Abstract
Objective
To review our experience and results in the diagnosis and treatment of urethral prolapse (UP) in Chinese girls.
Patients and methods
We conducted a retrospective chart review of 89 consecutive girls (aged <16 years) with UP and without other complications, who received treatment for UP from January 1999 to January 2015 (a study period of 16 years) at the Children’s Hospital of Chongqing Medical University, China. Data analysed included: age, symptoms, clinical findings, predisposing factors, management, and outcomes.
Results
The presenting symptoms in the 89 girls were: mass (54 girls), bleeding (34), and dysuria/straining at micturition (one). In all, 14 patients received conservative treatment as their symptoms were mild, and 75 were successfully treated by excision of the prolapsed urethral mucosa or ligation over a Foley catheter, as their symptoms were severe and recurred too frequently to be managed conservatively. The mean postoperative length of stay for ligation was 7.76 days and for excision was 4.57 days. Ligation over a Foley catheter had a longer hospital stay.
Conclusions
UP is a rare condition occurring in prepubertal girls, evidenced by a urethral mass and bleeding. Increased physician awareness and early recognition of UP avoids unnecessary examinations and patient anxiety.
Abbreviations: BMI, body mass index; FLACC, Face, Legs, Activity, Cry, Consolability (pain scale); UP, urethral prolapse
Keywords: Urethral prolapse, Girls, Management, China
Introduction
Urethral prolapse (UP) is a rare condition, evidenced by a circular protrusion of the distal urethra through the external meatus, and it was first described in 1732 by Solingen [1]. The exact incidence of UP is not well known, with a suggested incidence of one in 3000, and it occurs most often in prepubertal Black females and postmenopausal White women [2], [3], [4]. However, the rate of misdiagnosis is high because of the rare morbidity [5], [6]. Vaginal bleeding is the most common presenting symptom of UP and a perineal mass is often evident. Upon examination, a rounded ‘doughnut’-shaped mucosa can be seen protruding from the urethral opening and predisposing factors include: cough, trauma, and constipation. To date, to our knowledge, UP in prepubertal Chinese females has not been reported. The differential diagnoses of a urethral mass are broad, ranging from a simple urethral caruncle to rhabdomyosarcoma. Prolapse of a ureteric cyst, urethral or vaginal malignancy, ectopic ureterocele, condyloma are some common differential diagnosis. To date, published reports on UP have been predominantly in Black girls, with some reports in White girls, which suggest that UP occurs most often in January to July [7], [8]. The purpose of the present study was to summarise the clinical manifestation and physical examination findings of the medical records of Chinese girls with UP in order to identify opportunities to improve diagnosis and treatment of UP. Increased physician awareness and early recognition of UP should avoid unnecessary examinations and patient anxiety.
Patients and methods
Study design
This retrospective analysis involved the review of the medical records of 89 girls who received treatment for UP from January 1999 to January 2015 (a study period of 16 years) at the Children’s Hospital of Chongqing Medical University (Department of Urinary Surgery), the largest and one of the most famous child-care hospitals in southwestern China.
The inclusion criteria included all girls aged <16 years who had a diagnosis of UP. The exclusion criteria were: (i) no accurate pathological evidence of UP; (ii) concomitant other urinary tract malformation; and (iii) lost to follow-up (follow-up information was obtained through out-patient records and telephone interviews; 14 cases were lost to follow-up).
The management options were conservative treatment or surgery for all girls who had UP. Conservative therapy consisted of bed rest, sitz baths, local applications of antibiotic and steroid cream, antispasmodic drugs, decontamination of the urinary tract, and manipulative reduction. These conservative measures can sometimes shorten the process of UP and can also help avoid complications of ligation over a Foley catheter (uncomfortable feeling, partial recurrence, infection, postoperative pain).
Lack of response to conservative treatment or recurrence of UP (recurrence after conservative treatment was defined as a lump protruding from the urethra, genital haemorrhage and recurrence of pain) was an indication for surgery (surgical excision or ligation over a Foley catheter). Fig. 1 illustrates ligation over a Foley catheter.
Fig. 1.

