Abstract
Trigeminal neuralgia (TN) is a sudden, severe, brief, stabbing, and recurrent pain within one or more branches of the trigeminal nerve. Type 1 as intermittent and Type 2 as constant pain represent distinct clinical, pathological, and prognostic entities. Although multiple mechanism involving peripheral pathologies at root (compression or traction), and dysfunctions of brain stem, basal ganglion, and cortical pain modulatory mechanisms could have role, neurovascular conflict is the most accepted theory. Diagnosis is essentially clinically; magnetic resonance imaging is useful to rule out secondary causes, detect pathological changes in affected root and neurovascular compression (NVC). Carbamazepine is the drug of choice; oxcarbazepine, baclofen, lamotrigine, phenytoin, and topiramate are also useful. Multidrug regimens and multidisciplinary approaches are useful in selected patients. Microvascular decompression is surgical treatment of choice in TN resistant to medical management. Patients with significant medical comorbidities, without NVC and multiple sclerosis are generally recommended to undergo gamma knife radiosurgery, percutaneous balloon compression, glycerol rhizotomy, and radiofrequency thermocoagulation procedures. Partial sensory root sectioning is indicated in negative vessel explorations during surgery and large intraneural vein. Endoscopic technique can be used alone for vascular decompression or as an adjuvant to microscope. It allows better visualization of vascular conflict and entire root from pons to ganglion including ventral aspect. The effectiveness and completeness of decompression can be assessed and new vascular conflicts that may be missed by microscope can be identified. It requires less brain retraction.
Keywords: Cranial nerve, microvascular decompression, neurosurgical procedures/methods, route entry zone, trigeminal nerve diseases, trigeminal neuralgia, trigeminal neuralgia/surgery
Introduction
Trigeminal neuralgia (TN) is defined as sudden, severe, brief, stabbing, and recurrent pain within the distribution of one or more branches of the trigeminal nerve (TR N). Several destructive and nondestructive techniques are available for properly selected cases.[1] Microvascular decompression (MVD) may be considered over other techniques to provide the longest duration of pain freedom.[2] Younger patients benefit from MVD whereas the elderly patients with poor risk are more suitable for percutaneous procedures[3] and gamma knife radiosurgery (GKRS).[4]
This review is based on 17 years search on PubMed and Google including 27 years personal experience of over 600-microvscular decompression surgeries for TN.
Etiology
Although multiple mechanism involving peripheral pathologies at root (compression or traction), and dysfunctions of brain stem, basal ganglion, and cortical pain modulatory mechanisms could have role, neurovascular conflict is the most accepted theory. Artery or vein[5] is usually compressing the TR N near the pons injuring myelin sheath and causing erratic hyperactive functioning of the nerve. Focal arachnoid thickening, angulation, adhesion, traction, tethering or torsion, fibrous ring around the root, cerebello-pontine angle (CPA) tumors, brain stem infarction, aneurism, and arteriovenous malformation (AVM) can also cause TN.[6,7]
Central causes of the disease have also been proposed for TN; reduced basal ganglia μ-opioid receptor,[8] altered gray matter (GM) in sensory, and motor cortex has been implicated.[9] The dysfunction of multiple modulatory mechanisms probably plays a key role in the pathophysiology.[10]
Demyelination, dysmyelination giving increases to electrical hyper excitability, spontaneous and triggered ectopic impulse and cross excitation among neighboring afferents have been proposed in ignition hypothesis.[11] According to the bio resonance hypothesis, TR N fibers are damaged when the vibration frequency of nerve and surrounding structure becomes close to each other.[12] The brain sagging/arterial elongation hypothesis is also believed to cause nerve compression.[5]
Vascular theory
Although it has been generally assumed that vascular contact at the root entry zone (REZ) cause TN, conflict anywhere on the root at central or peripheral myelin, in the region of REZ, or at transition zone between central and peripheral myelin can cause TN.[6] REZ and transition zone between central and peripheral myelin are distinct sites and that these terms should never be used interchangeably.[13] Peripheral myelin is more resistant to compression as compared to central myelin or transition zone.[14] The normal pulsation of artery may not be traumatic[15] enough to produce TN, strokes due to unbending of artery loop usually causes pathological changes in root.[16] Although displacement or grooving of the nerves has been observed in normal individuals,[17] more severe root indentation or distortion in proximal root is likely to produce TN.[18] Arterial compression is commonly seen, venous conflict alone or in combination to arterial compression has been observed in some patients as a cause of TN.[19]
Persistent primitive trigeminal artery,[20] its aneurysm,[21] and vertebrobasilar dolichoectasia[22] may cause TN. Sharper trigeminal-pontine angle,[23] smaller CPA cisterns and short cisternal TR Ns[24,25] can facilitate the neurovascular compression (NVC). Narrow foramen may be etiologically important in a small percentage of TN patients, especially in recurrent or residual cases in the absence of vascular compression during surgery.[26]
Pathophysiology
Exact pathophysiology of TN remains controversial. Chronic nerve compression results in demyelination, with progressive axonal degeneration in small unmyelinated and thinly myelinated fibers. Demyelination can leads to ephaptic transmission; reentry mechanism causes an amplification of sensory inputs. Ultra-structural and biochemical changes in axon and myelin are not only seen in root but also in Gasserian ganglion or in both the structures.[27] Atrophy of the TR N is also seen.[28,29] The GM volume reduction in the primary and secondary somatosensory cortex, orbitofrontal areas, thalamus, insula, anterior cingulate cortex, cerebellum, and dorsolateral prefrontal cortex has been observed.[30,31] Lower axial kurtosis and higher axial diffusivity in corticospinal tract, superior longitudinal fasciculus, anterior thalamic radiation, inferior longitudinal fasciculus, inferior fronto-occipital fasciculus, cingulated gyrus, forceps major, and uncinate fasciculus was observed. There was complex functional connectivity density reorganization of hippocampus, striatum, thalamus, precentral gyrus, precuneus, prefrontal cortex, and inferior parietal lobule.[32] It is difficult to say whether the changes in cortical and subcortical area are cause or effect in TN.
Clinical Features
TN is characterized by episodes of spontaneous pain or a triggered intense facial pain that last for short duration. Pain may be like stabbing, electric shocks, burning, pressing, crushing, exploding, shooting, boring, shock-like sensations, migraine like, piercing, prickling, or a combination. TN is usually of two varieties with Type 1 as intermittent pain and Type 2 is constant. Although a subset of patients can progress from Type 1 to Type 2 TN over time, their pathological and prognostic profiles nevertheless resembled those of Type 1. Proponents of progressive change in character of pain theory think that the TN, atypical neuralgia, and trigeminal neuropathic pain may represent a continuous spectrum rather than discrete pathology,[33] whereas others believe that Type 1 and Type 2 TN represent distinct entities.[34]
Usually, pain resolves completely between the attacks. It usually does not occur when the person is asleep. It is estimated that 1 in 15,000 or 20,000 people suffer from TN, actual figure may be higher due to frequent misdiagnosis.[35] Higher incidence of TN as compared to other cranial nerves neuralgias could be due to longer lengths and more volumes of the central myelin.[36] Disease usually involve single division, it may slowly spread to other division. TN may be associated with ipsilateral hemifacial spasm (painful tic convulsive).[37] Multiple cranial nerve neuralgias, although rare, can occur.[38] It is usually unilateral, bilateral presentation is rare.[39] Rapid spreading to other division, bilateral involvement, or simultaneous involvement of other nerve suggests a secondary disease such as multiple sclerosis (MS) or expanding cranial tumor.
It is common after 50 years of age. TN is uncommon in young adults. Presentation in children is rare.[40] It is more common in females than males. Co-morbid depression is observed. It can be associated with Dandy walker syndrome, small posterior fossa, brain stem infarct, hydrocephalus, MS, lesions in relations to TR N, and opposite side tumor, etc.
Diagnosis
The diagnosis of TN is essentially clinical. Although such patients do not have any neurodeficit with normal blink reflex,[41] quantitative sensory testing have shown subtle sensory abnormalities which may not be detected in routine clinical examination.[42] Magnetic resonance imaging (MRI) imaging is aimed to detect changes in trigeminal root, any NVC and to rule out secondary pathology. MRI can diagnose entire course of nerve,[43] root atrophy, and CPA cistern.[28] Single finding (changes in nerve or the presence of vascular conflict) in MRI scan may not be helpful in deciding symptomatic side, combination of vascular conflict, and anatomical changes in nerve, are highly likely to be associated with symptomatic TN.[44]
Detection of changes in trigeminal root
Diffusion tensor imaging (DTI) can detect increase in apparent diffusion coefficient and decrease in fraction of anisotropy (FA) in TR N.[45,46] Atrophic changes are also associated in TN. Coregistration of three-dimensional fast imaging employing steady-state (3D FIESTA) imaging and DTI facilitates excellent delineation of cisternal segments of TR Ns.[47] The deformity of the cranial nerves can be demonstrated using multislice motion-sensitized driven equilibrium technique.[48]
Vascular conflict detection
3D FIESTA,[49,50] and contrast-enhanced 3D time-of-flight (TOF) magnetic resonance angiography (MRA) in combination with unenhanced MRA could help in the identification of vessel.[51] 3D T2 high-resolution MRI in combination with 3D TOF-MRA and 3D T1-gadolinium enhanced imaging is reliable in detecting the degree of the root compression.[52,53] Although 3D - magnetic resonance cisternography can determine NVC in most of patients, it does have limitations in identification of venous compression.[54] Such veins can be detected by the 3D multifusion volumetric imaging using multidetector row computed tomography.[55]
3D high resolution MRI and image fusion technology could be useful for diagnosis of NVC in majority of patients.[56,57] Image fusion of 3D constructive interference in steady-state and high-resolution MRA is able to depict the complex anatomical relationships between neural and vascular structures.[58,59] Fusion MRI with multiplanar reconstruction can provide information about severity of the neurovascular contact.[60] Although both 1.5 and 3.0-T MRI can provide preoperative assessment of the compressing vessels,[61] 3-T may be of value when 1.5-T is equivocal.[62]
Medical Treatment
Carbamazepine (CBZ) is drug of choice in TN; baclofen, lamotrigine, clonazepam, oxcarbazepine, topiramate, phenytoin, gabapentin, pregabalin, and sodium valproate can be used.[63,64,65] Multi drugs are useful when patients are unable to tolerate higher doses of CBZ.[66] With an availability of increasing number of anticonvulsant drugs, it is likely that surgical option may not be offered for many years.[67]
Intravenous infusion of a combination of magnesium and lidocaine can be very effective in some patients.[68] Five percent lidocaine plaster[69] and 8% capsaicin patch[70] can be useful in some TN. The 5-HT R3 antagonists, neurokinin-1 antagonists, or mast cell stabilizers may have role in the treatment of TN. A multidisciplinary approach using antidepressants and anti-anxiety drugs such as amitriptyline[71] and duloxetine is needed for the management of emotional status.[72]
Botulinum toxin Type A injections may be offered before surgery or unwilling to undergo surgery, and in failed drug treatment.[73] Tetracaine nerve block as an additional treatment after CBZ, acupuncture and peripheral nerve stimulation can be used.[74,75,76] Deep brain stimulation of the posterior hypothalamus may be considered as an adjunctive procedure for refractory TN of first division,[77] especially in MS.[78] Motor cortex stimulation can be used in certain neuropathic or deafferentation pain.[79] Treatment of associated tumor, AVM, epidermoid, aneurism, and hydrocephalus in Chiari malformation can resolve TN.[80]
Gamma Knife Radiosurgery
Radiation may block the conduction of excessive sensory information responsible for triggering pain attacks.[81] Radiosurgery results in about 50% drop in FA values at the target with no significant change in outside the target nerve. Radiosurgery primarily affects myelin sheath.[82]
TN after a failed MVD, significant medical comorbidities, and MS are generally recommended to undergo GKRS.[4] It is indicated in typical or atypical TN,[83] with or without vascular compression,[84] and in recurrence after GKRS, glycerol rhizotomy (GR), radiofrequency thermocoagulation (RFTC), and percutaneous balloon compression (PBC).[85,86,87] Repeat GKRS provides a similar rate of pain relief as the first procedure. The best responses are observed when there is good pain control after first procedure, with new sensory dysfunction and in single division nerve distribution typical TN.[85,86,87,88]
GKRS can be given using one or two isocenters[89] and targeting radiosurgery posteriorly at dorsal REZ,[90] or anteriorly in retrogasserian zone.[91] 80 Gy,[90] 85 Gy,[92] and 90 Gy can be used. Lower dose to the root are associated with less side effect, whereas higher doses provide better pain control with less risk of recurrences but more side effect such as facial numbness. The benefits and risks of higher dose must be carefully discussed with patients, since bothersome facial numbness, may be an acceptable for patients with severe pain.[93]
Radiosurgery can be given using single fraction; multiple fractions can deliver comparatively higher doses. Although hypofractionated stereotactic radiotherapy is not associated with any facial numbness, single fraction radiosurgery provides better pain relief and a lower recurrence rate as compared to hypofractionated technique.[94] Radiosurgery can be given with or without frame based method,[95] with MRI or computerized tomography (CT) planning when there is contraindication to MRI.[96]
Initial pain relief is 77%–96%, which takes about 1–3 weeks (sometimes 10 weeks or longer). Results are better in typical neuralgia with single nerve distribution pain.[88] About 37%[97] and 95%[98] of patients become pain free within 48 h, and 10 days of procedure, respectively. Although the long-term results of GKRS are not as satisfactory as MVD,[99,100] it is an effective alternative with more than 50% long-lasting pain relief.[101,102] Pain control rate is inferior in vertebrobasilar ectasia highlighting need for multimodality management.[103] Although GR provides urgent pain relief than GKRS, Gamma knife provides better long-term pain relief with less morbidity.[104,105]
Recurrence can be seen in about 15% and 50% at 32 months[98] and long-term follow up, respectively.[101,102] Trigeminal sensory deficit is observed in 30%–35%[98,106] which is more in diabetes mellitus, after RFTC,[107] pain relief coming after 30 days of GKRS,[97] failed MVD or GR[108] and repeat GKRS.[87] The cyber knife provides the high precision of dose with the sparing of healthy tissues.[109,110,111] Effectiveness and safety of frameless stereotactic radiosurgery (SRS) using cyber knife system are comparable to frame bases SRS.[112] X-knife radiosurgery also provides effective pain relief with a low complication rate.[113]
Percutaneous Balloon Compression
PBC selectively avoids injury to the small unmyelinated fibers that mediate the corneal reflex. Balloon compression is indicated in patients difficult to communicate, MS, failed MVD, with significant medical comorbidity, multiple divisions including first division,[114] without vascular compression,[115] and in repeat PBC.[116] PBC is reserved for patients in whom the effect of GR has been of short duration or difficult to repeat due to cisternal fibrosis.[117]
3D CT reconstructions can identify an ideal pear shape configuration to improve outcome.[118] Procedure can be performed under local or general anesthesia.[119] There is controversy regarding duration of compression, in one study there were no differences in outcomes between 60 s and longer times,[117] whereas in other study, longer compression time of 70–90 s resulted in better outcome.[119,120] Pear shape balloon is an indication of proper compression and higher pain-free survival,[120,121] whereas persistent elliptical shape is a bad sign and an indication for aborting the procedure. There is 2% risk of technical failures.[122]
PBC is a safe, simple, and effective method of about 90% temporary pain relief.[119,123] Repeat PBC, though associated with some increase in complications, is reasonably safe.[116] Single trigeminal division, primary procedure in the absence of previous operations, and the pear shape balloon are associated to higher pain-free survival.[119,120,121] Results in MS patients are comparable to classic TN. About 14%, 18.9%, 29.5% recurrence is observed within 2, 3, and 5 years follow up, respectively after PBC.[119] Symptomatic dysesthesias,[122] masseter muscle weakness,[124] cardiovascular stress, cheek hemorrhages, corneal ulceration, infections, and transient diplopia are also observed.[125]
Glycerol Rhizotomy
GR is indicated in patients unresponsive to pharmacotherapy,[126] significant medical comorbidities,[4] MS, unilateral and bilateral pain,[127] and after failed MVD.[4] It is cost-effective than MVD, RFTC and GKRS.[128] GR is a safe and efficacious method as a repeat procedure.[129]
The immediate success rate is about 95%[127] with 50%–60% recurrence at 24 months follow up. GR is a simple procedure, and most of the complications are reversible.[126] There is significant positive correlation between the presence of cerebrospinal fluid (CSF) outflow and good success rate.[127] Significant number may experience either mild numbness or dysesthesias. New facial numbness after GR is associated with excellent pain control. Anesthesia dolorosa although rare may be observed.
