Abstract
Optimization of medical therapy during discharge planning is vital for improving patient outcomes after hospitalization for acute myocardial infarction (AMI). However, limited information is available about recent trends in the prescribing of evidence-based medical therapies in these patients, especially from a population-based perspective. We describe decade-long trends in the discharge prescribing of aspirin, angiotensin-converting enzyme inhibitors/ angiotensin receptor blockers, β-blockers, and statins in hospital survivors of AMI. The study population consisted of 5,253 patients who were discharged from all 11 hospitals in central Massachusetts after AMI in 6 biennial periods between 2001 and 2011. Combination medical therapy (CMT) was defined as the prescription of all 4 cardiac medications at hospital discharge. The average age of this patient population was 69.2 years and 57.7% were men. Significant increases were observed in the use of CMT, from 25.6% in 2001 to 48.7% in 2011, with increases noted for each of the individual cardiac medications examined. Subgroup analysis also showed improvement in discharge prescriptions for P2Y12 inhibitors in patients who underwent a percutaneous coronary intervention (PCI). Presence of a do not resuscitate order, prior co-morbidities, hospitalization for NSTEMI, admission to a non-teaching hospital, and failure to undergo cardiac catheterization or a PCI were associated with underuse of CMT. In conclusion, our study demonstrates encouraging trends in the prescribing of evidence- based medications at hospital discharge for AMI. However, certain patient subgroups continue to be at risk for underuse of CMT, suggesting the need for strategies to enhance compliance with current practice guidelines.
Keywords: population-based study, hospital discharge medications, acute myocardial infarction
INTRODUCTION
The purpose of this community-wide observational study was to describe decade-long (2001–2011) trends in the prescribing of individual effective cardiac medications and combination medical therapy among patients discharged from all 11 medical centers in central Massachusetts after acute myocardial infarction (AMI); trends in discharge prescriptions for P2Y12 inhibitors in patients with AMI undergoing a percutaneous coronary intervention during this period are separately reported. We also examined several sociodemographic and clinical factors associated with the underuse of combination medical therapy. Data from the population-based Worcester Heart Attack Study were used for purposes of this investigation1–4.
METHODS
Residents of the Worcester, Massachusetts, metropolitan area hospitalized with a primary or secondary discharge diagnosis of AMI (International Classification of Diseases, Ninth Revision, code 410) from all Worcester Standard Metropolitan Statistical Area hospitals during 2001, 2003, 2005, 2007, 2009, and 2011 comprised the present study population. This study is part of an ongoing population-based investigation examining trends in hospital incidence and case-fatality rates among residents of the Worcester metropolitan area hospitalized with confirmed AMI at all 11 central Massachusetts medical centers 1–4. Although additional earlier study years were included, we restricted this study sample to patients hospitalized with validated AMI in the 2000’s and beyond for purposes of examining relatively contemporary, decade-long, trends in hospital medication practices. This period was also selected to capture the introduction of angiotensin receptor blockers (ARBs) and newer P2Y12 inhibitors to clinical practice in the early and mid-2000’s. These central Massachusetts medical centers included 3 tertiary care centers (teaching hospital) and 8 community hospitals (non-teaching hospital).
The medical records of residents of the Worcester metropolitan area with a discharge diagnosis of AMI from all 11 central Massachusetts hospitals were individually reviewed. The diagnosis of AMI was validated according to pre-established diagnostic criteria based on patient’s acute presenting symptoms, serum enzyme and biomarker findings, and serial electrocardiographic tracings during hospitalization typical of AMI 1–4. All autopsy-proven cases of AMI were included irrespective of the other criteria. Cases of perioperative-associated AMI were not included. The various complications of AMI, including atrial fibrillation, heart failure, and cardiogenic shock were assessed based on information available from clinical charts 1–7.
The medications of interest in this investigation included aspirin, angiotensin converting enzyme (ACE) inhibitors/ ARBs, β-blockers, and statins; combination medical therapy (CMT) was defined as the hospital prescription of all 4 cardiac medications. The use of P2Y12 inhibitors (e.g., clopidogrel, prasugrel, or ticagrelor) in patients who underwent a percutaneous coronary intervention (PCI) (in those with and without concurrent use of anticoagulants) was also separately explored.