The process of ligation over a Foley catheter. (A) diagram of UP. (B) Catheterisation with a Foley catheter, (C) the prolapsing mass is ‘slinged’ by suture. (D) Ligation over the Foley.
Data collection
Age, body mass index (BMI), season (seasons were defined as follows: Winter, December to February; Spring, March to May; Summer, June to August; and Autumn, September to November; to explore the variation in season, we estimated the mean number of cases diagnosed per season), symptoms, history (included their predisposing factors), physical examination, urine analysis, routine blood analysis, urine culture, and treatment methods (including conservative treatment and surgery) were reviewed. Responses to each therapy (including pain assessment) and follow-up (follow-up information was obtained through out-patient records and telephone interviews) were also recorded. The Face, Legs, Activity, Cry, Consolability (FLACC) pain scale [14] was used to evaluate pain and compared between the ligation and surgical excision groups.
Ethics
Ethics approval was not required as this research was conducted on previously collected non-identifiable information. Patients were identified via the electronic coding systems using both diagnostic and therapeutic codes for UP.
Statistics
Statistical analyses were performed using the Statistical Package for the Social Sciences (SPSS® software version 19.0; SPSS Inc., Chicago, IL, USA). Comparison between the ligation and surgical excision groups was performed using an independent-samples t-test. Differences with a P < 0.05 were considered statistically significant.
Results
Age at diagnosis
The mean (SD, range) of the girls was 6.8 (2.42, 0.92–12.7) years, with most being aged between 6 and 10 years (59/89). The age distribution of the girls at UP diagnosis is shown in Fig.2A.
Fig. 2.
(A) Age distribution of children at the time of diagnosis of UP. (B) BMI percentile of children with UP. (C) Seasonal distribution of UP. (D) Mass prolapsing from pudendal labia.
Predisposing factors
In all, 29 girls had varying degrees of malnutrition, nine were treated for UTIs, 17 had different degrees of cough (amongst them three were diagnosed with bronchial asthma), five were diagnosed with vulvitis, seven had a history of diarrhoea in the recent past, and three had constipation. The nine remaining girls did not have any obvious predisposing factors.
BMI percentile
The mean BMI was below the 50th percentile and only 6.7% of the girls were in the 90th percentile. There was an increase in the incidence of UP with a decrease in the BMI (Fig.2B).
Season of diagnosis
From 1999 onward, we found a tendency for a higher ratio of UP diagnosis in the spring (27/89), followed by the winter (23/89) (Fig.2C).
Symptoms and clinical findings
Most of the girls (54/89, 60.7%) were originally asymptomatic and the UP was noticed accidentally whilst bathing as a round, soft, and plain red coloured mass prolapsing from pudendal labia (Fig.2D). On examination, all had a 0.5–3 cm lump protruding from the urethra. The central urethral opening was clearly visible in all patients. In cases of uncertainty, a catheter was used to confirm that the meatus lay at the centre of the prolapsed mucosa. Genital haemorrhage was the second sign of UP (34/89). Bleeding was not often very profuse, and none needed blood transfusions because of intense bleeding. Urinary symptoms were less frequently experienced, with dysuria being the most common.
Management of UP
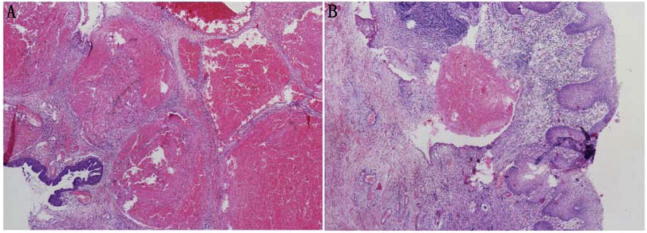
Conservative treatment was used in 14 girls for 3 days with good responses; whilst in the remaining 75 girls there was recurrence. Of the 75 recurrences, 55 were successfully treated by excision of the prolapsed urethral mucosa, and 20 were successfully treated by ligation over a Foley catheter. The histopathological appearance of the excised tissue was urethral mucosal congestion, oedema with infiltration of neutrophils, lymphocytes and plasma cells, and eosinophils were also seen. More submucous vascellum were seen and the congested lumens were obviously dilated (Fig. 3).