Radiofrequency Thermocoagulation
RFTC can be used in bilateral pathology,[130] elderly,[130] recurrence after failed MVD,[82] vertebrobasilar dolichoectasia,[131] and MS. Peripheral nerve block,[132] and general anesthesia could relieve perioperative pain without an increase in complications.[133] Although pulsed radiofrequency (PRF) treatment is associated with less complication than conventional RFTC, it is not as effective as the conventional procedure.[134] Higher intraoperative PRF voltage and electrical field intensity may provide better pain relief.[135] Combined PRF and continuous radiofrequency (CRF) can achieve comparable pain relief with lesser side effects as compared to CRF.[136,137] Initial pain control rate is about 95% with about 25% recurrent pain, occasional jaw weakness, corneal anesthesia, and troublesome dysesthesia.
Peripheral Nerve Section
Peripheral neurectomy is a safe and effective procedure for elderly patients, in rural and remote centers where neurosurgical facilities are not available.[138] Pterygopalatine fossa segment neurectomy of maxillary nerve can be used in elderly who may not tolerate craniotomy, or when RFTC and GR treatment is not possible.[139] Pain relief can be lasting from 15 to 24 months.[138] Loss of sensation and recurrences are associated with peripheral neurectomy.
Partial Sensory Root Section
Partial sensory root sectioning (PSRS) is indicated in MS associated with negative vessel explorations during MVD[140] and in large intra neural vein that is difficult to mobilize.[141] PSRS is also recommended in re exploration after failed MVD when there is no NVC.[142,143] Excellent to good outcome is observed in 70% cases[144] with minimal sensory loss.
Microvascular Decompression
MVD is indicated in Type 1[34,84] or Type 2 TN,[145] with NVC.[146] The cure rate is higher in arterial compression compared to venous or no NVC.[147] MVD is also indicated in MS,[148] isolated V2 TN,[149] ectatic vessel with neuralgia,[150] and after SRS.[151] MVD is recommended in younger patients with longer life expectancy and healthy elderly [Figure 1].[152] Although less invasive procedure may be preferable in elderly patients, as complications do tend to increase gradually with an advanced age, MVD in physiologically healthy elderly population remains a reasonable surgical option.[153,154]
Figure 1.
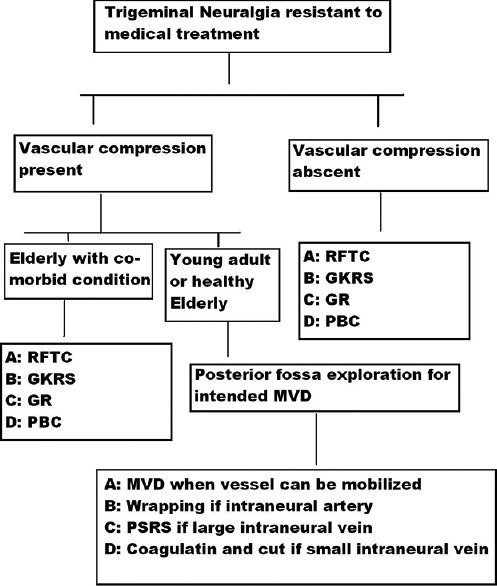
Flow chart showing treatment plan of trigeminal neuralgia resistant to medical management. GKRS = Gamma knife radiosurgery, GR = Glycerol rhizotomy, MVD = Microvascular decompression, PBC = Percutaneous balloon compression, PSRS = Partial sensory root sectioning, RFTC = Radiofrequency thermocoagulation
Dissection in MVD is not significantly difficult after GKRS.[151] Presurgical virtual endoscopy[155] and 3D computer graphics models can provide excellent visualization of NVC and allows simulation.[156] The dextroscope system can also create a stereoscopic neurovascular model to shorten the learning curve.[157]
Indocyanine green angiography could be a helpful adjunct in decompressing the TR N and can guide the surgeon to the nerve-vessel conflict.[158] All vessels, including the transverse pontine vein near meckel's cave, in relation to the nerve should be decompressed.[158,159,160,161] There may be multiple vessels related to the root.[162] Sacrifice of a small intraneural vein can be performed while PSRS is preferred over extensive mobilization of large vein.[141,163] Wrapping techniques can better decompress intraneural artery.[163]
Prominent suprameatal tubercle should be drilled out for better exposure of entire TR N and vascular conflicts.[164] Laterally placed craniotomy helps to visualize the whole nerve root along with REZ. Dissection of the cerebellar horizontal fissure and rostral retraction of the superior semilunar lobule allows easy identification of the REZ with minimal traction. Supracerebellar route permit identification and dissection of the offending supracerebellar artery. Whole surface of the TR N can be observed easily by combining these two approaches.[165] Preservation of the vestibular nerve arachnoid minimizes complications and optimizes surgical outcome.[166]
Autologous muscle graft,[167] oxidized regenerated cellulose,[168] and fibrin glue alone[169] can be used to transpose vessel away from the nerve. Transposition of the offending vessel with Teflon wool or slings, especially in tortuous NVC, is a useful.[170,171,172,173,174] Aneurysm clip with or without unabsorbable dural sling can be used.[175,176]
Adhesion between the trigeminal root and surrounding structures, secondary to fibrin glue or prosthesis, can stretch nerve,[172] which can cause recurrence.[177] Prosthesis if used should be lying in subarachnoid space or cistern avoiding contact to dura matter or tentorium.[178] Arachnoid membrane of CPA can be used as a sling to transpose the superior cerebellar artery.[179]
Combing[180,181] or PSRS[4] can be combined with MVD when no vascular conflict is detected.[182] Muscle pieces interposition between the duramater, artificial dura mater, cranioplasty, sealing of mastoid sinus by bone wax and muscle can be effective technique for the prevention of CSF leak.[183,184,185] Re surgery is an effective and safe after failed MVD.[142] The preservation of the petrosal vein and its tributaries, lateral inversion vein of ventricle IV is important in preventing the postoperative vestibular and cerebellar disorders.[186]
Early outcome after MVD in typical TN with associated NVC is 90%–95% which drops to 75% at 1and 5 years follow up.[67,187,188,189,190] MVD is significantly superior to GKRS.[191] TR N combing has a much higher pain relief in patients without vascular compression than those with vascular compression.[180] 3D models by fusing CTA and FIESTA can be used to evaluate the translational and rotational shift of the compressive artery, and decompressed distance from the root after failed MVD.[192]
Immediate postoperative pain relief is a good predictor of better long-term outcome.[193] Type 2 TN,[194] presence of autonomic symptoms,[195] MS[196] are associated with poor prognosis. Shorter preoperative duration, older age, and typical features are good predictors of favorable outcome.[197] Subset of patients progressed from Type 1 to Type 2 TN over time also have good outcome resembling Type 1.[34] Low FA values can be reversed after successful MVD.[198] Significant reduction of FA value may predict an optimistic outcome of MVD.[199]
The trigemino-cardiac reflex due to stimulation of the TR N during MVD may result in about 50% fall in heart rate and mean arterial blood pressure, cessation of manipulation lead to normalization of parameters.[34] Facial nerve dysfunction, hearing abnormality,[200] and TR N dysfunction may be observed, especially after more dissection and mobilization of respective nerve. Brainstem auditory evoked potential monitoring and neuro-endoscopy during MVD can preserve hearing function.[201]
Recurrences, ranging from 18% to 34%, may be seen at long-term follow up.[202,203] It is more common within 2 years of surgery and thereafter at a rate of 2%–3.5% per year.[202] Significant predictors of recurrence are younger age, and symptoms lasting longer than 10 years.[203] Recompression due to regrowth of new vein or artery[204] can cause TN. Hardened Teflon can pierce nerve and produce TN,[205] therefore the contact of prosthesis, if used, with the nerve should be avoided. Outcome can be improved by establishing center dealing TN.[206] Late communicating hydrocephalus may be a potential complication of MVD surgery.[207]
Endoscopic Vascular Decompression
Endoscopic techniques are increasingly being used in spine,[208,209,210] skull base[211,212,213] and intracranial pathologies.[214,215,216] Endoscopic technique can be used alone in TN[217,218] or as an adjuvant to microscope[219,220,221] It is a minimally invasive technique,[221,222] allows better visualization of entire root from pons to ganglion[217,222,223] including ventral aspect.[223] The endoscope is a valuable tool during MVD, especially when a bony ridge hiding the direct microscopic view of vascular conflict.[224] Effectiveness and completeness of decompression can be better assessed.[217,223] New nerve-vessel conflicts can be identified which may be missed by microscope in 7.5%–33% of patients.[225,226,227,228] It is safe,[218,229,230,231,232] requires less brain retraction[217,225,233,234,235] and associated with improved pain relief with lower complications as compared to MVD.[236] The vascular conflict is mostly distributed in the medial side on second division while it is in lateral area for third division in TN.[237]
Our recommendations
Medical treatment with drugs should be tried in TN. With an availability of increasing number of drugs it is likely that surgical option may not be offered for many years. Microscopic or endoscopic vascular decompression is recommended because of nondestructive nature, especially when NVC is present in young adults or healthy elderly [Figure 1]. GKRS, RFTC, GR, and PBC can be used in elderly patients with medical comorbidity and without NVC.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Zakrzewska JM, McMillan R. Trigeminal neuralgia: The diagnosis and management of this excruciating and poorly understood facial pain. Postgrad Med J. 2011;87:410–6. doi: 10.1136/pgmj.2009.080473. [DOI] [PubMed] [Google Scholar]
- 2.Cruccu G, Gronseth G, Alksne J, Argoff C, Brainin M, Burchiel K, et al. AAN-EFNS guidelines on trigeminal neuralgia management. Eur J Neurol. 2008;15:1013–28. doi: 10.1111/j.1468-1331.2008.02185.x. [DOI] [PubMed] [Google Scholar]
- 3.Emril DR, Ho KY. Treatment of trigeminal neuralgia: Role of radiofrequency ablation. J Pain Res. 2010;3:249–54. doi: 10.2147/JPR.S14455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Pollock BE. Surgical management of medically refractory trigeminal neuralgia. Curr Neurol Neurosci Rep. 2012;12:125–31. doi: 10.1007/s11910-011-0242-7. [DOI] [PubMed] [Google Scholar]
- 5.Thomas KL, Vilensky JA. The anatomy of vascular compression in trigeminal neuralgia. Clin Anat. 2014;27:89–93. doi: 10.1002/ca.22157. [DOI] [PubMed] [Google Scholar]