The hospital records of patients with validated AMI were abstracted for demographic, medical history, and clinical data. This included information about patient’s age, sex, medical history, occurrence of several clinical complications during hospitalization, and AMI order (initial vs. prior) and type (Q wave or non–Q wave, ST segment elevation (STEMI) and non-ST segment elevation AMI (NSTEMI) 8. Information about the prescribing of cardiac medications at the time of hospital discharge was obtained through the review of hospital medical records and physician’s and nurse’s progress notes 9,10.
Changes over time in the proportion of patients treated with different cardiac medications, both individually and as CMT, were examined through the use of chi square tests for trends. A modified Poisson multiple regression approach with a sandwich error term was used to examine demographic medical history, and clinical factors associated with the receipt of CMT with multivariable adjusted relative risks and accompanying 95% confidence intervals calculated.
RESULTS
During the period under study (2001–2011), a total of 5,253 patients were discharged from all 11 hospitals in central Massachusetts after a confirmed AMI. This included 1,089 patients in 2001, 1,056 during 2003, 816 in 2005, 818 in 2007, 735 in 2009, and 739 in 2011, respectively. The mean age of these patients was 69.2 years, 57.7% were men, and in approximately two thirds it was their first AMI.
Overall, aspirin was prescribed to 87.0% of patients discharged after AMI, ACE inhibitors/ ARBs to 62.0%, β-blockers to 85.6%, and statins to 74.3%; all 4 cardiac medications were prescribed as CMT to 44.0% of discharged patients.
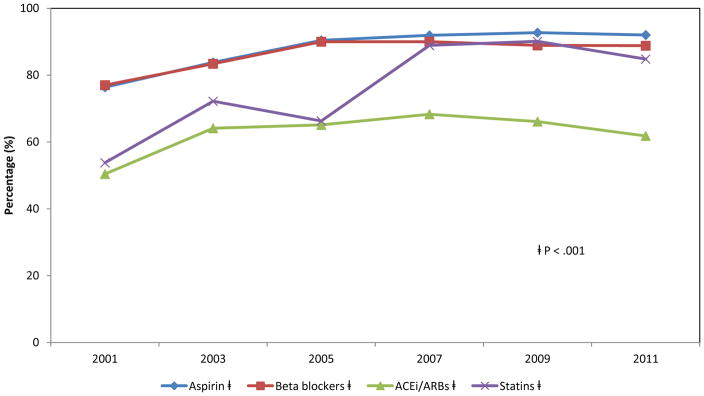
There was a significant and relatively consistent increase in the prescribing of each of the cardiac medications examined (p<0.05) (Figure 1). Prescriptions for aspirin increased from 76.4% in 2001 to 92.0% in 2011, ACE inhibitors/ ARBs increased from 50.4% to 61.8%, β-blockers increased from 77.0% to 88.8%, and statins increased from 53.8% to 84.8%, respectively (Figure 1). Marked increases in the prescribing of aspirin (69.5% in 2001 to 88.3% in 2011), ACE inhibitors/ARBs (40.9% to 48.5%), β-blockers (68.5% to 86.1%), and statins (38.7% to 76.1%) were observed in those who were not on these therapies previously whereas lesser increases between 2001 and 2011 were observed with regards to prescriptions for aspirin (85.7% to 95.7%), ACE inhibitors/ARBs (70.8% to 79.9%), β-blockers (88.5% to 91.4%), and statins (88.5% to 91.6%) for patients who were on these agents previously.
Figure 1.
