Abstract
Hypoxia is a common feature of many solid tumours, including cervical cancer. Aggressive tumour progression is mostly associated with hypoxia. Furthermore, hypoxic conditions in tumours are also associated with resistance to chemotherapy and radiation, and with poor prognosis. Hypoxia inducible factor (HIF)-1, composed of a constitutively expressed β-subunit (HIF-β/ARNT) and one of the three known oxygen-regulated α-subunits, HIF-1α, HIF-2α, or HIF-3α, mediates the tumour cell response to hypoxia. The distinction between the roles of HIF-1α and HIF-2α in tumorigenesis is not clearly delineated. Therefore, the aim of the present study was to investigate the effect of HIF-2α on the characteristics of a cervical cancer cell line and to compare the functions of HIF-1α and HIF-2α. The present study demonstrated that the levels of HIF-1α and HIF-2α expression increased under hypoxic exposure compared with normoxia. The major difference was the temporal expression of HIF-1α and HIF-2α, with expression of the two proteins peaking at different time-points. In addition, HIF-1α and HIF-2α had similar effects on proliferation, cell cycle and apoptosis. Suppression of expression of HIF-1α or HIF-2α inhibited proliferation, induced G1-phase arrest and promoted apoptosis in the cervical cancer cell line CaSki. However, the effects of HIF-1α and HIF-2α on invasion and cell autophagy were different. The inhibitory effect of HIF-1α on cell invasion was stronger compared with HIF-2α, while the inhibitory effect of HIF-1α on cell autophagy was weaker compared with HIF-2α. Together, these results demonstrate that HIF-1α and HIF-2α have similar effects on the characteristics of a cervical cancer cell line. The major difference that the authors observed between the effects exerted by the two proteins on the cervical cancer cell line studied is the extent of their effect on invasion and autophagy.
Keywords: hypoxia inducible factor-1α, hypoxia inducible factor-2α, cell invasion, autophagy, cervical cancer
Introduction
Cervical cancer is the second most commonly diagnosed cancer and third leading cause of mortality due to cancer among women in underdeveloped countries (1). In 2012, there were an estimated 527,600 novel cervical cancer cases and 265,700 mortalities worldwide (1). Although the majority of patients can be cured with treatments based on surgery and radiotherapy, a significant number eventually develop recurrent disease, with the the risk of recurrence being 10–20% for patients with stage IB-IIA [International Federation of Gynecology and Obstetrics (FIGO) stage] and 50–70% for those in stages IIB-IVA2 (2,3). With advances in the development of molecular-targeted drugs, novel diagnostic and therapeutic molecular targets may enable the development of novel therapies for cervical cancer. Therefore, it is important to study proteins that are differentially expressed or overexpressed in cervical cancer cells and investigate the mechanisms regulating the expression of these proteins.
Hypoxia, a reduction in tissue oxygen tension due to inadequate oxygen supply, is a common phenomenon that occurs in a majority of solid tumours in humans (4). The presence of hypoxia is associated with aggressive tumour progression, resistance to chemotherapy and radiation, and poor prognosis (5,6). Tumour cells and tissues adapt to a hypoxic microenvironment through the activation of a number of hypoxia-associated molecules and pathways, among which the hypoxia-inducible factor (HIF) is the most predominant factor (7). HIF is a heterodimeric basic helix-loop-helix PAS (Per-ARNT-Sim) domain-containing transcription factor that consists of a constitutively expressed β-subunit (HIF-β/ARNT) and one of the three oxygen-regulated α-subunits, HIF-1α, HIF-2α and HIF-3α (8,9). The α-subunits are constitutively transcribed and translated, but are regulated at the protein level by oxygen dependent hydroxylation of specific prolyl residues (10). In cervical cancer, the majority of studies on HIF have focused on HIF-1α. A number of studies have revealed significant associations between HIF-1α expression, FIGO stages, tumour grade and size (11). Although clinically relevant associations between HIF-1α expression and lymph node metastasis were not identified (12), HIF-1α was demonstrated to trigger angiogenesis and tumour invasiveness to surrounding tissues at an early stage of cervical carcinoma (13), and the inhibition of HIF-1α attenuated cell migration under normoxia and hypoxia in the uterine cervix cancer cell line SiHa (14). In addition, HIF-1α may affect proliferation, apoptosis and cell cycle (14,15). To date, there are a limited number of studies on the function of HIF-2α in cervical cancer. To the best of our knowledge, the only two studies on HIF-2α in cervical cancer have focused on radiotherapy. One study demonstrated that HIF-2α expression may have an important role in radioresistance in patients with locally advanced cervical cancer (16). The other study indicated that the proportion of HIF-2α-positive cells in tumour infiltrative macrophages may be a novel predictive indicator for prognosis prior to radiation therapy for uterine cervical cancer (17).
The difference in the roles of HIF-1α and HIF-2α in tumorigenesis remains to be clearly delineated. In the present study, the authors aimed to investigate the effect of HIF-2α on the characteristics of the cervical cancer cell line, including proliferation, apoptosis, cell cycle, invasion and cell autophagy. Furthermore, the authors of the present study investigated the function of HIF-1α to enable comparison with that of HIF-2α. The results of the present study indicate that HIF-1α and HIF-2α have similar effects on the characteristics of a cervical cancer cell line.
Materials and methods
Cell culture and hypoxic exposure
The human cervical cancer cell line CaSki was purchased from America Type Culture Collection (ATCC; Manassas, VA, USA). CaSki cells were grown in RPMI-1640 medium (HyClone; GE Healthcare Life Sciences, Logan, UT, USA) with 10% fetal bovine serum (FBS; Gibco; Thermo Fisher Scientific, Inc., Waltham, MA, USA), supplemented with 100 U/ml penicillin G and 100 µg/ml streptomycin (Sigma-Aldrich; Merck KGaA, Darmstadt, Germany). The cells were maintained at 37°C in a humidified 5% CO2 incubator. To expose cells to hypoxia, the cells were cultured in a Billups-Rothenburg chamber with 94% N2, 1% O2 and 5% CO2 at 37°C.