- 6.Sindou M, Howeidy T, Acevedo G. Anatomical observations during microvascular decompression for idiopathic trigeminal neuralgia (with correlations between topography of pain and site of the neurovascular conflict). Prospective study in a series of 579 patients. Acta Neurochir (Wien) 2002;144:1–12. doi: 10.1007/s701-002-8269-4. [DOI] [PubMed] [Google Scholar]
- 7.Ishikawa M, Nishi S, Aoki T, Takase T, Wada E, Ohwaki H, et al. Operative findings in cases of trigeminal neuralgia without vascular compression: Proposal of a different mechanism. J Clin Neurosci. 2002;9:200–4. doi: 10.1054/jocn.2001.0922. [DOI] [PubMed] [Google Scholar]
- 8.DosSantos MF, Martikainen IK, Nascimento TD, Love TM, Deboer MD, Maslowski EC, et al. Reduced basal ganglia μ-opioid receptor availability in trigeminal neuropathic pain: A pilot study. Mol Pain. 2012;8:74. doi: 10.1186/1744-8069-8-74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Desouza DD, Moayedi M, Chen DQ, Davis KD, Hodaie M. Sensorimotor and pain modulation brain abnormalities in trigeminal neuralgia: A paroxysmal, sensory-triggered neuropathic pain. PLoS One. 2013;8:e66340. doi: 10.1371/journal.pone.0066340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Dallel R, Villanueva L, Woda A, Voisin D. Neurobiology of trigeminal pain. Med Sci (Paris) 2003;19:567–74. doi: 10.1051/medsci/2003195567. [DOI] [PubMed] [Google Scholar]
- 11.Devor M, Govrin-Lippmann R, Rappaport ZH. Mechanism of trigeminal neuralgia: An ultrastructural analysis of trigeminal root specimens obtained during microvascular decompression surgery. J Neurosurg. 2002;96:532–43. doi: 10.3171/jns.2002.96.3.0532. [DOI] [PubMed] [Google Scholar]
- 12.Jia DZ, Li G. Bioresonance hypothesis: A new mechanism on the pathogenesis of trigeminal neuralgia. Med Hypotheses. 2010;74:505–7. doi: 10.1016/j.mehy.2009.09.056. [DOI] [PubMed] [Google Scholar]
- 13.Peker S, Kurtkaya Ö, Üzün I, Pamir MN. Microanatomy of the central myelin-peripheral myelin transition zone of the trigeminal nerve. Neurosurgery. 2006;59:354–9. doi: 10.1227/01.NEU.0000223501.27220.69. [DOI] [PubMed] [Google Scholar]
- 14.De Ridder D, Møller A, Verlooy J, Cornelissen M, De Ridder L. Is the root entry/exit zone important in microvascular compression syndromes? Neurosurgery. 2002;51:427–33. doi: 10.1097/00006123-200208000-00023. [DOI] [PubMed] [Google Scholar]
- 15.Adamczyk M, Bulski T, Sowinska J, Furmanek A, Bekiesinska-Figatowska M. Trigeminal nerve – Artery contact in people without trigeminal neuralgia – MR study. Med Sci Monit. 2007;13(Suppl 1):38–43. [PubMed] [Google Scholar]
- 16.Baliazina EV. Topographic anatomical relationship between the trigeminal nerve trunk and superior cerebellar artery in patients with trigeminal neuralgia. Morfologiia. 2009;136:27–31. [PubMed] [Google Scholar]
- 17.Ramesh VG, Premkumar G. An anatomical study of the neurovascular relationships at the trigeminal root entry zone. J Clin Neurosci. 2009;16:934–6. doi: 10.1016/j.jocn.2008.09.011. [DOI] [PubMed] [Google Scholar]
- 18.Miller JP, Acar F, Hamilton BE, Burchiel KJ. Radiographic evaluation of trigeminal neurovascular compression in patients with and without trigeminal neuralgia. J Neurosurg. 2009;110:627–32. doi: 10.3171/2008.6.17620. [DOI] [PubMed] [Google Scholar]
- 19.Dumot C, Brinzeu A, Berthiller J, Sindou M. Trigeminal neuralgia due to venous neurovascular conflicts: Outcome after microvascular decompression in a series of 55 consecutive patients. Acta Neurochir (Wien) 2017;159:237–49. doi: 10.1007/s00701-016-2994-y. [DOI] [PubMed] [Google Scholar]
- 20.Conforti R, Parlato RS, De Paulis D, Cirillo M, Marrone V, Cirillo S, et al. Trigeminal neuralgia and persistent trigeminal artery. Neurol Sci. 2012;33:1455–8. doi: 10.1007/s10072-012-0942-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ladner TR, Ehtesham M, Davis BJ, Khan IS, Ghiassi M, Ghiassi M, et al. Resolution of trigeminal neuralgia by coil embolization of a persistent primitive trigeminal artery aneurysm. J Neurointerv Surg. 2014;6:e22. doi: 10.1136/neurintsurg-2013-010703.rep. [DOI] [PubMed] [Google Scholar]
- 22.Ma X, Sun X, Yao J, Ni S, Gong J, Wang J, et al. Clinical analysis of trigeminal neuralgia caused by vertebrobasilar dolichoectasia. Neurosurg Rev. 2013;36:573–7. doi: 10.1007/s10143-013-0468-8. [DOI] [PubMed] [Google Scholar]
- 23.Ha SM, Kim SH, Yoo EH, Han IB, Shin DA, Cho KG, et al. Patients with idiopathic trigeminal neuralgia have a sharper-than-normal trigeminal-pontine angle and trigeminal nerve atrophy. Acta Neurochir (Wien) 2012;154:1627–33. doi: 10.1007/s00701-012-1327-z. [DOI] [PubMed] [Google Scholar]
- 24.Parise M, Acioly MA, Ribeiro CT, Vincent M, Gasparetto EL. The role of the cerebellopontine angle cistern area and trigeminal nerve length in the pathogenesis of trigeminal neuralgia: A prospective case-control study. Acta Neurochir (Wien) 2013;155:863–8. doi: 10.1007/s00701-012-1573-0. [DOI] [PubMed] [Google Scholar]
- 25.Rasche D, Kress B, Stippich C, Nennig E, Sartor K, Tronnier VM. Volumetric measurement of the pontomesencephalic cistern in patients with trigeminal neuralgia and healthy controls. Neurosurgery. 2006;59:614–20. doi: 10.1227/01.NEU.0000228924.20750.D4. [DOI] [PubMed] [Google Scholar]
- 26.Liu P, Zhong W, Liao C, Liu M, Zhang W. Narrow foramen ovale and rotundum: A role in the etiology of trigeminal neuralgia. J Craniofac Surg. 2016;27:2168–70. doi: 10.1097/SCS.0000000000003021. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 27.Marinkovic S, Gibo H, Todorovic V, Antic B, Kovacevic D, Milisavljevic M, et al. Ultrastructure and immunohistochemistry of the trigeminal peripheral myelinated axons in patients with neuralgia. Clin Neurol Neurosurg. 2009;111:795–800. doi: 10.1016/j.clineuro.2009.07.020. [DOI] [PubMed] [Google Scholar]
- 28.Park SH, Hwang SK, Lee SH, Park J, Hwang JH, Hamm IS. Nerve atrophy and a small cerebellopontine angle cistern in patients with trigeminal neuralgia. J Neurosurg. 2009;110:633–7. doi: 10.3171/2008.8.JNS08522. [DOI] [PubMed] [Google Scholar]
- 29.Wang Y, Li D, Bao F, Guo C, Ma S, Zhang M. Microstructural abnormalities of the trigeminal nerve correlate with pain severity and concomitant emotional dysfunctions in idiopathic trigeminal neuralgia: A randomized, prospective, double-blind study. Magn Reson Imaging. 2016;34:609–16. doi: 10.1016/j.mri.2015.11.013. [DOI] [PubMed] [Google Scholar]
- 30.Obermann M, Rodriguez-Raecke R, Naegel S, Holle D, Mueller D, Yoon MS, et al. Gray matter volume reduction reflects chronic pain in trigeminal neuralgia. Neuroimage. 2013;74:352–8. doi: 10.1016/j.neuroimage.2013.02.029. [DOI] [PubMed] [Google Scholar]
- 31.DeSouza DD, Hodaie M, Davis KD. Structural magnetic resonance imaging can identify trigeminal system abnormalities in classical trigeminal neuralgia. Front Neuroanat. 2016;10:95. doi: 10.3389/fnana.2016.00095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Tian T, Guo L, Xu J, Zhang S, Shi J, Liu C, et al. Brain white matter plasticity and functional reorganization underlying the central pathogenesis of trigeminal neuralgia. Sci Rep. 2016;6:36030. doi: 10.1038/srep36030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Burchiel KJ, Slavin KV. On the natural history of trigeminal neuralgia. Neurosurgery. 2000;46:152–4. [PubMed] [Google Scholar]
- 34.Miller JP, Acar F, Burchiel KJ. Classification of trigeminal neuralgia: Clinical, therapeutic, and prognostic implications in a series of 144 patients undergoing microvascular decompression. J Neurosurg. 2009;111:1231–4. doi: 10.3171/2008.6.17604. [DOI] [PubMed] [Google Scholar]
- 35.Tallawy HN, Farghaly WM, Rageh TA, Shehata GA, Badry R, Metwally NA, et al. Door-to-door survey of major neurological disorders (project) in Al Quseir City, Red Sea Governorate, Egypt. Neuropsychiatr Dis Treat. 2013;9:767–71. doi: 10.2147/NDT.S36956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Guclu B, Sindou M, Meyronet D, Streichenberger N, Simon E, Mertens P. Cranial nerve vascular compression syndromes of the trigeminal, facial and vago-glossopharyngeal nerves: Comparative anatomical study of the central myelin portion and transitional zone; correlations with incidences of corresponding hyperactive dysfunctional syndromes. Acta Neurochir (Wien) 2011;153:2365–75. doi: 10.1007/s00701-011-1168-1. [DOI] [PubMed] [Google Scholar]
- 37.Mittal P, Mittal G. Painful tic convulsif syndrome due to vertebrobasilar dolichoectasia. J Neurosci Rural Pract. 2011;2:71–3. doi: 10.4103/0976-3147.80111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Jia Y, Wenhua W, Quanbin Z. A single microvascular decompression surgery cures a patient with trigeminal neuralgia, hemifacial spasm, tinnitus, hypertension, and paroxysmal supraventricular tachycardia caused by the compression of a vertebral artery. Neurol India. 2013;61:73–5. doi: 10.4103/0028-3886.108016. [DOI] [PubMed] [Google Scholar]
- 39.Oliveira CM, Baaklini LG, Issy AM, Sakata RK. Bilateral trigeminal neuralgia: Case report. Rev Bras Anestesiol. 2009;59:476–80. doi: 10.1590/s0034-70942009000400010. [DOI] [PubMed] [Google Scholar]
- 40.Bender MT, Pradilla G, James C, Raza S, Lim M, Carson BS. Surgical treatment of pediatric trigeminal neuralgia: Case series and review of the literature. Childs Nerv Syst. 2011;27:2123–9. doi: 10.1007/s00381-011-1593-8. [DOI] [PubMed] [Google Scholar]
- 41.Mikula I, Trkanjec Z, Negovetic R, Miskov S, Demarin V. Differences of blink-reflex abnormalities in patients suffering from idiopathic and symptomatic trigeminal neuralgia. Wien Klin Wochenschr. 2005;117:417–22. doi: 10.1007/s00508-005-0364-5. [DOI] [PubMed] [Google Scholar]
- 42.Flor H, Rasche D, Islamian AP, Rolko C, Yilmaz P, Ruppolt M, et al. Subtle sensory abnormalities detected by quantitative sensory testing in patients with trigeminal neuralgia. Pain Physician. 2016;19:507–18. [PubMed] [Google Scholar]
- 43.Harsha KJ, Kesavadas C, Chinchure S, Thomas B, Jagtap S. Imaging of vascular causes of trigeminal neuralgia. J Neuroradiol. 2012;39:281–9. doi: 10.1016/j.neurad.2012.08.006. [DOI] [PubMed] [Google Scholar]
- 44.Antonini G, Di Pasquale A, Cruccu G, Truini A, Morino S, Saltelli G, et al. Magnetic resonance imaging contribution for diagnosing symptomatic neurovascular contact in classical trigeminal neuralgia: A blinded case-control study and meta-analysis. Pain. 2014;155:1464–71. doi: 10.1016/j.pain.2014.04.020. [DOI] [PubMed] [Google Scholar]
