Abstract
The differential diagnosis of exercise-induced lower leg pain in young individuals is extensive and includes entities such as chronic exertional compartment syndrome, popliteal arterial entrapment syndrome, cystic adventitial disease, medial tibial stress syndrome and tibial stress fractures. Peripheral nerve-related lower leg pain syndromes are unusual. We present a 41-year-old woman who was diagnosed with an ancient schwannoma of the right common peroneal nerve (CPN) as a rare cause of lower leg pain. This case report provides simple diagnostic bedside tools that may be used to diagnose CPN abnormalities. Altered lateral lower leg skin sensation was found using a simple cotton swab, whereas a nodule was palpated at the fibular head. A positive Tinel sign indicated CPN dysfunction. MRI confirmed the diagnosis. Surgical resection is simple and curative.
Keywords: pain; neurology; peripheral nerve disease; Surgery, sports and exercise medicine
Background
The differential diagnosis of exercise-induced lower leg pain in young individuals includes chronic exertional compartment syndrome (CECS), popliteal arterial entrapment syndrome (PAES), cystic adventitial disease (CAD), medial tibial stress syndrome (MTSS) and tibial stress fractures.1–3 However, lower leg nerve-related syndromes are rare. A young woman was diagnosed with an ancient schwannoma of the common peroneal nerve (CPN) as an uncommon cause of lower leg pain. Aim of this report is to discuss simple bedside tools for an early diagnosis and to report outcome following surgery.
Case presentation
A 41-year-old woman presented with pain of the lateral aspect of the right knee. Symptoms had started 8 years earlier during pregnancy and were progressive. The pain radiated towards dorsal portions of the foot and the big toe and was provoked by touching the lateral aspect of her knee but also while crouching and sitting. In addition, electrical shocks and unpleasant feelings were constantly experienced in her right foot. Doing sports activities such as running was virtually impossible because of these debilitating symptoms.
One year after the start of first symptoms, the patient was referred to the neurologist who considered an entrapment of the CPN. He referred the patient to a musculoskeletal doctor for mobilisation and manipulation of the proximal and distal fibula. The mobilisation was conducted several times over a 3-year period but provided only temporary pain relieve with a 10 to 4 decrease on an numerical rating scale (NRS).4 The symptoms kept recurring and became more intense over the years. Eventually, an ultrasound of the swelling on the right side of the knee was performed which suggested a cyst of the common peroneal nerve (figure 1). As symptoms were greatly interfering with daily functioning by then, she was presented to the department of surgery in our hospital.
Figure 1.
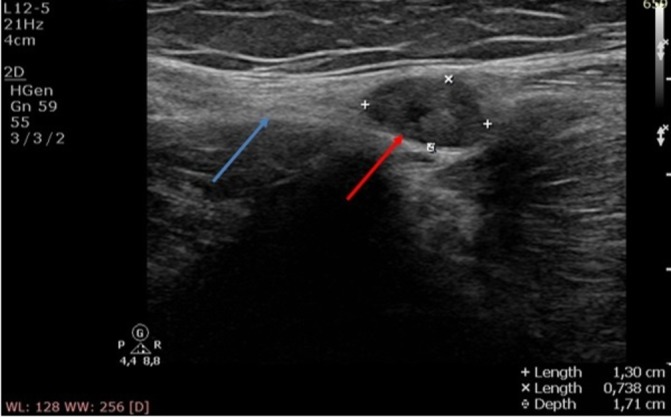
Ultrasound of the common peroneal nerve (blue arrow) demonstrating a 1.3 cm×0.74 cm echodense swelling behind the fibular head (red arrow).
On examination, a 1–2 cm swelling was palpated just behind the right fibular head. Finger tapping of the swelling elicited pain that radiated towards the dorsum of the foot (positive Tinel sign). Skin sensation of the anterolateral side of the right lower leg and dorsum of the foot (area of distribution of the common peroneal nerve) were abnormal compared with the left leg and foot, as demonstrated using a cotton swab. Lower leg and foot motor functions were normal.
