Abstract
We present a case of a 57-year-old man who presented with progressive cerebellar dysarthria and cerebellar ataxia. Additional investigations confirmed the diagnosis of progressive multifocal leukoencephalopathy (PML) in the posterior fossa. This is a demyelinating disease of the central nervous system, caused by an opportunistic infection with John Cunningham virus. PML has previously been considered a lethal condition, but because of careful monitoring of patients with HIV and of patients using immunosuppressive drugs it is discovered in earlier stages and prognosis can be improved. Our patient had no known immune-compromising state, but further work-up revealed that the PML was most likely the first presentation of a previous untreated autoimmune disorder: sarcoidosis.
Keywords: neurology, brain stem / cerebellum, infection (neurology), neuroimaging, immunology
Background
Progressive multifocal leukoencephalopathy (PML) is a life-threatening demyelinating disease of the central nervous system (CNS) caused by a viral infection, usually encountered in immune-compromised patients.1 With this case, we illustrate that physicians should also be aware of PML in supposedly immune-competent patients.
Case presentation
A 57-year-old man presented at a regional hospital with a 3-month history of gradually worsening of articulation and right-sided coordination problems. His medical history mentioned Raynaud phenomenon and transient muscle complaints with spontaneous normalised positive antinuclear antibodies (ANA) 15 years ago. Neurological examination revealed a cerebellar dysarthria and ataxia of his right arm and leg.
Investigations
MRI scanning of the brain showed non-specific white matter lesions in both cerebellar hemispheres, without contrast enhancement or diffusion restriction. Routine blood serum and cerebrospinal fluid (CSF) examinations were normal. ANA and extractable nuclear antigens (ENA) were increased; the antineutrophil cytoplasmic antibodies were negative. The patient clinically deteriorated during the following week and was referred to our university hospital for further work-up. Repeated CSF examination showed a mild mononuclear pleocytosis of 19 cells/mm3. Repeated brain MRI (figure 1) showed progressive white matter lesions (hyperintense on fluid-attenuated inversion recovery (FLAIR) and T2-weighted images and hypointense on T1-weighted images) displaying subtle peripheral diffusion restriction. Serum serological tests for Lyme disease, syphilis and HIV were negative. Additional laboratory findings showed a low CD4 count (0.24×109/L) and the angiotensin-converting enzyme (ACE) in serum was minimally increased (54 U/L). CSF cytology and PCR for cytomegalovirus, herpes zoster and herpes simplex virus 1 and 2 were negative. Paraneoplastic antibodies were also negative. Eventually, PCR for John Cunningham virus (JC virus) was positive in the CSF. Finally, a whole-body [18F]fluorodeoxyglucose positron emission tomography (PET)–CT showed symmetric mediastinal and hilar lymphadenopathy with increased tracer uptake, consistent with sarcoidosis.
Figure 1.
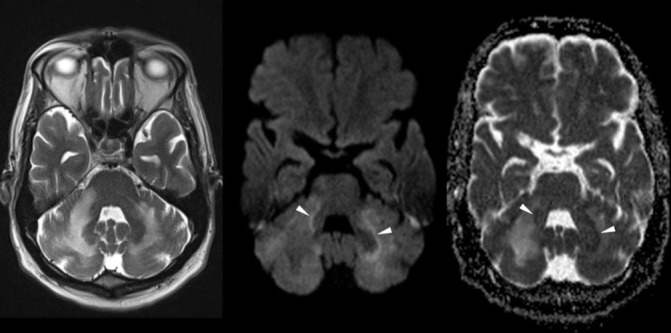
Follow-up MRI of the brain. Transverse T2-weighted image, diffusion-weighted image (DWI) and corresponding apparent diffusion coefficient (ADC) map (left to right). Transverse T2-weighted image of the posterior fossa shows confluent hyperintense white matter changes in both cerebellar hemispheres. On the right more than left side, there is extension through the middle cerebellar peduncle into the brainstem. DWI depicts high signal in the periphery of the white matter lesions left more than right (arrowheads) with corresponding low signal on the ADC map (arrowheads), consistent with restricted diffusion. There was no contrast enhancement (not shown).
