Abstract
Rotational vertebral artery occlusion (RVAO) is a well-documented surgically amenable cause of vertebrobasilar insufficiency. Traditionally, patients have been imaged using dynamic rotational angiography. We report a case of RVAO in which intraoperative indocyanine green angiography (ICGA) was used to confirm adequate surgical decompression of the VA. A 57-year-old female who presented with multiple episodes of syncope provoked by turning her head to the right. Rotational dynamic angiography revealed a dominant right VA that became occluded at the level of C5/6 with head rotation to the right. The patient underwent successful surgical decompression of the VA via an anterior cervical approach. ICGA demonstrated VA patency with head rotation. This was further confirmed by intraoperative dynamic catheter angiography. To the best of our knowledge, we present the first use of ICG combined with intra-operative dynamic rotational angiography to document the adequacy surgical decompression of the VA in a patient with RVAO.
Keywords: Bow Hunter's syndrome, dynamic angiography, indocyanine green video angiography, rotation vertebral artery occlusion, vertebral artery
Introduction
Vertebrobasilar insufficiency caused by rotational vertebral artery (VA) compression is a surgically amenable risk factor for posterior circulation stroke. VA compression by a fibrous band or osseous prominence during rotational head movement is a difficult diagnosis to confirm and requires a high degree of clinical suspicion. Indocyanine green (ICG) angiography has been described for extracranial vertebral surgery in the setting of tumors, aneurysms, and strokes.[1] To the best of our knowledge, we report the first case of combined use of intraoperative ICG and dynamic rotational angiography to document successful decompression of the VA in the setting of rotation VA occlusion (RVAO) syndrome.
Case Report
History
The patient is a 57-year-old female with history of hypertension, hypercholesterolemia, and mitral valve regurgitation. She presented with multiple episodes of syncope over the prior few months. Each episode was transient and was provoked by rotating her head toward the right. All episodes were self-limiting with none resulting in permanent neurological injury.
Objective exam
An extensive workup was conducted including computed tomography (CT), CT angiography, magnetic resonance imaging and angiography, and digital subtraction angiography of the head and neck. Rotational dynamic angiography revealed a dominant right VA that became occluded at the level of C5/6 with head rotation to the right side. The vertebral flow was reestablished by neutralizing or turning the head to the left [Figure 1a and b]. The patient also had a hypoplastic left VA and fetal posterior communicating arteries bilaterally. Thus, her entire posterior circulation was primarily dependent on the right VA. Cervical spine CT showed that she had extensive degenerative changes and spondylosis including auto-fusion between C2 and C3 as well as at C6 and C7 [Figure 2].
Figure 1.
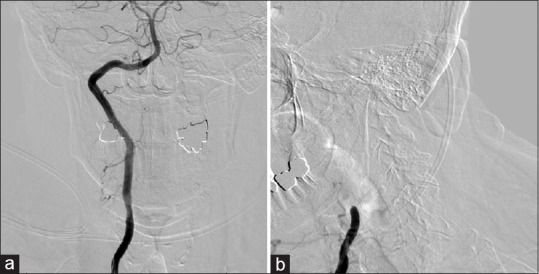
(a) Preoperative right vertebral artery angiogram (AP view) with the head neutral demonstrating patency of the vertebral artery. (b) Preoperative right vertebral artery angiogram (AP view) with the head turned to the right demonstrating occlusion of the vertebral artery segment at the level of C5/6
Figure 2.