Decade long trends in the prescribing of evidence-based cardiac medications in patients with acute myocardial infarction at the time of hospital discharge (Worcester Heart Attack Study)
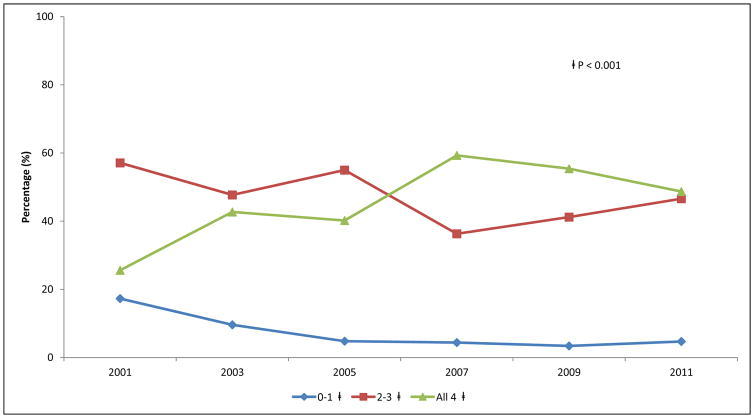
We observed considerable increases in the utilization of CMT over time, from 25.6% in 2001 to 48.7% in 2011 (p<0.001). These increases were particularly marked for patients who were not previously on these medications (22.5% in 2001 vs. 45.1% in 2011 ) with no increases observed among those who were on these multiple treatment regimens previously (68.5% in 2001 vs. 66.7% in 2011). The proportion of patients with prescriptions for 0–1 cardiac medication declined from 17.3% in 2001 to 4.7% in 2011 (Figure 2). Discharge prescriptions for P2Y12 inhibitors increased over time from 85.5% of post PCI patients in 2001 to 94.8% in 2011 (p<0.001).
Figure 2.
Decade long trends in the prescribing of 0–1, 2–3, and all 4 (CMT) evidence- based cardiac medications in patients with acute myocardial infarction at the time of hospital discharge (Worcester Heart Attack Study)
We examined differences in several socio-demographic and clinical characteristics between those who were prescribed 0–1, 2–3, and all 4 cardiac medications (Table 1). Patients prescribed 0–1 medication were more likely to be older, female, with an active do not resuscitate (DNR) order, have Medicare or belong to an HMO as their primary insurance, and have been admitted to a non-teaching medical center in central Massachusetts. They were more likely to have had multiple co-morbidities previously diagnosed and were more likely to have developed an NSTEMI. Patients who were prescribed 0–1 medication were less likely to have received coronary revascularization procedures and were more likely to have experienced multiple in-hospital complications prior to discharge. These patients were also more likely to have had a worse hemodynamic profile and physiologic/laboratory findings at the time of hospital admission as well as to have experienced a longer hospital stay in comparison with other medication groups (Table 1).
Table 1.
Characteristics of patients with acute myocardial infarction (AMI) according to the number of 4 evidence-based cardiac medications prescribed at the time of hospital discharge (Worcester Heart Attack Study)
| Number of Medications | ||||
|---|---|---|---|---|
|
| ||||
| Characteristic | 0 or 1 | 2 or 3 | All 4 | P value |
|
| ||||
| (n=424) | (n=2,519) | (n=2,310) | ||
| Age (mean, years) | 73.4 | 70.8 | 66.8 | <0.001 |
| Body mass index (mean) (Kg/m2) | 26.7 | 27.8 | 28.6 | <0.001 |
| Men | 56.8% | 55.2% | 60.5% | <0.01 |
| White | 91.8% | 89.7% | 89.4% | 0.32 |
| Do not resuscitate order present | 30.0% | 22.1% | 13.1% | <0.001 |
| Teaching hospital | 69.3 % | 91.9 % | 95.2 % | <.001 |
| Insurance status | ||||
| Self | 5.5% | 4.5% | 6% | <0.001 |
| Blue-cross/Private | 8.3% | 12.0% | 16.2% | |
| Medicaid | 1.7% | 3.5% | 4.4% | |
| Medicare | 42.0% | 38.2% | 33.3% | |
| Health maintenance organization | 42.5% | 41.9% | 40.1% | |
| Initial myocardial infarction | 70.5% | 65.0% | 63.8% | <0.05 |
| ST segment elevation myocardial infarction (%) | 23.6% | 26.8% | 38.4% | <0.001 |
| Angina pectoris | 14.4% | 16.5% | 12.2% | <0.001 |
| Chronic obstructive pulmonary disease | 26.9% | 17.6% | 14.3% | <0.001 |
| Diabetes mellitus | 27.8% | 33.1% | 37.2% | <0.001 |
| Heart failure | 28.3% | 24.5% | 19.2% | <0.001 |
| Hypertension | 67.5% | 73.1% | 75.2% | 0.003 |
| Renal disease | 20.8% | 21.8% | 16.4% | <0.001 |
| Stroke | 14.9% | 11.6% | 9.5% | <0.01 |
| Index Procedures | ||||
