Abstract
INTRODUCTION:
Hospital care transformation plan (HCTP) was implemented, in 2014, with the aim of ensuring all Iranians have fair access to hospital care, mainly in the public sector. It was assumed that HCTP would lead to increased quality and effectiveness of health care in public hospitals. To explore whether HCTP has achieved its aim, this study has investigated the impact of this plan on performance indicators (PIs) of the public hospitals.
MATERIALS AND METHODS:
This cross-sectional descriptive study was conducted in 2016. The study population included all hospitals in the Isfahan City. Data (10 selected PIs) were collected through formal reports which were available at the Isfahan University of Medical Sciences and analyzed using Statistical Package for Social Sciences (version 17). The statistical significant level analysis was 0.05.
RESULTS:
After HCTP, it was shown an increase of (1) Bed occupancy, bed turnover, occupied bed-days, inpatients visits, and number of surgeries in all types of hospitals, (2) Outpatients’ visits in all hospitals except private ones, (3) Emergency visits in public and social security hospitals, and (4) Natural deliveries in public and semi-public hospitals. Furthermore, the average length of stay and hospital mortality rate has decreased in all types of hospitals after HCTP implementation.
DISCUSSION AND CONCLUSION:
Although, improving PIs of hospitals were not directly stated and known objectives of HCTP implementation, it seems HCTP could improve the performance of all hospitals, including involved and noninvolved ones.
Keywords: Health care reform, hospitals, process assessment (health care), program evaluation
Introduction
Nowadays, the promotion, maintenance, and extension of health are the most basic and the key policies to ensure and improve the social equity in countries. Since a healthy person is the center of sustainable development and also health is perquisite for human beings to utilize the benefits of development, attention to health, and achieving health goals has been always considered national and international priority.[1] The health issue is a multi-dimensional subject which is affected by various elements. Among all these elements, the necessity of having the effective and well-being health system has the particular importance to develop justice, providing physical and mental opportunities for increasing and promoting health in society.[2]
According to the World Health Organization's definition, a health system includes all organizations, institutions, and resources which present or provide health services. Like every society systems, a health system works in the environment that changes regularly, and its stability is threatened every day. Survival in such environment requires making suitable reforms and improvements in the health system given to the conditions. Health reforms are dynamic, continuous, and permanent[3] and the health system steady moves toward the improvement itself in the light of developing systems of continuous quality.[4] In addition, increasing the costs of the health sector, the growth of people's expectations, the limited capacity of resources, uncertainty toward traditional approaches, inefficient use of limited resources, and inadequate access to necessary health care are key motivators that make the health reforms unavoidable.[5] Health reforms are the most strategic issues that have been the main focus of all governments worldwide. They contain long-lasting and targeted changes for increasing access to medical services, improving the quality of care, and controlling the growth of costs.[6] Our review of the literature shows that in the recent decades health system in different countries including developed and developing countries has been experiencing various reforms.[4,7,8,9,10,11] Although the goals and contents of these reforms are different, regarding the country's context, the crux, for all countries, is to satisfy the health demands and new expectations.
The health system of Iran has also experienced many reforms in its different levels of service provision.[12] The formation of regional health care organizations, setting up the country's health care networks, medical education integration, hospitals and medical centers autonomy plan, family physician plan, hospital management economic reform plan, and accreditation of treatment centers plan are examples of Iran's important reforms in the health system which have resulted in remarkable health improvements.[13] Its newest reform, since 2013, has been the health transformation plan (HTP). HTP has included different programs and interventions in the field of both primary and hospital cares and implemented through a gradual, step-by-step process.
One of the main parts of HTP covers public hospital care and has been effective since May 5, 2014. This part, hospital care transformation plan (HCTP), had seven programs, each with the aim of increasing fair access to hospital care. These programs were out-of-pocket payment reduction for in-patient services, practitioners’ retention in remote areas, overnight specialist cover in hospitals, improving the quality of outpatient visits (OVs), improving hoteling and ward upgrades, financial protection of incurable, specific and poor patients and promoting natural delivery.[14] HCTP was mainly focused on the performance of hospitals. However, the effects of these interventions on hospitals’ performance had not been evaluated yet. Therefore, it seemed necessary to conduct a quantitative study to evaluate this plan. Such study would give quantifiable information about the effects of the project and would also aid in visualizing the current situation which could lead to the effectiveness, efficiency, and expected productivity. The current analysis aims to compare the performance indicators (PIs) of all types of hospitals (both involved and noninvolved), before and after implementation of HCTP.