Investigations
An MRI suggested the presence of a schwannoma of the CPN (figure 2).
Figure 2.
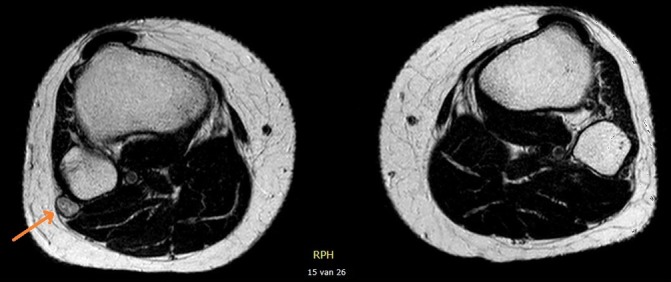
Transversal T2-weighted MRI slide of both lower legs. The right leg shows a lesion of the common peroneal nerve at the level of the fibular head suggesting a schwannoma.
Differential diagnosis
The differential diagnosis of lower leg pain in young sportive individuals is extensive. Different groups of entities must be considered. A CECS is characterised by exercise-induced pain that is usually relieved during rest. The diagnostic gold standard is a dynamic intracompartmental muscle pressure measurement.5 MTSS is a clinical diagnosis as palpation along distal portions of the inner tibial bone is painful.6 In other patients, constant lower leg pain may be due to a stress fracture that is confirmed by an X-ray, bone scan or a CT scan.2 A PAES is diagnosed by loss of distal arterial pulsations at extreme plantar or dorsiflexion whereas ultrasound/Doppler analysis may determine the location of arterial entrapment.1 CAD typically presents with intermittent claudication and is diagnosed by angiography, ultrasound, CT scan or MRI.3 CPN entrapment can be caused by different aetiologies, for instance fibular head malformation, soft tissue tumours or anatomical variations of the biceps femoris muscle. It is diagnosed by a positive Tinel, altered skin sensation and imaging of the lower leg.
Treatment
The patient was informed regarding the potential diagnosis, surgical options and possible complications and consented to a surgical exploration. Once the swelling was identified by palpation, it was exposed via a 6 cm longitudinal incision along the lateral aspect of the knee joint. The nerve’s protective layer termed the perineurium was opened longitudinally followed by enucleation of the schwannoma under direct vision (figure 3A,B). Loupes or other magnification are not required. It must be appreciated that the swelling is surrounded by nerve fascicles but not firmly attached to them.
Figure 3.
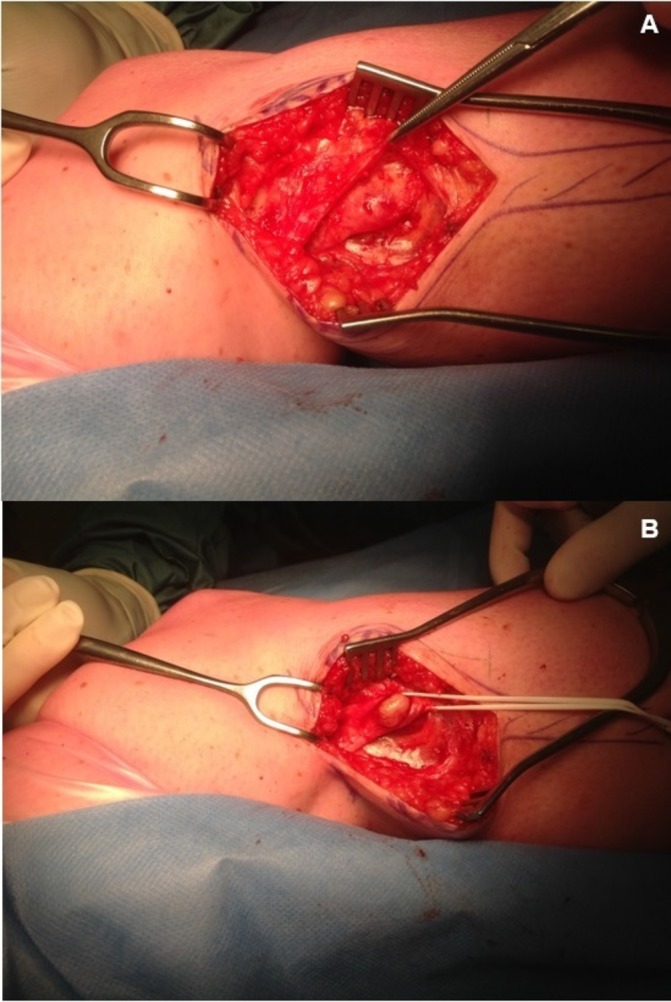
Lateral aspect of right lower leg. (A) The overlying fascia is incised. (B) After incision of the nerve’s perineurium, a 2×1 cm swelling was removed.
