Abstract
Severe extensive deep neck abscess in an infant is uncommon. We share the case of a previously well 4-month old infant who was referred for a 4-day history of fever, lethargy and left lateral neck swelling. Contrast-enhanced CT scan revealed a large 5.3×8 cm collection involving the left parapharyngeal and retropharyngeal space, causing significant airway narrowing. 40 mL of frank pus was drained via intraoral incision and drainage with the aid of endoscope, and undesirable complications from an external approach were averted. The infant was extubated 48 hours postsurgery and was discharged home well after completion of 1 week of intravenous antibiotics. The child was discharged well from our follow-up at 1 month review. We discuss the pathophysiology of deep neck space abscesses, its incidence in the paediatric population and the various management options.
Keywords: ear, nose and throat/otolaryngology; paediatric intensive care; otolaryngology / ent; paediatric surgery
Background
Deep neck space abscesses are commonly seen in the adult population especially in patients who are diabetics, immunocompromised or with a history of lodged foreign body. Although uncommon, they may present in the paediatric population at either extremes of the spectrum, that is, in a mild or severe life-threatening form. Prompt diagnosis and management is necessary to avoid potential complications such as airway obstruction, rupture of the abscess into the pharynx and trachea, empyema, mediastinitis and cavernous sinus thrombosis.
Case presentation
A previously well 4-month-old female infant was referred from a secondary healthcare centre with a 4-day history of fever, lethargy and left lateral neck swelling. She developed stridor and poor oral intake 2 days prior to admission. However, there were no episodes of cyanosis, vomiting or regurgitation. There were also no cough, ear discharge, previous trauma or insect bite and negative history of contact with tuberculosis-infected persons. The child was born at full term with a normal birth weight via spontaneous vertex delivery. Her growth parameters were within normal range and was immunised up to age by regular follow-up at the nearest primary care clinic. She is the only child and was exclusively breastfed by her mother. Both her parents are normal healthy individuals with no history of being immunocompromised.
Investigations
On examination, the child was pink but lethargic, tachycardic and febrile at 39°C, with the presence of an audible stridor and drooling of saliva. Neck examination revealed an inflamed 4 cm x 3 cm swelling at the left lateral aspect of the neck (figure 1). There was no cervical lymphadenopathy and other systemic examinations were unremarkable. Full blood counts showed leucocytosis with a white cell count of 15.5×105. Other parameters were within normal range. The child was intubated successfully at the second attempt by the paediatric consultant on call in view of worsening respiratory distress for airway protection. Contrasted CT scan of the neck revealed a large 5.3×8 cm collection involving the left parapharyngeal and retropharyngeal space (figure 2), extending superiorly to the level of skull base without intracranial extension, and inferiorly along the carotid sheath to the level of left sternoclavicular junction, causing significant airway narrowing.
Figure 1.

Left lateral neck swelling.
Figure 2.
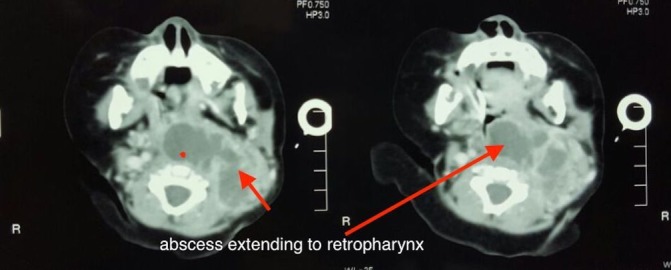
Axial CT demonstrating abscess collection within the parapharyngeal and retropharyngeal spaces.
Differential diagnosis
Deep neck abscess.