- 45.Liu Y, Li J, Butzkueven H, Duan Y, Zhang M, Shu N, et al. Microstructural abnormalities in the trigeminal nerves of patients with trigeminal neuralgia revealed by multiple diffusion metrics. Eur J Radiol. 2013;82:783–6. doi: 10.1016/j.ejrad.2012.11.027. [DOI] [PubMed] [Google Scholar]
- 46.Chen J, Guo ZY, Liang QZ, Liao HY, Su WR, Chen CX, et al. Structural abnormalities of trigeminal root with neurovascular compression revealed by high resolution diffusion tensor imaging. Asian Pac J Trop Med. 2012;5:749–52. doi: 10.1016/S1995-7645(12)60119-9. [DOI] [PubMed] [Google Scholar]
- 47.Lutz J, Linn J, Mehrkens JH, Thon N, Stahl R, Seelos K, et al. Trigeminal neuralgia due to neurovascular compression: High-spatial-resolution diffusion-tensor imaging reveals microstructural neural changes. Radiology. 2011;258:524–30. doi: 10.1148/radiol.10100477. [DOI] [PubMed] [Google Scholar]
- 48.Kanoto M, Hosoya T, Oda A, Honma T, Sugai Y. Focal deformity of the cranial nerves observed on multislice motion-sensitized driven equilibrium (MSDE) in patients with neurovascular compression. J Comput Assist Tomogr. 2012;36:121–4. doi: 10.1097/RCT.0b013e3182416f3b. [DOI] [PubMed] [Google Scholar]
- 49.Prieto R, Pascual JM, Yus M, Jorquera M. Trigeminal neuralgia: Assessment of neurovascular decompression by 3D fast imaging employing steady-state acquisition and 3D time of flight multiple overlapping thin slab acquisition magnetic resonance imaging. Surg Neurol Int. 2012;3:50. doi: 10.4103/2152-7806.96073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Zeng Q, Zhou Q, Liu Z, Li C, Ni S, Xue F. Preoperative detection of the neurovascular relationship in trigeminal neuralgia using three-dimensional fast imaging employing steady-state acquisition (FIESTA) and magnetic resonance angiography (MRA) J Clin Neurosci. 2013;20:107–11. doi: 10.1016/j.jocn.2012.01.046. [DOI] [PubMed] [Google Scholar]
- 51.Zhou Q, Liu Z, Li C, Qu C, Ni S, Zeng Q. Preoperative evaluation of neurovascular relationship by using contrast-enhanced and unenhanced 3D time-of-flight MR angiography in patients with trigeminal neuralgia. Acta Radiol. 2011;52:894–8. doi: 10.1258/ar.2011.110195. [DOI] [PubMed] [Google Scholar]
- 52.Leal PR, Hermier M, Souza MA, Cristino-Filho G, Froment JC, Sindou M. Visualization of vascular compression of the trigeminal nerve with high-resolution 3T MRI: A prospective study comparing preoperative imaging analysis to surgical findings in 40 consecutive patients who underwent microvascular decompression for trigeminal neuralgia. Neurosurgery. 2011;69:15–25. doi: 10.1227/NEU.0b013e318212bafa. [DOI] [PubMed] [Google Scholar]
- 53.Leal PR, Hermier M, Froment JC, Souza MA, Cristino-Filho G, Sindou M. Preoperative demonstration of the neurovascular compression characteristics with special emphasis on the degree of compression, using high-resolution magnetic resonance imaging: A prospective study, with comparison to surgical findings, in 100 consecutive patients who underwent microvascular decompression for trigeminal neuralgia. Acta Neurochir (Wien) 2010;152:817–25. doi: 10.1007/s00701-009-0588-7. [DOI] [PubMed] [Google Scholar]
- 54.Anqi X, Ding L, Jiahe X, Zhenlin L, Chunchao X, Chao Y. MR cisternography in the posterior fossa: The evaluation of trigeminal neurovascular compression. Turk Neurosurg. 2013;23:218–25. doi: 10.5137/1019-5149.JTN.6768-12.0. [DOI] [PubMed] [Google Scholar]
- 55.Oishi M, Fukuda M, Noto Y, Kawaguchi T, Hiraishi T, Fujii Y. Trigeminal neuralgia associated with the specific bridging pattern of transverse pontine vein: Diagnostic value of three-dimensional multifusion volumetric imaging. Stereotact Funct Neurosurg. 2011;89:226–33. doi: 10.1159/000326778. [DOI] [PubMed] [Google Scholar]
- 56.Guo ZY, Chen J, Yang G, Tang QY, Chen CX, Fu SX, et al. Characteristics of neurovascular compression in facial neuralgia patients by 3D high-resolution MRI and fusion technology. Asian Pac J Trop Med. 2012;5:1000–3. doi: 10.1016/S1995-7645(12)60190-4. [DOI] [PubMed] [Google Scholar]
- 57.Chen J, Guo ZY, Yang G, Wang X, Tang QY, Cheng YQ, et al. Characterization of neurovascular compression in facial neuralgia patients by 3D high-resolution MRI and image fusion technique. Asian Pac J Trop Med. 2012;5:476–9. doi: 10.1016/S1995-7645(12)60082-0. [DOI] [PubMed] [Google Scholar]
- 58.Granata F, Vinci SL, Longo M, Bernava G, Caffo M, Cutugno M, et al. Advanced virtual magnetic resonance imaging (MRI) techniques in neurovascular conflict: Bidimensional image fusion and virtual cisternography. Radiol Med. 2013;118:1045–54. doi: 10.1007/s11547-013-0928-9. [DOI] [PubMed] [Google Scholar]
- 59.Cha J, Kim ST, Kim HJ, Choi JW, Kim HJ, Jeon P, et al. Trigeminal neuralgia: Assessment with T2 VISTA and FLAIR VISTA fusion imaging. Eur Radiol. 2011;21:2633–9. doi: 10.1007/s00330-011-2216-1. [DOI] [PubMed] [Google Scholar]
- 60.Satoh T, Omi M, Nabeshima M, Onoda K, Date I. Severity analysis of neurovascular contact in patients with trigeminal neuralgia: Assessment with the inner view of the 3D MR cisternogram and angiogram fusion imaging. AJNR Am J Neuroradiol. 2009;30:603–7. doi: 10.3174/ajnr.A1409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Shimizu M, Imai H, Kagoshima K, Umezawa E, Shimizu T, Yoshimoto Y. Detection of compression vessels in trigeminal neuralgia by surface-rendering three-dimensional reconstruction of 1.5- and 3.0-T magnetic resonance imaging. World Neurosurg. 2013;80:378–85. doi: 10.1016/j.wneu.2012.05.030. [DOI] [PubMed] [Google Scholar]
- 62.Garcia M, Naraghi R, Zumbrunn T, Rösch J, Hastreiter P, Dörfler A. High-resolution 3D-constructive interference in steady-state MR imaging and 3D time-of-flight MR angiography in neurovascular compression: A comparison between 3T and 1.5T. AJNR Am J Neuroradiol. 2012;33:1251–6. doi: 10.3174/ajnr.A2974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Wang QP, Bai M. Topiramate versus carbamazepine for the treatment of classical trigeminal neuralgia: A meta-analysis. CNS Drugs. 2011;25:847–57. doi: 10.2165/11595590-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 64.Shaikh S, Yaacob HB, Abd Rahman RB. Lamotrigine for trigeminal neuralgia: Efficacy and safety in comparison with carbamazepine. J Chin Med Assoc. 2011;74:243–9. doi: 10.1016/j.jcma.2011.04.002. [DOI] [PubMed] [Google Scholar]
- 65.Tate R, Rubin LM, Krajewski KC. Treatment of refractory trigeminal neuralgia with intravenous phenytoin. Am J Health Syst Pharm. 2011;68:2059–61. doi: 10.2146/ajhp100636. [DOI] [PubMed] [Google Scholar]
- 66.Ariyawardana A, Pallegama R, Sitheeque M, Ranasinghe A. Use of single- and multi-drug regimens in the management of classic (idiopathic) trigeminal neuralgia: An 11-year experience at a single Sri Lankan institution. J Investig Clin Dent. 2012;3:98–102. doi: 10.1111/j.2041-1626.2011.00109.x. [DOI] [PubMed] [Google Scholar]
- 67.Zakrzewska JM, Coakham HB. Microvascular decompression for trigeminal neuralgia: Update. Curr Opin Neurol. 2012;25:296–301. doi: 10.1097/WCO.0b013e328352c465. [DOI] [PubMed] [Google Scholar]
- 68.Arai YC, Hatakeyama N, Nishihara M, Ikeuchi M, Kurisuno M, Ikemoto T. Intravenous lidocaine and magnesium for management of intractable trigeminal neuralgia: A case series of nine patients. J Anesth. 2013;27:960–2. doi: 10.1007/s00540-013-1641-5. [DOI] [PubMed] [Google Scholar]
- 69.Nalamachu S, Wieman M, Bednarek L, Chitra S. Influence of anatomic location of lidocaine patch 5% on effectiveness and tolerability for postherpetic neuralgia. Patient Prefer Adherence. 2013;7:551–7. doi: 10.2147/PPA.S42643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Wagner T, Poole C, Roth-Daniek A. The capsaicin 8% patch for neuropathic pain in clinical practice: A retrospective analysis. Pain Med. 2013;14:1202–11. doi: 10.1111/pme.12143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Macianskyte D, Janužis G, Kubilius R, Adomaitiene V, Šciupokas A. Associations between chronic pain and depressive symptoms in patients with trigeminal neuralgia. Medicina (Kaunas) 2011;47:386–92. [PubMed] [Google Scholar]
- 72.Anand KS, Dhikav V, Prasad A, Shewtengna Efficacy, safety and tolerability of duloxetine in idiopathic trigeminal neuralgia. J Indian Med Assoc. 2011;109:264–6. [PubMed] [Google Scholar]
- 73.Wu CJ, Lian YJ, Zheng YK, Zhang HF, Chen Y, Xie NC, et al. Botulinum toxin type A for the treatment of trigeminal neuralgia: Results from a randomized, double-blind, placebo-controlled trial. Cephalalgia. 2012;32:443–50. doi: 10.1177/0333102412441721. [DOI] [PubMed] [Google Scholar]
- 74.Shiiba S, Tanaka T, Sakamoto E, Oda M, Kito S, Ono K, et al. Can the neurovascular compression volume of the trigeminal nerve on magnetic resonance cisternography predict the success of local anesthetic block after initial treatment by the carbamazepine? Oral Surg Oral Med Oral Pathol Oral Radiol. 2014;117:e15–21. doi: 10.1016/j.oooo.2012.03.029. [DOI] [PubMed] [Google Scholar]
- 75.Liu H, Li H, Xu M, Chung KF, Zhang SP. A systematic review on acupuncture for trigeminal neuralgia. Altern Ther Health Med. 2010;16:30–5. [PubMed] [Google Scholar]
- 76.Stidd DA, Wuollet AL, Bowden K, Price T, Patwardhan A, Barker S, et al. Peripheral nerve stimulation for trigeminal neuropathic pain. Pain Physician. 2012;15:27–33. [PMC free article] [PubMed] [Google Scholar]
- 77.Cordella R, Franzini A, La Mantia L, Marras C, Erbetta A, Broggi G. Hypothalamic stimulation for trigeminal neuralgia in multiple sclerosis patients: Efficacy on the paroxysmal ophthalmic pain. Mult Scler. 2009;15:1322–8. doi: 10.1177/1352458509107018. [DOI] [PubMed] [Google Scholar]
- 78.Franzini A, Messina G, Cordella R, Marras C, Broggi G. Deep brain stimulation of the posteromedial hypothalamus: Indications, long-term results, and neurophysiological considerations. Neurosurg Focus. 2010;29:E13. doi: 10.3171/2010.5.FOCUS1094. [DOI] [PubMed] [Google Scholar]
- 79.Raslan AM, Nasseri M, Bahgat D, Abdu E, Burchiel KJ. Motor cortex stimulation for trigeminal neuropathic or deafferentation pain: An institutional case series experience. Stereotact Funct Neurosurg. 2011;89:83–8. doi: 10.1159/000323338. [DOI] [PubMed] [Google Scholar]
- 80.Gnanalingham K, Joshi SM, Lopez B, Ellamushi H, Hamlyn P. Trigeminal neuralgia secondary to Chiari's malformation – Treatment with ventriculoperitoneal shunt. Surg Neurol. 2005;63:586–8. doi: 10.1016/j.surneu.2004.06.021. [DOI] [PubMed] [Google Scholar]