RNA interference
Small interfering RNA (siRNA) targeting HIF-1α and HIF-2α were purchased from Shanghai Gene-Pharma Co., Ltd. (Shanghai, China). The siRNA sequences used were as follows: HIF-1α siRNA sense, 5′-GCCACUUCGAAGUAGUGCUTT-3′ and antisense, 5′-AGCACUACUUCGAAGUGGCTT-3′; HIF-2α siRNA sense, 5′-GCGACAGCUGGAGUAUGAATT-3′ and antisense, 5′-UUCAUACUCCAGCUGUCGCTT-3′; negative control siRNA sense, 5′-UUCUCCGAACGUGUCACGUTT-3′ and antisense, 5′-ACGUGACACGUUCGGAGAATT-3′. The cells were transfected with siRNAs by using Lipofectamine 2000 (Invitrogen; Thermo Fisher Scientific, Inc.) according to the manufacturer's instructions. The knockdown efficiency was determined by quantitative PCR and western blot analysis. A total of three independent transfection experiments were performed.
RNA extraction and reverse transcription-quantitative polymerase chain reaction (RT-qPCR)
Total RNA was extracted from each group of CaSki cells using TRIzol reagent (Invitrogen; Thermo Fisher Scientific, Inc.) according to the manufacturer's instructions. RNA was reverse transcribed into cDNA using a PrimeScript RT reagent kit with cDNA eraser (Takara Biotechnology Co., Ltd., Dalian, China) in a 10 µl reaction according to the manufacturer's instructions. Equal amounts of cDNAs were used as templates for RT-qPCR to detect the levels of HIF-1α and HIF-2α expression relative to that of 18S rRNA (endogenous control). The expression levels were quantified using the ABI PRISM 7500 Sequence Detection system with the SYBR Green qPCR SuperMix (Invitrogen; Thermo Fisher Scientific, Inc.). Primers used in the present study were as follows: HIF-1α forward, 5′-GTGGATTACCACAGCTGA-3′ and reverse, 5′-GCTCAGTTAACTTGATCCA-3′; HIF-2α forward, 5′-AATCCGAGCAGTGGAGTCAT-3′ and reverse, 5′-ACGTGCCATCAGACCCTCTT-3′; and 18S rRNA forward, 5′-CCTGGATACCGCAGCTAGGA-3′ and reverse, 5′-GCGGCGCAATACGAATGCCCC-3′. Experiments were performed in duplicate and were repeated three times. Fold induction of gene expression was calculated using the 2−ΔΔCq method (18).
Western blot analysis
CaSki cells in each group were washed twice with ice-cold phosphate-buffered saline and resuspended in ice-cold RIPA buffer (Beyotime Institute of Biotechnology, Nantong, China) containing 1 mmol/l phenylmethanesulfonyl fluoride and a cocktail of protease inhibitors (1:100; Beyotime Institute of Biotechnology). The samples were centrifuged at 4°C for 15 min at 800 × g. The supernatants were recovered and the total protein was quantified using BCA Protein Assay kit (Pierce; Thermo Scientific Inc.). Protein (30 µg) was loaded and separated on 8–12% SDS polyacrylamide gels and transferred to polyvinylidene difluoride membranes (EMD Millipore, Billerica, MA, USA). The membranes were blocked for 1 h at room temperature with 5% milk in TBS containing 0.05% Tween-20 (TBST) and incubated at 37°C for 1 h with anti-HIF-1α mouse monoclonal antibody (1:2,000 dilution, cat. no. ab113642), anti-HIF-2α mouse monoclonal antibody (dilution 1:2,000, cat. no. ab157249), anti-LC3B rabbit monoclonal antibody (dilution 1:1,000, cat. no. ab192890), to anti-Beclin 1 rabbit polyclonal antibody (dilution 1:500, cat. no. ab62557) and anti-GAPDH mouse monoclonal antibody (dilution 1:5,000, cat. no. ab8245) (all purchased from Abcam, Cambridge, MA, USA). The membranes were subsequently washed three times with TBST and incubated with a horseradish peroxidase-conjugated mouse anti-rabbit IgG (1:2,000, cat no. BM2006) or horseradish peroxidase-conjugated goat anti-mouse IgG (1:3,000, cat. no. BA1051) (Wuhan Boster Biological Technology, Ltd., Wuhan, China) for 40 min at 37°C. The membranes were then washed three times with TBST and visualized using Immobilon Western Chemiluminescent horseradish peroxidase substrate (EMD Millipore). GAPDH served as an internal loading control. The images of the blots were scanned, and densitometric analysis was performed using Image Pro-Plus 6.0 software (Media Cybernetics, Inc., Rockville, MD, USA). For quantification of specific bands, a square of the same size was drawn around each band to measure the density, and then the value was adjusted according to the density of the background near that band. The results of densitometric analysis have been expressed as a relative ratio of the target protein to reference protein. The relative ratio of the target protein of control group was arbitrarily presented as 1.
Cell proliferation assays
Proliferation of CaSki cells was monitored using the Cell Counting Kit-8 (CCK-8; Dojindo Molecular Technologies, Inc., Kumamoto, Japan) according to the manufacturer's instructions. A total of 24 h following transfection, the cells were seeded at 1×104/well in a 96-well plate. The optical density (OD) of each group was measured at 16, 24, 48 and 72 h. Briefly, 10 µl WST-8 was added to each well, and after 4 h of incubation at 37°C. Absorbance at 490 nm was measured using a microplate reader (Multiskan MK3; Thermo Fisher Scientific, Inc.). The proliferation ratio was calculated using the formula: Proliferation rate (survival rate) = (ODtest/ODnegative control) × 100%. All experiments were performed in triplicate and repeated three times.
