ABSTRACT
Ebolaviruses have a surface glycoprotein (GP1,2) that is required for virus attachment and entry into cells. Mutations affecting GP1,2 functions can alter virus growth properties. We generated a recombinant vesicular stomatitis virus encoding Ebola virus Makona variant GP1,2 (rVSV-MAK-GP) and observed emergence of a T544I mutation in the Makona GP1,2 gene during tissue culture passage in certain cell lines. The T544I mutation emerged within two passages when VSV-MAK-GP was grown on Vero E6, Vero, and BS-C-1 cells but not when it was passaged on Huh7 and HepG2 cells. The mutation led to a marked increase in virus growth kinetics and conferred a robust growth advantage over wild-type rVSV-MAK-GP on Vero E6 cells. Analysis of complete viral genomes collected from patients in western Africa indicated that this mutation was not found in Ebola virus clinical samples. However, we observed the emergence of T544I during serial passage of various Ebola Makona isolates on Vero E6 cells. Three independent isolates showed emergence of T544I from undetectable levels in nonpassaged virus or virus passaged once to frequencies of greater than 60% within a single passage, consistent with it being a tissue culture adaptation. Intriguingly, T544I is not found in any Sudan, Bundibugyo, or Tai Forest ebolavirus sequences. Furthermore, T544I did not emerge when we serially passaged recombinant VSV encoding GP1,2 from these ebolaviruses. This report provides experimental evidence that the spontaneous mutation T544I is a tissue culture adaptation in certain cell lines and that it may be unique for the species Zaire ebolavirus.
IMPORTANCE The Ebola virus (Zaire) species is the most lethal species of all ebolaviruses in terms of mortality rate and number of deaths. Understanding how the Ebola virus surface glycoprotein functions to facilitate entry in cells is an area of intense research. Recently, three groups independently identified a polymorphism in the Ebola glycoprotein (I544) that enhanced virus entry, but they did not agree in their conclusions regarding its impact on pathogenesis. Our findings here address the origins of this polymorphism and provide experimental evidence showing that it is the result of a spontaneous mutation (T544I) specific to tissue culture conditions, suggesting that it has no role in pathogenesis. We further show that this mutation may be unique to the species Zaire ebolavirus, as it does not occur in Sudan, Bundibugyo, and Tai Forest ebolaviruses. Understanding the mechanism behind this mutation can provide insight into functional differences that exist in culture conditions and among ebolavirus glycoproteins.
KEYWORDS: Ebola virus, Sudan ebolavirus, Bundibugyo ebolavirus, Tai Forest ebolavirus, glycoproteins, tissue culture, mutation, adaptation, virus entry, membrane fusion, tissue culture mutation
INTRODUCTION
Ebolaviruses (family Filoviridae, genus Ebolavirus) cause severe hemorrhagic fever in humans, often with high mortality rates (40 to 90%). Historically, outbreaks ranging from a few patients to hundreds occurred sporadically in central Africa. The 2013-2016 Ebola virus disease (EVD) outbreak in West Africa changed this. Caused by the Makona variant of the Ebola virus (EBOV), species Zaire ebolavirus, the outbreak was unprecedented in size, with nearly 29,000 suspected cases and over 11,000 deaths (1).
Ebolaviruses have nonsegmented negative-strand RNA genomes (19 kb) that carry seven genes. Of these, the most extensively studied gene product is the glycoprotein (GP1,2) on the virion surface, given its association with pathogenesis. EBOV GP1,2 has an important role in virus infection, as it functions in virus attachment and entry into the host cell. GP1,2 is synthesized as a 676-amino-acid precursor that is then cleaved by the host protease furin to create two subunits, GP1 and GP2. These subunits are linked by a disulfide bond to form a GP1,2 heterodimer. Membrane-associated GP1,2 is a trimer of the GP1,2 heterodimer. The GP1 subunit contains the conserved entry receptor binding site which binds to Niemann-Pick C1 (2). It also contains two heavily glycosylated domains known as the glycan cap and mucin-like domain (MLD). The GP2 subunit contains the putative internal fusion loop that induces fusion of the viral and cellular membranes. GP2 also contains the transmembrane domain that anchors the GP1,2 heterodimer into the virion membrane.
The ebolavirus GP1,2 shows significant sequence difference between species and species variants. Most of the amino acid changes that have been noted when comparing different species and different outbreak variants are positioned in the glycan cap and MLD, although mutations do occur in other regions of GP1,2, some of which have been shown to enhance virus entry. During the 2013-2016 West African outbreak, several substitutions occurred within the Makona variant GP1,2. A mutation in GP1, A82V, appeared early in the outbreak and became fixed in the virus population. A82V was shown to increase infectivity in cell-based assays and has been suggested to have led to increased viral pathogenicity (3, 4).
The amino acid position 544 has also been suggested to play a significant role in pathogenesis. Several recent publications have shown that there is heterogeneity at position 544, with some sequences coding for a threonine (T544) and others coding for an isoleucine (I544). There have been several different explanations for this heterogeneity. One study has suggested that GP1,2 containing I544 rather than T544 appeared during the EBOV Mayinga, Kikwit, and Makona outbreaks and was associated with increased disease progression and death (5). A second study suggested that the I544/T544 polymorphism might be implicated in human-to-human transmission (6). A third report suggests that the I544 residue was a tissue culture adaptation, but that study was unable to determine whether this appearance was a mutation or an outgrowth of an I544 population circulating in patients that became dominant upon growth in culture (7).
To investigate the potential that the polymorphism at position 544 was driven by cell culture adaptation, we generated a recombinant vesicular stomatitis virus (VSV) carrying the Makona GP1,2 gene (rVSV-MAK-GP). The resulting virus was replication competent and could be used to investigate adaptive mutations in GP1,2 in response to evolutionary pressures. Upon recovery of this virus, we identified plaque isolate clones that acquired the T544I mutation in the Makona GP1,2 within a small number of passages. Viruses that encoded this mutation quickly outcompeted wild-type (wt) viruses when mixed together in tissue culture. We also showed the emergence and dominance of this mutation during serial passage of three distinct Makona isolates in tissue culture. Interestingly, this mutation is not found in any deposited sequences for Sudan, Bundibugyo, or Tai Forest ebolaviruses, nor did we observe the mutation to appear during serial passage of recombinant VSV encoding GP1,2 from these species. These findings provide experimental evidence supporting that T544I is an adaptive response to tissue culture growth of only Zaire species ebolaviruses. These findings demonstrate that T544I is a mutation that is not present in natural EBOV infections but is strongly advantageous and selected for in commonly used tissue culture cells and is present in many EBOV stocks used in animal model studies. Further work is needed to understand how this mutation impacts the efficacy of EBOV infection in animal models or vaccine efficacy in the VSV-based EBOV vaccine.
RESULTS
Isolation of spontaneous VSV-MAK-GP clones encoding the GP1,2 T544I mutation.
To understand potential evolutionary pressures on the EBOV MAK GP1,2, we generated a recombinant VSV carrying the Makona GP1,2 gene in place of the VSV glycoprotein gene (rVSV-MAK-GP) (8, 9). The GP1,2 sequence from EBOV Makona (GenBank accession no. AHX24658.2) was used. It is derived from one of the first reported fatal cases (patient C07) from Guéckédou, Guinea (10). The C07 GP1,2 gene sequence was cloned into a plasmid carrying the VSV-ΔG genome between the matrix gene (M) and the large polymerase gene (L) and under the control of VSV transcription initiation and termination sequences (Fig. 1A).
FIG 1.