Treatment
An emergency intraoral incision and drainage was performed with endoscopic aid to enhance visualisation down the narrow pharynx. The incision was placed on the posterior pharyngeal wall bulge seen at the inferior level of the oropharynx (figure 3). We successfully drained 40 mL of frank pus intraoperatively (figures 4 and 5). Undesirable complications from an external approach were averted. The infant was extubated 48 hours post-surgery, resumed normal feeds after 72 hours and was discharged home well after completion of 1 week of intravenous cefotaxime and metronidazole. Cultures yielded no growth.
Figure 3.
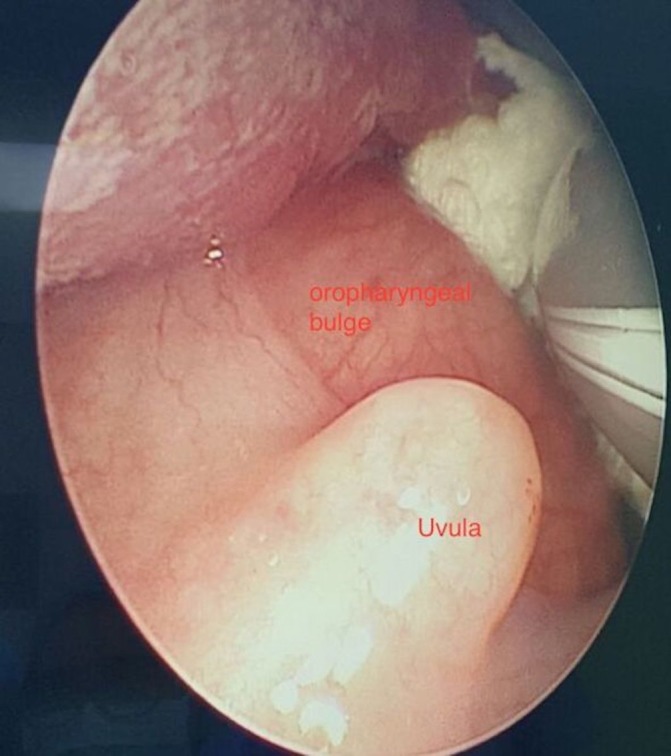
Endoscopic view of the inferior segment of the oropharynx demonstrating posterior pharyngeal wall bulge.
Figure 4.
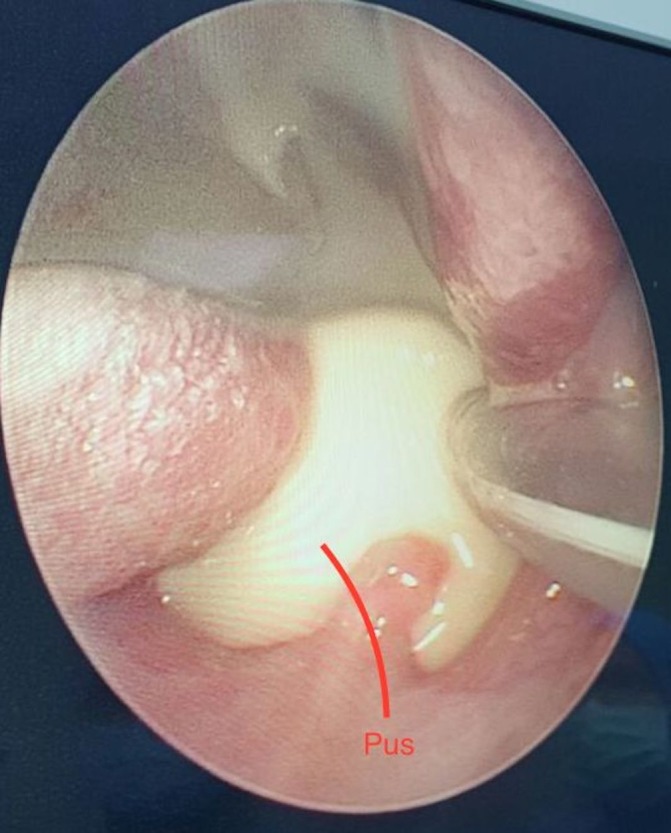
Endoscopic view showing pus drainage post incision.
