colon (Fig. 5A, B). First, the left-sided colon was mobilized using a medial approach. The mesentery was incised caudal to the ileocolic vessels, and the fusion fascia was mobilized, searching the anterior surface of the transverse portion of the duodenum. The ileocolic vessels were identified and divided after the superior mesenteric vein was exposed (Fig. 5C, D). Following mobilization of the ascending colon, dissection and reconstruction of the colon was performed using end-to-side anastomosis extracorporeally through a 2.5 cm skin incision continued to the umbilical port site. Operating time was 109 min and blood loss was 10 mL, similar to typical findings in orthotropic patients. Pathological findings showed a moderately differentiated adenocarcinoma measuring 1.4 × 1.2 cm, with invasion of the submucosa. In addition, 17 regional lymph nodes including one positive node were resected. The patient was discharged on the ninth postoperative day without any complications.
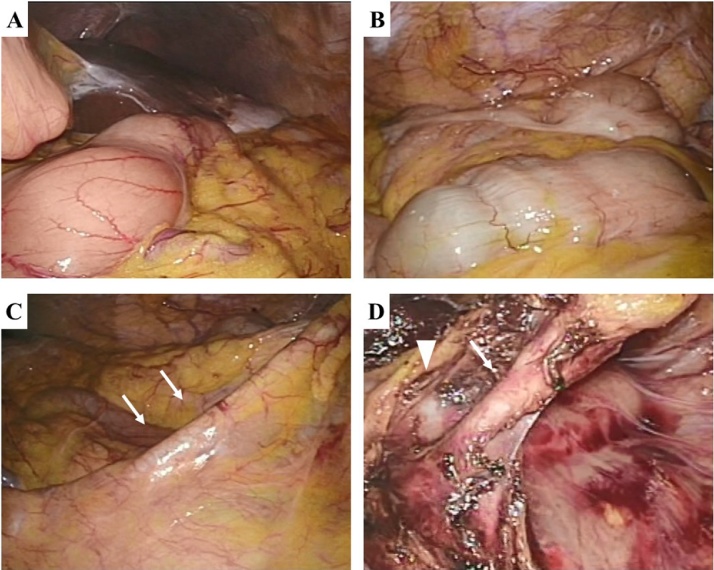
Fig. 5.
Intraoperative findings. (A)Right lobe of the liver and gallbladder are located in left upper quadrant. (B) The ascending colon is located on the left side. (C) The ileocolic vessels are identified (arrow). (D) The ileocolic vessels (arrow) and superior mesenteric vein (arrowhead) are identified.
3. Discussion
SIT is a rare congenital condition in which the structures of the abdominal and thoracic cavities are completely inverted. Cardiac and intestinal malformations, as well as other visceral and vascular anomalies associated with SIT, follow a variable pattern. Apart from genetic predisposition, no other etiology has been established, and SIT itself has no pathophysiologic significance. Congenital anomalies, such as syndromes of splenic anomalies (asplenia and polysplenia) and biliary atresia, have been reported to be common in patients with SIT [11]. With the radiologic modalities, diagnosis of SIT and concurrent anomalies has become relatively easy. However, not all anomalies are identified during radiologic evaluations, and unexpected conditions can sometime arise.
LCS was recently demonstrated to have several advantages for CRC treatment [12]. Thus, the laparoscopic approach has been used increasingly to treat CRC, as well as to correct anatomic anomalies. Several reports on surgical procedures document greater technical difficulties in SIT patients due to their abnormal anatomy. Laparoscopic procedures are considered especially more difficult in patients with SIT than in others because of the mirror-image anatomy. Because laparoscopic surgery in patients with SIT is very rare, it becomes a technical challenge for the surgeon; however, it has been performed more often in recent years, with most of these procedures being laparoscopic cholycystectomies [13]. A literature search for malignancy found only eight cases of LCS performed on patients with SIT (Table 1) [3], [4], [5], [6], [7], [8], [9]. Procedures were performed successfully in all eight cases with no reported complications. The authors of these reports suggested that LCS is a good option for patients with SIT, and emphasized that careful assessment and planning should be employed.