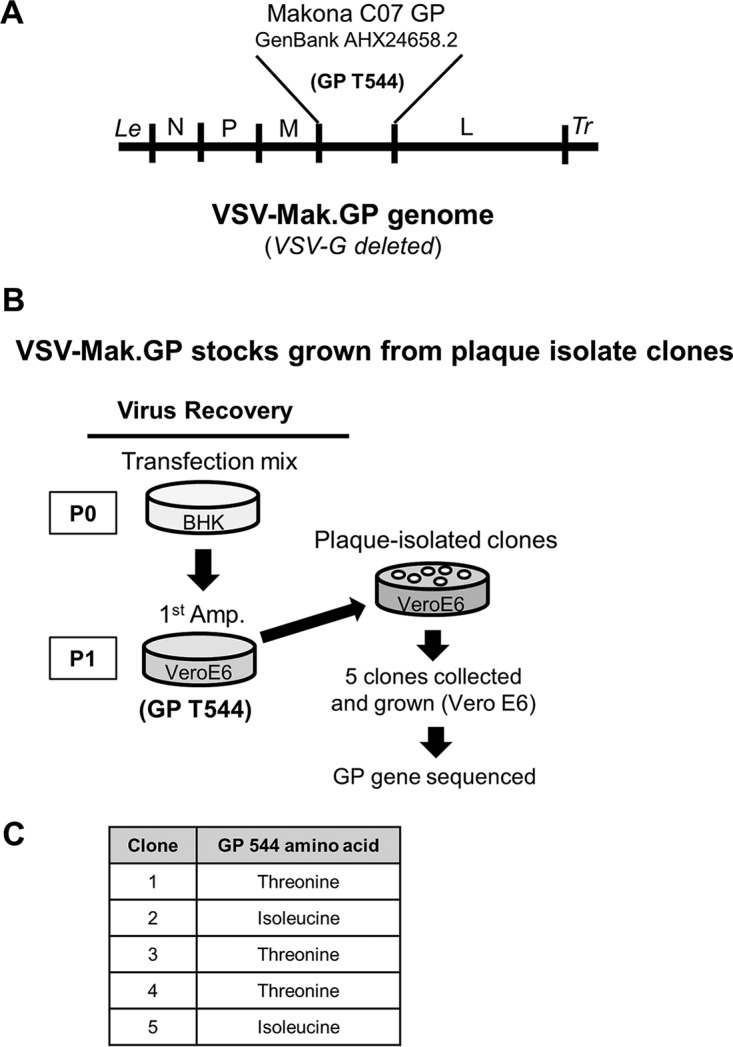
Genetic engineering and recovery of rVSV-MAK-GP virus clones that acquired the T544I mutation in the Makona GP1,2 gene. (A) Depiction of the VSV genome showing gene substitution of the VSV glycoprotein gene with the Makona GP1,2 gene, which encodes a T544 residue. (B) Schematic showing the workflow for generating rVSV-MAK-GP plaque isolate clones. Recovered virus in the P1 supernatant was confirmed by Sanger sequencing to encode the T544 residue in Makona GP1,2, as indicated in parentheses. (C) Residues encoded at position 544 of the Makona GP gene contained in the genomes of five rVSV-MAK-GP plaque isolate clones. cDNA was synthesized from virus genomes and sequenced by the Sanger method.
Replicating virus was recovered from the VSV-ΔG-MAK-GP full-length cDNA. Recovery showed lower efficiency than recovery using a wild-type VSV cDNA (1 of 5 independent attempts for VSV-MAK-GP versus 2 of 4 independent attempts for wt-VSV-dsRed). The appearance of cytopathic effect (CPE) in Vero E6 cells, an indicator of successful recovery of rVSV-MAK-GP, was not observed until ∼72 h of amplification (P1). The P1 supernatant was harvested at 96 h, when most of the cells showed CPE. Five plaque-isolated clones were collected from the P1 supernatant and grown on Vero E6 cells (Fig. 1B). The GP1,2 gene was sequenced (Sanger method) for each clone growth stock. This sequencing showed that two of the clones (2 and 5) contained a single point mutation. This mutation was a T544I mutation (Fig. 1C).
The T544I mutation in Makona GP1,2 leads to an increase in rVSV-MAK-GP growth kinetics.
To determine if the T544I mutation affected the growth characteristics of rVSV-Mak-GP, VeroE6 cells were infected with the rVSV-MAK-GP wild-type T544 or T544I mutant at a multiplicity of infection (MOI) of 5. Growth was monitored through observation of CPE, immunofluorescent labeling, and virus titration by plaque assay. Differences were visible, as cells infected with the T544I mutant repeatedly showed signs of CPE earlier than those infected by the wild type (T544). At 9 h postinfection (hpi), cells infected with T544I mutant showed widespread CPE across cell monolayers, whereas little to no CPE was observed in cell monolayers infected with wt GP1,2-expressing rVSV at the same time point (Fig. 2A, upper panels). Cell monolayers infected with wt GP1,2-expressing rVSV began to show increased CPE at 16 hpi; however, the spread of CPE was less apparent than that observed in cell monolayers infected with the T544I mutant. By 24 hpi, nearly all the cells in the T544I infection showed rounding and were detached from the plate, whereas about half of the cells in the wt infection were still attached and showed no cell rounding (Fig. 2A, lower panels). Infection of the full monolayer by wt virus, where most cells were rounded and detached, was not observed until ∼45 hpi.
FIG 2.
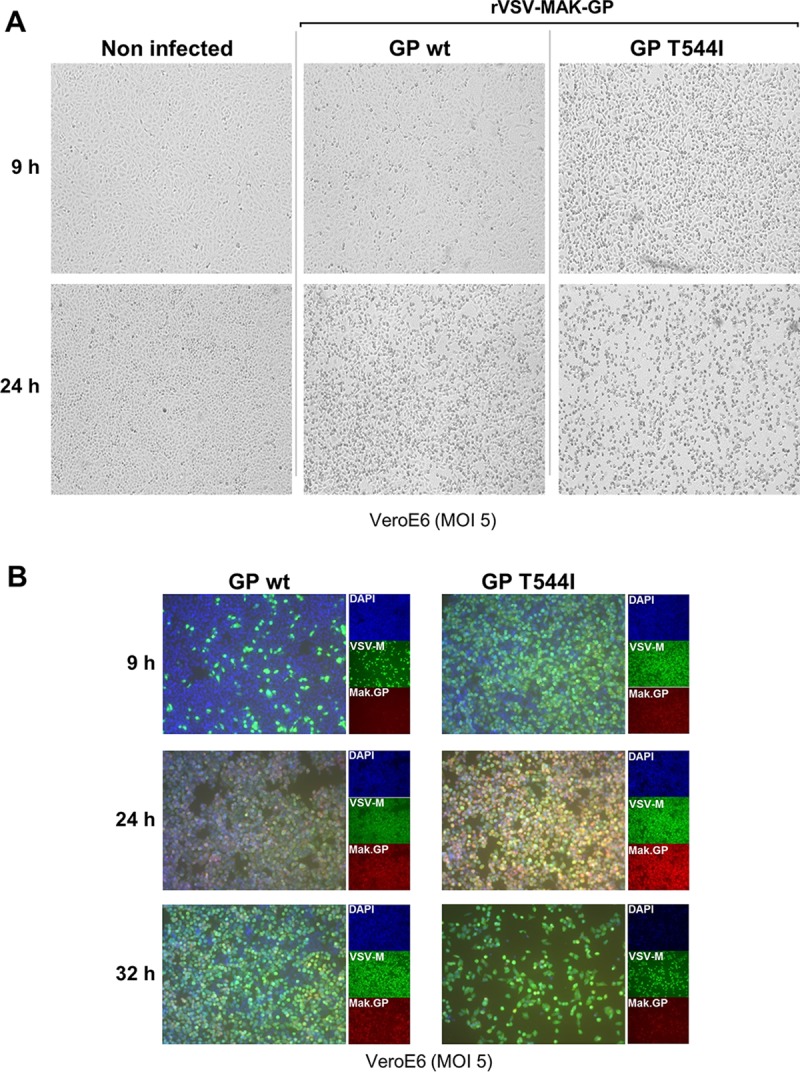
Phenotypic differences between rVSV-MAK-GP and mutant rVSV-MAK-GP T544I viruses. (A) Cells infected with mutant rVSV-MAK-GP show more rapid induction of CPE than cells infected by the wild type. Vero E6 cells were infected at a multiplicity of infection (MOI) of 5 and imaged by bright-field microscopy at the indicated times. Images are representative of the monolayer. (B) Immunofluorescence staining showing more rapid viral protein expression in cells infected with the mutant rVSV-MAK-GP T544I virus. Vero E6 cells infected at an MOI of 5 were stained at the indicated times for VSV M protein, Makona GP1,2 protein, and nuclei (4′,6′-diamidino-2-phenylindole [DAPI]). The large boxes show merged images, and the smaller boxes show separate channels. Images were captured with a 10× objective under identical exposure settings.
To investigate whether the slower appearance of CPE in the wt infection was due to these cells displaying a different CPE than T544I infected cells or whether there was a difference in virus infection/gene expression between the two viruses, cells were infected (MOI of 5), permeabilized, and analyzed by immunofluorescence. Cells were stained with an antibody against EBOV GP1,2 and an antibody against the VSV M protein to identify cells expressing these proteins. At 9 hpi, most cells infected by the T544I mutant expressed abundant amounts of M and GP1,2 protein (Fig. 2B, upper right panel). In contrast, only a small percentage of cells infected by wt virus expressed M and GP1,2 at this time, despite the high multiplicity of infection (Fig. 2B, upper left panel). Most cells in the wt infection did show M and GP1,2 expression by 24 hpi; however, the intensity of staining was markedly less than that of T544I at the same time point (Fig. 2B, middle panels). By 32 h, most cells in the T544I infection detached from the surface (Fig. 2B, lower right panel), whereas most cells in the wt infection remained attached (Fig. 2B, lower left panel), and their M and GP1,2 staining intensities were similar to those seen at 24 h for T544I. These observations suggest that cells in the wt infection were infected and/or showed virus gene expression at a lower rate that those infected by T544I mutant. This difference in CPE correlated with differences in overall virus growth. Repeated experiments showed that T544I titers were ∼2 logs higher than wt titers at 8 hpi and ∼5-fold higher than wt titers at 24 hpi (Fig. 3A); wt titers eventually reached a level comparable to those of T544I (less than 2-fold) at 32 hpi.