| Cardiac Catheterization | 28.5% | 59.8% | 77.1% | <0.001 |
| Percutaneous coronary intervention | 11.1% | 36.9% | 62.3% | <0.001 |
| Coronary artery bypass grafting | 6.4% | 11.3% | 1.9% | <0.001 |
| Atrial fibrillation | 25% | 21.2% | 14.4% | <0.001 |
| Cardiogenic shock | 4.7% | 3.3% | 3.0% | 0.21 |
| Heart failure | 41.0 % | 36.8% | 31.6% | <0.001 |
| Stroke | 2.6% | 1.7% | 0.7% | <0.001 |
| Length of stay, mean (days) | 5.9 | 6.1 | 4.6 | <0.001 |
| Admission lab findings (mean) | ||||
| Estimated glomerular filtration rate (ml/min/1.73m2) | 53.1 | 55.3 | 60.7 | <0.001 |
| Serum cholesterol (mg/dl) | 167.2 | 171.1 | 171.7 | 0.49 |
| Systolic blood pressure (mmHg) | 137.8 | 142.1 | 144.3 | <0.001 |
| Diastolic blood pressure (mmHg) | 75.0 | 76.4 | 80.0 | <0.001 |
After controlling for a variety of demographic and clinical factors that could affect physician’s prescribing practices, patients who were not prescribed CMT were significantly more likely to have had an active DNR order, to be admitted to a central Massachusetts community (non-teaching) hospital, have several co-morbidities previously diagnosed (e.g., COPD, MI, renal disease), but not diabetes or hypertension, and were more likely to have presented with an NSTEMI. Patients failing to receive CMT were less likely to have undergone cardiac catheterization or a PCI, but were significantly more likely to have undergone CABG surgery, to have developed an acute stroke but not heart failure, to have a relatively shorter hospital stay, and were less likely to have been treated during the most recent study years (Table 2).
Table 2.
Multivariable adjusted regression analysis of factors associated with prescription of combination medical therapy among patients discharged after hospitalization for acute myocardial infarction (Worcester Heart Attack Study)
| Characteristics | Odds ratio |
|---|---|
| Age (years) | |
| 55–64 | 0.97 |
| (0.89,1.05) * | |
| 65–74 | 0.92 ( |
| 0.84,1.00) | |
| ≥75 | 0.94 |
| (0.86,1.03) | |
| Male | 1.01 |
| (0.95,1.08) | |
| White | 1.07 |
| (0.97,1.17) | |
| Do not resuscitate order | 0.85 |
| (0.76,0.95) | |
| Teaching hospital | 1.35 |
| (1.14,1.60) | |
| Insurance | |
| Blue cross/Private | 0.95 |
| (0.84,1.08) | |
| Medicaid | 0.90 |
| (0.76,1.07) | |
| Medicare | 0.94 |
| (0.83,1.06) | |
| Health maintenance organization | 0.89 |
| (0.79,1.00) | |
| ST segment elevation myocardial infarction | 1.18 |
| (1.11,1.26) | |
| Initial myocardial infarction | 0.87 |
| (0.81,0.92) | |
| Angina pectoris | 0.95 |
| (0.86,1.05) | |
| Chronic obstructive pulmonary disease | 0.88 |
| (0.81,0.96) | |
| Diabetes mellitus | 1.20 |
| (1.13,1.27) | |
| Heart failure | 0.94 |
| (0.86,1.02) | |
| Hypertension | 1.16 |
| (1.08,1.24) | |
| Renal disease | 0.86 |
| (0.78,0.94) | |
| Stroke | 0.97 |
| (0.88,1.08) | |
| Index Procedures | |
| Cardiac Catheterization | 1.31 |
| (1.17,1.47) | |
| Percutaneous coronary intervention | 1.24 |
| (1.14,1.36) | |
| Coronary artery bypass grafting | 0.28 |
| (0.21,0.38) | |
| Atrial fibrillation | 0.92 |
| (0.84,1.01) | |
| Cardiogenic shock | 0.84 |
| (0.70,1.02) | |
| Heart failure | 1.15 |
| (1.07,1.24) | |
| Stroke | 0.60 |
| (0.40,0.91) | |
| Length of stay | 1.02 |
| (1.01,1.03) | |
95% confidence intervals
Referent categories: Age <55 years, women, non-white race, absence of do not resuscitate order, non teaching hospital, self-pay (insurance), initial MI, NSTEMI, absence of selected co-morbidities, lack of receipt of selected procedures during index hospitalization, absence of specific complications during current hospitalization.
