Abstract
Background
The number of patients in emergency departments has risen steadily in recent years, with a particular increase in patients not requiring urgent treatment. The aim of this study is to characterize this group of patients with respect to their sociodemographic features, health status, and reasons for attending an emergency department.
Methods
PiNo Nord is a cross-sectional observational study representing two full working weeks in five different hospitals. Patients were questioned in personal interviews, and medical diagnoses were documented. The data were analyzed with multivariate logistic regressions in mixed multilevel models. Predictors for the subjectively perceived treatment urgency were identified by stepwise backward selection.
Results
The 1175 patients questioned had an average age of 41.8 years and 52.9% were male. 54.7% said the degree of their treatment urgency was low. 41.3% had visited the emergency department on their own initiative, 17.0% on the advice or referral of their primary care physician, and 8.0% on the advice or referral of a specialist. The strongest predictors for low subjective treatment urgency were musculoskeletal trauma (odds ratio [OR] 2.18), skin conditions (OR 2.15), and the momentary unavailability of a primary care physician (OR 1.70).
Conclusion
More than half of the patients do not think their condition requires urgent treatment and thus do not meet the definition of a medical emergency. Patients’ reasons for visiting the emergency department are varied; aside from the treatment urgency of the health condition itself, the reason may lie in perceived structural circumstances and individual preferences.
According to a position paper by the German speaking specialist societies of emergency medicine, a medical emergency is defined as „changes in a person‘s health,“ for which the „patients themselves and/or a third party deem immediate medical and nursing care to be required“ (1). In Germany, emergency care is provided on an outpatient basis by statutory health insurance physicians as well as by ambulance services and hospital emergency departments. Outpatient treatment for members of the statutory health insurances is provided by registered physicians who—when practices are closed—fulfill their service mandate by means of emergency practices or emergency house call services, for example. The care of patients with life threatening or severe illnesses requiring inpatient treatment is the mandate of hospital emergency departments. These are supported by ambulance services and emergency physicians in terms of caring for and transporting patients (2).
However, the number of patients visiting emergency departments has substantially increased in recent years, and this increase seems to be mainly caused by patients not requiring urgent treatment (3– 8). Some authors regard the overcrowding in emergency departments as a problem of patient safety (9), as overcrowded emergency departments are associated with higher mortality, a longer time before medication is given to patients with pneumonia and acute pain, and a larger number of patients leaving emergency departments without having seen a doctor (9– 11). However, to date these international findings have not been confirmed for the German healthcare system.
A patient‘s decision to visit a hospital‘s emergency department for non-urgent conditions can be made for a variety of reasons. The few studies of this topic discuss consistently that in addition to a younger age, the convenience of attending emergency departments, recommendations from outpatient service providers, and a negative perception of care outside hospitals may play a part (12). Furthermore, a perceived lack of available appointments with outpatient physicians and the concentration of diagnostic and therapeutic options in hospitals seem to be crucial (6). However, the evidence shown here should be evaluated cautiously as, to date, only a few relevant studies exist that are of good methodological quality (12).
The study presented here therefore seeks to describe the population of patients with non-urgent conditions who visit emergency departments in Germany as to their sociodemographic characteristics, their health status, and their reasons for attending an emergency department.
Methods
The PiNo Nord (“Patienten in der Notaufnahme von norddeutschen Kliniken“ [”patients in the emergency departments of hospitals in Northern Germany”]) study is a cross-sectional observational study that was conducted in three hospitals in the Federal State of Hamburg and two hospitals in the Federal State of Schleswig-Holstein. Data were collected over a period of 210 days in total in a three-shift system; per hospital, the equivalent of two full working weeks was depicted. The hospitals‘ survey days were randomly assigned. Data were collected from 17 October 2015 through 18 July 2016.
The project included all patients of legal age who had been registered at the admissions desk in the emergency department or an emergency practice of the Association of Statutory Health Insurance Physicians in the hospital. Additionally, all minors were included who were accompanied by a legal guardian. Unaccompanied minors were not included because their ability to give consent is not legally regulated.
We excluded patients whose treatment urgency, according to the Manchester triage system (13), was categorized as „immediate“ (red) or „very urgent“ (orange), as well as non-triaged patients who—in equivalence to the Manchester triage system—required immediate or very urgent treatment in the opinion of doctors or nursing staff at the hospital. Patients were excluded if one or more of the following criteria applied:
Severe hearing, visual, or speech impairments (for example, patients with injuries to the mouth/face, non-compensated hearing loss/loss of visual acuity)
high level of symptom burden
verbal communication (if need be with an interpreter) in German/English not possible
lacking ability to consent (for example, in dementia)
isolation because of a disease
treatment without waiting time; and
direct referral to a different department within the hospital.
