Abstract
A 60-year-old Chinese woman presented with intermittent, painless, gross haematuria and subsequently complained of persistent milky urine. The diagnosis of chyluria was confirmed after cystoscopy demonstrated ureteric milky fluid discharge which had elevated levels of triglycerides. The patient did not travel to filarial endemic areas and her serum circulating filarial antigen was negative. Intravenous pyelography with CT of the abdomen did not reveal any masses or obstruction. It was determined that her chyluria was non-parasitic in origin and her symptoms improved with a low fat, high-protein diet. However, her chyluria recurred 1 year later, resulting in hypoalbuminaemia and proteinuria. Her symptoms resolved and her albumin levels normalised with adherence to dietary modifications.
Keywords: tropical medicine (infectious disease), medical management
Background
Chyluria is defined as the passage of chyle in the urine. Chyle is a milky fluid, rich in lymph and chylomicrons. It flows from the intestinal lacteals to the thoracic duct and finally drains into the left subclavian vein. Obstruction of the lymphatic system results in lymphatic dilatation and rupture. This leads to formation of lymphaticourinary fistulas and resultant leakage of chyle into the urinary tract.
Chyluria is most commonly associated with lymphatic filariasis and is rare in non-endemic areas. Failure to recognise this entity can result in unnecessary tests and invasive procedures such as renal biopsy. Existing literature focuses on filarial associated chyluria and there is a paucity of information on the management of chyluria in non-endemic areas. The aim of this paper is to present a case of chyluria in a patient without significant exposure to lymphatic filariasis. Literature review was conducted and an approach to non-parasitic chyluria is proposed to guide physician management in non-endemic areas.
Case presentation
A 60-year-old Chinese woman presented with intermittent, painless, gross haematuria. She did not complain of fever, poor appetite or loss of weight. Significant medical history included chronic hepatitis B which did not require antiviral therapy. The patient had a body mass index (BMI) of 24.6 kg/m2 and her physical examination was unremarkable. Initial serum alanine transaminase and alpha fetoprotein levels were normal. Prior ultrasonography of the liver showed fatty change and there was mild fibrosis on ultrasound elastography.
Microscopic examination of the urine revealed 118 red blood cells/UL and 1+albuminuria. Intravenous pyelography with CT of the abdomen did not reveal any calculus or obstruction. Generalised mural thickening and trabeculation of the urinary bladder on CT was suggestive of chronic cystitis.
Her symptoms progressed and she subsequently complained of persistent milky urine (figure 1). Cystoscopy revealed milky discharge from both ureteric orifices on a background of normal bladder mucosa. A free-floating chylous sac was observed in the bladder (figure 2) and a biopsy was performed. Fibrinous material, red blood cells and leucocytes were noted on histological examination. Urine triglycerides were elevated at 4.11 mmol/L, compared with a serum triglyceride level of 1.09 mmol/L. Urine cytology was negative for malignant cells.
Figure 1.

Photo of milky urine.
Figure 2.
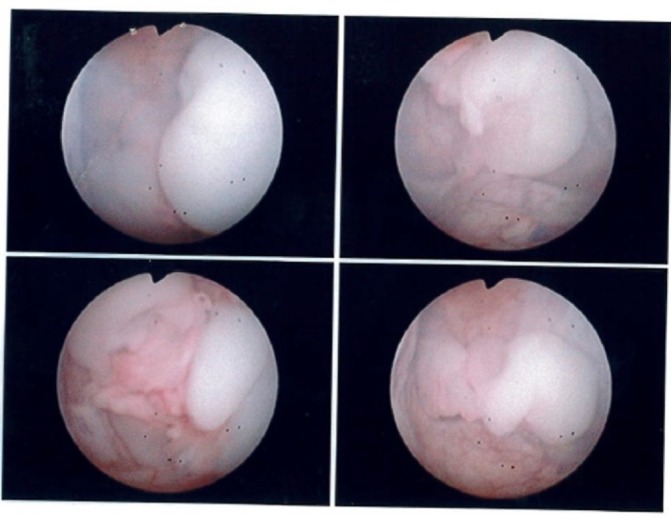
Cystoscopic views showing sac of chylous clot.
Based on the clinical findings of milky urine and elevated urinary triglycerides, the diagnosis of chyluria was made. She was advised to adhere to low fat, high-protein diet.
The patient returned a year after her initial presentation with complaints of bilateral symmetrical lower limb swelling and periorbital oedema. There were no complaints of dyspnoea, decreased effort tolerance or weight loss. She continued to have haematuria or milky urine intermittently.