DISCUSSION
Our findings suggest that the prescribing of a number of evidence- based cardiac medications has improved substantially among patients who were discharged from the hospital after an AMI. However, several subgroups of patients were found to be at greater risk of not being prescribed CMT during the years under study.
The role of several cardiac medications, including aspirin, ACE inhibitors/ ARBs, β-blockers, and statins in the secondary prevention of AMI has been well established 11–19. Current recommendations for patients who develop an acute coronary syndrome include routine prescriptions for the cardiac medications that we examined at the time of hospital discharge, unless contraindicated 20, 21. These guidelines recommend that even patients with initial contraindications to several of these medications should be re-evaluated to determine their eligibility prior to hospital discharge and to continue treatment thereafter if these medications can be tolerated 20,21.
In the National Registry of Myocardial Infarction, significant increases were observed in the use of aspirin, ACE inhibitors, and β-blockers in more than 1.5 million patients hospitalized with AMI between 1990 and 1999 22. Other studies that have examined trends in the treatment and outcomes of patients with AMI using Medicare, National Hospital Discharge Survey, and Get with the Guidelines Registry data had also observed that the use of these medications increased significantly over time, leading to reductions in 30-day death rates 23–25.
The encouraging trends in medication prescribing practices that we observed are due to a multiplicity of factors including greater accumulation of supportive evidence for the use of these medications over time and improved understanding and emphasis by physicians about the importance of these therapies for secondary disease prevention; enhanced reliance on critical care pathways and other quality improvement tools that are available to aid in the implementation of practice guidelines have also likely contributed to these trends 26–28. However, gaps persist in prescriptions for CMT. It remains important to identify patient, physician, and health system factors associated with the failure to prescribe CMT to enhance the treatment of these patients.
Our previous study of residents of the Worcester metropolitan area hospitalized with AMI in the 1990s observed that advanced age and several clinical factors were independently associated with the underuse of CMT29. Several prior studies had also noted that the elderly, among other risk groups, continue to be treated less aggressively with evidence- based therapies in the setting of AMI as compared with younger patients. The lack of association of age, gender, and race with CMT in the current study may suggest that such treatment disparities have improved over time.
Patients with a DNR order and those with several co-morbidities were less likely to have received discharge prescriptions for CMT than respective comparison groups. In the National Registry of Myocardial Infarction 30, patients with STEMI received these beneficial cardiac medications at rates higher than for those hospitalized with NSTEMI. Patients who underwent CABG surgery during hospitalization, those who developed an acute stroke, patients with a relatively shorter duration of hospitalization, those hospitalized at non-teaching medical centers and during early study years were at significantly lower odds of being prescribed CMT than respective comparison groups.
The strengths of this study include the large number of patients discharged after hospitalization for AMI at all medical centers in central Massachusetts and examination of trends in medication prescribing practices over a decade long period. Several limitations, however, need to be kept in mind in interpreting these results. We did not have documentation on contraindications for the medications under study, whether guideline-based recommended dosages were used, and the reasons why certain medications were not prescribed in individual patients. Additionally, we did not have information on the impact of prescribing CMT on patients’ long-term compliance or other changes in their health related behavior after hospital discharge.
Acknowledgments
We wish to express our appreciation to all persons involved in the review of data for this project during the years under study. This study was made possible through the cooperation of the administration, medical records, and cardiology departments of participating Worcester metropolitan area hospitals.
Funding Sources: Grant support for this project was provided by the National Heart, Lung, and Blood Institute (RO1 HL35434). Dr. McManus’ effort was funded by NIH grant KL2RR031981 and Drs. McManus, Gore, and Goldberg’s effort was supported in part by funding from the National Heart, Lung and Blood Institute U01HL105268. Mr. Erskine’s effort was supported by NHLBI grant 1T32HL120823-01.