Fig. 3.
Postoperative histopathological appearance of UP.
The mean (range) length of hospital stay was 7.76 (5–12) days in girls that underwent ligation over a Foley catheter and 4.57 (1–7) days in the surgical excision group. Ligation over a Foley catheter had a high incidence of postoperative pain (16/20) using the FLACC [10] pain scale. The mean (range) pain scale score after ligation over a Foley catheter was 4.08 (2–7) vs 2.78 (1–6) after surgical excision (P < 0.05). Consequently, ligation over a Foley catheter was performed less year by year.
Follow-up
All the girls were reviewed at 1–16 years after treatment. There were no recurrences after ligation over a Foley catheter. No patient had partial reduction, urinary flow returned to normal and there were no complaints from patients according to the follow-up data.
Discussion
UP is a rare benign condition that involves the distal urethra, and it occurs most commonly in prepubertal Black girls and postmenopausal White women [9], [11]. The present series, to our knowledge, is the first to report on UP in Chinese girls. The exact cause of UP remains unknown; however, several theories have been proposed. A popular theory involves weak pelvic floor structures, such as inadequate pelvic attachments and urethral hypermobility. Other theories include: intrinsic abnormalities of the urethra (e.g. an abnormally patulous urethra, a wide urethra, and redundant mucosa), neuromuscular disorders, urethral malposition, submucosal weakness, or deficient elastic tissue.
Risk factors for UP in children include increased intra-abdominal pressure as a result of chronic coughing or constipation. The relationship between genital trauma and UP remains controversial. Previous studies reported that overweight children might be more susceptible to UP secondary to an elevated resting abdominal pressure [1], [11], [12]. Our present study found that most UPs occurred in girls with BMIs <50th percentile, and the incidence of UP increased with a lower BMI percentile. The reason for this is not clear, but may possibly be associated with rapid growth.
The association between season and UP occurrence is also not clear. Rudin et al. [4] reported that most UPs occurred in the summer. However, in our present series, UPs occurred most in the spring (30.34%), followed by winter (25.84%), then summer, and lastly autumn. Considering that some of the predisposing factors, e.g. cough, diarrhoea, have seasonal distributions may influence this seasonal trend in UP occurrence.
The most common presentation of UP is a mass, and the second is genital bleeding, which is often misdiagnosed by primary care practitioners [13]. The girls in the present study displayed the common presenting features of the condition, i.e. bleeding (34/89 patients), mass (54/89) and dysuria/straining at micturition (one of 89). Other presenting features include: ‘discharge’ and urinary retention. As described above, the classical appearance of UP (i.e. the ‘doughnut’ sign) enables the diagnosis to be made easily on clinical grounds alone [1], [10]. Occasionally, a catheter or instrument tip may be used to confirm that the meatus lies at the centre of the prolapsed tissue. All our present patients had the diagnosis confirmed on physical examination, although one patient required a general anaesthetic to allow this examination to take place.
The optimal method of management UP in children remains controversial. The treatment course depends on the ‘severity of symptoms’. Conservative therapy appears to be effective for most patients with mild symptoms. Where ‘mild’ symptoms translate as a smaller size of lump protruding from the urethra and less bleeding, whilst ‘severe’ tends to be related to bigger size, severer genital haemorrhage, and the prolapse with an appearance suggestive of vascular compromise (e.g. dusky or blueish discolouration of the mucosa). However, the effectiveness of conservative treatment is limited with high recurrence rates [1], [4]. Surgical resection has been recommended as an effective primary treatment strategy [3], [12], [15]. The present study confirms the low complication and recurrence rates with this technique. UP can be surgically managed in two ways: by ligation over a Foley catheter or excision of the prolapsed urethral mucosa. In our present study, operative management followed standard treatment strategies; however, the length of stay was much longer than in other series. This might be due to pain as stated. Surgical excision had a shorter hospital stay, lower cost, easy nursing, and less pain than ligation over a Foley catheter, which is therefore recommended in Chinese girls.