Outcome and follow-up
Pathological examination revealed an ancient schwannoma. Immediately postoperatively, the patient was completely free of pain. Two years later, she is unrestricted regarding all movement and sport activities.
Discussion
A schwannoma (or neurilemmoma) is a benign nerve sheath neoplasm originating from the Schwann cells in peripheral nerves. Ancient schwannomas are longstanding neurilemmomas showing degenerative changes.7 This abnormality is preferentially located intracranially, especially at the vestibular nerve. In contrast, extracranial schwannomas are most frequently found in the head and neck area (45%) or at lower extremities flexor sites (13.5%), upper extremities (19%) and trunk (8.5%).8 CPN schwannomas are exceedingly rare and only scarcely reported in the last four decades, leading to a long doctor’s delay as in our patient.9–14
If a patient reports lower leg altered skin sensations, a neuropathy is a probable cause. However, one has to differentiate whether the neuropathy has a central or a peripheral origin. Simple bedside tests may aid in locating a peripheral problem (ie, tibial, sural or common peroneal nerve involvement). Gently touching the skin with a cotton swab may identify areas of altered skin sensation. A different sense of temperature may be tested using an alcohol-soaked gauze. Pinching the skin may be more painful than usual and finger tapping may evoke electrical sensations along the affected nerve (Tinel). These tests must be executed on both legs.
MRI can confirm the diagnosis. Schwannomas have an isointense signal similar to the skeletal muscle on T1-weighted images and increased signal intensity on T2-weighted images. Distinctive features such as a mass located in the area of a major nerve and the presence of a split fat sign, fascicular sign or target sign, can help identifying the neurogenic origin of the mass.7
Surgery is the treatment of choice for symptomatic schwannomas as resection is easily possible without damaging the nerve fascicles.15 Unrestricted recovery is often accomplished. Complication rates for surgery of peroneal nerve schwannoma are unknown. However, decreased motor function after surgery for brachial plexus schwannoma was documented in 12% of patients previously having normal functioning (3/25).15
In conclusion, altered lower leg skin sensation due to CPN dysfunction combined with a palpable mass along the nerve and a positive Tinel sign may be due to a CPN schwannoma. Confirmation using MRI is indicated. Surgery is usually curative.
Patient’s Perspective.
Before surgery I had been experiencing nerve pains for 8 years. I was limited in sports activities and constantly ‘watchful’ that nothing or nobody would touch my leg, because that would provoke the pain. From the first moment after surgery, the nerve pain I have been experiencing for so many years, was completely gone. Everyone can ‘accidentally’ touch my leg again without feeling an electrical shock and more important, I am unrestricted regarding all physical activities. There is only a small area of skin next to the incision that is a little numb. I am extremely happy with the result.
Learning points.
A schwannoma of the common peroneal nerve (CPN) should be considered if simple bedside tests reveal an altered lower leg skin sensation, altered temperature sense and positive Tinel sign, combined with a palpable mass at the fibular head.
MRI can confirm the diagnosis CPN schwannoma.