Flow cytometric analysis
CaSki cells from each group were digested with trypsin and centrifuged at 100 × g for 5 min. Following collection, the cells were washed twice with PBS and centrifuged at 100 × g for 5 min. For cell apoptosis analysis, Annexin V-allophycocyanin (APC) apoptosis detection kit (Nanjing KeyGen Biotech Co., Ltd., Nanjing, China) was used to detect the apoptotic rate according to the manufacturer's instructions (Nanjing KeyGen Biotech Co., Ltd.). Briefly, the cell pellet (~1-5×105 cells) was resuspended in 500 µl binding buffer. Then, 1.25 µl Annexin V-APC and 10 µl 7-aminoactinomycin D were added and mixed at room temperature (protected from light) for 15 min. Within 1 h, the cells in each group were detected by flow cytometry (BD Biosciences, San Jose, CA, USA) and data were interpreted using the FlowJo software version 8 (Tree Star, Inc., Ashland, OR, USA). For cell cycle analysis, cell cycle detection kits were used to detect cell cycle according to the manufacturer's instructions (Nanjing KeyGen Biotech Co., Ltd.). Briefly, the cells were fixed in 500 µl 70% precooled ethanol at 4°C overnight. An equal amount of PBS was added twice for washing. Up to 100 µl RNase A was added at 37°C for 30 min, followed by the addition of 100 µl propidium iodide at 4°C in the dark for 30 min. The different stages of the cell cycle were detected by flow cytometry (BD Biosciences) and cell cycle distribution was acquired using the ModFit LT 3.0 program (BD Biosciences). Each experiment was repeated three times.
Matrigel-Transwell invasion assay
CaSki cells from each group were harvested, and 1×105 cells in 100 µl serum-free medium were placed into the upper chamber of an insert pre-coated with Matrigel (pore size, 8 µm; BD Biosciences). The lower chamber was filled with 10% FBS (600 µl, Gibco; Thermo Fisher Scientific, Inc.). After 24 h incubation and removal of the cells on the upper chamber of the filter with a cotton swab, the cells on the underside were fixed with 4% paraformaldehyde for 15 min. The cells were subsequently stained with 0.1% crystal violet in 20% ethanol and counted in five randomly selected fields using a phase contrast microscope. Migrating cells were monitored by imaging them at ×200 magnification with an Olympus microscope (Olympus, Tokyo, Japan) in six independent fields for each well. The assays were performed in triplicate.
Transmission electron microscope
At the end of the intervention, CaSki cells from each group were digested with 0.25% trypsin and collected in centrifuge tubes, followed by centrifugation at 100 × g for 10 min at 4°C and then by a second centrifugation at a speed of 80 × g at 4°C for the same duration. The supernatant was discarded, and 2.5% glutaraldehyde was added to the tubes to fix the cells at 4°C for 2 h. Subsequent to dehydration and embedding, ultra-thin sections (70 nm) were prepared using a microtome and each section was mounted on a copper grid. Samples were contrasted in 4% aqueous uranyl acetate (10 min) and then in Reynolds lead citrate (2 min) using normal methods (19). The autophagosomes were observed under a transmission electron microscope (JEM-1010; Matsunaga Manufacturing, Yourou-cho, Japan), and images were captured. Images were captured in three fields and the assays were performed in triplicate. The number of autophagosomes was counted by two independent researchers.
Statistical analysis
All statistical analyses were performed using SPSS software, version 19.0 (IBM Corp., Armonk, NY, USA). Data are expressed as the mean ± standard deviation. Statistical comparisons were performed using one-way analysis of variance, followed by Scheffe's test. The statistical differences between two groups were determined using unpaired Student's t-test. P<0.05 was considered to indicate a statistically significant difference.
Results
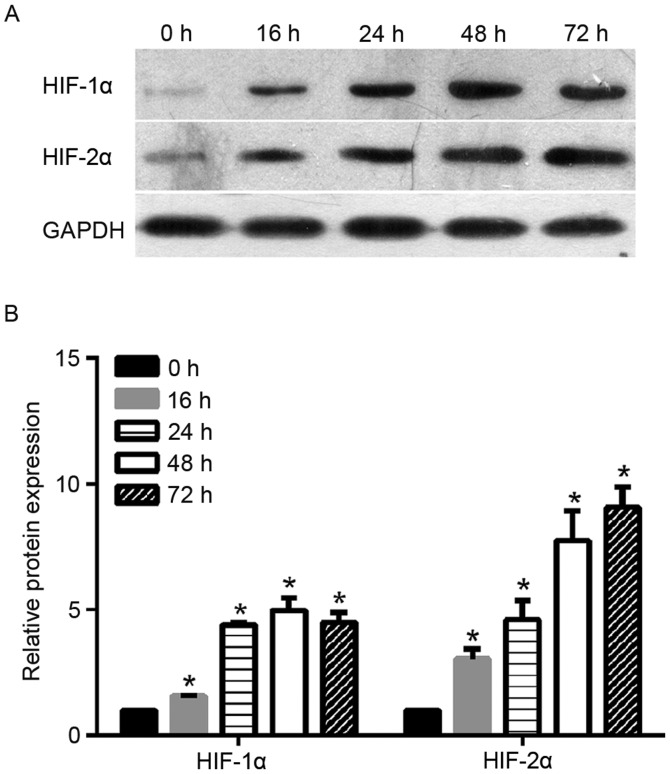
Expression profile of HIF-1α and HIF-2α under hypoxic exposure
To investigate the function of HIF-2α in cervical cancer, the authors of the present study monitored the protein expression levels of HIF-2α under hypoxic exposure at different time-points (0, 16, 24, 48 and 72 h). As shown in Fig. 1, the levels of HIF-2α protein increased steadily in the cervical cancer cells under hypoxic exposure from 16 to 72 h. The increase in HIF-2α protein expression in cells under hypoxic exposure was statistically significant when compared with the expression in cells under normoxia (0 h). As a control, the authors also monitored the protein expression level of HIF-1α under hypoxic exposure. As shown in Fig. 1, HIF-1α protein level increased steadily under hypoxic exposure from 16 to 24 h and peaked at 48 h. Similar to HIF-2α, the increase of level HIF-1α protein expression in cells under hypoxic exposure was statistically significant when compared with cells under normoxia (0 h).