FIG 3.
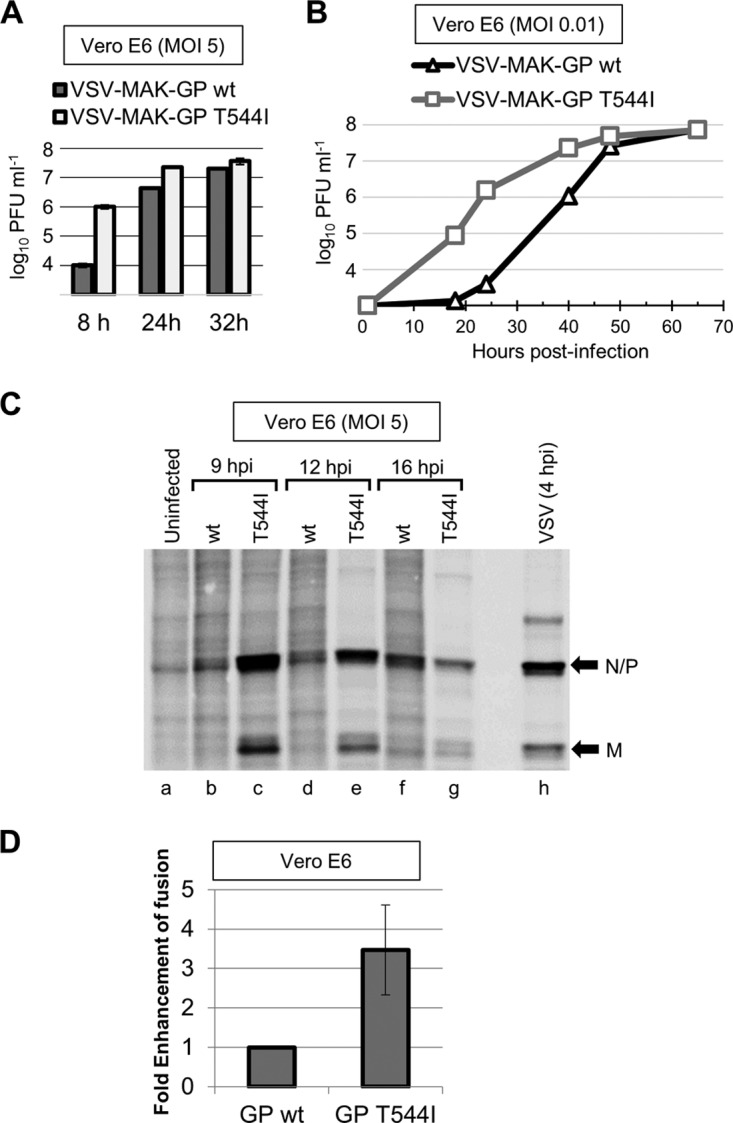
The mutant rVSV-MAK-GP T544I virus exhibits greater infectivity of cells than wild-type rVSV-MAK-GP. (A and B) High (A)- and low (B)-MOI infections of Vero E6 cells indicate that the mutant virus produces a faster accumulation of titers than wild-type virus. Titers were determined by plaque assay. Titers are the averages from duplicate samples. Error bars represent the range of duplicates for each data point. (C) Metabolic labeling of protein synthesis in infected cells, showing that mutant virus-infected cells exhibit viral protein synthesis earlier than wild-type-infected cells. Vero E6 cells were infected with the indicated virus and pulsed with 35S-labeled methionine for 15 min at the indicated times postinfection. Cells were immediately lysed after the pulse, and lysates were analyzed by SDS-PAGE. The gel was vacuum-dried and imaged with a phosphorimager. (D) T544I mutation results in increased GP1,2-mediated entry of pseudotyped lentivirus particles. HIV particles incorporating BlaM-Vpr fusion protein were pseudotyped with wt Makona GP1,2 or T544I mutant GP1,2. Beta-lactamase activity in cells was measured by FACS as an indicator of particle fusion with cells. Data shown are the mean fold increase from five independent experiments where the mean of the wild-type-pseudotyped particles is set to 1. Error bars represent standard deviations (SD).
To determine if a growth difference between the viruses was observed under multiple-cycle growth, low-MOI growth curves (MOI of 0.01) were carried out on Vero E6 cells. T544I infection titers also increased faster than wt titers in the low-MOI experiments, where T544I titers were ∼2 logs higher than wt titers at 18 and 24 hpi (Fig. 3B). As seen in the high-MOI infections, wt titers reached a level comparable to those of T544I at the late time points (>50 hpi).
To establish if differences between these viruses occurred early or late during infection, viral protein synthesis was analyzed by metabolic labeling. Vero E6 cells were infected with rVSV-MAK-GP wt or T544I (MOI 5) and pulsed with 35S-radiolabeled methionine at 9, 12, and 16 hpi. Cells were lysed immediately after being pulsed, and lysates were analyzed by SDS-PAGE. T544I-infected cells expressed viral proteins much earlier than wt-infected cells (Fig. 3C). At 9 hpi, T544I-infected cells showed robust protein synthesis, but wt-infected cells showed virus protein synthesis that was only slightly detectable compared to that of mock-infected cells (Fig. 3C, compare lanes a to c). By 12 hpi, host cell protein synthesis was inhibited in T544I-infected cells (lane e) by the VSV matrix (M) protein, a hallmark of VSV infection as shown in cells infected with rVSV (lane h). wt infection showed a slight increase in viral protein synthesis at 16 hpi (lane f), but host cell protein synthesis was still not inhibited. T544I-infected cells showed significant CPE with several dead floating cells at 16 hpi, explaining why labeled viral proteins were reduced at this time point (lane g) compared to earlier time points (lanes c and e). These data indicate that infections by these two viruses differ at an early stage.
The T544I mutation enhances GP1,2-mediated cell entry.
Amino acid 544 is located in the fusion loop of the GP2 subunit. In the prefusion state, this amino acid is part of an antiparallel beta-strand that is adjacent to the hydrophobic region that penetrates the cell membrane. This residue, as an isoleucine, is reported to have a critical role in the fusion process (11). To determine the impact that threonine and isoleucine residues have on virus entry, we used a pseudotyped lentivirus entry assay. Lentivirus virus-like particles (VLPs) were created using a beta-lactamase (BlaM)-Vpr fusion protein that is incorporated in VLPs (12). These VLPs were pseudotyped with T544-MAK-GP1,2 or I544-MAK-GP1,2 by cotransfection. Equal amounts of purified VLPs were then incubated with Vero E6 cells, followed by the addition of CCF2-AM substrate. Successful GP1,2-mediated entry was detected by measuring BlaM-positive cells using flow cytometry. While both T544- and I544-MAK-GP1,2-pseudotyped VLPs fused with Vero cells, I544-MAK-GP1,2-pseudotyped VLPs displayed approximately 3-times-higher levels of entry than the wild-type T544-MAK-GP1,2 VLPs (Fig. 3D). These data indicate that the T544I mutation in GP2 increases GP1,2-mediated cell entry and are consistent with the hypothesis that fusion is enhanced in Vero E6 cells following mutation from threonine to isoleucine at this residue.
Mutant rVSV-MAK-GP T544I virus outcompetes wild-type virus when grown together on Vero E6 cells.
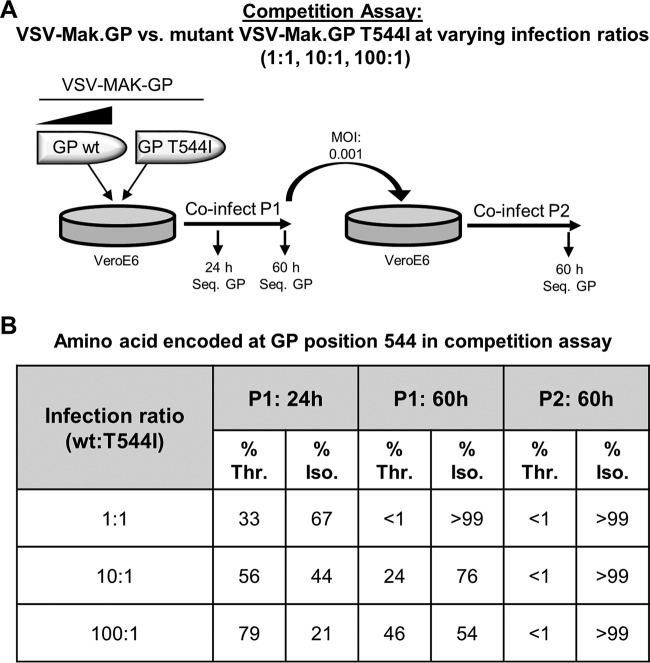
The faster growth kinetics exhibited by the rVSV-MAK-GP T544I mutant virus suggests that it has a competitive growth advantage over the wild-type virus. To test this, we carried out competition assays in which Vero E6 cells were coinfected at low MOI with a mixture of rVSV-MAK-GP wt and T544I viruses. Cells were infected at three different ratios, where the wt was present at ratios of 1:1, 10:1, and 100:1 to T544I. A schematic of the experimental approach is shown in Fig. 4A. Supernatant samples for each ratio were collected for sequencing (Sanger) at 24 and 60 hpi of the coinfection passage (coinfected P1). To determine the frequency of isoleucine in the coinfections after a second passage, fresh Vero E6 cells were infected at low MOI with the coinfected P1 virus (60-hpi samples) from each ratio. Supernatant samples from the second passages (coinfected P2) were collected for sequencing at 60 hpi. Threonine and isoleucine frequencies were measured by determining surface areas of the corresponding nucleotide peaks in the trace files.