Table 1.
Reports of laparoscopic colorectal surgery for colorectal cancer in patients with situs inversus totalis.
| Operation | Author | Year | Operation time (min) | Blood loss (ml) | Complications |
|---|---|---|---|---|---|
| Laparoscopic ileocolectomy | Hirano et al. | 2015 | 125 | minimal | None |
| Laparoscopic hemicolectomy | Present case | 2017 | 109 | 10 | None |
| Sumi et al. | 2013 | 402a | 230a | None | |
| Kim et al. | 2011 | 119 | minimal | None | |
| Fujiwara et al. | 2007 | 191 | 60 | None | |
| Laparoscopic sigmoidectomy | Yaegashi et al. | 2015 | 189 | 13 | None |
| Laparoscopic low anterior resection | Huh et al. | 2010 | 250 | 120 | None |
| Laparoscopic abdominoperineal resection | Choi et al. | 2011 | 325 | 300 | None |
The operating time and blood loss were affected with the intra-abdominal adhesions after open distal gastrectomy.
To safely perform laparoscopic surgery, careful assessment of the anatomy using preoperative imaging is very important. Both CT angiography and CT colonography are useful for investigating anatomy and allowing preoperative planning of the laparoscopic procedure. At our institution, LCS is always performed using five ports. In the present case, the positions of the operating surgeon and the assistants were reversed from those of used for orthotopic patients. Furthermore, trocar positions were different from usual, and adjusted to those of a left-side CRC. In this case, the operating surgeon was right-handed; therefore, the procedure for ligation of the ileocolic vessels and mobilization of ascending colon was performed with the right hand, through a 12-mm trocar in the right lower quadrant. Oms et al. [14] reported a potential advantage for left-handed surgeons during laparoscopic procedures in patients with SIT. With respect to laparoscopic right hemicolectomy, it is clear that left-handed operation techniques are important, however, being a right-handed surgeon is not disadvantageous if positioning during surgery is modified as described here.
In the present case, due to thorough understanding of the anatomy using CT angiography and CT colonography and careful planning of surgical procedure, such as the location of surgeons and trocar placement, there were no differences in terms of the length of time for surgery or blood loss, in comparison to orthotopic patients.
4. Conclusion
We here present a patient with ascending colon cancer and SIT who underwent laparoscopic right hemicolectomy with radical lymphadenectomy. Laparoscopic surgery represents a technical challenge for the surgeon, but remains a good option for patients with SIT. Therefore, if care is taken to understand the mirror-image anatomy and preoperative planning of the laparoscopic procedure, LCS may be safe and feasible operation for patients with CRC and SIT.
Conflicts of interest
None of the authors have any disclosures or conflict of interests.
Funding
None.
Ethical approval
Because of the case report and we have a consent by the patient, the ehics committee was not held.
Consent
Written informed consent was obtained from the patient for publication of this case and any accompanying images.
Authors’ contributions
KS conceived of this case presentation and drafted the manuscript. HN, KK, KH, TK, TT, TK, KO, MK, EK, KM, and TW participated in the treatment of this case. All authors read and approved the final manuscript.
Registration of research studies
N/A.
Guarantor
Kazuhito Sasaki accepts the full responsibility for the article.