Figure 1.
Protein expression profile of HIF-1α and HIF-2α under hypoxia at different time-points. (A) Representative images of levels of HIF-1α and HIF-2α protein as detected by western blot analysis. (B) Quantification of the expression levels of HIF-1α and HIF-2α in each group, presented as bar graphs. Bars represent fold change. *P<0.05 vs. 0 h. HIF, hypoxia-inducible factor.
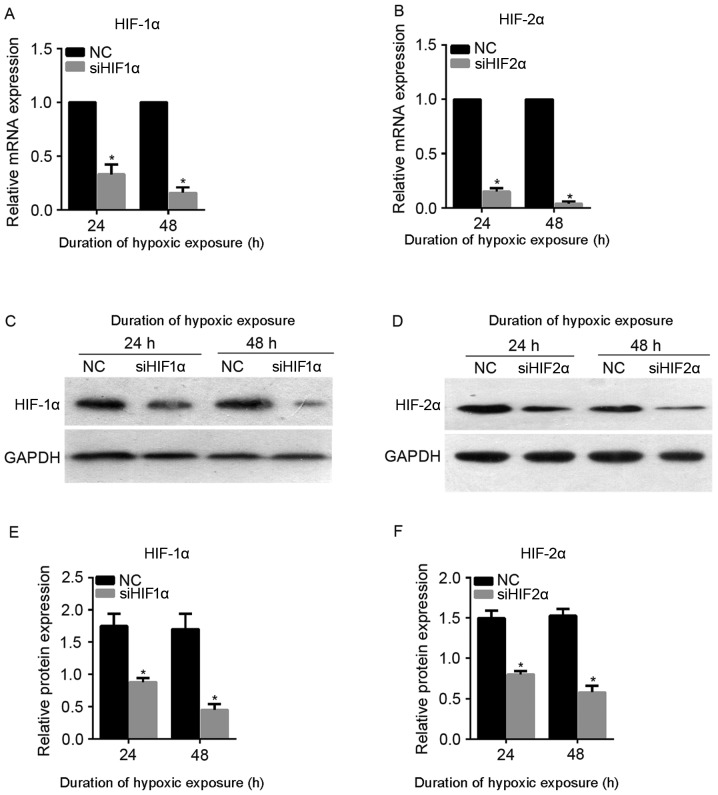
siHIF1α and siHIF2α may suppress the expression of HIF-1α and HIF-2α under hypoxic exposure
To attenuate the expression of HIF-1α and HIF-2α under hypoxic exposure, siHIF1α and siHIF2α were synthesized and transiently transfected into CaSki cells. The transfected CaSki cells were cultured under hypoxic exposure for 24 or 48 h. As shown in Fig. 2A and B, the mRNA expression level of HIF-1α and HIF-2α was successfully downregulated following siHIF1α or siHIF2α transfection at 24 and 48 h under hypoxic exposure. Furthermore, the level of protein expression was also successfully downregulated following siHIF1α or siHIF2α transfection at 24 and 48 h under hypoxic exposure (Fig. 2C-F). Therefore, transfection with siHIF1α or siHIF2α was able to successfully suppress the expression of HIF-1α and HIF-2α, respectively, under hypoxic exposure, and siHIF1α and siHIF2α were used for subsequent assays.
Figure 2.
mRNA and protein levels of HIF-1α and HIF-2α following siHIF1α and siHIF2α transfection under hypoxia. The mRNA levels of (A) HIF-1α and (B) HIF-2α following siHIF1α and siHIF2α transfection under hypoxia as detected by quantitative reverse transcription-polymerase chain reaction. The levels of protein expression of (C) HIF-1α and (D) HIF-2α following siHIF1α and siHIF2α transfection under hypoxia as detected by western blotting. Quantification of the expression levels of (E) HIF-1α and (F) HIF-2α in each group presented in bar graphs as fold increase. *P<0.05 vs. NC. HIF, hypoxia-inducible factor; NC, negative control; si, small interfering.
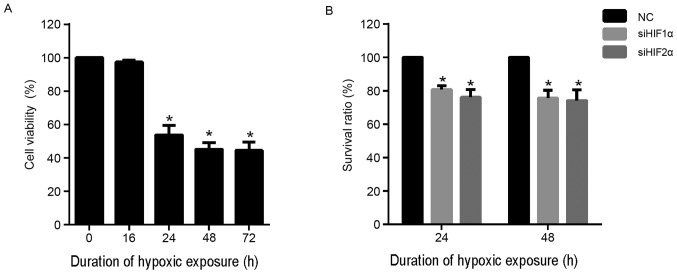
Effect of HIF-1α and HIF-2α silencing on cell proliferation in cervical cancer under hypoxic exposure
To determine the suitable duration of hypoxic exposure for the assays performed during the present study, CaSki cells were cultured under hypoxic conditions for 0, 16, 24, 48 and 72 h. CCK-8 assay was performed to detect the viability of each group of cells. As shown in Fig. 3A, there was no evident effect on cell viability when the duration of hypoxic exposure was 16 h. However, hypoxic exposure for 24, 48 and 72 h was able to significantly inhibit viability compared with normoxia (0 h). In addition, the effect of hypoxic exposure for 48 and 72 h was similar. Based on these results, duration of hypoxic exposure of 24 and 48 h were selected for further assays.
Figure 3.
Effect of silencing of HIF-1α and HIF-2α on cell proliferation under hypoxic exposure as detected by Cell Counting Kit-8 assay. (A) The viability of cells under hypoxic exposure for 0, 16, 24, 48 and 72 h. (B) The effect of HIF-1α and HIF-2α silencing on proliferation under hypoxic exposure. *P<0.05 vs. NC. HIF, hypoxia-inducible factor; NC, negative control.