FIG 4.
Mutant rVSV-MAK-GP T544I virus outcompetes wild-type virus in competition assays. (A) Schematic showing the workflow of the competition assay and time course collection of viral progeny in the P1 and P2 samples. Vero E6 cells were coinfected with increasing amounts of the wild-type virus and a constant amount of the T544I mutant virus (MOI of 0.001) at three different ratios, 1:1, 10:1, and 100:1. Supernatant virus samples were collected for sequencing at the indicated times. (B) Frequency of I544 and T544 residues in virus progeny from the coinfections described for panel A. cDNAs synthesized from viral genomes were sequenced by the Sanger method, and the percentages of genomes encoding T544 or I544 were calculated as described in Materials and Methods. Values of >99% indicates that only one amino acid was detected in the trace files.
Figure 4B shows that the 1:1 infection ratio resulted in a population fully encoding I544 by the end of the first coinfection passage (P1, 60 hpi). The 10:1 and 100:1 infection ratios had a heterogeneous population of threonine and isoleucine in the coinfection P1 samples at 24 and 60 hpi. However, a considerable increase in the isoleucine frequency occurred over the two time points for both ratios. By the end of the second passage (P2, 60 hpi), the wt T544 residue was no longer detected for the 10:1 and 100:1 infection ratios. These data show that the GP1,2 T544I mutation confers a strong selective advantage during growth of rVSV-MAK-GP in Vero E6 cells.
The T544I mutation emerges rapidly in monkey cells but not in some human cell lines.
Based on the appearance of the T544I mutation in viruses grown on Vero E6 cells, we were interested in determining whether this mutation was unique to growth on Vero E6 cells or if it would rapidly emerge during virus propagation in other monkey or human cell lines. To test this, VSV-MAK-GP encoding T544 was propagated at low MOI (0.001) in three different wells using Vero and BS-C-1 cells. It was also propagated on the human cell lines Huh-7 and HepG2. Each of the triplicate virus samples passaged in Vero cells had ∼90% of their sequences carrying the mutant I544 codon by the end of two serial passages (Fig. 5A). The I544 codon was also present in viruses grown on BS-C-1 cells, although not to the extent that was observed in Vero cells. Two of the three replicates grown on BS-C-1 cells had ∼10% of their sequences encoding the I544 codon; however, the third replicate had 50% of sequences encoding I544 (Fig. 5A). These data indicate that the T544I mutation emerges with high frequency in Vero and BS-C-1 cells, but it accumulates in the viral population at a higher rate when grown on Vero cells.
FIG 5.
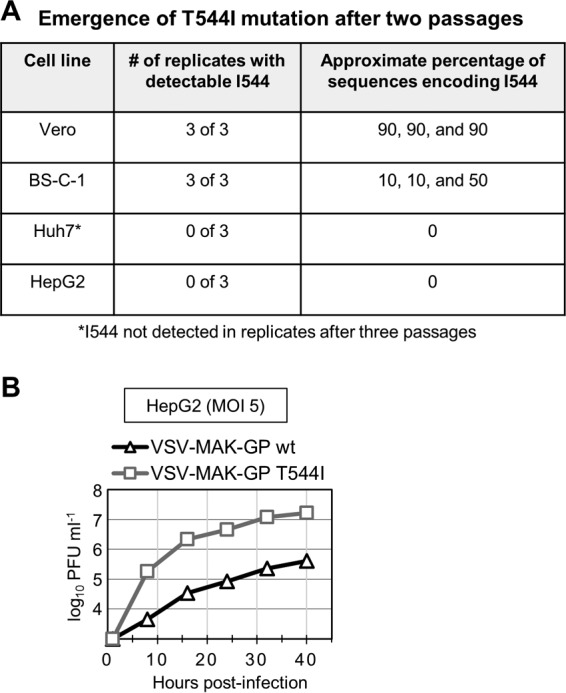
Determining the emergence of the T544I mutation during growth of VSV-MAK-GP in various cell lines. (A) Summary of the number of replicate wells that acquired the T544I mutation and their percentage of sequences encoding the mutation after two serial passages. Each cell line was infected in triplicate at an MOI of 0.001 with VSV-MAK-GP encoding the wild-type T544 residue. Cells were incubated at 37°C and 5% CO2 until CPE was observed across the entire monolayers (∼72 to 96 hpi). After two serial passages, supernatant viruses were collected and the GP gene sequenced by the Sanger method. Approximate percentages of sequences encoding I544 were determined from the sequencing chromatographs. Huh7 cells were sequenced after two and three serial passages. (B) Time course infection showing that mutant VSV-MAK-GP T544I virus exhibits faster growth kinetics than the wild-type virus on HepG2 cells (MOI of 5). Titers were determined by plaque assay on Vero E6 cells. Titers are averages for duplicate samples.
For viruses grown in HuH7 cells, three replicate samples showed no detection of the mutant I544 codon after three serial passages (Fig. 5A). Similarly, the mutant I544 codon was not detected in three replicate samples grown on HepG2 cells after two serial passages (Fig. 5A). Threonine was the only residue encoded at this position after passaging in these cell lines. Interestingly, we also observed in single-cycle infections of HepG2 cells that T544I mutant growth titers accumulated faster than wild-type titers by more than a log (Fig. 5B). Despite the apparent faster growth kinetics of T544I mutant viruses on HepG2 cells, we did not see a rapid emergence of T544I viruses in this cell line, suggesting that other factors may be involved. Collectively, these data show that the T544I mutation emerges rapidly during growth of VSV-MAK-GP on various monkey cell lines but does not emerge or emerges with substantially slower kinetics in the human cell lines we tested.
Rapid appearance and dominance of T544I during cell culture passage of EBOV Makona isolates.
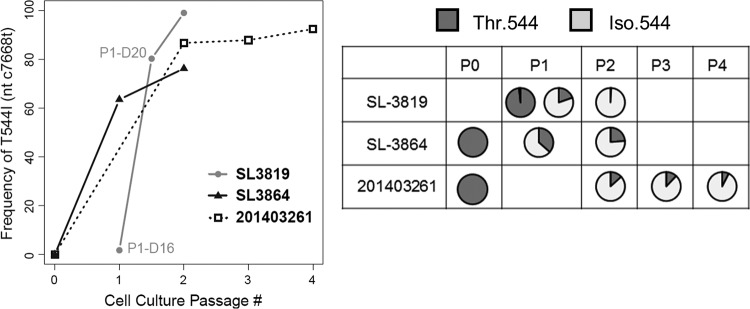
The observation that T544I occurred spontaneously in rVSV-MAK-GP and outcompeted wild-type virus in cell culture led us to ask if the same could be observed during tissue culture passage of EBOV Makona and to investigate the kinetics of the switch. To test for this, we analyzed three distinct Makona isolates that were passaged multiple times in Vero E6 cells. During the process, the original clinical sample and the serial passages of these isolates were collected for sequence analysis. Next-generation sequencing (NGS) was used to quantify the number of genomes in the virus population that contained a cytidine (GP1,2 T544) or a thymidine (GP1,2 I544) nucleotide at position 7668 (of the positive-sense genome). Figure 6 shows the frequency of the T544I mutation in each isolate over the course of serial passages. As can be seen in the SL-3864 and 201403261 isolates, the P0 populations had no statistically detectable amounts of genomes encoding isoleucine at this position (0% and 0.06%, respectively). SL-3864 showed a significant emergence of isoleucine in the first passage (P1), with 63% of genomes encoding I544. In P2, 76% of the genomes for this isolate encoded I544. P1 data were not available for the 201403261 isolate; however, the P2 passage showed that the bulk of genomes (87%) encoded isoleucine. This isolate illustrated that the I544 residue is stable in Vero E6 cells, as the percentage of genomes encoding I544 continued to steadily increase from P2 to P4.
FIG 6.
The T544I mutation rapidly emerges during passage of three distinct EBOV Makona isolates in tissue culture. The line plot and pie charts show the increase in frequency of T544I during serial passage of the three EBOV Makona isolates on Vero E6 cells. For the SL-3819 isolate, passage 1 (P1) was sampled twice, once on day 16 postinoculation (D16) and once on day 20 (D20). In all cases, the underlying mutation was a C to T at nucleotide position 7668 relative to the KJ660346.2 (GenBank) sequence.