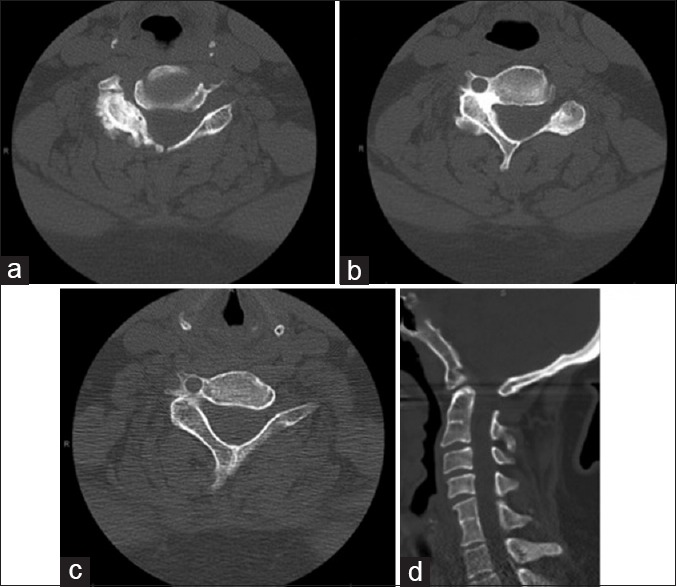
Preoperative computed tomography images of the cervical spine. (a) Axial section through the C5–6 disc space, (b) axial section through the right C5 foramen, (c) axial section through the right C6 foramen and (d) sagittal section of the cervical spine showing osteophytes and spondylotic changes on the right side
Treatment
The cause of the patient's syncope was determined to be hemodynamic insufficiency as the result of intermittent compression of the V2 segment of the VA at the level of C5/6.
The patient was taken to the operating room under general anesthesia and placed in the supine position with a shoulder roll placed in the interscapular region. Her neck was slightly extended. Baseline somatosensory and motor evoked potentials were obtained and continuously monitored throughout the duration of the procedure. A standard approach to the anterior cervical spine was performed utilizing an incision parallel to the anterior border of the sternocleidomastoid muscle.
The longus coli were dissected partially on the left side and more extensively on the right side, exposing the transverse processes of C5 to C7. The VA was identified as it entered the transverse foramen at C6, and the anterior bar of the transverse foramen at C5 and C6 was removed to decompress the artery. A partial discectomy and resection of the uncovertebral joint at C5–C6 on the right was performed. A fibrous band encasing the VA was identified and subsequently released. After the sectioning of the fibrous sheath, the VA began to expand and pulsate more prominently. An intraoperative ICG angiography demonstrated that the VA was patent during head rotation [Figure 3a]. This was also confirmed by an intraoperative right VA dynamic angiogram [Figure 3b]. The patient remains free of symptoms at 6-month follow-up.
Figure 3.
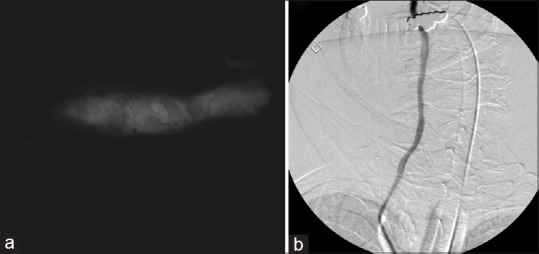
Postdecompression intraoperative indocyanine green (a) and right vertebral artery catheter angiography (b) with the head rotated to the right demonstrating adequate decompression of the vertebral artery
Discussion
RVAO, also known as Bow Hunter's syndrome (BHS), is clinical vertebrobasilar insufficiency caused by compression, stenosis, or occlusion of the VA with head rotation. Diagnosed clinically and confirmed by dynamic angiographic studies, BHS is a relatively rare, yet well-documented, entity that should be included in the differential diagnosis for patients who presents with dizziness, vertigo, ataxia, and syncope that is, provoked by head rotation. RVAO results in episodic, transient, and recurrent symptoms despite medical therapy[2] and only occurs when the contralateral VA is compromised (e.g., occlusion, stenosis, hypoplastic, or terminally ends in a posterior-inferior cerebellar artery) and there is no contribution from anterior circulation.[3] In addition to extrinsic compression, BHS has also been reported to occur as a result of VA stretching, vasospasm, and dissection. The vertigo associated with BHS is believed to occur as a result of transient superior vestibular labyrinth ischemia and is characterized by mixed torsional and downbeat nystagmus with a horizontal component beating toward the contralateral side of neck rotation during physical exam.[4,5]
Since BHS has been reported in the literature in the early 1900s, its diagnosis has been confirmed with various radiological modalities including dynamic angiography and duplex ultrasound. According to our review of the literature, we present the first case of successfully treated BHS confirmed with intraoperative ICG and standard catheter angiography.