To investigate the effect of inhibition of HIF-2α expression on cell proliferation, CaSki cells were transfected with siHIF2α or negative control (NC) and cultured under hypoxia for 24 and 48 h. The results for the CCK-8 assay demonstrated that suppression of HIF-2α expression significantly suppressed the viability of CaSki cells at 24 and 48 h compared with the NC group under hypoxia (Fig. 3B). Similarly, HIF-1α suppression also significantly suppressed the viability of CaSki cells at 24 and 48 h compared with the NC group under hypoxia (Fig. 3B).
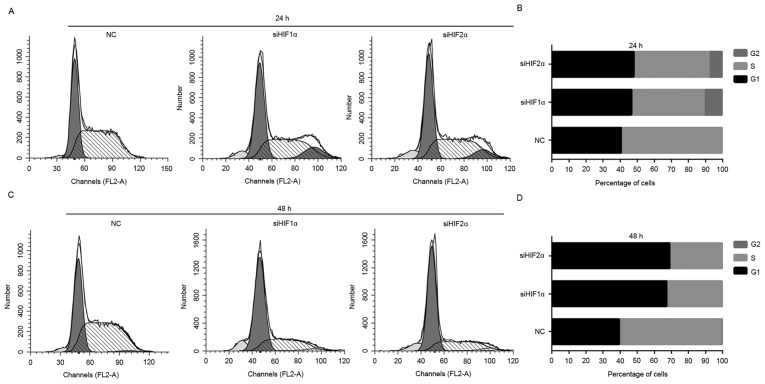
Effect of HIF-1α suppression and HIF-2α expression on cell cycle in cervical cancer under hypoxic exposure
To uncover the underlying mechanism of suppression of cell proliferation by downregulation of HIF-1α and HIF-2α expression, flow cytometry was used to observe the distribution of cells at different stages of the cell cycle. The downregulation of HIF-1α and HIF-2α expression induced a significant G1-phase and G2-phase arrest in CaSki cells, and the percentage of CaSki cells in S phase decreased significantly when placed for 24 h under hypoxic exposure (Fig. 4A and B). Downregulation of HIF-1α and HIF-2α expression induced a significant G1 phase arrest of CaSki cells, and the percentage of cells in S phase decreased markedly when placed for 48 h under hypoxic exposure compared with the NC-transfected group (Fig. 4C and D).
Figure 4.
Effect of suppression of HIF-1α and HIF-2α expression on cell cycle in cervical cancer under hypoxic exposure. (A) Representative graph of results from flow cytometric analysis of cell cycle of CaSki cells from each treatment group under hypoxic exposure for 24 h. (B) The percentage of cells in each cell phase from each treatment group under hypoxic exposure for 24 h. (C) Representative graph of results from flow cytometry of cell cycle of CaSki cells from each treatment group under hypoxic exposure for 48 h. (D) The percentage of cells in each cell phase from each treatment group under hypoxic exposure for 48 h. HIF, hypoxia-inducible factor; NC, negative control; si, small interfering.
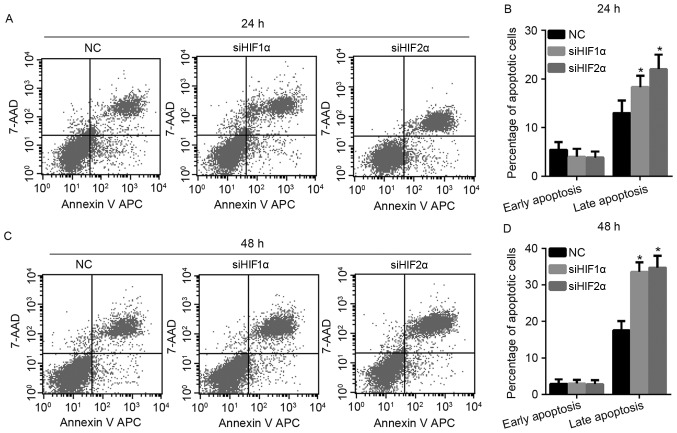
Effect of HIF-1α and HIF-2α suppression on cell apoptosis in cervical cancer under hypoxic exposure
To investigate the effect of HIF-1α and HIF-2α suppression on apoptosis in cervical cancer under hypoxic exposure, the authors of the present study monitored cell apoptosis by flow cytometry. As shown in Fig. 5A and B, when all the cells were exposed to hypoxia for 24 h, the percentage of late apoptotic cells increased when the expression of HIF-1α and HIF-2α was suppressed, while there was no effect on the percentage of early apoptotic cells in the siHIF1α and siHIF2α-transfected group compared with the NC-transfected group. The effect of HIF-1α and HIF-2α suppression on cell apoptosis at 48 h under hypoxic exposure was similar to the effect elicited by culturing the cells for 24 h under hypoxic exposure, as shown in Fig. 5C and D.
Figure 5.
Effect of HIF-1α and HIF-2α suppression on cell apoptosis in cervical cancer under hypoxic conditions. (A) Representative graph of flow cytometry results with Annexin V-APC/7-AAD staining of CaSki cells under hypoxic exposure for 24 h. (B) The percentage of early apoptotic and late apoptotic CaSki cells under hypoxic exposure for 24 h. (C) Representative graph of flow cytometry results with Annexin V-APC/7-AAD staining of CaSki cells under hypoxic exposure for 48 h. (D) The percentage of early apoptotic and late apoptotic CaSki cells under hypoxic exposure for 48 h. *P<0.05 vs. NC. APC, allophycocyanin; HIF, hypoxia-inducible factor; NC, negative control; si, small interfering; 7-AAD, 7-aminoactinomycin D.