- 81.Gorgulho A. Radiation mechanisms of pain control in classical trigeminal neuralgia. Surg Neurol Int. 2012;3(Suppl 1):S17–25. doi: 10.4103/2152-7806.91606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Hodaie M, Chen DQ, Quan J, Laperriere N. Tractography delineates microstructural changes in the trigeminal nerve after focal radiosurgery for trigeminal neuralgia. PLoS One. 2012;7:e32745. doi: 10.1371/journal.pone.0032745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Brisman R. Constant face pain in typical trigeminal neuralgia and response to γ knife radiosurgery. Stereotact Funct Neurosurg. 2013;91:122–8. doi: 10.1159/000343206. [DOI] [PubMed] [Google Scholar]
- 84.Sheehan JP, Ray DK, Monteith S, Yen CP, Lesnick J, Kersh R, et al. Gamma knife radiosurgery for trigeminal neuralgia: The impact of magnetic resonance imaging-detected vascular impingement of the affected nerve. J Neurosurg. 2010;113:53–8. doi: 10.3171/2009.9.jns09196. [DOI] [PubMed] [Google Scholar]
- 85.Park KJ, Kondziolka D, Berkowitz O, Kano H, Novotny J, Jr, Niranjan A, et al. Repeat gamma knife radiosurgery for trigeminal neuralgia. Neurosurgery. 2012;70:295–305. doi: 10.1227/NEU.0b013e318230218e. [DOI] [PubMed] [Google Scholar]
- 86.Dhople AA, Adams JR, Maggio WW, Naqvi SA, Regine WF, Kwok Y. Long-term outcomes of gamma knife radiosurgery for classic trigeminal neuralgia: Implications of treatment and critical review of the literature. Clinical article. J Neurosurg. 2009;111:351–8. doi: 10.3171/2009.2.JNS08977. [DOI] [PubMed] [Google Scholar]
- 87.Elaimy AL, Hanson PW, Lamoreaux WT, Mackay AR, Demakas JJ, Fairbanks RK, et al. Clinical outcomes of gamma knife radiosurgery in the treatment of patients with trigeminal neuralgia. Int J Otolaryngol. 2012;2012:919186. doi: 10.1155/2012/919186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Kano H, Kondziolka D, Yang HC, Zorro O, Lobato-Polo J, Flannery TJ, et al. Outcome predictors after gamma knife radiosurgery for recurrent trigeminal neuralgia. Neurosurgery. 2010;67:1637–44. doi: 10.1227/NEU.0b013e3181fa098a. [DOI] [PubMed] [Google Scholar]
- 89.Li P, Wang W, Liu Y, Zhong Q, Mao B. Clinical outcomes of 114 patients who underwent γ-knife radiosurgery for medically refractory idiopathic trigeminal neuralgia. J Clin Neurosci. 2012;19:71–4. doi: 10.1016/j.jocn.2011.03.020. [DOI] [PubMed] [Google Scholar]
- 90.Matsuda S, Serizawa T, Nagano O, Ono J. Comparison of the results of 2 targeting methods in gamma knife surgery for trigeminal neuralgia. J Neurosurg. 2008;109(Suppl):185–9. doi: 10.3171/JNS/2008/109/12/S28. [DOI] [PubMed] [Google Scholar]
- 91.Park SH, Hwang SK, Kang DH, Park J, Hwang JH, Sung JK. The retrogasserian zone versus dorsal root entry zone: Comparison of two targeting techniques of gamma knife radiosurgery for trigeminal neuralgia. Acta Neurochir (Wien) 2010;152:1165–70. doi: 10.1007/s00701-010-0610-0. [DOI] [PubMed] [Google Scholar]
- 92.Kim YH, Kim DG, Kim JW, Kim YH, Han JH, Chung HT, et al. Is it effective to raise the irradiation dose from 80 to 85 Gy in gamma knife radiosurgery for trigeminal neuralgia? Stereotact Funct Neurosurg. 2010;88:169–76. doi: 10.1159/000313869. [DOI] [PubMed] [Google Scholar]
- 93.Young B, Shivazad A, Kryscio RJ, St Clair W, Bush HM. Long-term outcome of high-dose γ knife surgery in treatment of trigeminal neuralgia. J Neurosurg. 2013;119:1166–75. doi: 10.3171/2013.1.JNS12875. [DOI] [PubMed] [Google Scholar]
- 94.Fraioli MF, Strigari L, Fraioli C, Lecce M, Lisciani D. Preliminary results of 45 patients with trigeminal neuralgia treated with radiosurgery compared to hypofractionated stereotactic radiotherapy, using a dedicated linear accelerator. J Clin Neurosci. 2012;19:1401–3. doi: 10.1016/j.jocn.2011.11.036. [DOI] [PubMed] [Google Scholar]
- 95.Latorzeff I, Debono B, Sol JC, Ménégalli D, Mertens P, Redon A, et al. Treatment of trigeminal neuralgia with radiosurgery. Cancer Radiother. 2012;16(Suppl):S57–69. doi: 10.1016/j.canrad.2012.01.007. [DOI] [PubMed] [Google Scholar]
- 96.Attia A, Tatter SB, Weller M, Marshall K, Lovato JF, Bourland JD, et al. CT-only planning for gamma knife radiosurgery in the treatment of trigeminal neuralgia: Methodology and outcomes from a single institution. J Med Imaging Radiat Oncol. 2012;56:490–4. doi: 10.1111/j.1754-9485.2012.02403.x. [DOI] [PubMed] [Google Scholar]
- 97.Tuleasca C, Carron R, Resseguier N, Donnet A, Roussel P, Gaudart J, et al. Patterns of pain-free response in 497 cases of classic trigeminal neuralgia treated with gamma knife surgery and followed up for least 1 year. J Neurosurg. 2012;117(Suppl):181–8. doi: 10.3171/2012.8.GKS121015. [DOI] [PubMed] [Google Scholar]
- 98.Lee JK, Kim DR, Huh YH, Kim JK, Namgung WC, Hong SH. Long-term outcome of gamma knife surgery using a retrogasserian petrous bone target for classic trigeminal neuralgia. Acta Neurochir Suppl. 2013;116:127–35. doi: 10.1007/978-3-7091-1376-9_20. [DOI] [PubMed] [Google Scholar]
- 99.Lee JK, Choi HJ, Ko HC, Choi SK, Lim YJ. Long term outcomes of gamma knife radiosurgery for typical trigeminal neuralgia-minimum 5-year follow-up. J Korean Neurosurg Soc. 2012;51:276–80. doi: 10.3340/jkns.2012.51.5.276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Tang X, Wang Y, Shu Z, Hou Y. Efficacy and prognosis of trigeminal neuralgia treated with surgical excision or gamma knife surgery. Zhong Nan Da Xue Xue Bao Yi Xue Ban. 2012;37:616–20. doi: 10.3969/j.issn.1672-7347.2012.06.012. [DOI] [PubMed] [Google Scholar]
- 101.Dos Santos MA, Pérez de Salcedo JB, Gutiérrez Diaz JA, Nagore G, Calvo FA, Samblás J, et al. Outcome for patients with essential trigeminal neuralgia treated with linear accelerator stereotactic radiosurgery. Stereotact Funct Neurosurg. 2011;89:220–5. doi: 10.1159/000325672. [DOI] [PubMed] [Google Scholar]
- 102.Riesenburger RI, Hwang SW, Schirmer CM, Zerris V, Wu JK, Mahn K, et al. Outcomes following single-treatment gamma knife surgery for trigeminal neuralgia with a minimum 3-year follow-up. J Neurosurg. 2010;112:766–71. doi: 10.3171/2009.8.JNS081706. [DOI] [PubMed] [Google Scholar]
- 103.Park KJ, Kondziolka D, Kano H, Berkowitz O, Ahmed SF, Liu X, et al. Outcomes of gamma knife surgery for trigeminal neuralgia secondary to vertebrobasilar ectasia. J Neurosurg. 2012;116:73–81. doi: 10.3171/2011.8.JNS11920. [DOI] [PubMed] [Google Scholar]
- 104.Henson CF, Goldman HW, Rosenwasser RH, Downes MB, Bednarz G, Pequignot EC, et al. Glycerol rhizotomy versus gamma knife radiosurgery for the treatment of trigeminal neuralgia: An analysis of patients treated at one institution. Int J Radiat Oncol Biol Phys. 2005;63:82–90. doi: 10.1016/j.ijrobp.2005.01.033. [DOI] [PubMed] [Google Scholar]
- 105.Sanchez-Mejia RO, Limbo M, Cheng JS, Camara J, Ward MM, Barbaro NM. Recurrent or refractory trigeminal neuralgia after microvascular decompression, radiofrequency ablation, or radiosurgery. Neurosurg Focus. 2005;18:e12. doi: 10.3171/foc.2005.18.5.13. [DOI] [PubMed] [Google Scholar]
- 106.Loescher AR, Radatz M, Kemeny A, Rowe J. Stereotactic radiosurgery for trigeminal neuralgia: Outcomes and complications. Br J Neurosurg. 2012;26:45–52. doi: 10.3109/02688697.2011.591849. [DOI] [PubMed] [Google Scholar]
- 107.Marshall K, Chan MD, McCoy TP, Aubuchon AC, Bourland JD, McMullen KP, et al. Predictive variables for the successful treatment of trigeminal neuralgia with gamma knife radiosurgery. Neurosurgery. 2012;70:566–72. doi: 10.1227/NEU.0b013e3182320d36. [DOI] [PubMed] [Google Scholar]
- 108.Park YS, Kim JP, Chang WS, Kim HY, Park YG, Chang JW. Gamma knife radiosurgery for idiopathic trigeminal neuralgia as primary vs. secondary treatment option. Clin Neurol Neurosurg. 2011;113:447–52. doi: 10.1016/j.clineuro.2011.01.006. [DOI] [PubMed] [Google Scholar]
- 109.Lallemand F, Janvary ZL, Jansen N, Coucke P. Cyberknife and benign pathologies. Rev Med Liege. 2011;66:568–74. [PubMed] [Google Scholar]
- 110.Sudahar H, Kurup PG, Murali V, Velmurugan J. Dosimetric analysis of trigeminal nerve, brain stem doses in CyberKnife radiosurgery of trigeminal neuralgia. J Med Phys. 2012;37:124–8. doi: 10.4103/0971-6203.99225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Lazzara BM, Ortiz O, Bordia R, Witten MR, Haas JA, Katz AJ, et al. Cyberknife radiosurgery in treating trigeminal neuralgia. J Neurointerv Surg. 2013;5:81–5. doi: 10.1136/neurintsurg-2011-010125. [DOI] [PubMed] [Google Scholar]
- 112.Soboleva OI, Golanov AV, Gorlachev GE, Galkin MV, Kadasheva AB, Antipina NA, et al. CyberKnife stereotactic radiosurgery in the treatment of patients with trigeminal neuralgia. Zh Vopr Neirokhir Im N N Burdenko. 2012;76:79–83. [PubMed] [Google Scholar]
- 113.Chen MJ, Shao ZY, Zhang WJ, Wang ZH, Zhang WH, Hu HS. X-knife stereotactic radiosurgery on the trigeminal ganglion to treat trigeminal neuralgia: A preliminary study. Minim Invasive Neurosurg. 2010;53:223–8. doi: 10.1055/s-0030-1269926. [DOI] [PubMed] [Google Scholar]
- 114.Brown JA. Percutaneous balloon compression for trigeminal neuralgia. Clin Neurosurg. 2009;56:73–8. [PubMed] [Google Scholar]
- 115.Revuelta-Gutierrez R, Martinez-Anda JJ, Coll JB, Campos-Romo A, Perez-Peña N. Efficacy and safety of root compression of trigeminal nerve for trigeminal neuralgia without evidence of vascular compression. World Neurosurg. 2013;80:385–9. doi: 10.1016/j.wneu.2012.07.030. [DOI] [PubMed] [Google Scholar]
- 116.Chen JF, Tu PH, Lee ST. Repeated percutaneous balloon compression for recurrent trigeminal neuralgia: A long-term study. World Neurosurg. 2012;77:352–6. doi: 10.1016/j.wneu.2011.06.013. [DOI] [PubMed] [Google Scholar]
- 117.Kouzounias K, Lind G, Schechtmann G, Winter J, Linderoth B. Comparison of percutaneous balloon compression and glycerol rhizotomy for the treatment of trigeminal neuralgia. J Neurosurg. 2010;113:486–92. doi: 10.3171/2010.1.JNS091106. [DOI] [PubMed] [Google Scholar]
- 118.Van Gompel JJ, Kallmes DF, Morris JM, Fode-Thomas NC, Atkinson JL. Dyna-CT as an imaging adjunct to routine percutaneous balloon compression for trigeminal neuralgia. Stereotact Funct Neurosurg. 2009;87:330–3. doi: 10.1159/000235805. [DOI] [PubMed] [Google Scholar]
- 119.Chen JF, Tu PH, Lee ST. Long-term follow-up of patients treated with percutaneous balloon compression for trigeminal neuralgia in Taiwan. World Neurosurg. 2011;76:586–91. doi: 10.1016/j.wneu.2011.05.021. [DOI] [PubMed] [Google Scholar]