Figure 5.
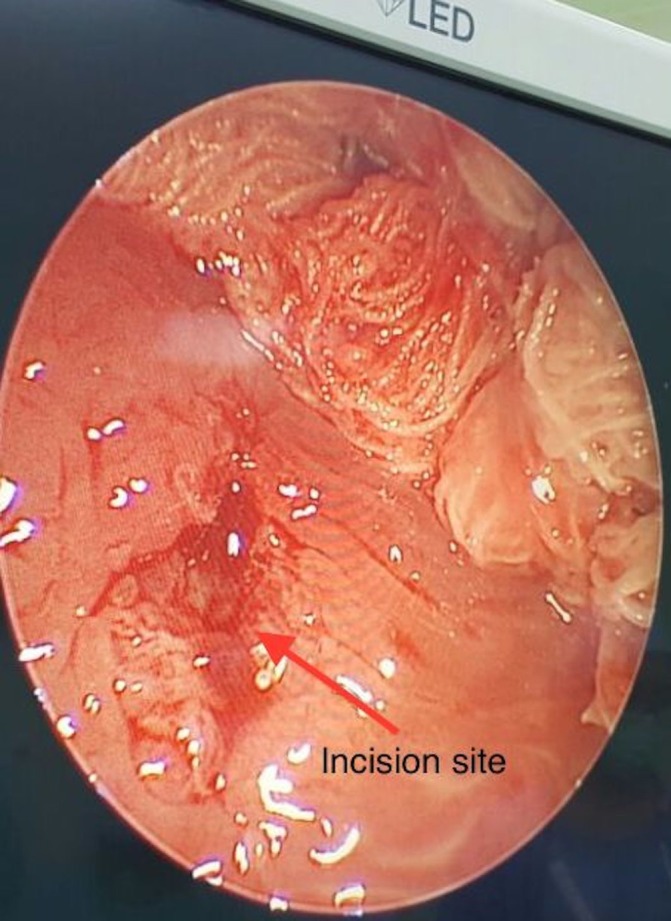
Reduction in size of the oropharyngeal bulge post drainage.
Outcome and follow-up
Bedside flexible laryngoscope prior to discharge showed a well-healed posterior pharyngeal wall with normal appearing neck (figure 6). The child was discharged from our follow-up at 1-month review.
Figure 6.

Resolved lateral neck swelling post drainage.
Discussion
The clinical presentation of a child with retropharyngeal abscess may be highly variable making diagnosis occasionally challenging. Children with deep neck space infections tend to have a more subtle presentation as compared with adults as they are seldom able to verbalise their symptoms or co-operate with physical examination. The most common cause of deep neck abscesses among children is upper respiratory tract infection (67%), followed by odontogenic origin (25.3%), as compared with trauma, foreign body ingestion or direct extension of a nasal or throat infection being the common causes in adults.1 2 These infection usually spread by direct continuity or via lymphatic drainage of the lymph nodes in children. Infection in children is contained within the retropharyngeal nodes and usually confined to the danger space as opposed to the widespread distribution and hence the more severe presentation in adults.2 Deep neck spaces are not true spaces, but in fact potential spaces partitioned by networks of fascia and areolar tissue. Hence, the mode of spread from one compartment to the other and the reason for the ability to drain multiple collections via a single compartment.
The common organisms responsible in causing deep neck abscesses are Staphylococcus aureus, S. viridans, beta-haemolytic streptococcus, Klebsiella pneumonia, Bacteroides and Peptostreptococcus.3 Penicillin with a combination of beta-lactamase inhibitor (clavulanic acid and ampicillin–sulbactam) or beta lactamase-resistant antibiotic (cefoxitin, cefuroxime, imipenem and meropenem) together with a combination of antianaerobic antibiotics (metronidazole or clindamycin) would usually be the empirical antibiotic of choice.2 3 Eventually culture directed therapy combined with clinical response would aid in deciding the appropriate antibiotics. Cefotaxime was administered in this child due to its broad-spectrum coverage against gram-positive and gram-negative organisms.