Materials and Methods
This cross-sectional analytic-descriptive study was conducted in 2016. All hospitals of Isfahan city in Iran were included in the study as the sample population, including 54 hospitals (public hospitals: 35, private hospitals: 6, social security hospitals: 3, semi-public hospitals: 10). Data included ten PIs of hospitals that were selected on the basis of inclusion criteria. These were (1) Relativeness, (2) Availability, (3) Accessibility, (4) Time period; that was 4 months before and after intervention in 2015 with respect to the same time interval of 2014. The ten PIs that were observed were as follows: Bed occupancy rate (BOR), average length of stay (ALOS), bed turnover ratio (BTR), occupied bed-days (OBD), in-patient visits (IVs), Out-patient visits (OVs), emergency visits (EVs), hospital mortality rate (HMR), number of surgeries (NOS), and Natural Delivery Portion (NDP). These performance indicators were measured after receiving ethical permission through reviewing the formal reports of hospital performance which were available in statistic departments of the university and hospitals. The intervention refers to HCTP which had focused on hospitals cares and implemented since May 5, 2015. The data were analyzed using Statistical Package for Social Sciences (SPSS Inc., Chicago, IL, USA) version 17 for Windows, whereas the significant level analysis was a solid 0.05.
Results
The mean period for selected PIs of hospitals was 4 months; before and after intervention in 2015 with respect to the same time interval of 2014 as shown in Table 1. According to this table, before and after HCTP, the mean of BOR was 62.79 and 68.5, ALOS was 2.82 and 2.65, BTR was 6.7 and 8, OBD was 116,405 and 130,804, IVs was 39,791 and 46,463, OVs 606,068 and 639,086, EVs was 125,185 and 127,910, HMR was 13.2 and 11.1, NOS was 17,388 and 21,097 and NDP was 34 and 38, respectively.
Table 1.
Performance indicators of hospitals before and after intervention
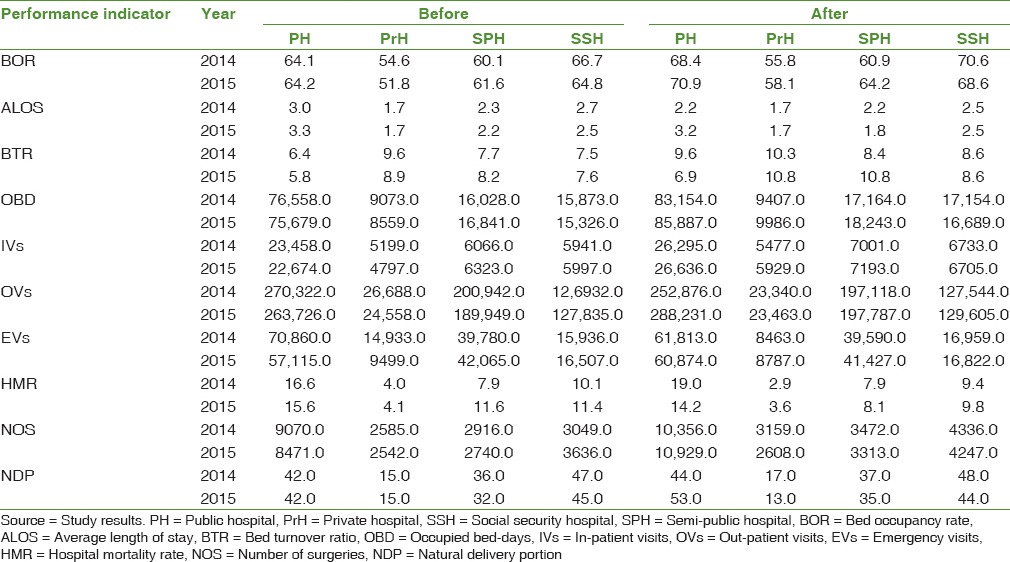
In addition, comparison of these selected PIs of hospitals before and after intervention in 2015 with respect to the same interval of 2014 displayed that BOR, BTR, OBD, IVs and NOS have increased in all types of hospitals. Except in private hospitals, OVs also had an increase in other types of hospitals. The increase of EVs only was shown in public and social security hospitals. Finally, the public and semi-public hospitals have experienced an increase of the NDP. The highest and lowest increase of BOR, OBD and IVs were, respectively, shown in private and social security hospitals. Semi-public and public hospitals had highest and lowest increase of BTR. OVs, EVs, and NOS had highest increase in public hospitals and lowest increase in social security hospitals. The highest and lowest increase of NDP was also related to public and semi-public hospitals, respectively. Furthermore, the results disclosed that ALOS and HMR have decreased in all types of hospitals after HCTP implementation. The highest and lowest decrease of ALOS was, respectively, shown in semi-public and public hospitals. HMR also had highest decrease in public hospitals and lowest decrease in semi-public hospitals.
Discussion
It is recommended that hospitals managers and authorities should always be aware of changes and interventions for better health care provision to progress the services and the overall outcome. This awareness will lead them to plan for future development and achieve organization's excellence. Implementation of HCTP is a major health reform; one that hospitals’ managers should, especially, be notified of its impacts on their system's performance. With this necessity in mind, this study aimed to compare selected PIs of hospitals before and after the implementation of HCTP.