The SL-3819 isolate showed the most drastic threonine-to-isoleucine conversion. This isolate did not have sequencing data available for P0, but day 16 of P1 showed that 98% of genomes encoded threonine. We note that growth of the clinical isolate required extended incubation for the infection to become apparent. At day 20 of P1, a stark conversion was observed, as only 20% of genomes encoded threonine and 80% encoded the isoleucine mutation. P2 for this isolate encoded almost entirely isoleucine (98%). These data highlight three independent cases where genomes containing I544 could not be detected in P0 sequences (or at P1 day 16 for SL-3819) before tissue culture passage but comprised the bulk of viruses upon passage in tissue culture. These findings support the hypothesis that the T544I mutation often occurs spontaneously during in vitro growth.
The T544I mutation is common in EBOV GP1,2 but is not found in certain ebolavirus species.
Sequences from other EBOV variants suggest that this T-I transition at residue 544 during cell culture growth is not EBOV Makona specific. The Mayinga and Kikwit sequences deposited in NCBI are all derived from virus passaged in tissue culture, and to our knowledge there are no reported sequences for clinical isolates from the 1976 (Mayinga) and 1995 (Kikwit) outbreaks. Of the sequences deposited, position 544 is reported as a mixture of T544 and I544. As illustrated in Fig. 7 (top row), 3 of 7 Mayinga GP1,2 sequences are reported as T544, and 4 of 7 are reported as I544. Five of 19 Kikwit GP1,2 sequences are reported as T544, and 14 are reported as I544. This supports the notion that the GP1,2 T544I mutation is selected for in multiple EBOV variants during tissue culture growth.
FIG 7.
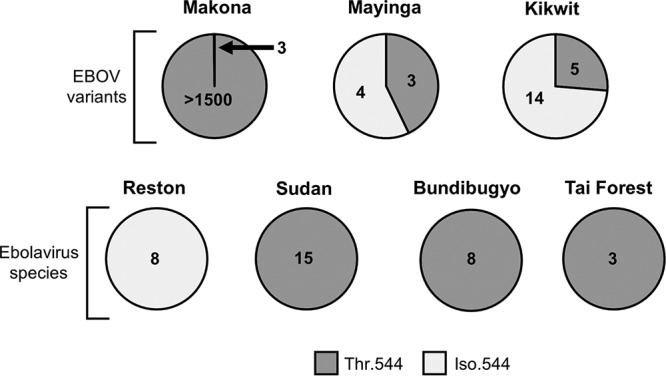
Distribution of threonine and isoleucine in all ebolavirus sequences deposited in NCBI. The upper row of pie charts shows the number of sequences encoding T544 or I544 in three EBOV (Zaire) variants. The lower row shows the number of sequences encoding T544 or I544 for the other ebolavirus species.
Further support for this hypothesis is provided by a recent report describing the generation of a Kikwit virus seed and challenge stock (13). In this study, the seed stock GP1,2 sequence (R4414) was T544 and was used to grow a working stock (R4415) on Vero E6 cells. The working stock is isogenic with the seed stock except for a single-amino-acid substitution, where the working stock encodes isoleucine at GP1,2 544. This finding shows that isoleucine at GP1,2 544 is selected for in EBOV Kikwit-passaged stocks as well as in EBOV Makona-passaged stocks.
To determine if the T544I mutation is found in other ebolaviruses, we analyzed sequences deposited in NCBI. Interestingly, all of the Reston sequences, which are derived from tissue culture virus, encoded isoleucine (Fig. 7, bottom row). Reston GP1,2 sequences are one amino acid larger than GP1,2 sequences of other ebolaviruses; hence, the analogous position is 545 for Reston GP1,2. To our knowledge, there are no P0 stocks reported for Reston virus. If it is assumed that Reston P0 stocks encode threonine at this position (T545), the deposited sequences suggest that the threonine-to-isoleucine mutation occurs with high frequency upon tissue culture passage of Reston ebolaviruses.
However, the T544I mutation may not be universally selected for during cell culture for all species of ebolavirus. Sequence comparison of EBOV (Makona), Sudan, Bundibugyo, and Tai' Forest GP1,2 sequences shows that the fusion loop is aligned and conserved across these species. All of these GP1,2s are identical in length (676 amino acids), and the flanking cysteine residues that define the fusion loop boundaries align to amino acids 511 and 556 for each GP1,2. The fusion loop is highly conserved between EBOV, Bundibugyo virus, and Tai' Forest virus, with 89% of its amino acids being identical. Sudan virus shows more variability, with 76% of fusion loop amino acids being identical to those of EBOV. The “AEGIYTEG” motif (amino acids 539 to 546) encompassing position 544 is identical for all reported sequences from these ebolaviruses (excluding 544 heterogeneity in EBOV sequences). Interestingly, all deposited sequences for Sudan, Tai' Forest, and Bundibugyo GP1,2 encode a threonine at position 544 (Fig. 7, bottom row). Many of these sequences come from tissue culture-passaged viruses. At least 8 of the 15 Sudan sequences are from tissue culture-passaged viruses; two of these were subsequently passaged multiple times in guinea pigs before being sequenced. Three of 8 Bundibugyo sequences and each of the three Tai' Forest sequences were passaged in tissue culture as well. Some of the passaged sequences were derived from viruses grown on Vero E6 cells, but for other sequences it is not clear which cell line was used. The nonappearance of I544 in these sequences suggests that the T544I mutation occurs with less frequency or is not selected for in these ebolaviruses during tissue culture growth.
We asked if the T544I mutation appears in GP1,2 from these species during repeated passage in tissue culture. To answer this, we utilized pseudotyped rVSV-ΔG generated by others (14, 15). rVSV-ΔG viruses carrying a GP1,2 gene from the Sudan, Bundibugyo, or Tai' Forest species were acquired and passaged on Vero E6 cells. Each virus was sequenced at passage 3 to determine the residue at GP1,2 position 544. T544 was found in passage 3 for each of the three pseudotyped viruses, and trace files showed no presence of I544 genomes. Consistent with the sequences deposited in NCBI, these data show that the T544I mutation does not appear, or appears with less frequency, in the GP1,2 of Sudan, Bundibugyo, and Tai' Forest ebolaviruses during tissue culture passage.
DISCUSSION
These data illustrate the strong selection pressure on position 544 of the EBOV GP1,2 in certain cell lines. The bulk of our virus studies were performed on Vero E6 cells and are in agreement with recent reports that T544I enhanced GP1,2-mediated entry in these cells (5, 6, 7). Our studies further show that the T544I mutation is a rapid and spontaneous mutation, likely not “carried” with T544 virus from clinical samples. The mutation occurred not only in the context of infectious EBOV but also when the GP1,2 was transferred to another virus system.
Because we generated recombinant VSV-MAK-GP by reverse genetics using a genomic plasmid that encoded GP1,2 T544, the P0 virus stock would have very likely been entirely T544. The first virus encoding I544 would have likely been produced very late in the P1 infection, during P2 plaque development, or early in the growth of picked-plaque stocks. This provides experimental evidence that a spontaneous T544I mutation can materialize from a pure T544 virus stock and emerge in the virus population rapidly, at least in Vero, Vero E6, and BS-C-1 cells. Other Ebola virus components are not required for this adaptation.
Deep-sequencing analysis of EBOV Makona growth stocks showed that the T544I mutation is also selected for on a very rapid time scale. All three Makona isolates that we tracked using NGS went from statistically insignificant numbers of genomes encoding I544 to a population that was I544 dominated within two passages. These data, together with the emergence of mutants from a pure T544 stock for VSV-MAK-GP, are consistent with the hypothesis that genomes encoding I544 in EBOV growth stocks could be the result of spontaneous mutation rather than the outgrowth of existing mutants in patients.
We observed that the T544I mutation emerged rapidly during growth of VSV-MAK-GP in Vero E6 cells but not in Huh7 cells. Our findings are in agreement with a recent report from Hoffman et al. (7). In that report, T544I conferred enhanced entry of pseudotyped viruses on Vero E6 but not on Huh7 cells. The authors also showed that EBOV encoding I544 exhibited enhanced growth over T544 on Vero E6 but not on Huh7 cells. It is worthwhile to note that studies by the Ebihara lab have shown that recombinant EBOV accumulates fewer mutations in Huh7 cells (16), a trend particularly notable in the GP1,2 gene, suggesting that these cells may have a unique ability to support replication of clinical isolates of EBOV with less adaptive pressure. We also show that T544I does not emerge in another human liver cell line, HepG2. This was intriguing since we had observed that mutant VSV-MAK-GP T544I grows faster than wild-type virus on these cells. It may prove interesting to investigate the different effects that the T544I mutation has on virus infection in Huh7 and HepG2 cells to understand a mechanistic basis for the mutation. Future studies analyzing the emergence of the T544I mutation on other monkey and human cell lines, as well as cell lines from other species such as bats, could provide additional insight into the basis of this mutation.