- 120.Montano N, Papacci F, Cioni B, Di Bonaventura R, Meglio M. Percutaneous balloon compression for the treatment of trigeminal neuralgia in patients with multiple sclerosis. Analysis of the potentially prognostic factors. Acta Neurochir (Wien) 2012;154:779–83. doi: 10.1007/s00701-012-1301-9. [DOI] [PubMed] [Google Scholar]
- 121.Asplund P, Linderoth B, Bergenheim AT. The predictive power of balloon shape and change of sensory functions on outcome of percutaneous balloon compression for trigeminal neuralgia. J Neurosurg. 2010;113:498–507. doi: 10.3171/2010.2.JNS091466. [DOI] [PubMed] [Google Scholar]
- 122.Skirving DJ, Dan NG. A 20-year review of percutaneous balloon compression of the trigeminal ganglion. J Neurosurg. 2001;94:913–7. doi: 10.3171/jns.2001.94.6.0913. [DOI] [PubMed] [Google Scholar]
- 123.Trojnik T, Smigoc T. Percutaneous trigeminal ganglion balloon compression rhizotomy: Experience in 27 patients. ScientificWorldJournal 2012. 2012:328936. doi: 10.1100/2012/328936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Chroni E, Constantoyannis C, Prasoulis I, Kargiotis O, Kagadis GC, Georgiopoulos M, et al. Masseter muscle function after percutaneous balloon compression of trigeminal ganglion for the treatment of trigeminal neuralgia: A neurophysiological follow-up study. Clin Neurophysiol. 2011;122:410–3. doi: 10.1016/j.clinph.2010.07.002. [DOI] [PubMed] [Google Scholar]
- 125.Bergenheim AT, Asplund P, Linderoth B. Percutaneous retrogasserian balloon compression for trigeminal neuralgia: Review of critical technical details and outcomes. World Neurosurg. 2013;79:359–68. doi: 10.1016/j.wneu.2012.03.014. [DOI] [PubMed] [Google Scholar]
- 126.Xu-Hui W, Chun Z, Guang-Jian S, Min-Hui X, Guang-Xin C, Yong-Wen Z, et al. Long-term outcomes of percutaneous retrogasserian glycerol rhizotomy in 3370 patients with trigeminal neuralgia. Turk Neurosurg. 2011;21:48–52. [PubMed] [Google Scholar]
- 127.Chen L, Xu M, Zou Y. Treatment of trigeminal neuralgia with percutaneous glycerol injection into Meckel's cavity: Experience in 4012 patients. Cell Biochem Biophys. 2010;58:85–9. doi: 10.1007/s12013-010-9094-z. [DOI] [PubMed] [Google Scholar]
- 128.Fransen P. Cost-effectiveness in the surgical treatments for trigeminal neuralgia. Acta Neurol Belg. 2012;112:245–7. doi: 10.1007/s13760-012-0095-0. [DOI] [PubMed] [Google Scholar]
- 129.Bender M, Pradilla G, Batra S, See A, Bhutiani N, James C, et al. Effectiveness of repeat glycerol rhizotomy in treating recurrent trigeminal neuralgia. Neurosurgery. 2012;70:1125–33. doi: 10.1227/NEU.0b013e31823f5eb6. [DOI] [PubMed] [Google Scholar]
- 130.Bozkurt M, Al-Beyati ES, Ozdemir M, Kahilogullari G, Elhan AH, Savas A, et al. Management of bilateral trigeminal neuralgia with trigeminal radiofrequency rhizotomy: A treatment strategy for the life-long disease. Acta Neurochir (Wien) 2012;154:785–91. doi: 10.1007/s00701-012-1311-7. [DOI] [PubMed] [Google Scholar]
- 131.Ishii A, Kubota Y, Okamoto S, Matsuoka G, Yato S, Hori T, et al. Electrical neurocoagulation may be effective for intractable trigeminal neuralgia caused by vertebrobasilar dolichoectasia. Neurosurg Rev. 2013;36:657–60. doi: 10.1007/s10143-013-0454-1. [DOI] [PubMed] [Google Scholar]
- 132.Weng Z, Halawa MA, Liu X, Zhou X, Yao S. Analgesic effects of preoperative peripheral nerve block in patients with trigeminal neuralgia undergoing radiofrequency thermocoagulation of gasserian ganglion. J Craniofac Surg. 2013;24:479–82. doi: 10.1097/SCS.0b013e31827c7d6f. [DOI] [PubMed] [Google Scholar]
- 133.Hart MG, Nowell M, Coakham HB. Radiofrequency thermocoagulation for trigeminal neuralgia without intra-operative patient waking. Br J Neurosurg. 2012;26:392–6. doi: 10.3109/02688697.2012.673650. [DOI] [PubMed] [Google Scholar]
- 134.Fang L, Ying S, Tao W, Lan M, Xiaotong Y, Nan J. 3D CT-guided pulsed radiofrequency treatment for trigeminal neuralgia. Pain Pract. 2014;14:16–21. doi: 10.1111/papr.12041. [DOI] [PubMed] [Google Scholar]
- 135.Luo F, Meng L, Wang T, Yu X, Shen Y, Ji N. Pulsed radiofrequency treatment for idiopathic trigeminal neuralgia: A retrospective analysis of the causes for ineffective pain relief. Eur J Pain. 2013;17:1189–92. doi: 10.1002/j.1532-2149.2012.00278.x. [DOI] [PubMed] [Google Scholar]
- 136.Li X, Ni J, Yang L, Wu B, He M, Zhang X, et al. A prospective study of gasserian ganglion pulsed radiofrequency combined with continuous radiofrequency for the treatment of trigeminal neuralgia. J Clin Neurosci. 2012;19:824–8. doi: 10.1016/j.jocn.2011.07.053. [DOI] [PubMed] [Google Scholar]
- 137.Yao P, Hong T, Zhu YQ, Li HX, Wang ZB, Ding YY, et al. Efficacy and safety of continuous radiofrequency thermocoagulation plus pulsed radiofrequency for treatment of V1 trigeminal neuralgia: A prospective cohort study. Medicine (Baltimore) 2016;95:e5247. doi: 10.1097/MD.0000000000005247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Ali FM, Prasant M, Pai D, Aher VA, Kar S, Safiya T. Peripheral neurectomies: A treatment option for trigeminal neuralgia in rural practice. J Neurosci Rural Pract. 2012;3:152–7. doi: 10.4103/0976-3147.98218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Zhu S, Rong Q, Chen S, Li X. Pterygopalatine fossa segment neurectomy of maxillary nerve through maxillary sinus route in treating trigeminal neuralgia. J Craniomaxillofac Surg. 2013;41:652–6. doi: 10.1016/j.jcms.2013.01.002. [DOI] [PubMed] [Google Scholar]
- 140.Abhinav K, Love S, Kalantzis G, Coakham HB, Patel NK. Clinicopathological review of patients with and without multiple sclerosis treated by partial sensory rhizotomy for medically refractory trigeminal neuralgia: A 12-year retrospective study. Clin Neurol Neurosurg. 2012;114:361–5. doi: 10.1016/j.clineuro.2011.11.018. [DOI] [PubMed] [Google Scholar]
- 141.Helbig GM, Callahan JD, Cohen-Gadol AA. Variant intraneural vein-trigeminal nerve relationships: An observation during microvascular decompression surgery for trigeminal neuralgia. Neurosurgery. 2009;65:958–61. doi: 10.1227/01.NEU.0000351757.29658.C0. [DOI] [PubMed] [Google Scholar]
- 142.Fernández-Carballal C, García-Salazar F, Pérez-Calvo J, García-Leal R, Gutiérrez FA, Carrillo R. Management of recurrent trigeminal neuralgia after failed microvascular decompression. Neurocirugia (Astur) 2004;15:345–52. doi: 10.1016/s1130-1473(04)70465-0. [DOI] [PubMed] [Google Scholar]
- 143.Kang IH, Park BJ, Park CK, Malla HP, Lee SH, Rhee BA. A clinical analysis of secondary surgery in trigeminal neuralgia patients who failed prior treatment. J Korean Neurosurg Soc. 2016;59:637–42. doi: 10.3340/jkns.2016.59.6.637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Young JN, Wilkins RH. Partial sensory trigeminal rhizotomy at the pons for trigeminal neuralgia. J Neurosurg. 1993;79:680–7. doi: 10.3171/jns.1993.79.5.0680. [DOI] [PubMed] [Google Scholar]
- 145.Sandell T, Eide PK. Effect of microvascular decompression in trigeminal neuralgia patients with or without constant pain. Neurosurgery. 2008;63:93–9. doi: 10.1227/01.NEU.0000335075.16858.EF. [DOI] [PubMed] [Google Scholar]
- 146.Zacest AC, Magill ST, Miller J, Burchiel KJ. Preoperative magnetic resonance imaging in type 2 trigeminal neuralgia. J Neurosurg. 2010;113:511–5. doi: 10.3171/2009.12.JNS09977. [DOI] [PubMed] [Google Scholar]
- 147.Han-Bing S, Wei-Guo Z, Jun Z, Ning L, Jian-Kang S, Yu C. Predicting the outcome of microvascular decompression for trigeminal neuralgia using magnetic resonance tomographic angiography. J Neuroimaging. 2010;20:345–9. doi: 10.1111/j.1552-6569.2009.00378.x. [DOI] [PubMed] [Google Scholar]
- 148.Sandell T, Eide PK. The effect of microvascular decompression in patients with multiple sclerosis and trigeminal neuralgia. Neurosurgery. 2010;67:749–53. doi: 10.1227/01.NEU.0000375491.81803.5D. [DOI] [PubMed] [Google Scholar]
- 149.Sekula RF, Frederickson AM, Jannetta PJ, Bhatia S, Quigley MR, Abdel Aziz KM. Microvascular decompression in patients with isolated maxillary division trigeminal neuralgia, with particular attention to venous pathology. Neurosurg Focus. 2009;27:E10. doi: 10.3171/2009.8.FOCUS09156. [DOI] [PubMed] [Google Scholar]
- 150.Yang XS, Li ST, Zhong J, Zhu J, Du Q, Zhou QM, et al. Microvascular decompression on patients with trigeminal neuralgia caused by ectatic vertebrobasilar artery complex: Technique notes. Acta Neurochir (Wien) 2012;154:793–7. doi: 10.1007/s00701-012-1320-6. [DOI] [PubMed] [Google Scholar]
- 151.Chen JC. Microvascular decompression for trigeminal neuralgia in patients with and without prior stereotactic radiosurgery. World Neurosurg. 2012;78:149–54. doi: 10.1016/j.wneu.2011.09.029. [DOI] [PubMed] [Google Scholar]
- 152.Sekula RF, Jr, Frederickson AM, Jannetta PJ, Quigley MR, Aziz KM, Arnone GD. Microvascular decompression for elderly patients with trigeminal neuralgia: A prospective study and systematic review with meta-analysis. J Neurosurg. 2011;114:172–9. doi: 10.3171/2010.6.JNS10142. [DOI] [PubMed] [Google Scholar]
- 153.Rughani AI, Dumont TM, Lin CT, Tranmer BI, Horgan MA. Safety of microvascular decompression for trigeminal neuralgia in the elderly. Clinical article. J Neurosurg. 2011;115:202–9. doi: 10.3171/2011.4.JNS101924. [DOI] [PubMed] [Google Scholar]
- 154.Ferroli P, Acerbi F, Tomei M, Tringali G, Franzini A, Broggi G. Advanced age as a contraindication to microvascular decompression for drug-resistant trigeminal neuralgia: Evidence of prejudice? Neurol Sci. 2010;31:23–8. doi: 10.1007/s10072-009-0156-1. [DOI] [PubMed] [Google Scholar]
- 155.Takao T, Oishi M, Fukuda M, Ishida G, Sato M, Fujii Y. Three-dimensional visualization of neurovascular compression: Presurgical use of virtual endoscopy created from magnetic resonance imaging. Neurosurgery. 2008;63(1 Suppl 1):ONS139–45. doi: 10.1227/01.neu.0000335028.77779.7c. [DOI] [PubMed] [Google Scholar]
- 156.Oishi M, Fukuda M, Hiraishi T, Yajima N, Sato Y, Fujii Y. Interactive virtual simulation using a 3D computer graphics model for microvascular decompression surgery. J Neurosurg. 2012;117:555–65. doi: 10.3171/2012.5.JNS112334. [DOI] [PubMed] [Google Scholar]
- 157.Du ZY, Gao X, Zhang XL, Wang ZQ, Tang WJ. Preoperative evaluation of neurovascular relationships for microvascular decompression in the cerebellopontine angle in a virtual reality environment. J Neurosurg. 2010;113:479–85. doi: 10.3171/2009.9.JNS091012. [DOI] [PubMed] [Google Scholar]