The first finding of this study was related to the three PIs including BOR, ALOS, and BTR. As stated in the literature, these PIs are the main indicators of hospital efficiency.[15] Regarding the results of this study (an increase of BOR, ALOS, and BTR), it seems that the HCTP implementation in public hospitals could improve hospital efficiency, although, this was not stated as the goals of HCTP.[16] It should not be ignored that to have a precise measurement of hospital efficiency, there is a need to conduct thorough econometrics studies, which make it easier to monitor and evaluate the efficiency of the changes. However, a simple rule of thumb given by the three mentioned indicators can easily show the efficiency improvement. This progress is justifiable in regard to the included interventions of the HCTP. These interventions included some actions that only increase the public hospitals’ inputs (e.g., financial resources and workforce), marginally. With such a limited increase in the inputs, these hospitals could provide the opportunity of better health care utilizations, especially for those people who are unable to pay for their health care due to financial constraints. Furthermore, some of the interventions focused on measures to improve the quality of health care in public hospitals (e.g., increasing overnight specialist cover, availability of pharmacy, consumable, medical devices, and surgical equipment, regarding hospital nutrition and hoteling/ward upgrades). These interventions led to improved willingness of people to come to these hospitals. Hence, all these changes have increased the output of public hospitals while altering their status from the nonefficient to efficient ones. There is a striking contrast between the outcome of public hospitals’ performance before and after the implementation of the HCTP, according to formal reports and documents.[16,17] These contrasts have cemented the result of this study with respect to the previous evidence.
It is worth mentioning that not only in the public hospitals but also in other types of hospitals, even those, which were not invovled in HCTP, similar improvements such as increased efficiency have been observed. This is very much predictable in a dynamic setting such as the health system,[18] in which a change in one part may effect and alter another part. Hence, some HCTP's actions, especially related to ensuring population intervention, helped to overcome the obstacles to utilize health care, resulting in more patients’ visits. This dramatic increase happened when the capacity of public hospitals did not change very much and they could not be able to respond adequately. Hence, now patients, who had a basic health insurance, would slant to other hospitals, which were not included in the HCTP. These hospitals did not have any additional inputs while they encountered more patients and experienced more outputs. This helped them to increase their efficiency and productivity. There is sparse evidence about the performance changes in noninvolved HCTP hospitals and this made it difficult to compare our findings with other studies. It is advisable to conduct more studies in these hospitals to draw a clear picture of HCTP evaluation.
Another finding of the present study demonstrated an increase in the main outputs of public hospitals including OBD, IVs, OVs, EVs, and NOS, which is in line with previous studies.[16] This increase is justifiable given those HCTP actions, which focus mainly on inpatient services and to some extent on out-patient services. However, it should be noted that such increase in outputs may show either more health care utilization or more induced health demands; the former is desirable while the latter is undesirable. Drawing on different national reports in the area of health care utilization,[17,19] before implementing HCTP, it has been reported that health care was underutilized, but this increase should not be misinterpreted as an increase in health care demand. Instead, it is a sign of more health care coverage. However, it is beyond the scope of this study to conclude whether HCTP has raised the induced demands for health care. There is a need to conduct another study to explore this issue in detail. Similar to the previous finding, the output increase was observed in other types of hospitals, too, which again relates to the dynamic nature of the health system.
A decrease of HMR was another interesting finding, showing the quality of hospital care. According to our study, post-HCTP, the health status of the covered population had not changed a lot, and this attribute could not be related to health improvement. After HCTP, most of the hospitals experienced the increasing of the workload, and there was a concern that this high workload threatens the quality of care. However, our evidence of HMR showed that, fortunately, high workload had not overshadowed the quality of hospital care.
The last finding of our study refers to the increase of the NDP, which was under the effect of the HCTP intervention. Considering the national reports and available evidence,[20,21] it can be argued that, Iran was previously challenged by the high number of cesarean sections. The HCTP interventions, and consequently promotion of natural childbirth can be considered levers to overcome high frequency of cesarean.
Conclusion
HCTP in Iran was implemented as a reform to accelerate achieving universal health coverage. The main goals of this plan were improving fair access to hospital care and improving the quality of health care. Given the important roles of monitoring and evaluation of this reform as well as the alignment of hospital performance with the overall mentioned goals, we studied PIs of hospitals before and after the implementation of HCTP. With our study findings in mind, it seems that HCTP could improve the PIs of hospitals, both involved and noninvolved. However, this study has its own limitations such as the time period, selected PIs, and quantitative design. Therefore, it is advisable to conduct more in-depth studies in the areas of hospital efficiency (by using more economic approaches) and eliciting managers’ perspective toward HCTP's by adopting qualitative approaches.