Our review of the literature found 29 previously reported cases of RVAO diagnosed with dynamic angiography and 4 reported cases diagnosed with duplex ultrasonography. Including our case, the median age of diagnosis is 49 (8–77-year-old), with an approximately 3:1 ratio of male to female patients. The most common causes of occlusions are compression due to osteophytes[6,7,8,9,10,11] (30%; 10/34) and fibrous bands[12,13] (20%; 7/34) with C2 being the most commonly affected level[9,13,14,15,16,17,18] (35%; 12/34). The few cases of RVAO diagnosed with duplex ultrasonography were due to intrinsic, rather than extrinsic, causes of the occlusion such as atherosclerosis[17] and VA anomalies.[3]
An anterior surgical approach was used in approximately 50% (14/29) of patients who underwent surgery. We also used an anterior cervical approach to decompress the VA. Surgery for RVAO typically involves decompression of the VA, discectomy, and occasionally fusion if cervical instability is present.[3,7,12] A noteworthy surgical complication of high cervical anterolateral exposure is damage to the accessory nerve leading to a winged scapula.[19] Patients who refused surgery[2,11,13,16] or were not surgical candidates[2,3] were managed conservatively with the restriction of head motion, neck brace fixation, and/or anticoagulant therapies.
Conclusion
Intraoperative ICG angiography is a useful adjunct and may potentially supplant the need for intraoperative catheter angiography in demonstrating the adequacy of surgical decompression of the VA in patients with RVAO.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Bruneau M, Sauvageau E, Nakaji P, Vandesteene A, Lubicz B, Chang SW, et al. Preliminary personal experiences with the application of near-infrared indocyanine green videoangiography in extracranial vertebral artery surgery. Neurosurgery. 2010;66:305–11. doi: 10.1227/01.NEU.0000363596.52283.65. [DOI] [PubMed] [Google Scholar]
- 2.Iguchi Y, Kimura K, Shibazaki K, Iwanaga T, Ueno Y, Inoue T. Transcranial doppler and carotid duplex ultrasonography findings in Bow hunter's syndrome. J Neuroimaging. 2006;16:278–80. doi: 10.1111/j.1552-6569.2006.00040.x. [DOI] [PubMed] [Google Scholar]
- 3.Yeh JF, Lin YJ, Po HL, Wang SF, Pan PY, Cheng SJ, et al. A case of Bow hunter's stroke caused by non-dominant vertebral artery. Acta Neurol Taiwan. 2005;14:69–73. [PubMed] [Google Scholar]
- 4.Kim HA, Yi HA, Lee CY, Lee H. Origin of isolated vertigo in rotational vertebral artery syndrome. Neurol Sci. 2011;32:1203–7. doi: 10.1007/s10072-011-0667-4. [DOI] [PubMed] [Google Scholar]
- 5.Marti S, Hegemann S, von Büdingen HC, Baumgartner RW, Straumann D. Rotational vertebral artery syndrome: 3D kinematics of nystagmus suggest bilateral labyrinthine dysfunction. J Neurol. 2008;255:663–7. doi: 10.1007/s00415-008-0773-2. [DOI] [PubMed] [Google Scholar]
- 6.Lu DC, Zador Z, Mummaneni PV, Lawton MT. Rotational vertebral artery occlusion-series of 9 cases. Neurosurgery. 2010;67:1066–72. doi: 10.1227/NEU.0b013e3181ee36db. [DOI] [PubMed] [Google Scholar]
- 7.Miele VJ, France JC, Rosen CL. Subaxial positional vertebral artery occlusion corrected by decompression and fusion. Spine (Phila Pa 1976) 2008;33:E366–70. doi: 10.1097/BRS.0b013e31817192a1. [DOI] [PubMed] [Google Scholar]