The present study is the first to report the diagnosis and treatment of UP in Chinese girls. Most patients in our present study were light and small for their age with BMIs <50th percentile. The results challenge the conclusions that being overweight may contribute to UP. Conservative therapy is effective for patients with mild symptoms, and surgical resection is a safe treatment option. Surgical management is more cost-effective, in that the condition is thus treated promptly with a single admission to hospital, whilst children managed conservatively may present repeatedly for medical attention. Fig. 4 summarises the present study.
Fig. 4.
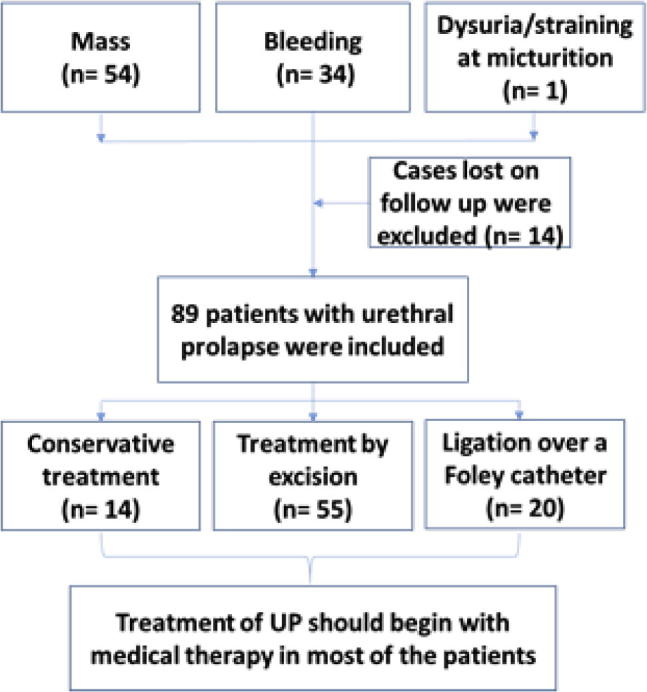
Summary of the study.
We acknowledge some limitations to assessing the management of the patients. The sample size is limited and there is the inherent bias of a retrospective study from a single centre. Whilst encouraging, we confirm our hypothesis that the basic data of season and response to different treatment (conservative treatment, ligation over a Foley catheter or excision) is different from other countries. This may help in improving the diagnosis and treatment of UP in our hospital, which should apply to all parts of China.
Conclusions
UP is a rare condition occurring in prepubertal girls, which results in a discernible mass and bleeding. UP treatment should begin with conservative therapy in most patients. A lack of response to conservative therapy or recurrence of UP would then indicate surgical intervention. The best results were obtained by complete excision of the UP.
Conflict of interest
The authors declare that they have no competing interests.
Funding
Supported by National Natural Science Foundation of China (No. 81370701, No. 81571425), Chongqing Municipal Education Commission of Science and Technology Research Project (KJ1600229).
Acknowledgements
Yi Wei and Shengde Wu conceived and designed the study, advised on the search, read and analysed documents, and drafted the paper. Tao Lin conducted the document search, read and analysed the documents, and revised the manuscript. Dawei He, Guanghui Wei and Xuliang Li conceived and designed the study, advised on the search, read and analysed documents, and edited the paper. All six authors take responsibility for the content of the paper.
Supported by the National Natural Science Foundation of China (No. 81070475, No. 81100414, No. 30872706) and Chongqing Science and Technology Commission (CSTC, 2011BA5036).
Pediatric Urology
Footnotes
Peer review under responsibility of Arab Association of Urology.