Physical examination revealed bilateral pitting pedal oedema. Her weight and BMI were stable. There were no crackles on lung auscultation and her jugular venous pressure was not elevated. There were no palpable abdominal masses or lymph nodes. Ascites was absent.
Investigations
Laboratory investigations showed mild leucopaenia (3.91, normal range: 4.0–10.0×10^9/L). There was no eosinophilia. Renal function was normal. Serum albumin levels were on a downward trend over the course of the year; from 32 g/L to 24 g/L (normal range: 40–51 g/L). Alanine and aspartate transaminase were within normal range.
There was 10 red blood cells/UL on urine full examination and microscopy. There were no cast cells. Urine phase contrast showed predominantly isomorphic red blood cells. Twenty-four-hour urine collection revealed proteinuria of 1.25 g and urine triglycerides were elevated at 7.19 mmol/L. Serum and urine electrophoresis were negative for monoclonal gammopathy. Autoimmune screening which consisted of antinuclear, antidouble stranded DNA, antineutrophil cytoplasmic and antiglomerular basement membrane antibodies was negative.
Transthoracic echocardiogram revealed a normal ejection fraction and diastolic function. Left atrial size was normal. Ultrasonography of the abdomen showed slightly coarse liver parenchyma. The kidneys were normal, with no hydronephrosis, masses or calculi seen. Doppler ultrasound was negative for renal vein thrombosis.
Treatment
It was ascertained that her symptoms of lower limb swelling and periorbital oedema were secondary to her persistent chyluria, which resulted in significant proteinuria and hypoalbuminaemia. The patient’s lower limb oedema resolved with diuretics. There was also a gradual decrease in the frequency of milky urine with dietary modifications.
The patient is a resident of Singapore and has never travelled to or lived in a country endemic for filarial disease. Lymphatic filariasis is not endemic to Singapore. She grew up in rural farming area as a child and has been staying in an urban area for the past 40 years. Of note, her serology for circulating filarial antigen was negative. On discharge, dietary modifications and restrictions were reinforced to the patient.
Outcome and follow-up
The patient was reviewed 1 month after discharge. There was no recurrence of pedal oedema or chyluria. Her serum albumin had improved to 38 g/L. She continues to attend regular follow-up appointments at our institution and will continue to be monitored for recurrence of chyluria.
Discussion
Chyluria can be parasitic or non-parasitic in origin (table 1). Majority of parasitic causes are due to lymphatic filariasis, with the nematode Wuchereria bancrofti contributing to more than 90% of all cases. In Asia, it can also be caused by Brugia malayi and Brugia timori. Lymphatic filariasis is mainly found in the tropics and subtropics of Asia, Africa, the Western Pacific and parts of the Caribbean and South America. An estimated 120 million people in 73 countries are affected.1–6
Table 1.
Causes of chyluria
| Parasitic causes | Non-parasitic causes |
|
|
Non-parasitic causes are rare and are mainly described in case reports. The causes include that of granulomatous infection,7 pregnancy,8 9 massive mesenteric adenitis,10 glomerular disease,11–13 aortic aneurysm,14 15 neoplasms16–20 and malformations of the lymphatic system.21–27 It has also been reported to occur following trauma28 or surgical procedures like partial nephrectomy,29 30 hemicolectomy,31 cardiac catheterisation,32 oesophagectomy,33 posterior spinal fusion34 and radiofrequency ablation of renal cell carcinoma.35 36 No apparent causes are found in some cases.37 38
Patients with chyluria present with cloudy or milky urine, which resolves with fasting and can be aggravated by a meal rich in fats. Chyluria can be asymptomatic, while symptomatic patients may suffer from gross haematuria, renal colic or obstructive uropathy due to chylous clots.39 Genital and lower limb swelling may develop as a result of lymphatic obstruction.5 Persistent chyluria leads to excessive loss of lipids and protein, resulting in malnutrition, weight loss, anaemia, hypoalbuminaemia and oedema. This can be mistaken for nephrotic syndrome.40 Hypercoagulopathy secondary to severe proteinuria has also been described.41
Investigation of chyluria includes confirmation of the diagnosis, ascertaining the aetiology and localising the site of chyle leakage.42–46
The diagnosis of chyluria is confirmed via urine examination. Collecting a urine specimen approximately 4 hours after a fatty meal will increase the sensitivity.47 Gross examination of the urine will reveal milky urine which frequently contains gelatinous clots of blood and fibrin. On standing, the urine will separate into three layers; a top layer of chylomicrons, a middle layer of protein and a bottom layer containing fibrin clots. The presence of urinary triglycerides is 100% sensitive and specific in the diagnosis of chyluria.45 46 Chyluria can still be diagnosed if triglycerides are present in clear urine. Other confirmatory tests include mixing a cloudy urine sample with equal amounts of ether, which clears the urine. Oral ingestion of fat labelled with Sudan III will cause orange pink discolouration of urine.46
Other findings include haematuria and proteinuria. Urine phase contrast will reveal predominantly isomorphic red blood cells and lymphocyturia. Twenty-four hours urine protein collection often reveal nephrotic range proteinuria. Spot urine protein can be normal as chyluria may be intermittent, appearing only after a fatty meal. The clinical features and absence of fatty cast cells, lipid laden oval bodies differentiate chyluria from nephrotic syndrome (table 2).47
Table 2.