Surgery is usually safe and successful.
Footnotes
Handling editor: Seema Biswas
Contributor: PC and MS contributed to the diagnosis and management of this patient. PC, MS and AVZ all contributed to the writing of this article.
Competing interests: None declared.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Apigian AK, Landry GJ. Basic data underlying decision making in nonatherosclerotic causes of intermittent claudication. Ann Vasc Surg 2015;29:138–53. 10.1016/j.avsg.2014.09.013 [DOI] [PubMed] [Google Scholar]
- 2.Burrus MT, Werner BC, Starman JS, et al. Chronic leg pain in athletes. Am J Sports Med 2015;43:1538–47. 10.1177/0363546514545859 [DOI] [PubMed] [Google Scholar]
- 3.Li S, King BN, Velasco N, et al. Cystic adventitial disease-case series and review of literature. Ann Transl Med 2017;5:327 10.21037/atm.2017.05.04 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Williamson A, Hoggart B. Pain: a review of three commonly used pain rating scales. J Clin Nurs 2005;14:798–804. 10.1111/j.1365-2702.2005.01121.x [DOI] [PubMed] [Google Scholar]
- 5.Pedowitz RA, Hargens AR, Mubarak SJ, et al. Modified criteria for the objective diagnosis of chronic compartment syndrome of the leg. Am J Sports Med 1990;18:35–40. 10.1177/036354659001800106 [DOI] [PubMed] [Google Scholar]
- 6.McKeag DB, Dolan C, Garrick JG. Overuse syndromes of the lower extremity. Phys Sportsmed 1989;17:108–23. 10.1080/00913847.1989.11709830 [DOI] [PubMed] [Google Scholar]
- 7.Pilavaki M, Chourmouzi D, Kiziridou A, et al. Imaging of peripheral nerve sheath tumors with pathologic correlation: pictorial review. Eur J Radiol 2004;52:229–39. 10.1016/j.ejrad.2003.12.001 [DOI] [PubMed] [Google Scholar]
- 8.Das Gupta TK, Brasfield RD, Strong EW, et al. Benign solitary Schwannomas (neurilemomas). Cancer 1969;24:355–66. [DOI] [PubMed] [Google Scholar]
- 9.Kwon NY, Oh HM, Ko YJ, et al. Multiple Lower Extremity Mononeuropathies by Segmental Schwannomatosis: A Case Report. Ann Rehabil Med 2015;39:833–7. 10.5535/arm.2015.39.5.833 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Shariq O, Radha S, Konan S. Common peroneal nerve schwannoma: an unusual differential for a symptomatic knee lump. BMJ Case Rep 2012;2012:bcr2012007346 10.1136/bcr-2012-007346 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Andrychowski J, Czernicki Z, Jasielski P. Schwannoma of the common peroneal nerve. A differential diagnosis versus rare popliteal cyst. Neurol Neurochir Pol 2012;46:396–400. [DOI] [PubMed] [Google Scholar]
- 12.de Jonge M, Deutman R, van Raay JJ. A swelling in the knee cavity, not caused by a Baker’s cyst but by a nerve sheath tumour. Ned Tijdschr Geneeskd 2005;149:312–6. [PubMed] [Google Scholar]
- 13.Houshian S, Freund KG. Gigantic benign schwannoma in the lateral peroneal nerve. Am J Knee Surg 1999;12:41–2. [PubMed] [Google Scholar]
- 14.Clifford JR, Pennington DG, Mills NL, et al. Thrombosis of the popliteal artery caused by a neurinoma of the common peroneal nerve. Am Surg 1974;40:392–4. [PubMed] [Google Scholar]
- 15.Kim DH, Murovic JA, Tiel RL, et al. Operative outcomes of 546 Louisiana State University Health Sciences Center peripheral nerve tumors. Neurosurg Clin N Am 2004;15:177–92. 10.1016/j.nec.2004.02.006 [DOI] [PubMed] [Google Scholar]