- 158.von Eckardstein KL, Mielke D, Akhavan-Sigari R, Rohde V. Enlightening the cerebellopontine angle: Intraoperative indocyanine green angiography in microvascular decompression for trigeminal neuralgia. J Neurol Surg A Cent Eur Neurosurg. 2017;78:161–6. doi: 10.1055/s-0036-1586746. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 159.Zhong J, Li ST, Zhu J, Guan HX, Zhou QM, Jiao W, et al. A clinical analysis on microvascular decompression surgery in a series of 3000 cases. Clin Neurol Neurosurg. 2012;114:846–51. doi: 10.1016/j.clineuro.2012.01.021. [DOI] [PubMed] [Google Scholar]
- 160.Hong W, Zheng X, Wu Z, Li X, Wang X, Li Y, et al. Clinical features and surgical treatment of trigeminal neuralgia caused solely by venous compression. Acta Neurochir (Wien) 2011;153:1037–42. doi: 10.1007/s00701-011-0957-x. [DOI] [PubMed] [Google Scholar]
- 161.Dumot C, Sindou M. Trigeminal neuralgia due to neurovascular conflicts from venous origin: An anatomical-surgical study (consecutive series of 124 operated cases) Acta Neurochir (Wien) 2015;157:455–66. doi: 10.1007/s00701-014-2330-3. [DOI] [PubMed] [Google Scholar]
- 162.Choudhari KA. Quadruple vessel involvement at root entry zone in trigeminal neuralgia. Clin Neurol Neurosurg. 2007;109:203–5. doi: 10.1016/j.clineuro.2006.09.009. [DOI] [PubMed] [Google Scholar]
- 163.Zheng X, Feng B, Hong W, Zhang W, Yang M, Tang Y, et al. Management of intraneural vessels during microvascular decompression surgery for trigeminal neuralgia. World Neurosurg. 2012;77:771–4. doi: 10.1016/j.wneu.2011.08.031. [DOI] [PubMed] [Google Scholar]
- 164.Oiwa Y, Hirohata Y, Okumura H, Yamaga H, Takayama M, Terui K, et al. Bone drilling in microvascular decompression for trigeminal neuralgia: High morphological variety of the petrous bone. No Shinkei Geka. 2013;41:601–7. [PubMed] [Google Scholar]
- 165.Fujimaki T, Kirino T. Combined transhorizontal-supracerebellar approach for microvascular decompression of trigeminal neuralgia. Br J Neurosurg. 2000;14:531–4. doi: 10.1080/02688690020005536. [DOI] [PubMed] [Google Scholar]
- 166.Bond AE, Zada G, Gonzalez AA, Hansen C, Giannotta SL. Operative strategies for minimizing hearing loss and other major complications associated with microvascular decompression for trigeminal neuralgia. World Neurosurg. 2010;74:172–7. doi: 10.1016/j.wneu.2010.05.001. [DOI] [PubMed] [Google Scholar]
- 167.Jagannath PM, Venkataramana NK, Bansal A, Ravichandra M. Outcome of microvascular decompression for trigeminal neuralgia using autologous muscle graft: A five-year prospective study. Asian J Neurosurg. 2012;7:125–30. doi: 10.4103/1793-5482.103713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Broggi G, Broggi M, Ferroli P, Franzini A. Surgical technique for trigeminal microvascular decompression. Acta Neurochir (Wien) 2012;154:1089–95. doi: 10.1007/s00701-012-1324-2. [DOI] [PubMed] [Google Scholar]
- 169.Ryu H, Yamamoto S. A simple technique for neurovascular decompression of the cranial nerves. Br J Neurosurg. 2000;14:132–4. doi: 10.1080/02688690050004561. [DOI] [PubMed] [Google Scholar]
- 170.Matsushima T, Yamaguchi T, Inoue TK, Matsukado K, Fukui M. Recurrent trigeminal neuralgia after microvascular decompression using an interposing technique. Teflon felt adhesion and the sling retraction technique. Acta Neurochir (Wien) 2000;142:557–61. doi: 10.1007/s007010050469. [DOI] [PubMed] [Google Scholar]
- 171.Masuoka J, Matsushima T, Kawashima M, Nakahara Y, Funaki T, Mineta T. Stitched sling retraction technique for microvascular decompression: Procedures and techniques based on an anatomical viewpoint. Neurosurg Rev. 2011;34:373–9. doi: 10.1007/s10143-011-0310-0. [DOI] [PubMed] [Google Scholar]
- 172.Shigeno T, Kumai J, Endo M, Oya S, Hotta S. Snare technique of vascular transposition for microvascular decompression – Technical note. Neurol Med Chir (Tokyo) 2002;42:184–9. doi: 10.2176/nmc.42.184. [DOI] [PubMed] [Google Scholar]
- 173.Komatsu F, Imai M, Hirayama A, Hotta K, Hayashi N, Oda S, et al. Endoscopic microvascular decompression with transposition for trigeminal neuralgia and hemifacial spasm: Technical note. J Neurol Surg A Cent Eur Neurosurg. 2016 doi: 10.1055/s-0036-1592077. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 174.Meybodi AT, Habibi Z, Miri M, Tabatabaie SA. Microvascular decompression for trigeminal neuralgia using the ‘stitched sling retraction’ technique in recurrent cases after previous microvascular decompression. Acta Neurochir (Wien) 2014;156:1181–7. doi: 10.1007/s00701-014-2092-y. [DOI] [PubMed] [Google Scholar]
- 175.Lin CF, Chen HH, Hernesniemi J, Lee CC, Liao CH, Chen SC, et al. An easy adjustable method of ectatic vertebrobasilar artery transposition for microvascular decompression. Clin Neurol Neurosurg. 2012;114:951–6. doi: 10.1016/j.clineuro.2012.02.021. [DOI] [PubMed] [Google Scholar]
- 176.Attabib N, Kaufmann AM. Use of fenestrated aneurysm clips in microvascular decompression surgery. Technical note and case series. J Neurosurg. 2007;106:929–31. doi: 10.3171/jns.2007.106.5.929. [DOI] [PubMed] [Google Scholar]
- 177.Ohta M, Komatsu F, Abe H, Sakamoto S, Tsugu H, Oshiro S, et al. Complication caused by use of fibrin glue in vessel transposition for trigeminal neuralgia. Neurol Med Chir (Tokyo) 2008;48:30–2. doi: 10.2176/nmc.48.30. [DOI] [PubMed] [Google Scholar]
- 178.Sindou M, Leston JM, Decullier E, Chapuis F. Microvascular decompression for trigeminal neuralgia: The importance of a noncompressive technique – Kaplan-Meier analysis in a consecutive series of 330 patients. Neurosurgery. 2008;63(4 Suppl 2):341–50. doi: 10.1227/01.NEU.0000327022.79171.D6. [DOI] [PubMed] [Google Scholar]
- 179.Skrap M, Tuniz F. Use of the arachnoid membrane of the cerebellopontine angle to transpose the superior cerebellar artery in microvascular decompression for trigeminal neuralgia: Technical note. Neurosurgery. 2010;66(3 Suppl Operative):88–91. doi: 10.1227/01.NEU.0000367556.35258.FA. [DOI] [PubMed] [Google Scholar]
- 180.Jie H, Xuanchen Z, Deheng L, Kun G, Fengyang X, Xiang C, et al. The long-term outcome of nerve combing for trigeminal neuralgia. Acta Neurochir (Wien) 2013;155:1703–8. doi: 10.1007/s00701-013-1804-z. [DOI] [PubMed] [Google Scholar]
- 181.Zhao H, Zhang X, Tang D, Li S. Nerve combing for trigeminal neuralgia without vascular compression. J Craniofac Surg. 2017;28:e15–6. doi: 10.1097/SCS.0000000000003161. [DOI] [PubMed] [Google Scholar]
- 182.Zhang L, Zhang Y, Li C, Zhu S. Surgical treatment of primary trigeminal neuralgia: Comparison of the effectiveness between MVD and MVD PSR in a series of 210 patients. Turk Neurosurg. 2012;22:32–8. doi: 10.5137/1019-5149.JTN.4447-11.2. [DOI] [PubMed] [Google Scholar]
- 183.Park JS, Kong DS, Lee JA, Park K. Intraoperative management to prevent cerebrospinal fluid leakage after microvascular decompression: Dural closure with a “plugging muscle” method. Neurosurg Rev. 2007;30:139–42. doi: 10.1007/s10143-006-0060-6. [DOI] [PubMed] [Google Scholar]
- 184.Li N, Zhao WG, Pu CH, Shen JK. Clinical application of artificial dura mater to avoid cerebrospinal fluid leaks after microvascular decompression surgery. Minim Invasive Neurosurg. 2005;48:369–72. doi: 10.1055/s-2005-915629. [DOI] [PubMed] [Google Scholar]
- 185.Tanrikulu L, Buchfelder M, Naraghi R. Fleece-bound tissue sealing in microvascular decompression. Turk Neurosurg. 2016 doi: 10.5137/1019-5149.JTN.17462-16.2. doi: 10.5137/1019-5149JTN17462-162 [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 186.Baliazin VA, Baliazina EV. Methods of reducing the number of complications and relapses after microvascular decompression in patients with trigeminal neuralgia. Zh Vopr Neirokhir Im N N Burdenko. 2003;2:6–9. [PubMed] [Google Scholar]
- 187.Zhang H, Lei D, You C, Mao BY, Wu B, Fang Y. The long-term outcome predictors of pure microvascular decompression for primary trigeminal neuralgia. World Neurosurg. 2013;79:756–62. doi: 10.1016/j.wneu.2012.01.040. [DOI] [PubMed] [Google Scholar]
- 188.Jo KW, Kong DS, Hong KS, Lee JA, Park K. Long-term prognostic factors for microvascular decompression for trigeminal neuralgia. J Clin Neurosci. 2013;20:440–5. doi: 10.1016/j.jocn.2012.03.037. [DOI] [PubMed] [Google Scholar]
- 189.Shibahashi K, Morita A, Kimura T. Surgical results of microvascular decompression procedures and patient's postoperative quality of life: Review of 139 cases. Neurol Med Chir (Tokyo) 2013;53:360–4. doi: 10.2176/nmc.53.360. [DOI] [PubMed] [Google Scholar]
- 190.Zhong J, Zhu J, Sun H, Dou NN, Wang YN, Ying TT, et al. Microvascular decompression surgery: Surgical principles and technical nuances based on 4000 cases. Neurol Res. 2014;36:882–93. doi: 10.1179/1743132814Y.0000000344. [DOI] [PubMed] [Google Scholar]
- 191.Linskey ME, Ratanatharathorn V, Peñagaricano J. A prospective cohort study of microvascular decompression and Gamma Knife surgery in patients with trigeminal neuralgia. J Neurosurg. 2008;109(Suppl):160–72. doi: 10.3171/JNS/2008/109/12/S25. [DOI] [PubMed] [Google Scholar]
- 192.Christiano LD, Singh R, Sukul V, Prestigiacomo CJ, Gandhi CD. Microvascular decompression for trigeminal neuralgia: Visualization of results in a 3D stereoscopic virtual reality environment. Minim Invasive Neurosurg. 2011;54:12–5. doi: 10.1055/s-0031-1273731. [DOI] [PubMed] [Google Scholar]
- 193.Oesman C, Mooij JJ. Long-term follow-up of microvascular decompression for trigeminal neuralgia. Skull Base. 2011;21:313–22. doi: 10.1055/s-0031-1284213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 194.Degn J, Brennum J. Surgical treatment of trigeminal neuralgia. Results from the use of glycerol injection, microvascular decompression, and rhizotomia. Acta Neurochir (Wien) 2010;152:2125–32. doi: 10.1007/s00701-010-0840-1. [DOI] [PubMed] [Google Scholar]
- 195.Simms HN, Honey CR. The importance of autonomic symptoms in trigeminal neuralgia. Clinical article. J Neurosurg. 2011;115:210–6. doi: 10.3171/2011.4.JNS101843. [DOI] [PubMed] [Google Scholar]
- 196.Broggi G, Ferroli P, Franzini A, Nazzi V, Farina L, La Mantia L, et al. Operative findings and outcomes of microvascular decompression for trigeminal neuralgia in 35 patients affected by multiple sclerosis. Neurosurgery. 2004;55:830–8. [PubMed] [Google Scholar]