References
- 1.Mayo C.W., Rice R.G. Situs inversus totalis; a statistical review of data on 76 cases with special reference to disease of the biliary tract. Arch. Surg. 1949;58:724–730. [PubMed] [Google Scholar]
- 2.Varano N.R., Merklin R.J. Situs inversus: review of the literature, report of four cases and analysis of the clinical implications. J. Int. Coll. Surg. 1960;33:131–148. [PubMed] [Google Scholar]
- 3.Hirano Y., Hattori M., Douden K., Hashizume Y. Single-incision laparoscopic surgery for colon cancer in patient with situs inversus totalis: report of a case. Indian J. Surg. 2015;77:26–28. doi: 10.1007/s12262-014-1075-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sumi Y., Tomono A., Suzuki S., Kuroda D., Kakeji Y. Laparoscopic hemicolectomy in a patient with situs inversus totalis after open distal gastrectomy. World J. Gastrointest. Surg. 2013;5:22–26. doi: 10.4240/wjgs.v5.i2.22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kim H.J., Choi G.S., Park J.S., Lim K.H., Jang Y.S., Park S.Y. Laparoscopic right hemicolectomy with D3 lymph node dissection for a patient with situs inversus totalis: report of a case. Surg. Today. 2011;41:1538–1542. doi: 10.1007/s00595-010-4530-7. [DOI] [PubMed] [Google Scholar]
- 6.Fujiwara Y., Fukunaga Y., Higashino M., Tanimura S., Takemura M., Tanaka Y. Laparoscopic hemicolectomy in a patient with situs inversus totalis. World J. Gastroenterol. 2007;13:5035–5037. doi: 10.3748/wjg.v13.i37.5035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Yaegashi M., Kimura T., Sakamoto T., Sato T., Kawasaki Y., Otsuka K. Laparoscopic sigmoidectomy for a patient with situs inversus totalis: effect of changing operator position. Int. Surg. 2015;100:638–642. doi: 10.9738/INTSURG-D-14-00217.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Huh J.W., Kim H.R., Cho S.H., Kim C.Y., Kim H.J., Joo J.K. Laparoscopic total mesorectal excision in a rectal cancer patient with situs inversus totalis. J. Korean Med. Sci. 2010;25:790–793. doi: 10.3346/jkms.2010.25.5.790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Choi S.I., Park S.J., Kang B.M., Lee K.Y., Lee H.C., Lee S.H. Laparoscopic abdominoperineal resection for rectal cancer in a patient with situs inversus totalis. Surg. Laparosc. Endosc. Percutan. Tech. 2011;21:e87–e90. doi: 10.1097/SLE.0b013e31820b0258. [DOI] [PubMed] [Google Scholar]
- 10.Agha R.A., Fowler A.J., Saetta A., Barai I., Rajmohan S., Orgill D.P., for the SCARE Group The SCARE Statement: consensus-based surgical case report guidelines. Int. J. Surg. 2016;34:180–186. doi: 10.1016/j.ijsu.2016.08.014. [DOI] [PubMed] [Google Scholar]
- 11.Iwamura T., Shibata N., Haraguchi Y., Hisashi Y., Nishikawa T., Yamada H. Synchronous double cancer of the stomach and rectum with situs inversus totalis and polysplenia syndrome. J. Clin. Gastroenterol. 2001;33:148–153. doi: 10.1097/00004836-200108000-00012. [DOI] [PubMed] [Google Scholar]
- 12.Lee W.J., Chan C.P., Wang B.Y. Recent advances in laparoscopic surgery. Asian J. Endosc. Surg. 2013;6:1–8. doi: 10.1111/ases.12001. [DOI] [PubMed] [Google Scholar]
- 13.Deguchi Y., Mitamura K., Omotaka S., Eguchi J., Sakuma D., Sato M. Single-incision cholecystectomy in a patient with situs inversus totalis presenting with cholelithiasis: a case report. Asian J. Endosc. Surg. 2015;8:347–349. doi: 10.1111/ases.12180. [DOI] [PubMed] [Google Scholar]
- 14.Oms L.M., Badia J.M. Laparoscopic cholecystectomy in situs inversus totalis: the importance of being left-handed. Surg. Endosc. 2013;17:1859–1861. doi: 10.1007/s00464-003-9051-7. [DOI] [PubMed] [Google Scholar]