Differential diagnosis
Initial differential diagnostic thoughts were among others opportunistic viral infections, acute disseminated encephalomyelitis (ADEM) and neurosarcoidosis. But imaging findings were not fully consistent with both ADEM and neurosarcoidosis.
Finally, the positive PCR for JC virus, combined with clinical and radiological features, made a clear diagnosis: PML.1 Further work-up made an underlying autoimmune disease plausible.
Outcome and follow-up
Our patient deteriorated fast suffering from progressive ataxia of both arms and legs, severe dysarthria, swallowing difficulties, behavioural changes and depression. He declined any further diagnostic work-up; therefore, histopathological evidence of a suspected underlying immune-suppressive disease is not available. Treatment with mirtazapine was started, unfortunately without any measurable clinical improvement. The patient died about 2 months after first presentation. We obtained no obduction.
Discussion
PML is a demyelinating disease and a rare complication of an opportunistic JC virus infection; a polyomavirus that infects >50% of the world’s population.1 Clinical symptoms depend on the location of demyelination of the CNS. Most common locations are the frontal or parieto-occipital regions; only 1 out of 10 patients has brainstem or cerebellar lesions.1 2 However, in patients with HIV/AIDS, cerebellar localisation of PML lesions seems to be less rare: about 34%.3 MRI scanning is an important diagnostic tool to identify PML. FLAIR images have the highest sensitivity showing hyperintense lesions. Lesions are hyperintense on T2 sequences too and hypointense on T1 sequences. Only 15%–40% of cases show contrast enhancement and also diffusion restriction may occur on diffusion-weighted images.1 4 Currently, definite PML can be diagnosed considering the triad of compatible clinical features, compatible imaging findings and positive CSF PCR for JC virus. A brain biopsy is not obligatory for the diagnosis.1
PML is a disease mostly seen in immune-compromised patients. It is traditionally associated with HIV or AIDS, but in the past decades there has been a shift to medication-associated PML with the increasing use of immune-compromising medication. Also, long-standing inflammatory disorders (eg sarcoidosis, systemic lupus erythematosus) seem to be related with developing PML.1 5–7 Using MRI as a screening tool for early detection of PML is suggested in some of these patient groups.8 Current treatment consists of withdrawal of the causative immune-compromising agent, treatment of the underlying disease and supportive care. PML used to be a lethal condition, but nowadays mortality and functional outcome depend more and more on the underlying condition and PML stage at time of diagnosis.7 9 Different small trials suggest cidofovir, acyclovir, cytarabine, chlorpromazine, mefloquine, mirtazapine or interleukin-7 as treatment options.4 10 Some of these seem to give a favourable outcome, but they are not yet proven to cure or end disease progression.4
Our case shows a relatively rare presentation of PML in the posterior fossa structures in an initial supposedly immunocompetent patient. Our hypothesis is, however, that an untreated autoimmune disease has caused reactivation of the JC virus with PML as the presenting symptom. This is supported by the patient’s medical history and current mediastinal lymphadenopathy on PET–CT, low CD4 count and positive results of ENA and ANA in serum. This, combined with increased serum ACE, makes sarcoidosis our probable diagnosis. PML as a first presentation of an inflammatory or autoimmune disorder is also rare, but there are a few other case reports concerning PML as a first presentation of sarcoidosis.5 11–13 We were not able to confirm the suspected diagnosis of sarcoidosis with histopathological findings in this case, which is our limitation.
Our case illustrates that PML needs to be considered as a differential diagnosis even if there is no known actual immune-compromising state. And when there is no obvious cause of PML, it is important to search for an underlying immunological disorder like an untreated autoimmune disease.
Learning points.
Progressive multifocal leukoencephalopathy (PML) can be diagnosed with the triad of compatible clinical features, compatible imaging findings and positive cerebrospinal fluid PCR for John Cunningham virus; a brain biopsy is not necessary.
Although relatively rare, PML can present in the posterior fossa structures.
Consider PML in your differential diagnosis, even when there is no known immune-compromising state.