Main differences between nephrotic syndrome and chyluria
| Nephrotic syndrome | Chyluria | |
| Clinical features | Gradual onset and persistent Pitting oedema |
Episodic, aggravated by fatty meal Haematuria Cloudy, milky urine Clots in urine, with resultant renal colic Pitting oedema in malnourished cases |
| Investigations | Hypoalbuminaemia, hypercholesterolaemia Dysmorphic red blood cell in urine if present Fatty cast cells with oval fat bodies |
Hypoalbuminaemia in malnourished cases Milky urine with clots, clears with ether Isomorphic red blood cell Lymphocytes in urine No cast cells Chylomicrons, triglycerides in urine |
The next step in management is to ascertain the aetiology and determine the site of chyle leakage. Lymphatic filariasis is the most common cause of chyluria and should be a top differential. History of travel or residence in an endemic area should be sought. Detection of microfilariae on peripheral blood smears taken at night or positive serum circulating filarial antigen will diagnose Wuchereira bancrofti infections. Serum filarial antigen has higher sensitivity when compared with blood smears and can be used on blood samples taken in the day. Patients48 49 with lymphatic filariasis should be treated with a course of diethylcarbamazine. Combination therapy with doxycycline, albendazole or ivermectin have also been used.2 4 46 Two or three courses of antihelminthics may be required.
Spontaneous resolution of chyluria occurs in 50% to 70% of patients after dietary modification.50–52 This involves removing long-chain triglycerides from the diet and supplementing the diet with protein and medium chain triglycerides. It works by preventing chylomicron production by enterocytes. Medium chain triglycerides are directly absorbed into the portal circulation, bypassing the lymphatics. In view of this, Singh et al43 and Al-Anazi53 advocate for a conservative approach and propose advanced or invasive investigations in non-responders.43 53Non-responders tend to have multiple episodes of haematuria with passage of blood clots, received multiple course of antihelminthics and heavier urinary cholesterol losses.51
Lymphatic filariasis in individuals without significant exposure to the pathogen is unlikely and can be attributed to the low transmissibility and life cycle requirements of Wuchereria and Brugia.54 Non-parasitic chyluria may be caused by a myriad of diseases and serious ailments must be excluded. Significant weight loss may suggest an underlying malignancy. Prolonged fever and respiratory complaints will require investigations to exclude tuberculosis. If clinical features raise the suspicion of tuberculosis, chest radiograph and appropriate microbiological specimens should be taken for staining for acid fast bacilli and culture. The yield of urinary testing for genitourinary mycobacterium is poor, which may require repeated testing if index of suspicion remains high.7 55 56 History of recent surgery should also be elicited. In most cases, imaging of the abdomen to look for causes of lymphatic obstructions will be necessary. If urinalysis is suggestive of glomerulonephritis, further investigations for autoimmune diseases should be considered.