T544I is also apparent in GP1,2 from other EBOVs. It is not certain whether the mixtures of sequences deposited in NCBI that contain threonine or isoleucine for EBOV Mayinga and Kikwit are also due to tissue culture adaptation, since P0 sequences for these strains are not available. However, P0 sequences for more recent EBOV outbreaks (other than Makona) include threonine at this position in all directly sequenced clinical isolates. This is consistent with threonine as the conserved residue for clinical EBOV, and therefore we infer that isoleucine is likely a cell culture derived mutation in the Mayinga and Kikwit sequences. We also find evidence of the T544I mutation occurring in the EBOV Kikwit variant when analyzing sequences from a recent report detailing a stock preparation (13). Collectively, these findings support our hypothesis that the tissue culture adaptation caused by the T544I mutation occurs across multiple EBOV variants.
Our data, together with those reported by Hoffman et al. (7), strongly support that T544I is a tissue culture-specific mutation for EBOV. Two other reports identified heterogeneity at position 544 (5, 6), and both suggested that a polymorphism at this residue was involved in virus pathogenesis. The high frequency of the T544I mutation occurring in tissue-cultured EBOV may have led to the belief that low levels of virus encoding I544 were present in patient samples. Our findings, however, do not agree with amino acid 544 playing a role in viral pathogenesis or disease outcome. Our data show that T544I can be and is commonly acquired by spontaneous mutation in tissue culture and is rapidly selected for within 1 to 2 passages. To our knowledge, there are no reports of EBOV clinical isolate samples that have detectable genomes encoding I544 prior to being passaged in tissue culture.
Sudan, Bundibugyo, and Tai' Forest ebolaviruses do not show evidence of the T544I mutation. All deposited sequences for these viruses, many of which come from passaged stocks, encode threonine. We made use of recombinant VSV (delta-G) that encoded a GP1,2 gene from these species to test this. Consistent with the NCBI-deposited sequences, P3 or P4 stocks for these recombinant VSVs grown on Vero E6 cells continued to encode T544 (as determined by Sanger sequencing), and trace files showed no hint of I544-encoding genomes. It is not clear why I544 does not appear in these GP1,2s during tissue culture passaging. It is possible that an analogous tissue culture adaptation occurs at a different position in these species. It will be interesting for mechanistic purposes to determine why T544I does not emerge, or possibly emerges with less frequency, for these ebolaviruses.
Residue 544 is part of a hydrophobic structure that is critical for GP2-driven fusion and entry (11, 17). Residue 544 lies at the base of an extended loop structure in GP2. Crystal structures of the EBOV Mayinga fusion loop in the prefusion state containing either threonine or isoleucine at position 544 are reported in the literature (18, 19). We analyzed these structures and did not see a major structural difference between them, either globally or in the localized region of residue 544. A nuclear magnetic resonance (NMR) structure of the fusion loop in a fusion-competent conformation at pH 5.5 shows that residue 544, as an isoleucine, is part of a three-residue hydrophobic scaffold that includes leucine 529 and phenylalanine 535 (11). This triad forms a hydrophobic tip that is postulated to penetrate the cell membrane and initiate fusion with the viral membrane. This triad was defined using a GP1,2 that contains isoleucine at position 544 instead of the conserved threonine, but it shows a clear interaction of the methyl group of the isoleucine with the other two residues. Based on our work here, we propose that the longer hydrophobic side chain of isoleucine provides a longer and more optimal reach for the proposed “hydrophobic fist” to potentiate entry.
We observed by Western blotting that wild-type VSV-MAK-GP has an approximately 2-fold-higher particle-to-PFU ratio than mutant VSV-MAK-GP T544I (not shown). This observation suggests that wild-type particles have fewer successful infection events than mutant particles. It is possible that the T544I mutation increases particle infectivity by potentiating fusion. Alternatively, particle infectivity could be increased by T544I via other mechanisms, such as by potentiating cathepsin cleavage of GP. Future studies will be needed to elucidate a mechanism for the increased particle infectivity conferred by the T544I mutation.
It is unclear why this substitution does not occur in vivo. The GP1,2 region where this mutation occurs appears to be accessible to host immune responses, as several neutralizing antibodies bind to the fusion loop. The KZ52, 2G4, and 4G2 antibodies in particular have epitopes that lie near position 544 (20). Substitution with isoleucine could possibly result in an unfavorable structural change that causes greater exposure to cell-mediated and/or humoral immune responses. Hence, preserving T544 could serve to evade immune surveillance.
The robust emergence of T544I in monkey cell lines could lend the notion that EBOV circulating in monkeys and other nonhuman primates in the wild might encode isoleucine at this position. To our knowledge, the only report of Ebola virus genomic sequences collected from nonhuman primates in the wild does not support this notion (21). In that report, several great ape carcasses were discovered in the wild. Sampling showed that multiple animals tested positive for EBOV, and genomic sequences were made available in the NCBI database. We analyzed these sequences and found that all encoded T544. Thus, while the T544I mutation readily emerges in monkey-derived tissue culture cells, T544 appears to be the residue present during natural EBOV infection of at least certain nonhuman primates such as great apes.
We found evidence for the reversion of T544I in vivo in a report describing the generation of mouse-adapted EBOV Mayinga virus (22). The parental Mayinga virus encoded isoleucine at position 544. Upon successive passaging of this virus in mice, threonine was coded for at this position in the third passage and remained fixed upon further passage. Although two additional amino acid substitutions were reported at other positions in GP1,2 for the mouse-adapted virus, this finding strongly suggests that reversion to the conserved threonine residue occurred within three passages in mice and may play a role in allowing appropriate entry in this model.
We have presented evidence here that a spontaneous T544I mutation in EBOV GP1,2 is sufficient to confer tissue culture adaptation for recombinant VSV and EBOV. EBOVs harboring this change and their genomic sequences have been used in a number of published studies, both in vitro and in vivo. This work highlights the need to screen future ebolavirus laboratory stocks for this and other mutations that appear in vitro that could alter virus properties.
MATERIALS AND METHODS
Cell culture and viruses.
Baby hamster kidney (BHK) cells, kindly provided by Michael Whitt, and Vero E6 cells were grown in Dulbecco's modified Eagle's medium (DMEM) supplemented with 10% fetal bovine serum (FBS). HepG2 cells were grown in Eagle's minimum essential medium supplemented with 10% FBS. Recombinant viruses were generated by the reverse genetics technique described below, and virus stocks were grown on Vero E6 cells in DMEM supplemented with 10% FBS.
Recombinant DNA cloning of plasmid encoding the VSV-ΔG genome containing the Makona GP1,2 gene.
A human codon-optimized gene carrying the GP1,2 open reading frame from the EBOV Makona C07 isolate reported by Baize et al. (10) (GenBank accession no. AHX24658.2) was synthesized (DNA 2.0). The GP1,2 gene was subcloned into the pAK-VSVΔG-3N-SSS vector between the M and L genes using XhoI and NheI restriction sites. Transcription initiation and termination sequences controlling expression of the GP1,2 gene were preserved during cloning. The resulting plasmid was designated pVSVΔG-MAK-GP.
Recovery of recombinant VSV-MAK-GP virus.
Recovery of recombinant VSVs and those encoding ebolavirus GP1,2 in place of the VSV glycoprotein is described elsewhere (8, 9). Briefly, BHK cells in 6-well dishes (∼75% confluent) were infected with recombinant vaccinia virus encoding the T7 RNA polymerase at an MOI of 5 for 1 h. The virus inoculum was removed after incubation, and 3 ml of DMEM with 10% FBS was added to the wells. Cells were immediately transfected with a plasmid mixture of pVSVΔG-MAK-GP (1.1 μg) and VSV support plasmids pBS-N (0.6 μg), pBS-P (1.6 μg), and pGEM-L (0.9 μg) using polyethyleneimine (PEI) transfection (catalog no. 24765; Polysciences, Inc.). At 48 h posttransfection, the supernatants (P0) were collected, clarified by centrifugation, and filtered using a 0.22-μm syringe filter (Millex-GS) to remove vaccinia virus. Vero E6 cells in 10-cm plates were infected with filtered supernatant samples in the presence of cytosine beta-d-arabinofuranoside (2 μg/ml) to inhibit any carryover vaccinia virus. Cytopathic effect (CPE) indicative of VSV infection was first observed in Vero E6 cells at ∼72 h postinfection. Supernatant was collected (P1 stock) when all cells in the monolayer showed CPE (96 hpi). Cell lysates were analyzed by Western blotting to confirm expression of viral proteins (VSV P and Makona GP1,2). The P1 supernatant was clarified by centrifugation, and viral genomic RNA was used to synthesize cDNA to sequence the Makona GP1,2 gene (see below). Nucleotide substitutions were not observed in the P1 GP1,2 gene compared to the reference synthetic gene.
Sequencing of the GP1,2 gene from virus stocks.