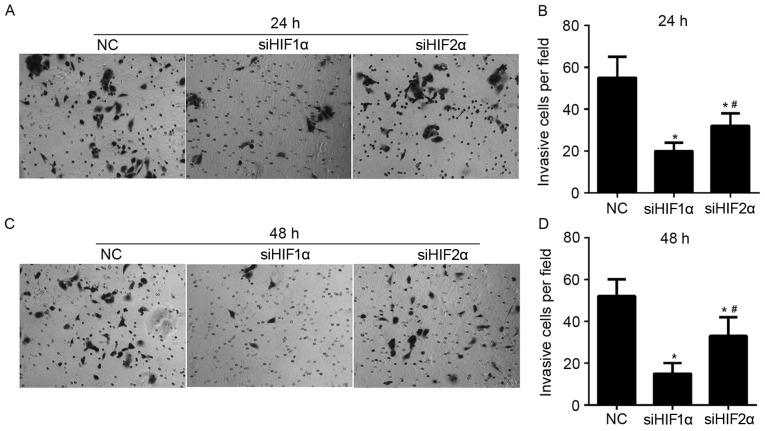
Effect of HIF-1α and HIF-2α suppression on cell invasion in cervical cancer under hypoxic exposure
To demonstrate the role of HIF-1α and HIF-2α in regulating invasion of CaSki cells, Matrigel-Transwell assays were performed following siHIF1α, siHIF2α or NC transfection under hypoxic exposure. The number of cells that passed through the Matrigel-coated membrane into the lower chamber was significantly lower in the siHIF1α or siHIF2α-transfected cells compared with the NC-transfected cells that were cultured for 24 h under hypoxic exposure (Fig. 6A and B). The number of cells that passed through the Matrigel-coated membrane onto the lower chamber was significantly higher in siHIF2α-transfected cells compared with the siHIF1α-transfected cells cultured for 24 h under hypoxic exposure (Fig. 6A and B). The effect of HIF-1α and HIF-2α suppression on invasion in cells cultured for 48 h under hypoxic exposure was similar to the effect on cells cultured for 24 h under hypoxic exposure, as shown in Fig. 6C and D.
Figure 6.
Effect of HIF-1α and HIF-2α suppression on cell invasion in cervical cancer under hypoxic exposure. (A) Representative graph of Matrigel-Transwell results of CaSki cells in each treatment group under hypoxic exposure for 24 h. Magnification, ×200. (B) Quantification of invasive cells per field in each group under hypoxic exposure for 24 h, presented in bar graphs. (C) Representative graph of Matrigel-Transwell results of CaSki cells in each treatment group under hypoxic exposure for 48 h. Magnification, ×200. (D) Quantification of invasive cells per field in each group under hypoxic exposure for 48 h, presented in bar graphs. *P<0.05 vs. NC; #P<0.05 vs. siHIF2α group. HIF, hypoxia-inducible factor; NC, negative control; si, small-interfering.
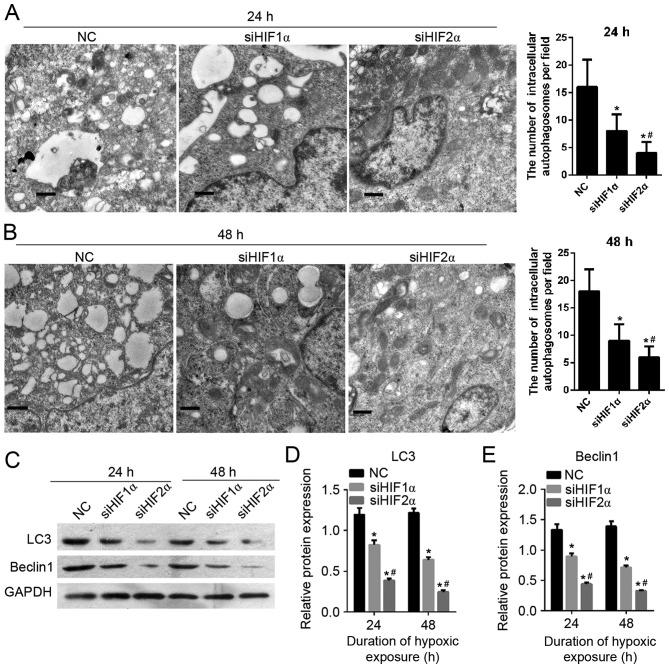
Effect of HIF-1α and HIF-2α suppression on cell autophagy in cervical cancer under hypoxic exposure
To detect the effect of HIF-1α and HIF-2α suppression on CaSki cell autophagy, the formation of autophagosomes was observed using transmission electron microscopy. As shown in Fig. 7A and B, the number of intracellular autophagosomes following siHIF1α or siHIF2α transfection decreased compared with the cells in the NC-transfected group which were cultured under hypoxic exposure for 24 h. The cells in the siHIF2α and siHIF1α-transfected groups were cultured under hypoxia for 24 h. There was a lower number of intracellular autophagosomes in the siHIF2α-transfected group compared with the siHIF-1α-transfected group. Furthermore in order to determine the effect of HIF-1α and HIF-2α suppression on cell autophagy, the expression of autophagy-related gene LC3 and beclin 1 was examined using western blotting. The level of protein expression of LC3 and beclin 1 following siHIF1α or siHIF2α transfection was decreased compared with the NC-transfected group under hypoxia for 24 h (Fig. 7C-E). The level of LC3 and beclin1 protein expression in cells (cultured under hypoxia for 24 h) in the siHIF2α-transfected group was lower compared with the expression in the NC-transfected group (Fig. 7C-E). The effect of HIF-1α and HIF-2α suppression on cell autophagy on cells cultured for 48 h under hypoxia was similar to the effect on cells cultured for 24 h under hypoxia, as shown in Fig. 7C-E.
Figure 7.
Effect of HIF-1α and HIF-2α suppression on cell autophagy in cervical cancer cells under hypoxia. (A) Representative transmission electron microscope images (left) and statistical result of the number of intracellular autophagosomes per field (right) from each treatment group. The cells were cultured for 24 h under hypoxic exposure. Scale bar, 600 nm. (B) Representative transmission electron microscope images (left) and statistical result of the number of intracellular autophagosomes per field (right) from each group, where the cells were cultured for 48 h under hypoxic exposure. Scale bar, 600 nm. (C) Representative images of the level of protein expression of autophagy-related gene LC3 and beclin 1 as examined using western blotting. (D and E) Quantification of the expression levels of LC3 and beclin 1 in each group, presented in bar graphs as fold increase. *P<0.05 vs. NC; #P<0.05 vs. siHIF2α group. HIF, hypoxia-inducible factor; LC3, autophagy-related protein LC3; NC, negative control; si, small interfering.