Treatment for non-parasitic chyluria will be dependent on the underlying cause. For idiopathic, non-parasitic cases of chyluria, bed rest, abdominal binders and dietary modifications will help alleviate the symptoms.37 38 57 Somatostatin analogues like octreotide had been used successfully in patients with post-traumatic and idiopathic chyluria.58–61 Somatostatin analogues reduce splanchnic blood flow, slowing gastrointestinal transit time and inhibiting absorption of nutrients. This reduces lymphatic flow and subsequent chyle leakage. Similarly, ezetimibe which inhibits dietary and biliary cholesterol absorption has been used successfully.62 The use of the angiotensin-converting enzyme inhibitor enalapril to treat chyluria has also been described.63
If chyluria is recurrent or associated with severe malnutrition, advanced imaging and endoscopy should be used to localise the site of chyle leakage. This will provide important information to guide subsequent intervention. Cystoscopy can help in determining the side involved. Among the imaging modalities used, lymphangiography is considered to be the gold standard. It can demonstrate the site, calibre and number of lymphaticourinary fistulas. It can also be therapeutic as the sclerosing effect of contrast on lymphatics can result in the closure of fistulas. However, it is invasive, time consuming, technically demanding and rarely used nowadays.3 46 Alternative modalities include intravenous urography, retrograde pyelography, lymphoscintigraphy and MR pyelography. Lymphoscintigraphy allows functional assessment of lymphatic transport and depiction of regional lymph nodes and has been shown to be able to detect abnormal lymphatic drainage in chyluria. It is fast, non-invasive and has no known side effects.64 65 Lymphoscintigraphy has also been combined with single-photon emission CT/CT for improved anatomical correlation.66 MR retrograde pyelography avoids radiation exposure and the use of ionic contrast. It provides detailed evaluation of abdominal anatomy, which is important in non-filarial chyluria.67 The modality to use will depend on the availability, technical expertise and the depth of anatomical correlation required.
Various interventions have been described in treating refractory chyluria. Sclerotherapy by endoscopic instillation of sclerosants into the renal pelvis has been shown to be effective. Sclerosants used include 0.1% to 3% silver nitrate, 0.2% povidone iodine and 50% dextrose.68 69 While sclerotherapy is generally considered to be safe, serious complications have been described. Acute necrotising ureteritis with obstructive uropathy, renal artery pseudoaneurysm formation, arterial haemorrhage, acute renal and hepatic failure have been reported after instillation of silver nitrate into the renal pelvis.70–77
If renal pelvic instillation sclerotherapy fails to provide relief to symptoms, surgery can then be considered. Various surgical techniques have been described, of which surgical or retroperitoneoscopic renal pedicle lymphatic disconnection is the treatment of choice.4 43
In my patient, her chyluria resolved with dietary modifications. While she did not report any significant exposure to lymphatic filariasis, surrounding countries in Singapore are known to be endemic. However, testing for circulating filarial antigens was negative and her chyluria was deemed to be non-parasitic in nature. Of note, intravenous pyelography with CT of the abdomen did not reveal any abdominal masses or obstructions. She did not display any symptoms that were suggestive of tuberculosis. As she responded to conservative therapy, with no suggestion of any serious pathology, I plan to monitor her for recurrence. Further investigations such as lymphoscintigraphy or MRI will be considered if there is recurrence or development of symptoms that point to a cause for chyluria.
Chyluria is a rarely encountered condition in countries not endemic for lymphatic filariasis. Failure to recognise this entity can result in unnecessary and invasive investigations. Chyluria responds well to dietary modifications. However, non-parasitic chyluria may portend a serious underlying condition and further workup is thus recommended.
Learning points.
Chyluria is a rare condition and recognition is important to avoid unnecessary investigations and interventions.
Though the symptoms are alarming, the overall prognosis is good with conservative therapy.
Detailed history should be taken to ascertain exposure to filarial disease.
Non-filarial chyluria will need further workup to exclude other serious causes like malignancies and granulomatous infections.
Invasive therapy can be considered if chyluria results in severe malnutrition or fails to respond to dietary modifications.
Footnotes
Contributors: I am the primary physician of the patient, and is continuing follow-up for the patient. I did the literature search, review and wrote the article in its entirety.
Competing interests: None declared.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.CDC. Prevention C-C for DC and. CDC-lymphatic filariasis-epidemiology & risk Factors. http://www.cdc.gov/parasites/lymphaticfilariasis/epi.html (accessed 18 Apr 2017).