For each patient registered at the admissions desk in the emergency department, the researchers verified on the basis of the inclusion and exclusion criteria whether he or she was eligible for inclusion in the study. Eligible patients were asked for written informed consent and—if it was given—surveyed in personal interviews. An abbreviated version of the interview in German and English was available for patients with poor German language skills.
Patients‘ symptoms were recorded using the hospitals‘ medical diagnoses encoded by a trained project assistant into an abbreviated version of the International Classification of Primary Care (ICPC-2) adapted to the emergency setting (14, 15). Patients‘ health status and sociodemographic data were documented in the interview by means of a standardized questionnaire. The patients‘ general and vocational education were classified into three groups, according to the Comparative Analysis of Social Mobility in Industrial Nations (CASMIN) classification system:
Low—i.e., inadequately completed general education, general elementary education and/or basic vocational qualification.
Intermediate—i.e., secondary school certificate or A level equivalent
High—i.e., higher or lower tertiary education.
Recommendations from others and reasons for attending an emergency department were captured in the interview by using open-ended questions. Qualified interviewers entered the patients‘ answers into a pre-defined category system during the interview. Those answers that could not be categorized were documented verbatim and encoded afterwards, creating respective new categories, if necessary. Patients themselves estimated how urgently they needed treatment by using a numerical rating scale from 0 to 10; subsequently the subjectively perceived treatment urgency was categorized into two groups:
Low—i.e., 0–5
High—i.e., 6–10.
The data analysis was first carried out using descriptive statistics. Chi–square tests and t-tests were used to determine differences between patients whose subjectively perceived treatment urgency was low and patients whose self-reported urgency was high. Multivariate logistic regression in mixed models was used to analyze statistical inference; the models were adjusted for random effects at the level of the federal states and the hospitals within the states.
We used stepwise backward selection to select the predictors for the subjectively perceived treatment urgency, with a significance level of p = 0.05. Variables with characteristics represented in less than 1% of the population were excluded in advance. The tested variables were:
Age
Sex
Educational level
Migration status
12 ICPC-2 areas/organ systems
25 ICPC-2 codes
3 variables of awareness of outpatient emergency services