Discussion
Cancer cells adapt to hypoxia by stabilising HIF-α isoforms, which increase the transcription of several genes (10). Among the genes regulated by HIF are enzymes that have a role in proliferation, invasion, metastasis and metabolism of tumour cells (20). To date, numerous cancer studies have investigated HIF-1α as an important cancer drug target (21). In cervical cancer, HIF-1α is able to affect proliferation, apoptosis, cell cycle and invasion (14,15). However, less is known about HIF-2α, another HIF-α isoform. Furthermore, one previous study demonstrated that the HIF isoforms (HIF-1α and HIF-2α) have divergent effects on invasion, metastasis, metabolism and formation of lipid droplets in human breast cancer cells (10). Therefore, the present study comprehensively investigated the function of HIF-2α in cervical cancer cell line CaSki and compared the function of HIF-1α and HIF-2α on proliferation, cell cycle, apoptosis, cell invasion and cell autophagy. To the best our knowledge, this is the first study where two isoforms of HIFα have been investigated simultaneously in cervical cancer. The effect of HIF-1α and HIF-2α on cell autophagy has also been investigated in the present study.
In the present study, the authors investigated the function of HIF-1α and HIF-2α on proliferation, cell cycle, apoptosis, invasion and cell autophagy. The results indicated that HIF-1α and HIF-2α have similar effects on proliferation, cell cycle and apoptosis. HIF-1α or HIF-2α suppression may suppress proliferation, induce G1 phase arrest and promote apoptosis in cervical cancer cell line CaSki. However, the effect of HIF-1α and HIF-2α on invasion and cell autophagy was different. The inhibitory effect of HIF-1α on invasion was greater compared with the effect of HIF-2α, while the inhibitory effect of HIF-1α on cell autophagy was weaker compared with HIF-2α. The results revealed that HIF-1α and HIF-2α have similar effects on the characteristics of the cervical cancer cell line. The only difference is that the degree of effect on cell invasion and autophagy. This similarity in the roles of HIF-1α and HIF-2α in cervical cancer was supported by the studies of HIF expression under hypoxia in the present study. It was demonstrated that the level of HIF-1α and HIF-2α expression was increased under hypoxia compared with normoxia. The major difference was that the time-point at which the expression of these proteins peaked. These results show that HIF-1α and HIF-2α may have different roles at different stages of tumour progression, and hence at different stages of hypoxia.
The results of the present study vary from a number of previous studies (10,22,23). In colon cancer, HIF-1α and HIF-2α have divergent roles in cell proliferation and migration (22). Specifically, HIF-1α-deficient cells exhibit lower rates of proliferation and migration. However, HIF-2α-deficient cells exhibit increased anchorage independent growth in a soft agar assay (22). In human breast cancer cells, suppression of only one of the HIF-1α or HIF-2α protein expression was not sufficient to attenuate invasiveness, and cells with suppression of expression of both proteins show significant reduction in invasive characteristics (10). In hepatocellular carcinoma, the knockdown of HIF-2α increased the autophagic activity of the tumour cells, and attenuated apoptosis by increasing HIF-1α expression (23). These results show that the functions of HIF-1α and HIF-2α in cancer cells may differ with the type of cancer, and this may be due to differences in the downstream genes regulated by them.
In conclusion, the expression of HIF-1α and HIF-2α increased under hypoxic exposure. The suppression of HIF-1α or HIF-2α was able to inhibit proliferation, migration and autophagy, induce G1 phase arrest and promote apoptosis. Therefore, HIF-1α and HIF-2α exert a similar role in altering the biological characteristics of cervical cancer cell line CaSki.
Acknowledgements
The present study was supported by grants from the National Natural Science Foundation of China (grant no. 30760280), the Natural Science Foundation of Jiangxi, China (grant nos. 2011ZBAB204019 and 20132BAB205101), and Science and Technology Support Program of Jiangxi Province, China (grant nos. 2007BS12802 and 20142BBG70044). Funding was also provided by the Educational Department Foundation of Jiangxi Province, China (grant nos. GJJ08126, GJJ10060 and GJJ13682), and the Public Health Department of Jiangxi Province, China (grant nos. 20072016, 20092025 and 20113071).