References
- 1.Valerie E., Gilchrist B.F., Frischer J., Scriven R., Klotz D.H., Ramenofsky M.L. Diagnosis and treatment of urethral prolapse in children. Urology. 1999;54:1082–1084. doi: 10.1016/s0090-4295(99)00311-8. [DOI] [PubMed] [Google Scholar]
- 2.Hillyer S., Mooppan U., Kim H., Gulmi F. Diagnosis and treatment of urethral prolapse in children: experience with 34 cases. Urology. 2009;73:1008–1011. doi: 10.1016/j.urology.2008.10.063. [DOI] [PubMed] [Google Scholar]
- 3.Holbrook C., Misra D. Surgical management of urethral prolapse in girls: 13 years’ experience. BJU Int. 2012;110:132–134. doi: 10.1111/j.1464-410X.2011.10752.x. [DOI] [PubMed] [Google Scholar]
- 4.Rudin J.E., Geldt V.G., Alecseev E.B. Prolapse of urethral mucosa in white female children: experience with 58 cases. J Pediatr Surg. 1997;32:423–425. doi: 10.1016/s0022-3468(97)90596-0. [DOI] [PubMed] [Google Scholar]
- 5.Ballouhey Q., Abbo O., Sanson S., Cochet T., Galinier P., Pienkowski C. Urogenital bleeding revealing urethral prolapse in a prepubertal girl. Gynecol Obstet Fertil. 2013;41:404–406. doi: 10.1016/j.gyobfe.2013.04.006. [DOI] [PubMed] [Google Scholar]
- 6.Aprile A., Ranzato C., Rizzotto M.R., Arseni A., Da Dalt L., Facchin P. “Vaginal” bleeding in prepubertal age: a rare scaring riddle, a case of the urethral prolapse and review of the literature. Forensic Sci Int. 2011;210:e16–e20. doi: 10.1016/j.forsciint.2011.04.017. [DOI] [PubMed] [Google Scholar]
- 7.Vunda A., Vandertuin L., Gervaix A. Urethral prolapse: an overlooked diagnosis of urogenital bleeding in pre-menarcheal girls. J Pediatr. 2011;158:682–683. doi: 10.1016/j.jpeds.2010.11.050. [DOI] [PubMed] [Google Scholar]
- 8.Quinlan M.P. Urethral prolapse in a premenarchal Asian girl. Obstet Gynecol. 2009;113:1174. doi: 10.1097/AOG.0b013e3181a3d271. [DOI] [PubMed] [Google Scholar]
- 9.Jerkins G.R., Verheeck K., Noe H.N. Treatment of girls with urethral prolapse. J Urol. 1984;132:732–733. doi: 10.1016/s0022-5347(17)49845-4. [DOI] [PubMed] [Google Scholar]
- 10.Lowe F.C., Hill G.S., Jeffs R.D., Brendler C.B. Urethral prolapse in children: insights into etiology and management. J Urol. 1986;135:100–103. doi: 10.1016/s0022-5347(17)45530-3. [DOI] [PubMed] [Google Scholar]
- 11.Sugerman H., Windsor A., Bessos M., Kellum J., Reines H., DeMaria E. Effects of surgically induced weight loss on urinary bladder pressure, sagittal abdominal diameter and obesity co-morbidity. Int J Obes Relat Metab Disord. 1998;22:230–235. doi: 10.1038/sj.ijo.0800574. [DOI] [PubMed] [Google Scholar]
- 12.Ballouhey Q., Galinier P., Gryn A., Grimaudo A., Pienkowski C., Fourcade L. Benefits of primary surgical resection for symptomatic urethral prolapse in children. J Pediatr Urol. 2014;10:94–97. doi: 10.1016/j.jpurol.2013.06.011. [DOI] [PubMed] [Google Scholar]
- 13.Anveden-Hertzberg L., Gauderer M.W., Elder J.S. Urethral prolapse: an often misdiagnosed cause of urogenital bleeding in girls. Pediatr Emerg Care. 1995;11:212–214. doi: 10.1097/00006565-199508000-00004. [DOI] [PubMed] [Google Scholar]
- 14.Nilsson S., Finnström B., Kokinsky E. The FLACC behavioral scale for procedural pain assessment in children aged 5–16 years. Paediatr Anaesth. 2008;18:767–774. doi: 10.1111/j.1460-9592.2008.02655.x. [DOI] [PubMed] [Google Scholar]
- 15.Chiba M., Toki A., Sugiyama A., Suganuma R., Osawa S., Ishii R. Urethral caruncle in a 9-year-old girl: a case report and review of the literature. J Med Case Rep. 2015;9:71. doi: 10.1186/s13256-015-0518-7. [DOI] [PMC free article] [PubMed] [Google Scholar]