24 individual categories and 6 supercategories of reasons for visiting an emergency department
7 categories of persons who had recommended visiting an emergency department.
We defined an alpha level of 5% (p= 0.05) as the threshold for all analyses of the statistical inference. As we report the results of an exploratory observational study, the p-values throughout are descriptive. We used the software package Stata 12.1 to analyze the data. On 22 July 2015, the study received approval from the ethics committee of the Hamburg Medical Association (Ref No PV4993).
Results
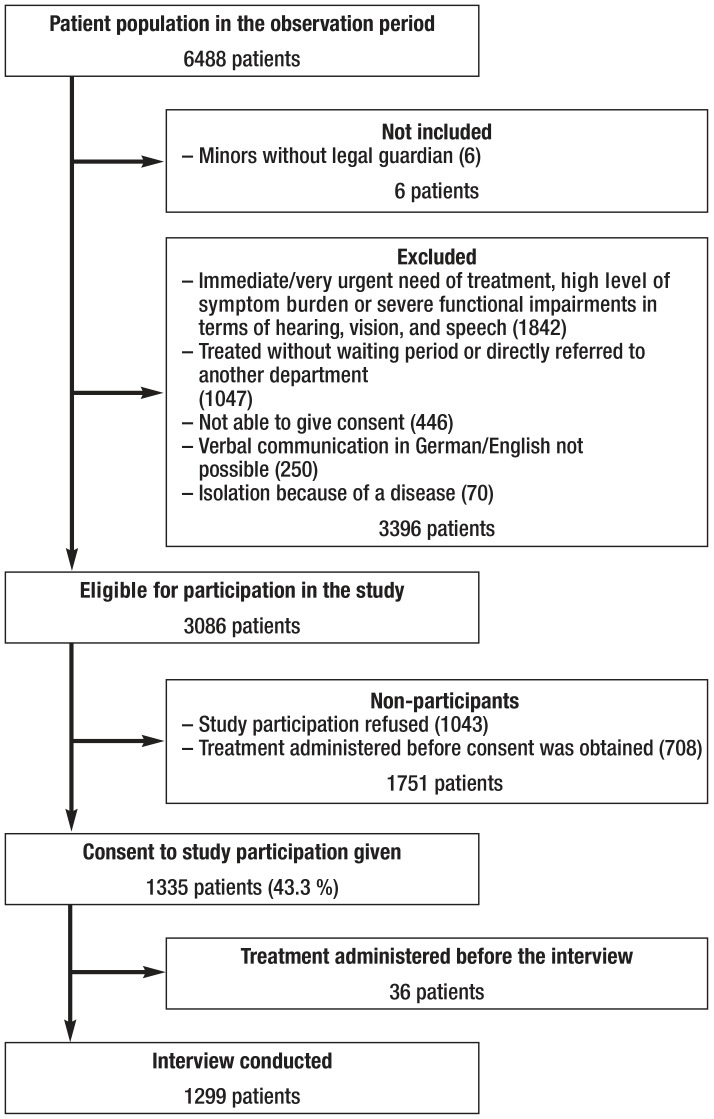
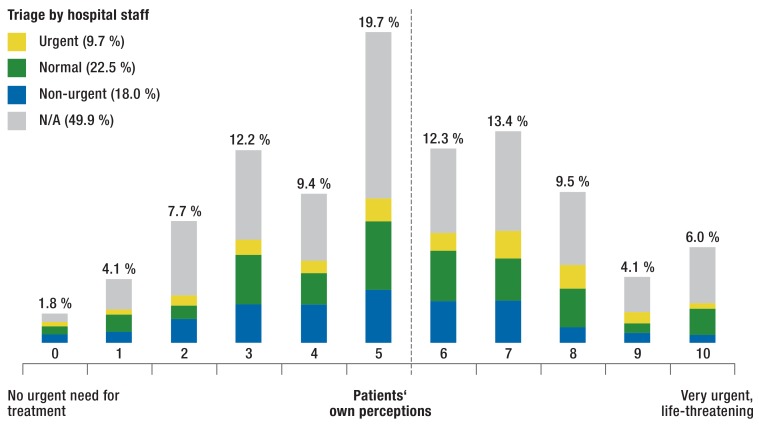
Figure 1 depicts the recruitment process. In total 6488 patients were registered, of whom 3086 were eligible for study participation. Of these, 1335 patients (43.3%) agreed to participate in the study, whereas 1043 refused. The eTable shows a comparison between the two groups (non-responder analysis). The interviews were completed with 1299 patients. However, 124 patients (9.5%) did not provide any information on their self-reported treatment urgency; consequently, the maximum case number for the analyses presented here is 1175 patients. 677 study participants were from Hamburg. Of the 498 patients recruited in Schleswig-Holstein, 133 (26.7%) had received treatment in an emergency practice of the Association of Statutory Health Insurance Physicians. Figure 2 shows the assessments of patients and hospital staff of the patients‘ treatment urgency. A low treatment urgency was reported by 54.7% of patients.
Figure 1.
Recruitment process
eTable. Non-responder analysis.
|
Study participation refused (n = 1 043) |
Agreed to study participation (n = 1335) |
p | |
| Health insurance – Statutory – Private – Employer’s Liability Insurance Association – None |
90.7 % 5.0 % 3.5 % 0.8 % (n = 990) |
84.9 % 8.0 % 6.7 % 0.4 % (n = 1221) |
<0.001 |
| Age: mean ± standard deviation |
46.0 ± 21.1 years (n = 1020) |
42.4 ± 19.5 years (n = 1335) |
<0.001 |
| Sex – Female – Male |
52.5 % 47.5 % (n = 1032) |
47.6 % 52.4 % (n = 1334) |
0.018 |
Figure 2.
Triage by hospital staff and patients‘ own perceptions of the treatment urgency (n = 1175)
N/A, not available
Table 1 shows sociodemographic data. Patients‘ average age was 41.8 years; patients whose subjectively perceived treatment urgency was low were on average 7.3 years younger than patients whose self-reported urgency was high. The majority of patients with low subjectively perceived treatment urgency were single. (52.1% versus 39.5%), pupils, university students or trainees (17.1% versus 11.3%). Fewer patients with low subjective urgency were retired (13.9% versus 23.2%) or had been born abroad (9.0% versus 13.5%) than patients whose subjectively perceived treatment urgency was high.