Various case series have reported on the rise of community-acquired methicillin-resistant S. aureus (CAMRSA), as high as 61%, as the isolated pathogen in paediatric deep neck abscesses.4 5 This possibility is worth bearing in mind and addition of clindamycin or vancomycin would be appropriate in such circumstances.4 5 The child in our case was nursed at home, was not cared for at a day care centre, had not been admitted or received prior antibiotics. Hence, the reason for not covering for MRSA here. Moreover, as the child showed remarkable rapid response within 24 hours of treatment and cultures were negative, escalation of antibiotics was deemed unnecessary.
Prompt antibiotic treatment, early detection and the availability of imaging modalities have significantly reduced the devastating consequences of an untreated abscess.6
A positive finding on lateral cervical X-ray which carries a sensitivity of 83%, coupled with clinical symptoms should suffice in diagnosing and managing an otherwise well child with retropharyngeal abscess conservatively, avoiding the unnecessary radiation of a CT.3 7 CT scans may fail to differentiate between abscess and phlegmons especially in a well child. However, in symptomatic children, coupled with clinical findings, CT may not be specific, but highly sensitive in diagnosing an abscess (92%).7 CT is especially useful for surgical planning, to assess the adjacent neurovascular structures, the extent of collection and to rule out other pathologies.
Smaller (<2.2 cm), non-symptomatic collections in older children (>4 years old) may be managed conservatively with trial of antibiotics for up to 48 hours.3 This also holds true for small locules in difficult to access locations, for example, collections in proximity to the skull base. However, a high index of suspicion and close observation is warranted in these children and the threshold to operate should be low if there is no clinical improvement. This is especially so because these children can progress to mediastinitis without any overt clinical findings.8
The principle of management of a larger symptomatic abscess is surgical drainage coupled with antibiotics. It is the approach that differs depending on the site of abscess. Although external approach is the common preferred option for surgical access, intraoral access may prove superior in selected cases with the advantage of avoiding neurovascular injuries. An external approach is commonly used in uncomplicated cases such as in superficial abscesses or when there is evidence of medial displacement of adjacent vital structures based on the results of CT scan.3 The risks involved in an external approach are haemorrhage from injury to the adjacent jugular vein or carotid artery, and injury to the cranial nerve branches, which can lead to severe morbidity.3 It is important to bear in mind that inflammation of nearby structures causes oedema, and this can make identifying and protecting vital neurovascular structures more challenging and demanding, especially so in infants with short, thick necks. Intraoral approach in draining a deep neck abscess have advantages of shorter hospital stay, lesser morbidity and hospital costs. However, it should not be the method of choice in patients with trismus, or when the collection is lateral to the major vessels. Occasionally, a combination of intraoral and external approach may prove necessary for adequate drainage of a multicompartment large collection.
Intubation remains a challenge in patients with deep neck abscesses, be it paediatrics or adults. Direct laryngoscopy and oral intubation have a risk of puncturing the abscess and causing aspiration of the pus.9 As a result of multiple unsuccessful intubation, the pus may tract into the airway and spread the infection downwards causing pneumonitis, bronchitis and tracheitis. In such situations, flexible fibre-optic nasal intubation may be necessary to secure the airway and avoid a tracheostomy.9 Retromolar intubation may be an option in patients with trismus, but again not without the risk of abscess wall puncture from manipulation. A tracheostomy under local anaesthesia might be necessary in select cases where attempt at intubation may prove to be more risky, especially with the possibility of loss of airway control. However, the technical challenge here would be the distortion of the dissection plane and tracheal deviation due to the oedema and inflammation from the abscess. Occasionally, a huge collection can be initially aspirated to reduce its size to provide better access for airway control, be it intubation or tracheostomy.