References
- 1.Goldberg RJ, Gore JM, Alpert JS, Dalen JE. Recent changes in attack and survival rates of acute myocardial infarction (1975 through 1981). The Worcester Heart Attack Study. JAMA. 1986;255:2774–2779. [PubMed] [Google Scholar]
- 2.Goldberg RJ, Gore JM, Alpert JS, Dalen JE. Incidence and case fatality rates of acute myocardial infarction (1975–1984): the Worcester Heart Attack Study. Am Heart J. 1988;115:761–767. doi: 10.1016/0002-8703(88)90876-9. [DOI] [PubMed] [Google Scholar]
- 3.Goldberg RJ, Yarzebski J, Lessard D, Gore JM. A two-decades (1975 to 1995) long experience in the incidence, in-hospital and long-term case-fatality rates of acute myocardial infarction: a community-wide perspective. J Am Coll Cardiol. 1999;33:1533–1539. doi: 10.1016/s0735-1097(99)00040-6. [DOI] [PubMed] [Google Scholar]
- 4.Floyd KC, Yarzebski J, Spencer FA, Lessard D, Dalen JE, Alpert JS, Gore JM, Goldberg RJ. A 30-year perspective (1975–2005) into the changing landscape of patients hospitalized with initial acute myocardial infarction: Worcester Heart Attack Study. Circ Cardiovasc Qual Outcomes. 2009;2:88–95. doi: 10.1161/CIRCOUTCOMES.108.811828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.McManus DD, Saczynski JS, Lessard D, Kinno M, Pidikiti R, Esa N, Harrington J, Goldberg RJ. Recent trends in the incidence, treatment, and prognosis of patients with heart failure and atrial fibrillation (the Worcester Heart Failure Study) Am J Cardiol. 2013;111:1460–1465. doi: 10.1016/j.amjcard.2013.01.298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Goldberg RJ, Spencer FA, Gore JM, Lessard D, Yarzebski J. Thirty year trends (1975–2005) in the magnitude of, management of, and hospital death rates associated with cardiogenic shock in patients with acute myocardial infarction: A population-based perspective. Circulation. 2009;119:1211–1219. doi: 10.1161/CIRCULATIONAHA.108.814947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.McManus DD, Huang W, Domakonda KV, Ward J, Saczynski JS, Gore JM, Goldberg RJ. Trends in atrial fibrillation in patients hospitalized with an acute coronary syndrome. Am J Med. 2012;125:1076–1084. doi: 10.1016/j.amjmed.2012.05.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.McManus DD, Gore J, Yarzebski J, Spencer F, Lessard D, Goldberg RJ. Recent trends in the incidence, treatment, and outcomes of patients with STEMI and NSTEMI. Am J Med. 2011;124:40–47. doi: 10.1016/j.amjmed.2010.07.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Spencer F, Scleparis G, Goldberg RJ, Yarzebski J, Lessard D, Gore JM. Decade-long trends (1986 to 1997) in the medical treatment of patients with acute myocardial infarction: A community-wide perspective. Am Heart J. 2001;142:594–603. doi: 10.1067/mhj.2001.117776. [DOI] [PubMed] [Google Scholar]
- 10.Fornasini M, Yarzebski J, Chiriboga D, Lessard D, Spencer FA, Aurigemma P, Gore JM, Goldberg RJ. Contemporary trends in evidence-based treatment for acute myocardial infarction. Am J Med. 2010;123:166–172. doi: 10.1016/j.amjmed.2009.06.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Yusuf S, Sleight P, Pogue J, Bosch J, Davies R, Dagenais G. Effects of an angiotensin-converting-enzyme inhibitor, ramipril, on cardiovascular events in high-risk patients. The Heart Outcomes Prevention Evaluation Study Investigators. N Engl J Med. 2000;342:145–153. doi: 10.1056/NEJM200001203420301. [DOI] [PubMed] [Google Scholar]
- 12.A randomized trial of propranolol in patients with acute myocardial infarction. I. Mortality results. JAMA. 1982;247:1707–1714. doi: 10.1001/jama.1982.03320370021023. [DOI] [PubMed] [Google Scholar]