Table 1. Sociodemographic data.
| Total |
High subjectively perceived treatment urgency |
Low subjectively perceived treatment urgency |
p | |
|
Age Range |
41.8 ± 19.3 years 2 –93 years (n = 1175) |
45.8 ± 18.9 years 2–93 years (n = 532) |
38.5 ± 19.1 years 2 –93 years (n = 643) |
<0.001 |
|
Sex – Female – Male |
47.1 % 52.9 % (n = 1174) |
48.7 % 51.3 % (n = 532) |
45.8 % 54.2 % (n = 642) |
0.096 |
|
Civil status – Single – Married, cohabiting – Married, separated – Widowed – Divorced |
46.2 % 38.9 % 2.1 % 3.9 % 8.8 % (n = 1099) |
39.5 % 44.0 % 2.7 % 4.5 % 9.3 % (n = 514) |
52.1 % 34.5 % 1.5 % 3.4 % 8.4 % (n = 585) |
0.001 |
|
Migration status – Patient and at least one parent born in Germany – Patient born in Germany, both parents born abroad – Patient born abroad |
84.3 % 4.6 % 11.1 % (n = 1091) |
82.6 % 3.9 % 13.5 % (n = 512) |
85.8 % 5.2 % 9.0 % (n = 579) |
0.044 |
|
Educational level according to CASMIN – High – Intermediate – Low |
21.2 % 55.2 % 23.7 % (n =1095) |
19.7 % 53.9 % 26.5 % (n = 514) |
22.6 % 56.3 % 21.2 % (n = 581) |
0.101 |
|
Employment status – Employed – Retiree/pensioner – Pupil/student/trainee – Self employed – Looking for work/unemployed – Homemaker |
52.3 % 18.2 % 14.4 % 6.2 % 4.2 % 3.7 % (n = 1098) |
50.1 % 23.2 % 11.3 % 5.9 % 3.5 % 4.7 % (n = 513) |
54.2 % 13.9 % 17.1 % 6.5 % 4.8 % 2.9 % (n = 585) |
0.176 <0.001 0.006 0.657 0.292 0.122 |
CASMIN, Comparative Analysis of Social Mobility in Industrial Nations
Patients reported symptoms lasting between 30 minutes and 38 years. 28.1% of the patients had had the symptoms prompting them to visit the emergency department for less than 6 hours, whereas 35.4% of the patients had had their symptoms for three days or longer. Symptoms most often related to the musculoskeletal/locomotor system (36.0%), skin (14.1%), digestive system (12.0%), and circulatory system (10.5%); neurological symptoms (8.5%), respiratory symptoms (6.8%), or general and nonspecific symptoms (5.7%) were reported less frequently. Patients whose subjectively perceived treatment urgency was low mostly reported symptoms of the musculoskeletal/locomotor system (40.4% versus 30.6%; p=0.001) and skin (17.1% versus 10.6%; p=0.003) and fewer symptoms of the digestive system (9.6% versus 14.8%; p=0.009), circulatory system (8.2% versus 13.3%; p=0.016), psyche (0.9% versus 2.7%; p=0.022), as well as endocrine, metabolic, and nutrition-related problems (0.4% versus 2.7%; p=0.0001).
41.3% of the patients had visited the emergency department on their own initiative. Some patients reported a recommendation or referral from their GP (17.0%) or medical specialist (8.0%); both these were mentioned less frequently by patients whose subjectively perceived treatment urgency was low (14.0% versus 20.7%; p=0.003 and 6.3% versus 10.1%; p=0.016). Recommendations from other healthcare professionals were mentioned by 14.0% of patients. In 10.5% of the patients, their spouse/life partner had recommended that they visit the emergency department, in 7.7%, the recommendations had come from other relatives, and in 9.0%, from acquaintances, neighbors, or work colleagues. Recommendations from the latter were more common in patients with a low self-reported urgency (10.7% versus 6.9%; p=0.024). Almost all patients (97.6%) knew of the possibility to consult the fire and rescue services. However, comparatively few patients were aware emergency practices of the Association of Statutory Health Insurance Physicians (44.8%) and their emergency house call services (32.6%).
Table 2 shows subjective reasons why the problem had not been dealt with in the outpatient setting. Patients with low self-reported urgency reported less often that their visit to the emergency department was due to the severity of (19.7% versus 39.4%) or increase in symptoms (6.7% versus 14.0%), or that their fear of serious causes or progression of their health problems had been crucial (14.4% versus 21.6%). The perceived unavailability of open general practices did, however, play a greater part for these patients than for patients whose subjectively perceived treatment urgency was high (28.9% versus 16.8%).