- 2.Abeygunasekera AM, Sutharshan K, Balagobi B. New developments in chyluria after global programs to eliminate lymphatic filariasis. Int J Urol 2017;24:582–8. 10.1111/iju.13378 [DOI] [PubMed] [Google Scholar]
- 3.Saha M, Ray S, Goswami M, et al. An occult filarial infection presenting as chyluria with proteinuria: a case report and review of literature. BMJ Case Rep 2012;2012:bcr0120125635 10.1136/bcr.01.2012.5635 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sinha RK, Ranjan N, Singh N, et al. Chyluria: a scourge of our region. BMJ Case Rep 2015;2015:bcr2014209188 10.1136/bcr-2014-209188 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Tada I. Pathogenesis and treatment of chronic symptoms with emphasis on chyluria and elephantiasis. Trop Med Health 2011;39:47–50. 10.2149/tmh.39-1-suppl_2-47 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hagiya H, Otsuka F. Refractory chyluria due to filariasis. Infection 2015;43:785–6. 10.1007/s15010-015-0804-8 [DOI] [PubMed] [Google Scholar]
- 7.Wilson RS, White RJ. Lymph node tuberculosis presenting as chyluria. Thorax 1976;31:617–20. 10.1136/thx.31.5.617 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mahmood K, Ahmad A, Kumar K, et al. Chyluria in pregnancy-a decade of experience in a single tertiary care hospital. Nephrourol Mon 2015;7 10.5812/numonthly.26309 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Onyeije CI, Sherer DM, Trambert J. Nonfilarial chyluria during pregnancy. Obstet Gynecol 1997;90:699–700. 10.1016/S0029-7844(97)00243-3 [DOI] [PubMed] [Google Scholar]
- 10.Cohen PG, Glenn JF, Franco NM, et al. Nontropical chyluria secondary to massive mesenteric adenitis. Case report with metabolic and immunologic studies. Am J Med 1984;77:583–8. [DOI] [PubMed] [Google Scholar]
- 11.El-Reshaid KA, Madda JP, Sherif MF. Chyluria associated with renal vasculitis. Saudi J Kidney Dis Transpl 1998;9:152. [PubMed] [Google Scholar]
- 12.Lewsuwan S, Kanjanabuch T, Avihingsanon Y, et al. A rare case of chylous ascites and chyluria in an adult nephrotic syndrome with focal segmental glomerulosclerosis. J Med Assoc Thai 2006;89 Suppl 2:S253–6. [PubMed] [Google Scholar]
- 13.Knier B, Büschges-Seraphin B, Hilgers KF, et al. From red to white urine: a patient’s nightmare with a rather benign outcome. BMC Nephrol 2012;13:7 10.1186/1471-2369-13-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Garrido P, Arcas R, Bobadilla JF, et al. Thoracic aneurysm as a cause of chyluria: resolution by surgical treatment. Ann Thorac Surg 1995;60:687–9. 10.1016/0003-4975(95)00333-G [DOI] [PubMed] [Google Scholar]
- 15.Salinas Sánchez AS, Hernández Millán I, Beltrán Pedrero JM, et al. [Chyluria of non-parasitic origin. Presentation of a case and review of the literature]. Actas Urol Esp 1992;16:247–53. [PubMed] [Google Scholar]
- 16.Morice AH, Wood JR. Chyluria associated with bronchial carcinoma. Postgrad Med J 1981;57:193–5. 10.1136/pgmj.57.665.193 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.van Apeldoorn MJ, Rustemeijer C, Voerman BJ, et al. Mesothelioma of the tunica vaginalis complicated by chyluria. J Clin Oncol 2006;24:5329–30. 10.1200/JCO.2006.07.6596 [DOI] [PubMed] [Google Scholar]
- 18.McNeil JC, Corbett ST, Kuruvilla S, et al. Metanephric adenoma in a five-year-old boy presenting with chyluria: case report and review of literature. Urology 2008;72:545–7. 10.1016/j.urology.2008.04.010 [DOI] [PubMed] [Google Scholar]
- 19.Rittenberg GM, Schabel SI, Allen R, et al. Nontropical chyluria associated with pelvic lipomatosis. South Med J 1980;73:1385–6. 10.1097/00007611-198010000-00028 [DOI] [PubMed] [Google Scholar]
- 20.Cluskey SA, Myatt A, Ferro MA. The treatment of chyluria secondary to advanced carcinoma of the prostate. Prostate Cancer Prostatic Dis 2008;11:102–5. 10.1038/sj.pcan.4500994 [DOI] [PubMed] [Google Scholar]