Multidisciplinary team effort is crucial in managing such patients. In the paediatric population, it is a shared airway between the paediatrician, anaesthetist and the surgeon. If the paediatrician, anaesthetist or emergency physician fail to secure the airway, the surgeon has to be prepared to perform a tracheostomy. Ideally the senior most available person should attempt the intubation, as in our case. The perioperative management is jointly done by the various teams as well to ensure a successful outcome for the patient.
Learning points.
Severe deep neck abscess, although uncommon in infants, is a life-threatening potentially lethal condition.
Prompt multidisciplinary management and appropriate surgical access can save lives without undesirable complications.
Intraoral drainage of an abscess collection with the aid of an endoscope should be considered when feasible.
Antimicrobial coverage for community-acquired methicillin-resistant Staphylococcus aureus should be considered given the rising prevalence of this organism in the published literature.
Footnotes
Contributors: AB: conception and design of the work, the acquisition, analysis or interpretation of data; drafting the work or revising it critically for important intellectual content; agreement to be accountable for all aspects of the work. JRS: drafting the work or revising it critically for important intellectual content; agreement to be accountable for all aspects of the work. NG: revising critically and final approval of the version published; agreement to be accountable for all aspects of the work. PR: revising critically and final approval of the version published; agreement to be accountable for all aspects of the work.
Competing interests: None declared.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Weed HG, Forest LA. Deep neck infection : Cummings C, Flint P, Harker L, Otolaryngology head and neck surgery. Philadelphia, PA: Mosby, 2005:2515–24. [Google Scholar]
- 2.Harkani A, Hassani R, Ziad T, et al. Retropharyngeal abscess in adults: five case reports and review of the literature. ScientificWorldJournal 2011;11:1623–9. 10.1100/2011/915163 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lawrence R, Bateman N. Controversies in the management of deep neck space infection in children: an evidence-based review. Clin Otolaryngol 2017;42:156–63. 10.1111/coa.12692 [DOI] [PubMed] [Google Scholar]
- 4.Naidu SI, Donepudi SK, Stocks RM, et al. Methicillin-resistant Staphylococcus aureus as a pathogen in deep neck abscesses: a pediatric case series. Int J Pediatr Otorhinolaryngol 2005;69:1367–71. 10.1016/j.ijporl.2005.04.001 [DOI] [PubMed] [Google Scholar]
- 5.Fleisch AF, Nolan S, Gerber J, et al. Methicillin-resistant Staphylococcus aureus as a cause of extensive retropharyngeal abscess in two infants. Pediatr Infect Dis J 2007;26:1161–3. 10.1097/INF.0b013e3181461b3a [DOI] [PubMed] [Google Scholar]
- 6.Page NC, Bauer EM, Lieu JE. Clinical features and treatment of retropharyngeal abscess in children. Otolaryngol Head Neck Surg 2008;138:300–6. 10.1016/j.otohns.2007.11.033 [DOI] [PubMed] [Google Scholar]
- 7.Grisaru-Soen G, Komisar O, Aizenstein O, et al. Retropharyngeal and parapharyngeal abscess in children--epidemiology, clinical features and treatment. Int J Pediatr Otorhinolaryngol 2010;74:1016–20. 10.1016/j.ijporl.2010.05.030 [DOI] [PubMed] [Google Scholar]
- 8.Shah RK, Chun R, Choi SS. Mediastinitis in infants from deep neck space infections. Otolaryngol Head Neck Surg 2009;140:936–8. 10.1016/j.otohns.2009.02.032 [DOI] [PubMed] [Google Scholar]
- 9.Cho SY, Woo JH, Kim YJ, et al. Airway management in patients with deep neck infections: A retrospective analysis. Medicine 2016;95:e4125 10.1097/MD.0000000000004125 [DOI] [PMC free article] [PubMed] [Google Scholar]