Table 2. Subjective reasons why the problem was not resolved on an outpatient basis*.
|
Total (n = 1139) |
High subjectively perceived treatment urgency (n = 513) |
Low subjectively perceived treatment urgency (n = 626) |
p | |
| Urgency, of these | 48.7 % | 57.9 % | 41.1 % | <0.001 |
| – Urgency because of the severity of the symptoms/pain | 28.5% | 39.4 % | 19.7 % | <0.001 |
| – Patient is afraid of serious cause/disease progression | 17.7 % | 21.6 % | 14.4 % | 0.001 |
| – Urgency because of an increase in symptoms/pain | 10.0 % | 14.0 % | 6.7 % | <0.001 |
| Primary care services/availability, of these | 26.1 % | 19.9 % | 31.2 % | <0.001 |
| – No open general practice was available. | 23.4 % | 16.8 % | 28.9 % | <0.001 |
| Specialized outpatient care/availability, of these | 21.7 % | 19.5 % | 23.5 % | 0.104 |
| – No open specialist practice was available. | 13.9 % | 12.5 % | 15.0 % | 0.217 |
| Hospital specific factors, of these | 20.6 % | 22.0 % | 19.5 % | 0.292 |
| – Patient had previously attended this hospital | 9.5 % | 10.3 % | 8.8 % | 0.376 |
| – Hospital is close to patient‘s residence/ easily accessible | 7.8 % | 7.0 % | 8.5 % | 0.365 |
| – Hospital has a good reputation/had been recommended | 6.1 % | 7.0 % | 5.3 % | 0.219 |
| Emergency department is preferred to outpatient treatment, of these | 19.1 % | 19.5 % | 18.7 % | 0.731 |
| – Emergency department has better diagnostic facilities. | 7.9 % | 8.2 % | 7.7 % | 0.746 |
| – Emergency department has better treatment facilities. | 6.0 % | 7.2 % | 5.0 % | 0.109 |
| Unawareness/ignorance | 2.7 % | 2.3 % | 3.0 % | 0.473 |
| Patient has no health insurance | 0.1 % | – | 0.1 % | 0.365 |
* Multiple answers were permitted
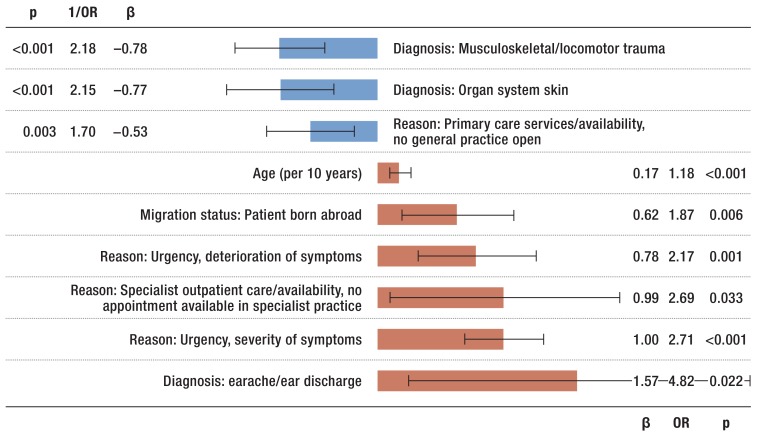
The stepwise regression identified a total of 9 predictors for the subjectively perceived treatment urgency, of which 6 were characteristic for a high, and 3 for a low self-reported treatment urgency (figure 3). 11.% of the variance in subjectively perceived treatment urgency could be explained with the statistical model.
Figure 3.
Differences between patients with low (blue bars) and high (red bars) subjectively perceived treatment urgency;
results of a multivariate logistic regression adjusted for random effects at the level of the federal states and hospitals (n = 950).
ß, regression coefficient; OR, odds ratio; p, probability value
Discussion
One reason for the high number of patients in emergency departments seems to be that a large proportion of patients use medical emergency structures without actually meeting the definition of an emergency (3, 4, 7, 8). In our study, more than half of the patients interviewed rated the urgency of their medical treatment as low. This was more the case for younger than for older patients, which is consistent with most of the available studies (10, 17). Migrants reported a low treatment urgency less frequently. Whether this is due to differences in healthcare user behavior or due to a higher degree of fearfulness relating to the symptoms (6) was not the subject of the present study.