- 21.Liu DY, Wang HF, Xia WM, et al. Right-crossed, fused renal ectopia L-shaped kidney type with urinary chyluria. Urol Int 2015;95:243–5. 10.1159/000382132 [DOI] [PubMed] [Google Scholar]
- 22.Singh K, Kumar M, Jhanwar A, et al. Crossed fused renal ectopia with chyluria: a rare presentation. BMJ Case Rep 2016;2016:bcr2015213050 10.1136/bcr-2015-213050 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kekre NS, Arun N, Date A. Retroperitoneal cystic lymphangioma causing intractable chyluria. Br J Urol 1998;81:327–8. [DOI] [PubMed] [Google Scholar]
- 24.Kano K, Arisaka O. Chyluria due to retroperitoneal lymphangioma producing nephrotic syndrome. J Pediatr 2003;143:685 10.1067/S0022-3476(03)00288-9 [DOI] [PubMed] [Google Scholar]
- 25.Eisner BH, Tanrikut C, Dahl DM. Chyluria secondary to lymphorenal fistula. Kidney Int 2009;76:126 10.1038/ki.2009.64 [DOI] [PubMed] [Google Scholar]
- 26.van Olden RW, van Dam FE, Kho S, et al. Chyluria caused by congenital retroperitoneal lymphangiectasis. Ned Tijdschr Geneeskd 1989;133:1701–3. [PubMed] [Google Scholar]
- 27.Taylor TV, Strachan AW, Isherwood I, et al. Non-parasitic chyluria (presenting with urinary retention). Br J Urol 1975;47:419–23. 10.1111/j.1464-410X.1975.tb03999.x [DOI] [PubMed] [Google Scholar]
- 28.Rycyna KJ, Casella D, D’Agostino L. Blunt force trauma as a rare mechanism for chyluria. Can J Urol 2016;23:8318–20. [PubMed] [Google Scholar]
- 29.Komeya M, Sahoda T, Sugiura S, et al. Chyluria after partial nephrectomy: a rare but considerable complication. Int J Urol 2013;20:242–5. 10.1111/j.1442-2042.2012.03139.x [DOI] [PubMed] [Google Scholar]
- 30.Tuck J, Pearce I, Pantelides M. Chyluria after radical nephrectomy treated with N-butyl-2-cyanoacrylate. J Urol 2000;164:778–9. 10.1016/S0022-5347(05)67305-3 [DOI] [PubMed] [Google Scholar]
- 31.Hoven N, Fister M, Niendorf E. Lipiduria presenting following right hemicolectomy: A case presentation and brief review of the literature. Radiol Case Rep 2015;10:49–52. 10.1016/j.radcr.2015.06.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Chen HS, Yen TS, Lu YS, et al. Transient ’milky urine' after cardiac catheterization: another unreported cause of non-parasitic chyluria. Nephron 1996;72:367–8. 10.1159/000188892 [DOI] [PubMed] [Google Scholar]
- 33.Takeno A, Tamura S, Miki H, et al. Chyluria after ligation of the thoracic duct: a rare complication after thoracoscopic-assisted esophagectomy for esophageal cancer. Surg Today 2014;44:757–60. 10.1007/s00595-012-0443-y [DOI] [PubMed] [Google Scholar]
- 34.Weening AA, Schurink B, Ruurda JP, et al. Chyluria and chylothorax after posterior selective fusion for adolescent idiopathic scoliosis. Eur Spine J 2017. 10.1007/s00586-017-5066-y [DOI] [PubMed] [Google Scholar]
- 35.Kaur H, Matin SF, Javadi S, et al. Chyluria after radiofrequency ablation of renal tumors. J Vasc Interv Radiol 2011;22:924–7. 10.1016/j.jvir.2011.02.014 [DOI] [PubMed] [Google Scholar]
- 36.Wah TM. An unusual cause of chyluria after radiofrequency ablation of a renal cell carcinoma: a case report. J Med Case Rep 2011;5:307 10.1186/1752-1947-5-307 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Mendu DR, Sternlicht H, Ramanathan LV, et al. Two cases of spontaneous remission of non-parasitic chyluria. Clin Biochem 2017;50:886–8. 10.1016/j.clinbiochem.2017.05.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Neuwirt H, Eller P, Tiefenthaler M, et al. A rare case of milky urine. Wien Klin Wochenschr 2010;122:596–600. 10.1007/s00508-010-1465-3 [DOI] [PubMed] [Google Scholar]
- 39.Nag VL, Sen M, Dash NR, et al. Hematuria without chyluria: It could still be due to filarial etiology. Trop Parasitol 2016;6:151–4. 10.4103/2229-5070.190834 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Kaul A, Bhadhuria D, Bhat S, et al. Chyluria: a mimicker of nephrotic syndrome. Ann Saudi Med 2012;32:593–5. 10.5144/0256-4947.2012.593 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Golestaneh L, Karam S, Lawrence J, et al. Hypercoagulability in a patient with chronic chyluria, proteinuria and hypoalbuminaemia. Nephrol Dial Transplant 2009;24:3240–3. 10.1093/ndt/gfp283 [DOI] [PubMed] [Google Scholar]