Financial support and sponsorship
Isfahan University of Medical Sciences, Isfahan, Iran (grant number: 194019).
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
The authors gratefully acknowledge the reviewers for their comments.
References
- 1.World Health Organization. World Health Statistics 2016: Monitoring Health for the SDGs, Sustainable Development Goals. Geneva: WHO Press; 2016. [Google Scholar]
- 2.World Health Organization. The World Health Report 2000: Health Systems: Improving Performance. Geneva: World Health Organization; 2000. [Google Scholar]
- 3.Frenk J. The global health system: Strengthening national health systems as the next step for global progress. PLoS Med. 2010;7:e1000089. doi: 10.1371/journal.pmed.1000089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.McDonough JE. Health system reform in the United States. Int J Health Policy Manag. 2013;2:5–8. doi: 10.15171/ijhpm.2014.02. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Roberts M, Hsiao W, Berman P, Reich M. Getting Health Reform Right: A Guide to Improving Performance and Equity. Oxford, New York: Oxford University Press; 2003. [Google Scholar]
- 6.Dentzer S. The ‘triple aim’ goes global, and not a minute too soon. Health Aff (Millwood) 2013;32:638. doi: 10.1377/hlthaff.2013.0274. [DOI] [PubMed] [Google Scholar]
- 7.Atun R, de Andrade LO, Almeida G, Cotlear D, Dmytraczenko T, Frenz P, et al. Health-system reform and universal health coverage in Latin America. Lancet. 2015;385:1230–47. doi: 10.1016/S0140-6736(14)61646-9. [DOI] [PubMed] [Google Scholar]
- 8.Frenk J, González-Pier E, Gómez-Dantés O, Lezana MA, Knaul FM. Comprehensive reform to improve health system performance in Mexico. Lancet. 2006;368:1524–34. doi: 10.1016/S0140-6736(06)69564-0. [DOI] [PubMed] [Google Scholar]
- 9.Limwattananon S, Neelsen S, O’Donnell O, Prakongsai P, Tangcharoensathien V, Van Doorslaer E, et al. Universal coverage with supply-side reform: The impact on medical expenditure risk and utilization in Thailand. J Public Econ. 2015;121:79–94. [Google Scholar]
- 10.Marten R, McIntyre D, Travassos C, Shishkin S, Longde W, Reddy S, et al. An assessment of progress towards universal health coverage in Brazil, Russia, India, China, and South Africa (BRICS) Lancet. 2014;384:2164–71. doi: 10.1016/S0140-6736(14)60075-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Yasar GY. ‘Health transformation programme’ in Turkey: An assessment. Int J Health Plann Manage. 2011;26:110–33. doi: 10.1002/hpm.1065. [DOI] [PubMed] [Google Scholar]
- 12.World Bank. Islamic Republic of Iran: Health Sector Review: Volume I. Washington DC: Word Bank; 2008. [Google Scholar]
- 13.Lankarani KB, Alavian SM, Peymani P. Health in the Islamic Republic of Iran, challenges and progresses. Med J Islam Repub Iran. 2013;27:42–9. [PMC free article] [PubMed] [Google Scholar]
- 14.Moradi-Lakeh M, Vosoogh-Moghaddam A. Health sector evolution plan in Iran; equity and sustainability concerns. Int J Health Policy Manag. 2015;4:637–40. doi: 10.15171/ijhpm.2015.160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sajjadi H, Sajjadi Z, Hadi M. Is there a method for the simultaneous comparison of key hospital performance indicators? Health Inf Manage. 2011;8:71–81. [Google Scholar]
- 16.Ministry of Health and Medical Education. Evaluation of health transportation plan of Iran. Tehran: Ministry of Health and Medical Education; 2015. [Google Scholar]
- 17.Rezaei Z, Akbari A, Saba R. Utilization of health care in Iran. Tehran: National Institute of Health Research; 2015. [Google Scholar]
- 18.Koelling P, Schwandt MJ. Health systems: A dynamic system-benefits from system dynamics. Proceedings of the 37th Conference on Winter Simulation. Orlando, Florida: 2005. Dec 04-07, [Google Scholar]
- 19.Iranian Health Insurance Organization. The formal report of performance evaluation of Iranian Health Insurance Organization. Tehran: Iranian Health Insurance Organization; 2014. [Google Scholar]
- 20.Shahshahan Z, Heshmati B, Akbari M, Sabet F. Caesarean section in Iran. Lancet. 2016;388:29–30. doi: 10.1016/S0140-6736(16)30899-6. [DOI] [PubMed] [Google Scholar]
- 21.Sepanlou SG, Akbarian A. Growing rate of cesarean section in Iran: Dimensions and concerns. Arch Iran Med. 2012;15:2–3. [PubMed] [Google Scholar]