In patients with a low subjectively perceived treatment urgency, musculoskeletal trauma and affections of the skin more often were the diagnoses leading the patients to seek emergency consultations. Furthermore, these patients complained less frequently about increasing and severe symptoms than patients who assessed their treatment urgency as high. This is consistent with findings from other studies (6, 18, 19).
One of the tasks of outpatient therapy is risk assessment and, if required, hospital admission of the patient (2). In the literature, recommendations from outpatient physicians are often discussed as an important reason for visits to emergency departments (6, 20, 21). In our study, up to 25% of the participants reported that they had visited the emergency department because of a referral or doctor‘s recommendation.
A further factor influencing patient numbers is the use of the emergency department by patients who could have been treated in outpatient care. This may in part be due to the deficits in awareness of the emergency care of the Association of Statutory Health Insurance Physicians, which have also been reported elsewhere (21). Fewer than half of the patients in our study were aware of the outpatient emergency care provision.
Further barriers to using outpatient care that are known from the literature include considerations of convenience (6, 22– 24) or the expectation of better care in the emergency department than in the doctor’s office (23, 25). In our study, these reasons were important for almost one in every four patients.
Closed practices of general practitioners or specialist doctors have often been mentioned in the literature (26, 27), and in our study, almost one third of the patients named this as a reason for visiting emergency departments. However, this perception of the availability of outpatient medical services in Germany‘s large cities, such as Hamburg, may be the result of patients‘ expectations of a 24/7 availability of healthcare services, rather than actual structural deficits in healthcare provision.
Strengths and limitations of the study
Patients‘ symptoms were collected by means of medical diagnoses. For all other variables we used patient data, which are not in every case consistent with doctors‘ perspectives. This is obviously also the case for the subjectively perceived treatment urgency (28). However, data on patient triage were available for only 50% of the patients. Regarding the data on „admissions/referrals,“ misunderstandings and misreporting are possible—for example the interpretation of a doctor‘s words that a patient uses to justify their visit to the emergency department. Reasons for visiting emergency departments varied according to the time and day of the week—for example, patients‘ views of the availability of outpatient physicians.
Concerning the statistical analyses it should be noted that the backward selection algorithm is sensitive to differences in the distribution of the included variables. Therefore, the identified model does not necessarily constitute the best set of predictors for a high subjectively perceived treatment urgency. As the rate of explained variance is only 11.0%, further factors are obviously characteristic for patients whose self-reported urgency is low. Furthermore, some of the identified predictors were present in only a small proportion of the patient population (for example, earache/ear discharge in 1.6% of the patients).
PiNo Nord has a comparatively large number of patients (1175), which allows for differentiated analyses. However, four out of the five study hospitals were located in large university cities, with rural regions not being represented in the study. Furthermore, only hospitals in Northern Germany were included. In Schleswig-Holstein, in the evening and on weekends, patients with non-urgent conditions are usually redirected to the emergency practices of the Association of Statutory Health Insurance Physicians affiliated to the hospitals, which were therefore also used for patient recruitment. By this route, some patients may have been inadvertently included into the study who were intentionally trying to visit an emergency practice of the Association of Statutory Health Insurance Physicians.
Patients were excluded from the study if they needed treatment immediately or very urgently, or if they had severe symptoms. 33.8% of eligible patients refused participation in the study. Furthermore, patients were excluded if they had received treatment—due to low patient numbers at certain times of the day—before receiving information, giving consent, being interviewed, or if they were directly referred to a different department within the hospital. The latter especially applied to patients visiting for gynecological symptoms.
On the other hand, the possibility to survey patients with a German or English short version of the interview enabled patients with only basic German language skills to participate in the study. The random assignment of survey days within a time frame of nine months minimized the study results’ dependency on events, such as flu epidemics or TV reports. Furthermore, in extensive sections of the interview, open-ended questions were asked, which enabled interviewees to give unforeseen responses.
Key Messages.
More than half of patients who attended emergency departments assessed their treatment urgency as low and therefore did not meet the definition of an emergency.
Patients with low subjectively perceived treatment urgency were younger; fewer were born abroad; they reported increasing and severe symptoms less often than patients with greater self-reported treatment urgency.
The reasons for attending emergency departments were manifold and may, in addition to the urgency of the health problem, lie in perceived structural conditions and individual patient preferences.
In the patient population under study,emergency practices of the Association of Statutory Health Insurance Physicians as well as their emergency house call services were relatively unknown.