- 13.Freemantle N, Cleland J, Young P, Mason J, Harrison J. Beta Blockade after myocardial infarction: systematic review and meta regression analysis. BMJ. 1999;318:1730–1737. doi: 10.1136/bmj.318.7200.1730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Cannon CP, Steinberg BA, Murphy SA, Mega JL, Braunwald E. Meta-analysis of cardiovascular outcomes trials comparing intensive versus moderate statin therapy. J Am Coll Cardiol. 2006;48:438–445. doi: 10.1016/j.jacc.2006.04.070. [DOI] [PubMed] [Google Scholar]
- 15.Cholesterol Treatment Trialists C. Baigent C, Blackwell L, Emberson J, Holland LE, Reith C, Bhala N, Peto R, Barnes EH, Keech A, Simes J, Collins R. Efficacy and safety of more intensive lowering of LDL cholesterol: a meta-analysis of data from 170,000 participants in 26 randomised trials. Lancet. 2010;376:1670–1681. doi: 10.1016/S0140-6736(10)61350-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Antithrombotic Trialists C. Collaborative meta-analysis of randomised trials of antiplatelet therapy for prevention of death, myocardial infarction, and stroke in high risk patients. BMJ. 2002;324:71–86. doi: 10.1136/bmj.324.7329.71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Schomig A, Neumann FJ, Kastrati A, Schuhlen H, Blasini R, Hadamitzky M, Walter H, Zitzmann-Roth EM, Richardt G, Alt E, Schmitt C, Ulm K. A randomized comparison of antiplatelet and anticoagulant therapy after the placement of coronary-artery stents. N Engl J Med. 1996;334:1084–1089. doi: 10.1056/NEJM199604253341702. [DOI] [PubMed] [Google Scholar]
- 18.Smith SC, Jr, Benjamin EJ, Bonow RO, Braun LT, Creager MA, Franklin BA, Gibbons RJ, Grundy SM, Hiratzka LF, Jones DW, Lloyd-Jones DM, Minissian M, Mosca L, Peterson ED, Sacco RL, Spertus J, Stein JH, Taubert KA World Heart F the Preventive Cardiovascular Nurses A. AHA/ACCF Secondary Prevention and Risk Reduction Therapy for Patients with Coronary and other Atherosclerotic Vascular Disease: 2011 update: a guideline from the American Heart Association and American College of Cardiology Foundation. Circulation. 2011;124:2458–2473. doi: 10.1161/CIR.0b013e318235eb4d. [DOI] [PubMed] [Google Scholar]
- 19.Yan AT, Yan RT, Tan M, Huynh T, Soghrati K, Brunner LJ, DeYoung P, Fitchett DH, Langer A, Goodman SG Canadian ACSRI. Optimal medical therapy at discharge in patients with acute coronary syndromes: temporal changes, characteristics, and 1-year outcome. Am Heart J. 2007;154:1108–1115. doi: 10.1016/j.ahj.2007.07.040. [DOI] [PubMed] [Google Scholar]
- 20.O’Gara PT, Kushner FG, Ascheim DD, Casey DE, Jr, Chung MK, de Lemos JA, Ettinger SM, Fang JC, Fesmire FM, Franklin BA, Granger CB, Krumholz HM, Linderbaum JA, Morrow DA, Newby LK, Ornato JP, Ou N, Radford MJ, Tamis-Holland JE, Tommaso CL, Tracy CM, Woo YJ, Zhao DX, Anderson JL, Jacobs AK, Halperin JL, Albert NM, Brindis RG, Creager MA, DeMets D, Guyton RA, Hochman JS, Kovacs RJ, Kushner FG, Ohman EM, Stevenson WG, Yancy CW American College of Cardiology Foundation/American Heart Association Task Force on Practice G. 2013 ACCF/AHA guideline for the management of ST-elevation myocardial infarction: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Circulation. 2013;127:e362–425. doi: 10.1161/CIR.0b013e3182742cf6. [DOI] [PubMed] [Google Scholar]
- 21.Amsterdam EA, Wenger NK, Brindis RG, Casey DE, Jr, Ganiats TG, Holmes DR, Jr, Jaffe AS, Jneid H, Kelly RF, Kontos MC, Levine GN, Liebson PR, Mukherjee D, Peterson ED, Sabatine MS, Smalling RW, Zieman SJ, Members AATF. 2014 AHA/ACC guideline for the management of patients with non-ST-elevation acute coronary syndromes: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation. 2014;130:2354–2394. doi: 10.1161/CIR.0000000000000133. [DOI] [PubMed] [Google Scholar]