Genomic RNA from the virus stocks was purified using the ZR viral RNA kit (Zymo Research). GP1,2 gene cDNA was synthesized from genomic RNA using the SuperScript III one-step reverse transcription-PCR (RT-PCR) kit (Invitrogen). Primers used to synthesize GP1,2 cDNA bound to the VSV M (forward, 5′-AAATCCTGCACAACAGATTCTTC) and L (reverse, 5′-GCGCTCATCGGGATTCA) genes. The RT-PCR was processed on an agarose gel, and a 2.7-kb fragment containing GP1,2 cDNA was cut out and purified with the QIAquick gel extraction kit (Qiagen). The gel-purified fragment was submitted for Sanger sequencing using primers specific for the GP1,2 synthesized gene. Contiguous sequences were generated with the CAP3 Program (23). All nucleotide sequence comparisons were performed with the NIH BLAST program.
Isolation and growth of plaque clones.
Plaques were isolated from the P1 supernatant by standard plaque assay on Vero E6 cells. Five primary plaques were picked from the same monolayer and individually transferred into 0.5 ml of DMEM with 10% FBS. Primary plaque isolates were designated clones 1 to 5. Clone 1 and 2 growth stocks were prepared concurrently, and clone 3 to 5 growth stocks were prepared concurrently at a subsequent time. Each clone stock was made by inoculating Vero E6 cells in T-75 flasks with 0.25 ml of the picked plaque stock. Stocks were grown in DMEM containing 10% FBS for 60 h at 37°C and 5% CO2. Supernatants were collected after incubation and clarified by centrifugation. Clarified supernatants were aliquoted and stored at −80°C. Stock titers were determined by standard plaque assay on Vero E6 cells. Plaques were fixed (4% formaldehyde) and stained with 1% crystal violet at 25 to 30 h postinfection.
Immunofluorescent staining of viral proteins.
Vero E6 cells in 6-well plates were fixed with 4% paraformaldehyde and permeabilized with 0.1% Triton X-100 at the indicated times postinfection. Cells were blocked with 2% bovine serum albumin (BSA) for 1 h prior to adding antibodies. EBOV GP1,2 was probed with c4G7 primary antibody (MAPP Biopharmaceutical) and anti-human Alexa Fluor 568 secondary antibody (Thermo Fisher Scientific). VSV M protein was probed with mouse 23H12 primary antibody and anti-mouse Alexa Fluor 488 secondary antibody (Thermo Fisher Scientific). Fluorescent images were captured on a Zeiss 200M epifluorescence microscope using similar exposure settings.
Lentivirus particle cell entry assay.
Lentivirus particles (HIV-1) incorporating β-lactamase (BlaM)-Vpr fusion protein were pseudotyped with EBOV Makona wt GP1,2 or EBOV Makona GP1,2 T544I mutant. Lentiviral particles were purified by ultracentrifugation through a 20% sucrose cushion (24,000 rpm and 4°C for 2 h with a SW28 rotor [Beckman Coulter]). The virus pellets were resuspended in phosphate-buffered saline (PBS), aliquoted, and stored at −80°C until use. The capsid content of HIV-1 was determined by a p24gag enzyme-linked immunosorbent assay (ELISA) (24). Vero cells were infected with either 100 ng or 200 ng of virus particles (1-h spinoculation and then incubation for 2 h at 37°C) in 12-well plates. Virus particle inputs were normalized by p24gag capsid content. Cells were washed to remove unbound particles, trypsinized, transferred to 96-well U-bottom plates, and incubated with CCF2-AM reporter overnight at 18°C. Cells were fixed with 4% paraformaldehyde, and the extent of virus particle-mediated fusion was determined by fluorescence-activated cell sorting (FACS).
Competition assay.
Vero E6 cells were coinfected with rVSV-MAK-GP and rVSV-MAK-GP T544I mutant viruses at three different PFU ratios, 1:1, 10:1, and 100:1. Clone 1 infections were done with increasing MOI (0.001, 0.01, and 0.1). Clone 2 infections were constant at an MOI of 0.001. After removal of the virus inoculum, cells were washed twice with PBS and fed 1 ml of DMEM with 10% FBS. Supernatant samples were collected for sequencing from the first coinfection (P1) at 24 and 60 h postinfection. At 60 h, the P1 coinfection was harvested and passaged on fresh cells at an MOI of 0.001 (coinfection P2). Supernatant samples were collected for sequencing from P2 at 60 h postinfection. GP1,2 gene cDNA was synthesized from virus in clarified supernatants as described above and sequenced by the Sanger method. Trace files from sequencing were analyzed to identify samples with dual peaks occurring at the single nucleotide position that differentiated between threonine and isoleucine codons. Surface areas of the cytidine peak (for threonine) and thymidine peak (for isoleucine) were determined with FIJI (25). The incidence of threonine and isoleucine for each sample is reported as a percentage of the sum of both nucleotide peaks. A report of >99% indicates that only one amino acid was detected. The experiment shown was done using duplicate samples. Data shown are from one set of replicates.
Deep-sequencing analysis of EBOV Makona isolate viruses.
The EBOV Makona virus stocks were sequenced at the U.S. Army Medical Research Institute of Infectious Diseases using an unbiased amplification protocol. RNA was isolated from TRIzol-treated material using the Zymo Direct-Zol kit (Zymo Research, Irvine, CA, USA). Sequence-independent single-primer amplification (SISPA) was performed as previously described (26). Amplified material was prepared for Illumina-based next-generation sequencing by shearing DNA to ∼400 bp using an M220 focused ultrasonicator (Covaris, Woburn, MA). Sequencing libraries were prepared using the Apollo 324 PrepX ILM 32I (Wafergen, Fremont, CA) with in-house dual indexes. The quality of the libraries was assessed for correct size on a DNA 1000 chip (Agilent Technologies, Santa Clara, CA) and quantified using the quantitative PCR (qPCR) library quantification kit for Illumina sequencing platforms (KAPA Biosystems, Wilmington, MA). Sequencing was performed on a MiSeq benchtop sequencer (Illumina, San Diego, CA) with either V2 or V3 MiSeq kits producing 2 × 151 paired-end reads.
Consensus sequences from two distinct samples for 201403261 P0 were previously published (27) (GenBank accession no. KP240932 and KP240933); those authors kindly provided us with the sequencing reads used to generate these genomes.
For each of the viral stocks, we estimated the frequency of the C-to-T mutation at nucleotide 7668 resulting in the T544I amino acid change by aligning the sequencing reads to Ebola virus/H.sapiens-wt/SLE/2014/Makona-G3864.1 (GenBank accession no. KR013754). Amplification primers were removed from the sequencing reads using Cutadapt v1.9.dev1 (28), and low-quality reads/bases were filtered using Prinseq-lite v0.20.3 (29). Reads were aligned to the reference using Bowtie2 v2.0.6 (30), and duplicates were removed with Picard (broadinstitute.github.io/picard). FreeBayes v1.0.2 (31) was used to estimate the frequency of the T544I variant. We only used reads with mapping quality of ≥30 and positions with base quality of ≥30.
Accession number(s).
Sequencing libraries were deposited in the GenBank database under the BioProject accession number PRJNA386278.
ACKNOWLEDGMENTS
We thank Anna Honko at Integrated Research Facility (NIAID) at Fort Detrick, MD, and Erica Ollmann Saphire at The Scripps Research Institute, La Jolla, CA, for helpful discussions. We also thank the members of the Connor laboratory at Boston University School of Medicine for their critical reading of the manuscript. We thank S. Whitmer and U. Stroeher for sharing the sequencing data used for the assembly of the 201403261 P0 genomes.
The content of this publication does not necessarily reflect the views or policies of the U.S. Army.
This work was funded in part by National Institutes of Health grants R01AI1096159 (J.H.C.) and R01AI064099 (S.G.). Work at the U.S. Army Medical Research Institute of Infectious Diseases was funded by the Defense Threat Reduction Agency, project CB10246 (G.P.).
REFERENCES
- 1.WHO. 2016. Ebola situation report, 30 March 2016. http://apps.who.int/ebola/current-situation/ebola-situation-report-30-march-2016 Accessed 28 February 2017.