Individual motives, such as convenience, negative expectations of the availability of outpatient physicians, or expectations of better healthcare services in emergency departments than in the outpatient system played an important role for many patients.
Acknowledgments
Acknowledgement
The study received funding from the Association of Statutory Health Insurance Physicians of Hamburg, the Association of Statutory Health Insurance Physicians of Schleswig-Holstein, and the Zentralinstitut für die Kassenärztliche Versorgung in Deutschland [Central Research Institute of Ambulatory Health Care in Germany]. Data were collected at the Evangelisch-Lutherische Diakonissenanstalt zu Flensburg, the Sana Kliniken Lübeck, the Katholisches Marienkrankenhaus Hamburg, the Bethesda Krankenhaus Bergedorf, and the University Medical Center Hamburg-Eppendorf. We wish to thank the funders/supporters and the participating hospitals for enabling us to undertake this study.
Footnotes
Conflict of interest statement
The authors declare that no conflict of interest exists.
Translated from the original German by Birte Twisselmann, PhD.
References
- 1.Behringer W, Buergi U, Christ M, Dodt C, Hogan B. Fünf Thesen zur Weiterentwicklung der Notfallmedizin in Deutschland, Österreich und der Schweiz. Notfall Rettungsmed. 2013;16:625–626. [Google Scholar]
- 2.Beivers A, Dodt C. Ökonomische Aspekte der ländlichen Notfallversorgung. Notfall Rettungsmed. 2014;17:190–198. [Google Scholar]
- 3.Köster C, Wrede S, Herrmann T, et al. Ambulante Notfallversorgung Analyse und Handlungsempfehlungen. Göttingen: AQUA-Institut. 2016 [Google Scholar]
- 4.IGES Institut. IGES Institut. Berlin: 2016. Ambulantes Potenzial in der stationären Notfallversorgung Projektphase II. Ergebnisbericht für das Zentralinstitut für die Kassenärztliche Versorgung in Deutschland. Stand: 19. Juli 2016. [Google Scholar]
- 5.Zimmermann M, Brokmann JC, Gräff I, Kumle B, Wilke P, Gries A. Zentrale Notaufnahme - Update 2016. Anaesthesist. 2016;65:243–249. doi: 10.1007/s00101-016-0142-y. [DOI] [PubMed] [Google Scholar]
- 6.Schmiedhofer M, Möckel M, Slagman A, Frick J, Ruhla S, Searle J. Patient motives behind low-acuity visits to the emergency department in Germany: a qualitative study comparing urban and rural sites. BMJ Open. 2016;6 doi: 10.1136/bmjopen-2016-013323. e013323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Pines JM, Hilton JA, Weber EJ, et al. International perspectives on emergency department crowding. Acad Emerg Med. 2011;18:1358–1370. doi: 10.1111/j.1553-2712.2011.01235.x. [DOI] [PubMed] [Google Scholar]
- 8.Pines JM, Mullins PM, Cooper JK, Feng LB, Roth KE. National trends in emergency department use, care patterns, and quality of care of older adults in the United States. J Am Geriatr Soc. 2013;61:12–17. doi: 10.1111/jgs.12072. [DOI] [PubMed] [Google Scholar]
- 9.Carter EJ, Pouch SM, Larson EL. The relationship between emergency department crowding and patient outcomes: a systematic review. J Nurs Scholarsh. 2014;46:106–115. doi: 10.1111/jnu.12055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bernstein SL, Aronsky D, Duseja R, et al. Society for academic emergency medicine, Emergency Department Crowding Task Force: the effect of emergency department crowding on clinically oriented outcomes. Acad Emerg Med. 2009;16:1–10. doi: 10.1111/j.1553-2712.2008.00295.x. [DOI] [PubMed] [Google Scholar]
- 11.Johnson KD, Winkelman C. The effect of emergency department crowding on patient outcomes: a literature review. Adv Emerg Nurs J. 2011;33:39–54. doi: 10.1097/TME.0b013e318207e86a. [DOI] [PubMed] [Google Scholar]
- 12.Uscher-Pines L, Pines J, Kellermann A, Gillen E, Mehrotra A. Deciding to visit the emergency department for non-urgent conditions: a systematic review of the literature. Am J Manag Care. 2013;19:47–59. [PMC free article] [PubMed] [Google Scholar]