- 8.Petridis AK, Barth H, Buhl R, Mehdorn HM. Vertebral artery decompression in a patient with rotational occlusion. Acta Neurochir (Wien) 2008;150:391–4. doi: 10.1007/s00701-008-1502-4. [DOI] [PubMed] [Google Scholar]
- 9.Taylor WB, 3rd, Vandergriff CL, Opatowsky MJ, Layton KF. Bow hunter's syndrome diagnosed with provocative digital subtraction cerebral angiography. Proc (Bayl Univ Med Cent) 2012;25:26–7. doi: 10.1080/08998280.2012.11928776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Tsutsumi S, Ito M, Yasumoto Y. Simultaneous bilateral vertebral artery occlusion in the lower cervical spine manifesting as bow hunter's syndrome. Neurol Med Chir (Tokyo) 2008;48:90–4. doi: 10.2176/nmc.48.90. [DOI] [PubMed] [Google Scholar]
- 11.Velat GJ, Reavey-Cantwell JF, Ulm AJ, Lewis SB. Intraoperative dynamic angiography to detect resolution of Bow hunter's syndrome: Technical case report. Surg Neurol. 2006;66:420–3. doi: 10.1016/j.surneu.2006.03.040. [DOI] [PubMed] [Google Scholar]
- 12.Kuether TA, Nesbit GM, Clark WM, Barnwell SL. Rotational vertebral artery occlusion: A mechanism of vertebrobasilar insufficiency. Neurosurgery. 1997;41:427–32. doi: 10.1097/00006123-199708000-00019. [DOI] [PubMed] [Google Scholar]
- 13.Saito K, Hirano M, Taoka T, Nakagawa H, Kitauchi T, Tanizawa E, et al. Artery-to-artery embolism with a mobile mural thrombus due to rotational vertebral artery occlusion. J Neuroimaging. 2010;20:284–6. doi: 10.1111/j.1552-6569.2008.00309.x. [DOI] [PubMed] [Google Scholar]
- 14.Cornelius JF, George B, N’dri Oka D, Spiriev T, Steiger HJ, Hänggi D. Bow-hunter's syndrome caused by dynamic vertebral artery stenosis at the cranio-cervical junction – A management algorithm based on a systematic review and a clinical series. Neurosurg Rev. 2012;35:127–35. doi: 10.1007/s10143-011-0343-4. [DOI] [PubMed] [Google Scholar]
- 15.Matsuyama T, Morimoto T, Sakaki T. Bow hunter's stroke caused by a nondominant vertebral artery occlusion: Case report. Neurosurgery. 1997;41:1393–5. doi: 10.1097/00006123-199712000-00030. [DOI] [PubMed] [Google Scholar]
- 16.Sakai K, Tsutsui T. Bow hunter's stroke associated with atlantooccipital assimilation – Case report. Neurol Med Chir (Tokyo) 1999;39:696–700. doi: 10.2176/nmc.39.696. [DOI] [PubMed] [Google Scholar]
- 17.Tominaga T, Takahashi T, Shimizu H, Yoshimoto T. Rotational vertebral artery occlusion from occipital bone anomaly: A rare cause of embolic stroke. Case report. J Neurosurg. 2002;97:1456–9. doi: 10.3171/jns.2002.97.6.1456. [DOI] [PubMed] [Google Scholar]
- 18.Yoshimura K, Iwatsuki K, Ishihara M, Onishi Y, Umegaki M, Yoshimine T. Bow hunter's stroke due to instability at the uncovertebral C3/4 joint. Eur Spine J. 2011;20(Suppl 2):S266–70. doi: 10.1007/s00586-010-1669-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Fox MW, Piepgras DG, Bartleson JD. Anterolateral decompression of the atlantoaxial vertebral artery for symptomatic positional occlusion of the vertebral artery. Case report. J Neurosurg. 1995;83:737–40. doi: 10.3171/jns.1995.83.4.0737. [DOI] [PubMed] [Google Scholar]