When PML is diagnosed search for an underlying cause: typical causes ((untreated) HIV or the use of immune-suppressive drugs) or atypical causes (unknown or untreated inflammatory/autoimmune disease).
Footnotes
Contributors: PS: main contributor, manuscript concept and design. PK: contributor of the radiological data and conclusions, revision of the manuscript. BJ: supervisor, critical revision of the manuscript.
Competing interests: None declared.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Berger JR, Aksamit AJ, Clifford DB, et al. . PML diagnostic criteria: consensus statement from the AAN Neuroinfectious disease section. Neurology 2013;80:1430–8. 10.1212/WNL.0b013e31828c2fa1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Patil MA, Redkar NN, Ballikar R, et al. . Progressive multifocal leucoencephalopathy isolated to the posterior fossa. BMJ Case Rep 2013;2013:bcr2012008078 10.1136/bcr-2012-008078 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Berger JR, Pall L, Lanska D, et al. . Progressive multifocal leukoencephalopathy in patients with HIV infection. J Neurovirol 1998;4:59–68. 10.3109/13550289809113482 [DOI] [PubMed] [Google Scholar]
- 4.Sahraian MA, Radue EW, Eshaghi A, et al. . Progressive multifocal leukoencephalopathy: a review of the neuroimaging features and differential diagnosis. Eur J Neurol 2012;19:1060–9. 10.1111/j.1468-1331.2011.03597.x [DOI] [PubMed] [Google Scholar]
- 5.Jamilloux Y, Valeyre D, Lortholary O, et al. . The spectrum of opportunistic diseases complicating sarcoidosis. Autoimmun Rev 2015;14:64–74. 10.1016/j.autrev.2014.10.006 [DOI] [PubMed] [Google Scholar]
- 6.Palazzo E, Yahia SA. Progressive multifocal leukoencephalopathy in autoimmune diseases. Joint Bone Spine 2012;79:351–5. 10.1016/j.jbspin.2011.11.002 [DOI] [PubMed] [Google Scholar]
- 7.Maas RP, Muller-Hansma AH, Esselink RA, et al. . Drug-associated progressive multifocal leukoencephalopathy: a clinical, radiological, and cerebrospinal fluid analysis of 326 cases. J Neurol 2016;263:2004–21. 10.1007/s00415-016-8217-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.McGuigan C, Craner M, Guadagno J, et al. . Stratification and monitoring of natalizumab-associated progressive multifocal leukoencephalopathy risk: recommendations from an expert group. J Neurol Neurosurg Psychiatry 2016;87:117–25. 10.1136/jnnp-2015-311100 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Dong-Si T, Richman S, Wattjes MP, et al. . Outcome and survival of asymptomatic PML in natalizumab-treated MS patients. Ann Clin Transl Neurol 2014;1:755–64. 10.1002/acn3.114 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Alstadhaug KB, Croughs T, Henriksen S, et al. . Treatment of progressive multifocal leukoencephalopathy with interleukin 7. JAMA Neurol 2014;71:1030–5. 10.1001/jamaneurol.2014.825 [DOI] [PubMed] [Google Scholar]
- 11.Davis MJ, Khan A, Royal W. Progressive multifocal leukoencephalopathy as the first manifestation of occult sarcoidosis: case report and review of the literature. Neurologist 2013;19:26–9. 10.1097/NRL.0b013e31827c6c3d [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.De Raedt S, Lacor P, Michotte A, et al. . Progressive multifocal leukoencephalopathy as first manifestation of sarcoidosis. Clin Neurol Neurosurg 2008;110:186–9. 10.1016/j.clineuro.2007.09.012 [DOI] [PubMed] [Google Scholar]
- 13.Hohlfeld SK, Günthard HF, Zeitz J, et al. . Progressive multi-focal leukoencephalopathy as a rare lethal complication in untreated sarcoidosis. BMJ Case Rep 2012;2012:bcr0320114036 10.1136/bcr.03.2011.4036 [DOI] [PMC free article] [PubMed] [Google Scholar]