- 42.Sunder S, Jayaraman R, Mahapatra HS, et al. Analysis of case series of milky urine: a single center and departmental clinical experience with emphasis on management perspectives: a prospective observational study. Urol Ann 2014;6:340–5. 10.4103/0974-7796.141002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Singh I, Dargan P, Sharma N. Chyluria-a clinical and diagnostic stepladder algorithm with review of literature. Indian J Urol 2004;20:79. [Google Scholar]
- 44.Graziani G, Cucchiari D, Verdesca S, et al. Chyluria associated with nephrotic-range proteinuria: pathophysiology, clinical picture and therapeutic options. Nephron Clin Pract 2011;119:c248–c254. 10.1159/000329154 [DOI] [PubMed] [Google Scholar]
- 45.Dalela D. Issues in etiology and diagnosis making of chyluria. Indian Journal of Urology 2005;21:18 10.4103/0970-1591.19545 [DOI] [Google Scholar]
- 46.Sharma S, Hemal AK. Chyluria-An Overview. Int J Nephrol Urol 2009;1:14–26. [Google Scholar]
- 47.Cheng JT, Mohan S, Nasr SH, et al. Chyluria presenting as milky urine and nephrotic-range proteinuria. Kidney Int 2006;70:1518–22. 10.1038/sj.ki.5001703 [DOI] [PubMed] [Google Scholar]
- 48.Weil GJ, Jain DC, Santhanam S, et al. A monoclonal antibody-based enzyme immunoassay for detecting parasite antigenemia in bancroftian filariasis. J Infect Dis 1987;156:350–5. 10.1093/infdis/156.2.350 [DOI] [PubMed] [Google Scholar]
- 49.Weil GJ, Curtis KC, Fakoli L, et al. Laboratory and field evaluation of a new rapid test for detecting Wuchereria bancrofti antigen in human blood. Am J Trop Med Hyg 2013;89:11–15. 10.4269/ajtmh.13-0089 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Ohyama C, Saita H, Miyasato N. Spontaneous remission of chyluria. J Urol 1979;121:316–7. 10.1016/S0022-5347(17)56767-1 [DOI] [PubMed] [Google Scholar]
- 51.Goyal NK, Goel A, Sankhwar S, et al. Factors affecting response to medical management in patients of filarial chyluria: A prospective study. Indian J Urol 2014;30:23–7. 10.4103/0970-1591.124201 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Yu HH, Ngan H, Leong CH. Chyluria-a 10 year follow-up. Br J Urol 1978;50:126–33. [DOI] [PubMed] [Google Scholar]
- 53.Al-Anazi AR. Membranous glomerulonephritis in a patient presenting with chyluria, probably due to filariasis: how far should we investigate? Saudi J Kidney Dis Transpl 1999;10:167. [PubMed] [Google Scholar]
- 54.Jones RT. Non-endemic cases of lymphatic filariasis. Trop Med Int Health 2014;19:1377–83. 10.1111/tmi.12376 [DOI] [PubMed] [Google Scholar]
- 55.Merchant S, Bharati A, Merchant N. Tuberculosis of the genitourinary system-Urinary tract tuberculosis: Renal tuberculosis-Part I. Indian J Radiol Imaging 2013;23:46–63. 10.4103/0971-3026.113615 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Merchant S, Bharati A, Merchant N. Tuberculosis of the genitourinary system-Urinary tract tuberculosis: Renal tuberculosis-Part II. Indian J Radiol Imaging 2013;23:64–77. 10.4103/0971-3026.113617 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Triffoni-Melo AT, Diez-Garcia RW, Barros Silva GE, et al. Good response of low-fat/high-protein diet in a patient with chyluria. Ren Fail 2014;36:453–6. 10.3109/0886022X.2013.865485 [DOI] [PubMed] [Google Scholar]
- 58.Giordano M, Crillo D, Baron I, et al. Treatment of post-traumatic chyluria with subcutaneous octreotide administration. Nephrol Dial Transplant 1996;11:365–7. 10.1093/oxfordjournals.ndt.a027271 [DOI] [PubMed] [Google Scholar]
- 59.Cheung Y, Leung MP, Yip M. Octreotide for treatment of postoperative chylothorax. J Pediatr 2001;139:157–9. 10.1067/mpd.2001.115572 [DOI] [PubMed] [Google Scholar]
- 60.Campieri C, Raimondi C, Dalmastri V, et al. Posttraumatic chyluria due to lymphorenal fistula regressed after somatostatin therapy. Nephron 1996;72:705–7. 10.1159/000188968 [DOI] [PubMed] [Google Scholar]