- 22.Rogers WJ, Canto JG, Lambrew CT, Tiefenbrunn AJ, Kinkaid B, Shoultz DA, Frederick PD, Every N. Temporal trends in the treatment of over 1. 5 million patients with myocardial infarction in the US from 1990 through 1999: the National Registry of Myocardial Infarction 1, 2 and 3. J Am Coll Cardiol. 2000;36:2056–2063. doi: 10.1016/s0735-1097(00)00996-7. [DOI] [PubMed] [Google Scholar]
- 23.Heidenreich PA, McClellan M. Trends in treatment and outcomes for acute myocardial infarction: 1975–1995. Am J Med. 2001;110:165–174. doi: 10.1016/s0002-9343(00)00712-9. [DOI] [PubMed] [Google Scholar]
- 24.Somma KA, Bhatt DL, Fonarow GC, Cannon CP, Cox M, Laskey W, Peacock WF, Hernandez AF, Peterson ED, Schwamm L, Saxon LA. Guideline adherence after ST-segment elevation versus non-ST segment elevation myocardial infarction. Circ Cardiovasc Qual Outcomes. 2012;5:654–661. doi: 10.1161/CIRCOUTCOMES.111.963959. [DOI] [PubMed] [Google Scholar]
- 25.Goldberg RJ, Spencer FA, Steg PG, Flather M, Montalescot G, Gurfinkel EP, Kennelly BM, Goodman SG, Dedrick R, Gore JM Global Registry of Acute Coronary Events I. Increasing use of single and combination medical therapy in patients hospitalized for acute myocardial infarction in the 21st century: a multinational perspective. Arch Intern Med. 2007;167:1766–1773. doi: 10.1001/archinte.167.16.1766. [DOI] [PubMed] [Google Scholar]
- 26.Rogers AM, Ramanath VS, Grzybowski M, Riba AL, Jani SM, Mehta R, De Franco AC, Parrish R, Skorez S, Baker PL, Faul J, Chen B, Roychoudhury C, Elma MA, Mitchell KR, Froehlich JB, Montoye C, Eagle KA American College of Cardiology Foundation Bethesda MD. The association between guideline-based treatment instructions at the point of discharge and lower 1-year mortality in Medicare patients after acute myocardial infarction: the American College of Cardiology’s Guidelines Applied in Practice (GAP) initiative in Michigan. Am Heart J. 2007;154:461–469. doi: 10.1016/j.ahj.2007.05.003. [DOI] [PubMed] [Google Scholar]
- 27.Lappe JM, Muhlestein JB, Lappe DL, Badger RS, Bair TL, Brockman R, French TK, Hofmann LC, Horne BD, Kralick-Goldberg S, Nicponski N, Orton JA, Pearson RR, Renlund DG, Rimmasch H, Roberts C, Anderson JL. Improvements in 1-year cardiovascular clinical outcomes associated with a hospital-based discharge medication program. Ann Intern Med. 2004;141:446–453. doi: 10.7326/0003-4819-141-6-200409210-00010. [DOI] [PubMed] [Google Scholar]
- 28.Choudhry NK, Avorn J, Glynn RJ, Antman EM, Schneeweiss S, Toscano M, Reisman L, Fernandes J, Spettell C, Lee JL, Levin R, Brennan T, Shrank WH. Post-Myocardial Infarction Free Rx E and Economic Evaluation T. Full coverage for preventive medications after myocardial infarction. N Engl J Med. 2011;365:2088–2097. doi: 10.1056/NEJMsa1107913. [DOI] [PubMed] [Google Scholar]
- 29.Spencer FA, Lessard D, Yarzebski J, Gore JM, Goldberg RJ. Decade-long changes in the use of combination evidence-based medical therapy at discharge for patients surviving acute myocardial infarction. Am Heart J. 2005;150:838–844. doi: 10.1016/j.ahj.2004.11.005. [DOI] [PubMed] [Google Scholar]
- 30.Roe MT, Parsons LS, Pollack CV, Jr, Canto JG, Barron HV, Every NR, Rogers WJ, Peterson ED the National Registry of Myocardial Infarction I. Quality of care by classification of myocardial infarction: treatment patterns for ST-segment elevation vs non-ST-segment elevation myocardial infarction. Arch Intern Med. 2005;165:1630–1636. doi: 10.1001/archinte.165.14.1630. [DOI] [PubMed] [Google Scholar]