- 197.Sarsam Z, Garcia-Fiñana M, Nurmikko TJ, Varma TR, Eldridge P. The long-term outcome of microvascular decompression for trigeminal neuralgia. Br J Neurosurg. 2010;24:18–25. doi: 10.3109/02688690903370289. [DOI] [PubMed] [Google Scholar]
- 198.Herweh C, Kress B, Rasche D, Tronnier V, Tröger J, Sartor K, et al. Loss of anisotropy in trigeminal neuralgia revealed by diffusion tensor imaging. Neurology. 2007;68:776–8. doi: 10.1212/01.wnl.0000256340.16766.1d. [DOI] [PubMed] [Google Scholar]
- 199.Chen F, Chen L, Li W, Li L, Xu X, Li W, et al. Pre-operative declining proportion of fractional anisotropy of trigeminal nerve is correlated with the outcome of micro-vascular decompression surgery. BMC Neurol. 2016;16:106. doi: 10.1186/s12883-016-0620-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 200.Thirumala P, Meigh K, Dasyam N, Shankar P, Sarma KR, Sarma DR, et al. The incidence of high-frequency hearing loss after microvascular decompression for trigeminal neuralgia, glossopharyngeal neuralgia, or geniculate neuralgia. J Neurosurg. 2015;123:1500–6. doi: 10.3171/2014.10.JNS141101. [DOI] [PubMed] [Google Scholar]
- 201.Lee CC, Liao CH, Lin CF, Yang TF, Hsu SP, Yen YS, et al. Brainstem auditory evoked potential monitoring and neuro-endoscopy: Two tools to ensure hearing preservation and surgical success during microvascular decompression. J Chin Med Assoc. 2014;77:308–16. doi: 10.1016/j.jcma.2014.02.016. [DOI] [PubMed] [Google Scholar]
- 202.Olson S, Atkinson L, Weidmann M. Microvascular decompression for trigeminal neuralgia: Recurrences and complications. J Clin Neurosci. 2005;12:787–9. doi: 10.1016/j.jocn.2005.08.001. [DOI] [PubMed] [Google Scholar]
- 203.Theodosopoulos PV, Marco E, Applebury C, Lamborn KR, Wilson CB. Predictive model for pain recurrence after posterior fossa surgery for trigeminal neuralgia. Arch Neurol. 2002;59:1297–302. doi: 10.1001/archneur.59.8.1297. [DOI] [PubMed] [Google Scholar]
- 204.Inoue H, Kondo A, Shimano H, Yasuda S. Recurrent trigeminal neuralgia at 20 years after surgery: Case report. Neurol Med Chir (Tokyo) 2013;53:37–9. doi: 10.2176/nmc.53.37. [DOI] [PubMed] [Google Scholar]
- 205.Vitali AM, Sayer FT, Honey CR. Recurrent trigeminal neuralgia secondary to teflon felt. Acta Neurochir (Wien) 2007;149:719–22. doi: 10.1007/s00701-007-1174-5. [DOI] [PubMed] [Google Scholar]
- 206.Kalkanis SN, Eskandar EN, Carter BS, Barker FG., 2nd Microvascular decompression surgery in the United States, 1996 to 2000: Mortality rates, morbidity rates, and the effects of hospital and surgeon volumes. Neurosurgery. 2003;52:1251–61. doi: 10.1227/01.neu.0000065129.25359.ee. [DOI] [PubMed] [Google Scholar]
- 207.Muratorio F, Tringali G, Levi V, Ligarotti GK, Nazzi V, Franzini AA. Hydrocephalus: An underrated long-term complication of microvascular decompression for trigeminal neuralgia. A single institute experience. Acta Neurochir (Wien) 2016;158:2203–6. doi: 10.1007/s00701-016-2911-4. [DOI] [PubMed] [Google Scholar]
- 208.Yadav YR, Parihar V, Namdev H, Agarwal M, Bhatele PR. Endoscopic interlaminar management of lumbar disc disease. J Neurol Surg A Cent Eur Neurosurg. 2013;74:77–81. doi: 10.1055/s-0032-1333127. [DOI] [PubMed] [Google Scholar]
- 209.Yadav YR, Parihar V, Kher Y, Bhatele PR. Endoscopic inter laminar management of lumbar disease. Asian J Neurosurg. 2016;11:1–7. doi: 10.4103/1793-5482.145377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 210.Yadav YR, Madhariya SN, Parihar VS, Namdev H, Bhatele PR. Endoscopic transoral excision of odontoid process in irreducible atlantoaxial dislocation: Our experience of 34 patients. J Neurol Surg A Cent Eur Neurosurg. 2013;74:162–7. doi: 10.1055/s-0032-1327441. [DOI] [PubMed] [Google Scholar]
- 211.Yadav YR, Parihar V, Janakiram N, Pande S, Bajaj J, Namdev H. Endoscopic management of cerebrospinal fluid rhinorrhea. Asian J Neurosurg. 2016;11:183–93. doi: 10.4103/1793-5482.145101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 212.Zada G, Woodmansee WW, Iuliano S, Laws ER. Perioperative management of patients undergoing transsphenoidal pituitary surgery. Asian J Neurosurg. 2010;5:1–6. [PMC free article] [PubMed] [Google Scholar]
- 213.Charalampaki P, Igressa A, Mahvash M, Pechlivanis I, Schick B. Optimal invasive key-hole neurosurgery with a miniaturized 3D chip on the tip: Microendoscopic device. Asian J Neurosurg. 2013;8:125–31. doi: 10.4103/1793-5482.121681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 214.Yadav YR, Parihar VS, Todorov M, Kher Y, Chaurasia ID, Pande S, et al. Role of endoscopic third ventriculostomy in tuberculous meningitis with hydrocephalus. Asian J Neurosurg. 2016;11:325–9. doi: 10.4103/1793-5482.145100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 215.Diyora B, Nayak N, Kukreja S, Sharma A. Hemorrhagic colloid cyst: Case report and review of the literature. Asian J Neurosurg. 2013;8:162. doi: 10.4103/1793-5482.121689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 216.Zohdi AZ, El Damaty AM, Aly KB, El Refaee EA. Success rate of endoscopic third ventriculostomy in infants below six months of age with congenital obstructive hydrocephalus (a preliminary study of eight cases) Asian J Neurosurg. 2013;8:147–52. doi: 10.4103/1793-5482.121686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 217.Jarrahy R, Eby JB, Cha ST, Shahinian HK. Fully endoscopic vascular decompression of the trigeminal nerve. Minim Invasive Neurosurg. 2002;45:32–5. doi: 10.1055/s-2002-23586. [DOI] [PubMed] [Google Scholar]
- 218.Yadav YR, Parihar V, Agarwal M, Sherekar S, Bhatele P. Endoscopic vascular decompression of the trigeminal nerve. Minim Invasive Neurosurg. 2011;54:110–4. doi: 10.1055/s-0031-1283129. [DOI] [PubMed] [Google Scholar]
- 219.Rak R, Sekhar LN, Stimac D, Hechl P. Endoscope-assisted microsurgery for microvascular compression syndromes. Neurosurgery. 2004;54:876–81. doi: 10.1227/01.neu.0000115151.52925.37. [DOI] [PubMed] [Google Scholar]
- 220.Miyazaki H, Deveze A, Magnan J. Neuro-otologic surgery through minimally invasive retrosigmoid approach: Endoscope assisted microvascular decompression, vestibular neurotomy, and tumor removal. Laryngoscope. 2005;115:1612–7. doi: 10.1097/01.mlg.0000172038.22929.63. [DOI] [PubMed] [Google Scholar]
- 221.Charalampaki P, Kafadar AM, Grunert P, Ayyad A, Perneczky A. Vascular decompression of trigeminal and facial nerves in the posterior fossa under endoscope-assisted keyhole conditions. Skull Base. 2008;18:117–28. doi: 10.1055/s-2007-1003927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 222.El-Garem HF, Badr-El-Dine M, Talaat AM, Magnan J. Endoscopy as a tool in minimally invasive trigeminal neuralgia surgery. Otol Neurotol. 2002;23:132–5. doi: 10.1097/00129492-200203000-00004. [DOI] [PubMed] [Google Scholar]
- 223.Abdeen K, Kato Y, Kiya N, Yoshida K, Kanno T. Neuroendoscopy in microvascular decompression for trigeminal neuralgia and hemifacial spasm: Technical note. Neurol Res. 2000;22:522–6. doi: 10.1080/01616412.2000.11740712. [DOI] [PubMed] [Google Scholar]
- 224.Sandell T, Ringstad GA, Eide PK. Usefulness of the endoscope in microvascular decompression for trigeminal neuralgia and MRI-based prediction of the need for endoscopy. Acta Neurochir (Wien) 2014;156:1901–9. doi: 10.1007/s00701-014-2171-0. [DOI] [PubMed] [Google Scholar]
- 225.Duntze J, Litré CF, Eap C, Théret E, Bazin A, Chays A, et al. Adjunctive use of endoscopy during microvascular decompression in the cerebellopontine angle: 27 case reports. Neurochirurgie. 2011;57:68–72. doi: 10.1016/j.neuchi.2011.03.003. [DOI] [PubMed] [Google Scholar]
- 226.Chen MJ, Zhang WJ, Yang C, Wu YQ, Zhang ZY, Wang Y. Endoscopic neurovascular perspective in microvascular decompression of trigeminal neuralgia. J Craniomaxillofac Surg. 2008;36:456–61. doi: 10.1016/j.jcms.2008.05.002. [DOI] [PubMed] [Google Scholar]
- 227.Jarrahy R, Berci G, Shahinian HK. Endoscope-assisted microvascular decompression of the trigeminal nerve. Otolaryngol Head Neck Surg. 2000;123:218–23. doi: 10.1067/mhn.2000.107451. [DOI] [PubMed] [Google Scholar]
- 228.Teo C, Nakaji P, Mobbs RJ. Endoscope-assisted microvascular decompression for trigeminal neuralgia: Technical case report. Neurosurgery. 2006;59(4 Suppl 2):ONSE489–90. doi: 10.1227/01.NEU.0000232768.47615.82. [DOI] [PubMed] [Google Scholar]
- 229.Artz GJ, Hux FJ, Larouere MJ, Bojrab DI, Babu S, Pieper DR. Endoscopic vascular decompression. Otol Neurotol. 2008;29:995–1000. doi: 10.1097/MAO.0b013e318184601a. [DOI] [PubMed] [Google Scholar]
- 230.Lang SS, Chen HI, Lee JY. Endoscopic microvascular decompression: A stepwise operative technique. ORL J Otorhinolaryngol Relat Spec. 2012;74:293–8. doi: 10.1159/000342795. [DOI] [PubMed] [Google Scholar]
- 231.Kher Y, Yadav N, Yadav YR, Parihar V, Ratre S, Bajaj J. Endoscopic vascular decompression in trigeminal neuralgia. Turk Neurosurg. 2016 doi: 10.5137/1019-5149.JTN.17046-16.1. doi: 10.5137/1019-5149JTN17046-161 [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 232.Bohman LE, Pierce J, Stephen JH, Sandhu S, Lee JY. Fully endoscopic microvascular decompression for trigeminal neuralgia: Technique review and early outcomes. Neurosurg Focus. 2014;37:E18. doi: 10.3171/2014.7.FOCUS14318. [DOI] [PubMed] [Google Scholar]
- 233.King WA, Wackym PA, Sen C, Meyer GA, Shiau J, Deutsch H. Adjunctive use of endoscopy during posterior fossa surgery to treat cranial neuropathies. Neurosurgery. 2001;49:108–15. doi: 10.1097/00006123-200107000-00017. [DOI] [PubMed] [Google Scholar]
- 234.Balansard ChF, Meller R, Bruzzo M, Chays A, Girard N, Magnan J. Trigeminal neuralgia: Results of microsurgical and endoscopic-assisted vascular decompression. Ann Otolaryngol Chir Cervicofac. 2003;120:330–7. [PubMed] [Google Scholar]
- 235.Huang H, Hu ZQ, Zhu GT, Guan F, Dai B, Mao BB, et al. Endoscopic microvacular decompression for trigeminal neuralgia. Zhonghua Yi Xue Za Zhi. 2011;91:2491–3. [PubMed] [Google Scholar]
- 236.Kabil MS, Eby JB, Shahinian HK. Endoscopic vascular decompression versus microvascular decompression of the trigeminal nerve. Minim Invasive Neurosurg. 2005;48:207–12. doi: 10.1055/s-2005-870928. [DOI] [PubMed] [Google Scholar]
- 237.Zhang W, Chen M, Zhang W, Chai Y. Trigeminal neuralgia: Evaluation of the relationship between the region of neuralgic manifestation and the site of neurovascular compression under endoscopy. J Craniofac Surg. 2015;26:1596–9. doi: 10.1097/SCS.0000000000001525. [DOI] [PubMed] [Google Scholar]