- 61.Yashi M, Ishikawa S, Nishizawa S, et al. Pharmacotherapy for chyluria by subcutaneous injection with a somatostatin analogue. BJU Int 2002;90:e12–e13. 10.1111/j.1464-410X.2002.02876.x [DOI] [Google Scholar]
- 62.Tanaka S, Tsuruya K, Tsuchimoto A, et al. Successful treatment of massive proteinuria and severe chyluria by inhibition of cholesterol absorption with ezetimibe in a patient with filariasis. Clin Kidney J 2012;5:449–52. 10.1093/ckj/sfs110 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Saleh AE. Angiotensin-converting-enzyme inhibitors and chyluria. Ann Intern Med 1993;119:1223–4. 10.7326/0003-4819-119-12-199312150-00018 [DOI] [PubMed] [Google Scholar]
- 64.Pui MH, Yueh TC. Lymphoscintigraphy in chyluria, chyloperitoneum and chylothorax. J Nucl Med 1998;39:1292–6. [PubMed] [Google Scholar]
- 65.Sun T, Hu F, Cui S, et al. Localization diagnosis of chyluria by radionuclide lymphoscintigraphy. Zhonghua Yi Xue Za Zhi 2002;82:247–8. [PubMed] [Google Scholar]
- 66.Suh M, Cheon GJ, Seo HJ, et al. Usefulness of Additional SPECT/CT Identifying Lymphatico-renal Shunt in a Patient with Chyluria. Nucl Med Mol Imaging 2015;49:61–4. 10.1007/s13139-014-0300-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Goel A, Goyal NK, Parihar A, et al. Magnetic resonance-retrograde pyelography: A novel technique for evaluation of chyluria. Indian J Urol 2014;30:115–6. 10.4103/0970-1591.124221 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Guttilla A, Beltrami P, Bettin L, et al. Non-parasitic chyluria: our experience with sclerotherapy with solution of povidone-lodine and destrose and a review of the literature. Urol Case Rep 2016;8:28–30. 10.1016/j.eucr.2016.05.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Dalela D, Rastogi M, Goel A, et al. Silver nitrate sclerotherapy for ’clinically significant' chyluria: a prospective evaluation of duration of therapy. Urol Int 2004;72:335–40. 10.1159/000077689 [DOI] [PubMed] [Google Scholar]
- 70.Dash SC, Bhargav Y, Saxena S, et al. Acute renal failure and renal papillary necrosis following instillation of silver nitrate for treatment of chyluria. Nephrol Dial Transplant 1996;11:1841–2. 10.1093/ndt/11.9.1841 [DOI] [PubMed] [Google Scholar]
- 71.Su CM, Lee YC, Wu WJ, et al. Acute necrotizing ureteritis with obstructive uropathy following instillation of silver nitrate in chyluria: a case report. Kaohsiung J Med Sci 2004;20:512–5. 10.1016/S1607-551X(09)70251-7 [DOI] [PubMed] [Google Scholar]
- 72.Kulkarni AA, Pathak MS, Sirsat RA. Fatal renal and hepatic failure following silver nitrate instillation for treatment of chyluria. Nephrol Dial Transplant 2005;20:1276–7. 10.1093/ndt/gfh790 [DOI] [PubMed] [Google Scholar]
- 73.Mandhani A, Kapoor R, Gupta RK, et al. Can silver nitrate instillation for the treatment of chyluria be fatal? Br J Urol 1998;82:926–7. 10.1046/j.1464-410X.1998.00839.x [DOI] [PubMed] [Google Scholar]
- 74.Garg M, Dalela D, Goel A. Devastating complication of silver nitrate instillation for the treatment of chyluria. BMJ Case Rep 2013;2013:bcr2013201270 10.1136/bcr-2013-201270 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Dhabalia JV, Nelivigi GG, Suryavanshi M, et al. An unusual complication of silver nitrate therapy for chyluria. Indian J Urol 2007;23:203–4. 10.4103/0970-1591.32078 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Srivastava DN, Yadav S, Hemal AK, et al. Arterial haemorrhage following instillation of silver nitrate in chyluria: treatment by coil embolization. Australas Radiol 1998;42:234–5. 10.1111/j.1440-1673.1998.tb00502.x [DOI] [PubMed] [Google Scholar]
- 77.Gulati MS, Sharma R, Kapoor A, et al. Pelvi-calyceal cast formation following silver nitrate treatment for chyluria. Australas Radiol 1999;43:102–3. 10.1046/j.1440-1673.1999.00604.x [DOI] [PubMed] [Google Scholar]