- 2.Carette JE, Raaben M, Wong AC, Herbert AS, Obernosterer G, Mulherkar N, Kuehne AI, Kranzusch PJ, Griffin AM, Ruthel G, Cin PD, Dye JM, Whelan SP, Chandran K, Brummelkamp TR. 2011. Ebola virus entry requires the cholesterol transporter Niemann-Pick C1. Nature 477:340–343. doi: 10.1038/nature10348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Diehl WE, Lin AE, Grubaugh ND, Carvalho LM, Kim K, Kyawe PP, McCauley SM, Donnard E, Kucukural A, McDonel P, Schaffner SF, Garber M, Rambaut A, Andersen KG, Sabeti PC, Luban J. 2016. Ebola virus glycoprotein with increased infectivity dominated the 2013-2016 epidemic. Cell 167:1088–1098. doi: 10.1016/j.cell.2016.10.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Urbanowicz RA, McClure CP, Sakuntabhai A, Rey A, Simon-Loriere E, Sall AA, Kobinger G, Mü MA, Holmes EC, Lix F, Ball JK. 2016. Human adaptation of Ebola virus during the West African outbreak. Cell 167:1079–1087. doi: 10.1016/j.cell.2016.10.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ueda MT, Kurosaki Y, Izumi T, Nakano Y, Oloniniyi OK, Yasuda J, Koyanagi Y, Sato K, Nakagawa S. 13 January 2017. Functional mutations in spike glycoprotein of Zaire ebolavirus associated with an increase in infection efficiency. Genes Cells doi: 10.1111/gtc.12463. [DOI] [PubMed] [Google Scholar]
- 6.Wang MK, Lim S-Y, Lee SM, Cunningham JM. 2017. Biochemical basis for increased activity of Ebola glycoprotein in the 2013-16 epidemic. Cell Host Microbe 21:367–375. doi: 10.1016/j.chom.2017.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hoffmann M, Crone L, Dietzel E, Paijo J, González-Hernández M, Nehlmeier I, Kalinke U, Becker S, Pöhlmann S. 22 February 2017. A polymorphism within the internal fusion loop of the Ebola virus glycoprotein modulates host cell entry. J Virol doi: 10.1128/JVI.00177-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lawson ND, Stillman EA, Whitt MA, Rose JK. 1995. Recombinant vesicular stomatitis viruses from DNA. Proc Natl Acad Sci U S A 92:4477–4481. doi: 10.1073/pnas.92.10.4477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Garbutt M, Liebscher R, Wahl-Jensen V, Jones S, Möller P, Wagner R, Volchkov V, Klenk H-D, Feldmann H, Ströher U. 2004. Properties of replication-competent vesicular stomatitis virus vectors expressing glycoproteins of filoviruses and arenaviruses. J Virol 78:5458–5465. doi: 10.1128/JVI.78.10.5458-5465.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Baize S, Pannetier D, Oestereich L, Rieger T, Koivogui L, Magassouba N, Soropogui B, Sow MS, Keïta S, De Clerck H, Tiffany A, Dominguez G, Loua M, Traoré A, Kolié M, Malano ER, Heleze E, Bocquin A, Mély S, Raoul H, Caro V, Cadar D, Gabriel M, Pahlmann M, Tappe D, Schmidt-Chanasit J, Impouma D, Diallo AK, Formenty P, Van Herp M, Günther S. 2014. Emergence of Zaire Ebola virus disease in Guinea. N Engl J Med 371:pp 1418–1425. doi: 10.1056/NEJMoa1404505. [DOI] [PubMed] [Google Scholar]
- 11.Gregory SM, Larsson P, Nelson EA, Kasson PM, White JM, Tamm LK. 2014. Ebolavirus entry requires a compact hydrophobic fist at the tip of the fusion loop. J Virol 88:6636–6649. doi: 10.1128/JVI.00396-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cavrois M, de Noronha C, Greene WC. 2002. A sensitive and specific enzyme-based assay detecting HIV-1 virion fusion in primary T lymphocytes. Nat Biotechnol 20:1151–1154. doi: 10.1038/nbt745. [DOI] [PubMed] [Google Scholar]
- 13.Kugelman JR, Rossi CA, Wiley MR, Ladner JT, Nagle ER, Pfeffer BP, Garcia K, Prieto K, Wada J, Kuhn JH, Palacios G. 2016. Informing the historical record of experimental nonhuman primate infections with ebola virus: genomic characterization of USAMRIID ebola virus/H.sapiens-tc/COD/1995/Kikwit-9510621 challenge stock ‘R4368′ and its replacement ‘R4415′. PLoS One 11:1–9. doi: 10.1371/journal.pone.0150919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Geisbert TW, Daddario-DiCaprio KM, Williams KJN, Geisbert JB, Leung A, Feldmann F, Hensley LE, Feldmann H, Jones SM. 2008. Recombinant vesicular stomatitis virus vector mediates postexposure protection against Sudan Ebola hemorrhagic fever in nonhuman primates. J Virol 82:5664–5668. doi: 10.1128/JVI.00456-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mire CE, Geisbert JB, Marzi A, Agans KN, Feldmann H, Geisbert TW. 2013. Vesicular stomatitis virus-based vaccines protect nonhuman primates against Bundibugyo ebolavirus. PLoS Negl Trop Dis 7:e2600. doi: 10.1371/journal.pntd.0002600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Tsuda Y, Hoenen T, Banadyga L, Weisend C, Ricklefs SM, Porcella SF, Ebihara H. 2015. An improved reverse genetics system to overcome cell-type–dependent Ebola virus genome plasticity. J Infect Dis 212(Suppl 2):S129–S137. doi: 10.1093/infdis/jiu681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gregory SM, Harada E, Liang B, Delos SE, White JM, Tamm LK. 2011. Structure and function of the complete internal fusion loop from Ebolavirus glycoprotein 2. Proc Natl Acad Sci U S A 108:11211–11216. doi: 10.1073/pnas.1104760108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bornholdt ZA, Ndungo E, Fusco ML, Bale S, Flyak AI, Crowe JE, Chandran K, Saphire EO. 2016. Host-primed Ebola virus GP exposes a hydrophobic NPC1 receptor-binding pocket, revealing a target for broadly neutralizing antibodies. mBio 7:e02154-15. doi: 10.1128/mBio.02154-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Misasi J, Gilman MSA, Kanekiyo M, Gui M, Cagigi A, Mulangu S, Corti D, Ledgerwood JE, Lanzavecchia A, Cunningham J, Muyembe-Tamfun JJ, Baxa U, Graham BS, Xiang Y, Sullivan NJ, McLellan JS. 2016. Structural and molecular basis for Ebola virus neutralization by protective human antibodies. Science 6117:1343–1346. doi: 10.1126/science.aad6117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Davidson E, Bryan C, Fong RH, Barnes T, Pfaff JM, Mabila M, Rucker JB, Doranz BJ. 2015. Mechanism of binding to Ebola virus glycoprotein by the ZMapp, ZMAb, and MB-003 cocktail antibodies. J Virol 89:10982–10992. doi: 10.1128/JVI.01490-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wittmann TJ, Biek R, Hassanin A, Rouquet P, Reed P, Yaba P, Pourrut X, Real LA, Gonzalez J-P, Leroy EM. 2007. Isolates of Zaire ebolavirus from wild apes reveal genetic lineage and recombinants. Proc Natl Acad Sci U S A 104:17123–17127. doi: 10.1073/pnas.0704076104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Bray M, Davis K, Geisbert T, Schmaljohn C, Huggins J. 1998. A mouse model for evaluation of prophylaxis and therapy of Ebola hemorrhagic fever. J Infect Dis 179(Suppl):651–661. doi: 10.1086/515386. [DOI] [PubMed] [Google Scholar]
- 23.Huang X, Madan A. 1999. CAP3: a DNA sequence assembly program. Genome Res 9:868–877. doi: 10.1101/gr.9.9.868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hatch SC, Archer J, Gummuluru S. 2009. Glycosphingolipid composition of human immunodeficiency virus type 1 (HIV-1) particles is a crucial determinant for dendritic cell-mediated HIV-1 trans-infection. J Virol 83:3496–3506. doi: 10.1128/JVI.02249-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Schindelin J, Arganda-Carreras I, Frise E, Kaynig V, Longair M, Pietzsch T, Preibisch S, Rueden C, Saalfeld S, Schmid B, Tinevez J-Y, White DJ, Hartenstein V, Eliceiri K, Tomancak P, Cardona A. 2012. Fiji: an open-source platform for biological-image analysis. Nat Methods 9:676–682. doi: 10.1038/nmeth.2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Djikeng A, Halpin R, Kuzmickas R, DePasse J, Feldblyum J, Sengamalay N, Afonso C, Zhang X, Anderson NG, Ghedin E, Spiro DJ. 2008. Viral genome sequencing by random priming methods. BMC Genomics 9:5. doi: 10.1186/1471-2164-9-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Whitmer SLM, Albariño C, Shepard SS, Dudas G, Sheth M, Brown SC, Cannon D, Erickson BR, Gibbons A, Schuh A, Sealy T, Ervin E, Frace M, Uyeki TM, Nichol ST, Ströher U. 2016. Preliminary evaluation of the effect of investigational Ebola virus disease treatments on viral genome sequences. J Infect Dis 214(Suppl 3):S333–S341. doi: 10.1093/infdis/jiw177. [DOI] [PubMed] [Google Scholar]
- 28.Martin M. 2011. Cutadapt removes adapter sequences from high-throughput sequencing reads. EMBnet J 17:10. doi: 10.14806/ej.17.1.200. [DOI] [Google Scholar]
- 29.Schmieder R, Edwards R. 2011. Quality control and preprocessing of metagenomic datasets. Bioinformatics 27:863–864. doi: 10.1093/bioinformatics/btr026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Langmead B, Salzberg SL. 2012. Fast gapped-read alignment with Bowtie 2. Nat Methods 9:357–359. doi: 10.1038/nmeth.1923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Garrison E, Marth G. 2012. Haplotype-based variant detection from short-read sequencing. arxiv:1207.3907. [Google Scholar]