- 13.Schellein O, Ludwig-Pistor F, Bremerich DH. [Manchester triage system Process optimization in the interdisciplinary emergency department] Anaesthesist. 2009;58:163–170. doi: 10.1007/s00101-008-1477-9. [DOI] [PubMed] [Google Scholar]
- 14.WONCA International Classification Committee. Oxford University Press. Oxford: 2005. ICPC-2-R: International classification of primary care. Revised 2nd edition. [Google Scholar]
- 15.Körner T, Saad A, Laux G, Rosemann T, Beyer M, Szecsenyi J. Die Episode als Grundlage der Dokumentation Eine episodenbezogene Patientenakte mit einer speziell für die Allgemeinmedizin entwickelten Klassifikation verbessert die Datenbasis in der hausärztlichen Versorgung. Dtsch Arztebl. 2005;102:A 3168–A 3172. [Google Scholar]
- 16.Brauns H, Steinmann S. Educational reform in france, West-Germany and the United Kingdom: updating the CASMIN Educational Classification. ZUMA-Nachrichten. 1999;44:7–44. [Google Scholar]
- 17.Campbell PA, Pai RK, Derksen DJ, Skipper B. Emergency department use by family practice patients in an academic health center. Fam Med. 1998;30:272–275. [PubMed] [Google Scholar]
- 18.Unwin M, Kinsman L, Rigby S. Why are we waiting? Patients‘ perspectives for accessing emergency department services with non-urgent complaints. Int Emerg Nurs. 2016;29:3–8. doi: 10.1016/j.ienj.2016.09.003. [DOI] [PubMed] [Google Scholar]
- 19.Kraaijvanger N, Rijpsma D, van Leeuwen H, Edwards M. Self-referrals in the emergency department: reasons why patients attend the emergency department without consulting a general practitioner first-a questionnaire study. Int J Emerg Med. 2015;8 doi: 10.1186/s12245-015-0096-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lowthian JA, Smith C, Stoelwinder JU, Smit DV, McNeil JJ, Cameron PA. Why older patients of lower clinical urgency choose to attend the emergency department. Intern Med J. 2013;43:59–65. doi: 10.1111/j.1445-5994.2012.02842.x. [DOI] [PubMed] [Google Scholar]
- 21.Somasundaram R, Geissler A, Leidel BA, Wrede CE. Beweggründe für die Inanspruchnahme von Notaufnahmen - Ergebnisse einer Patientenbefragung Stuttgart, New York. Thieme-Verlag; Gesundheitswesen. 2016 doi: 10.1055/s-0042-112459. [DOI] [PubMed] [Google Scholar]
- 22.Redstone P, Vancura JL, Barry D, Kutner JS. Nonurgent use of the emergency department. J Ambul Care Manage. 2008;31:370–376. doi: 10.1097/01.JAC.0000336555.54460.fe. [DOI] [PubMed] [Google Scholar]
- 23.Shesser R, Kirsch T, Smith J, Hirsch R. An analysis of emergency department use by patients with minor illness. Ann Emerg Med. 1991;20:743–748. doi: 10.1016/s0196-0644(05)80835-2. [DOI] [PubMed] [Google Scholar]
- 24.Sarver JH, Cydulka RK, Baker DW. Usual source of care and nonurgent emergency department use. Acad Emerg Med. 2002;9:916–923. doi: 10.1111/j.1553-2712.2002.tb02193.x. [DOI] [PubMed] [Google Scholar]
- 25.Northington WE, Brice JH, Zou B. Use of an emergency department by nonurgent patients. Am J Emerg Med. 2005;23:131–137. doi: 10.1016/j.ajem.2004.05.006. [DOI] [PubMed] [Google Scholar]
- 26.Gill JM, Riley AW. Nonurgent use of hospital emergency departments: urgency from the patient‘s perspective. J Fam Pract. 1996;42:491–496. [PubMed] [Google Scholar]
- 27.Durand AC, Palazzolo S, Tanti-Hardouin N, Gerbeaux P, Sambuc R, Gentile S. Nonurgent patients in emergency departments: rational or irresponsible consumers? Perceptions of professionals and patients. BMC Res Notes. 2012;5:525. doi: 10.1186/1756-0500-5-525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ruud SE, Hjortdahl P, Natvig B. Is it a matter of urgency? A survey of assessments by walk-in patients and doctors of the urgency level of their encounters at a general emergency outpatient clinic in Oslo, Norway. BMC Emerg Med. 2016;16 doi: 10.1186/s12873-016-0086-1. [DOI] [PMC free article] [PubMed] [Google Scholar]