References
- 1.Torre LA, Bray F, Siegel RL, Ferlay J, Lortet-Tieulent J, Jemal A. Global cancer statistics, 2012. CA Cancer J Clin. 2015;65:87–108. doi: 10.3322/caac.21262. [DOI] [PubMed] [Google Scholar]
- 2.Kawano M, Mabuchi S, Matsumoto Y, Sasano T, Takahashi R, Kuroda H, Kozasa K, Hashimoto K, Isobe A, Sawada K, et al. The significance of G-CSF expression and myeloid-derived suppressor cells in the chemoresistance of uterine cervical cancer. Sci Rep. 2015;5:18217. doi: 10.1038/srep18217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Eifel PJ, Winter K, Morris M, Levenback C, Grigsby PW, Cooper J, Rotman M, Gershenson D, Mutch DG. Pelvic irradiation with concurrent chemotherapy versus pelvic and para-aortic irradiation for high-risk cervical cancer: An update of radiation therapy oncology group trial (RTOG) 90–01. J Clin Oncol. 2004;22:872–880. doi: 10.1200/JCO.2004.07.197. [DOI] [PubMed] [Google Scholar]
- 4.Li SH, Shin DH, Chun YS, Lee MK, Kim MS, Park JW. A novel mode of action of YC-1 in HIF inhibition: Stimulation of FIH-dependent p300 dissociation from HIF-1{alpha} Mol Cancer Ther. 2008;7:3729–3738. doi: 10.1158/1535-7163.MCT-08-0074. [DOI] [PubMed] [Google Scholar]
- 5.Lou JJ, Chua YL, Chew EH, Gao J, Bushell M, Hagen T. Inhibition of hypoxia-inducible factor-1alpha (HIF-1alpha) protein synthesis by DNA damage inducing agents. PLoS One. 2010;5:0010522. doi: 10.1371/journal.pone.0010522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Zhang J, Cao J, Weng Q, Wu R, Yan Y, Jing H, Zhu H, He Q, Yang B. Suppression of hypoxia-inducible factor 1α (HIF-1α) by tirapazamine is dependent on eIF2α phosphorylation rather than the mTORC1/4E-BP1 pathway. PLoS One. 2010;5:0013910. doi: 10.1371/journal.pone.0013910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rankin EB, Giaccia AJ. The role of hypoxia-inducible factors in tumorigenesis. Cell Death Differ. 2008;15:678–685. doi: 10.1038/cdd.2008.21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hu CJ, Sataur A, Wang L, Chen H, Simon MC. The N-terminal transactivation domain confers target gene specificity of hypoxia-inducible factors HIF-1alpha and HIF-2alpha. Mol Biol Cell. 2007;18:4528–4542. doi: 10.1091/mbc.E06-05-0419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Tian H, McKnight SL, Russell DW. Endothelial PAS domain protein 1 (EPAS1), a transcription factor selectively expressed in endothelial cells. Genes Dev. 1997;11:72–82. doi: 10.1101/gad.11.1.72. [DOI] [PubMed] [Google Scholar]
- 10.Shah T, Krishnamachary B, Wildes F, Mironchik Y, Kakkad SM, Jacob D, Artemov D, Bhujwalla ZM. HIF isoforms have divergent effects on invasion, metastasis, metabolism and formation of lipid droplets. Oncotarget. 2015;6:28104–28119. doi: 10.18632/oncotarget.4612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Huang M, Chen Q, Xiao J, Yao T, Bian L, Liu C, Lin Z. Overexpression of hypoxia-inducible factor-1α is a predictor of poor prognosis in cervical cancer: A clinicopathologic study and a meta-analysis. Int J Gynecol Cancer. 2014;24:1054–1064. doi: 10.1097/IGC.0000000000000162. [DOI] [PubMed] [Google Scholar]
- 12.Ellingsen C, Andersen LM, Galappathi K, Rofstad EK. Hypoxia biomarkers in squamous cell carcinoma of the uterine cervix. BMC Cancer. 2015;15:805. doi: 10.1186/s12885-015-1828-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kim NS, Kang YJ, Jo JO, Kim HY, Oh YR, Kim YO, Jung MH, Ock MS, Cha HJ. Elevated expression of thymosin β4, vascular endothelial growth factor (VEGF) and hypoxia inducible factor (HIF)-1α in early-stage cervical cancers. Pathol Oncol Res. 2011;17:493–502. doi: 10.1007/s12253-010-9327-x. [DOI] [PubMed] [Google Scholar]
- 14.Tang B, Qu Y, Zhao F, Mao M, Tang J, Li X, Ferriero D, Mu D. In vitro effects of hypoxia-inducible factor 1alpha on the biological characteristics of the SiHa uterine cervix cancer cell line. Int J Gynecol Cancer. 2009;19:898–904. doi: 10.1111/IGC.0b013e3181a14f9a. [DOI] [PubMed] [Google Scholar]
- 15.Schwock J, Geddie WR, Hedley DW. Analysis of hypoxia-inducible factor-1alpha accumulation and cell cycle in geldanamycin-treated human cervical carcinoma cells by laser scanning cytometry. Cytometry A. 2005;68:59–70. doi: 10.1002/cyto.a.20192. [DOI] [PubMed] [Google Scholar]
- 16.Kim MK, Kim TJ, Sung CO, Choi CH, Lee JW, Bae DS, Kim BG. Clinical significance of HIF-2α immunostaining area in radioresistant cervical cancer. J Gynecol Oncol. 2011;22:44–48. doi: 10.3802/jgo.2011.22.1.44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kawanaka T, Kubo A, Ikushima H, Sano T, Takegawa Y, Nishitani H. Prognostic significance of HIF-2alpha expression on tumor infiltrating macrophages in patients with uterine cervical cancer undergoing radiotherapy. J Med Invest. 2008;55:78–86. doi: 10.2152/jmi.55.78. [DOI] [PubMed] [Google Scholar]
- 18.Livak KJ, Schmittgen TD. Analysis of relative gene expression data using real-time quantitative PCR and the 2(-Delta Delta C(T)) method. Methods. 2001;25:402–408. doi: 10.1006/meth.2001.1262. [DOI] [PubMed] [Google Scholar]
- 19.Lin Q, Wang Y, Chen D, Sheng X, Liu J, Xiong H. Cisplatin regulates cell autophagy in endometrial cancer cells via the PI3K/AKT/mTOR signalling pathway. Oncol Lett. 2017;13:3567–3571. doi: 10.3892/ol.2017.5894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lin D, Wu J. Hypoxia inducible factor in hepatocellular carcinoma: A therapeutic target. World J Gastroenterol. 2015;21:12171–12178. doi: 10.3748/wjg.v21.i42.12171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Masoud GN, Li W. HIF-1alpha pathway: Role, regulation and intervention for cancer therapy. Acta Pharm Sin B. 2015;5:378–389. doi: 10.1016/j.apsb.2015.05.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Imamura T, Kikuchi H, Herraiz MT, Park DY, Mizukami Y, Mino-Kenduson M, Lynch MP, Rueda BR, Benita Y, Xavier RJ, Chung DC. HIF-1alpha and HIF-2alpha have divergent roles in colon cancer. Int J Cancer. 2009;124:763–771. doi: 10.1002/ijc.24032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Menrad H, Werno C, Schmid T, Copanaki E, Deller T, Dehne N, Brüne B. Roles of hypoxia-inducible factor-1alpha (HIF-1alpha) versus HIF-2alpha in the survival of hepatocellular tumor spheroids. Hepatology. 2010;51:2183–2192. doi: 10.1002/hep.23597. [DOI] [PubMed] [Google Scholar]