Abstract
Background:
Computed tomography (CT) scans are useful for objectively measuring bone alignment because they show bone detail particularly well, and these scans have been used extensively to assess patellar orientation. The tibial tubercle–trochlear groove (TT-TG) offset distance has been shown to be influenced by knee flexion and weightbearing, yet conventional CT scans are obtained with the subject relaxed, supine, and with the knee in full extension. A new cone-beam CT scanner has been designed to allow for weightbearing images, potentially providing a more physiologically relevant assessment of patellofemoral alignment.
Purpose/Hypothesis:
The purpose of this study was to measure the TT-TG offset in healthy individuals without any history of knee complaints when CT scans were obtained while fully weightbearing on a flexed knee. Our hypothesis was that the TT-TG offset measurement in these healthy knees would be reproducible and less than the historically reported normal range.
Study Design:
Cross-sectional study; Level of evidence, 3.
Methods:
Twenty healthy volunteers without any history of knee complaint were recruited to undergo a weightbearing cone-beam CT scan of the knee flexed at 30°. The scans were reviewed by a radiologist and an orthopaedic surgeon, and TT-TG offset was measured using the digital tools of a picture archiving and communication system. Paired t tests were used to compare TT-TG offset on 2 separate occasions for both raters. Inter- and intrarater reliability were assessed using a 2-way mixed-effects model intraclass correlation coefficient with corresponding 95% confidence intervals for TT-TG offset.
Results:
The mean TT-TG offset was 2.7 mm. There were no statistically significant differences in TT-TG offset between raters (P rater1 = .70; P rater2 = .49) and time of read (P time1 = .83; P time2 = .19). Good to moderate interrater reliability was found at the time of both reads, and good intrarater reliability was found for both raters.
Conclusion:
When measured by CT scan and obtained from a subject while weightbearing on a flexed knee, the TT-TG offset is reproducible and the distance is less than that obtained via a conventional CT scan.
Keywords: tibial tubercle, trochlear groove, CT scan, patella
The tibial tubercle–trochlear groove (TT-TG) offset distance has been recognized6,10,15,18,26 as an important radiographic measure of the lateralizing effect of the tibial tubercle position on the patellofemoral joint since described by Goutallier et al.15 Computed tomography (CT) scans, because they show bone detail particularly well, are useful for objectively measuring bone alignment and have been used extensively to assess patellar orientation in all 3 cardinal planes. Conventional CT scans of the knee are acquired with the patient in a supine, nonweightbearing position, but limitations of this technique have been reported.16,22 New CT systems, including the On-Sight cone-beam CT scanner (Carestream Health), are available to acquire images while the patient is standing and to allow various positions of knee flexion and extension.11,22,33 It has been shown that knee position and weightbearing can independently affect the TT-TG offset distance.2,12,16,22,32,37
The purpose of this study was to measure the TT-TG offset distance in a series of patients without any history of knee complaints when the scans were obtained while fully weightbearing on a flexed knee. Our hypothesis was that the TT-TG offset distance in these healthy knees would be reproducible and less than the historically reported normal range of 10 to 15 mm.
Methods
Sample Selection
Permission to conduct this study was obtained from our institutional review board for human subject research (IRB No. 00000568) and is registered at ClinicalTrials.gov. Twenty healthy volunteers (10 females and 10 males) were recruited by responding to flyers distributed to orthopaedic residents, employees, and medical students from our institution. Patients were screened and enrolled by a trained research assistant. Exclusion criteria were a history of patellar instability, a history of any previous surgery on the knee, a fracture of the patellofemoral joint, a knee ligament injury, a history of high radiation exposure, current pregnancy, inability to bear weight for the cone-beam CT scan, or inability to speak English. The first 20 healthy volunteers who were screened and met the study criteria were enrolled.
Data Collection
Demographic data (age, sex, race, height, weight) were collected. An equal number of left and right knees were imaged for males and females. Each subject attended 1 study visit, at which time an investigational prototype CT scan (slice thickness 2 × 2 mm; radiation exposure 5 mA 90 kV) of the knee was obtained by trained CT technicians at a single hospital. Each CT scan was obtained after attaching a fixed-angle (30°) goniometer to the lateral aspect of the leg with lightweight elastic wrap, prompting the participant to stand on the designated leg with full single-leg weightbearing (Figure 1).
Figure 1.

Representation of a subject in the prototype cone-beam computer tomography scanner while weightbearing on a flexed knee. (Used with permission from Carestream Health, Rochester, New York, USA.)
The images were then reviewed on a reading station (GE PACS; GE Healthcare) by an experienced fellowship-trained musculoskeletal radiologist (rater 1) and an experienced fellowship-trained sports orthopaedic surgeon (rater 2). The images were presented in anonymous and sequential order (time 1) and were read a second time after 3 months (time 2). The TT-TG offset distance was measured with the digital tools of the PACS system as described in the literature and illustrated in Figure 2. The readers met to agree on the method as described by Goutallier et al,15 which measures the distance in millimeters between the most anterior point of the tibial tuberosity and the deepest bony point of the trochlear groove, along a line perpendicular to the bony borders of the posterior femoral condyles on axial CT scans.
Figure 2.
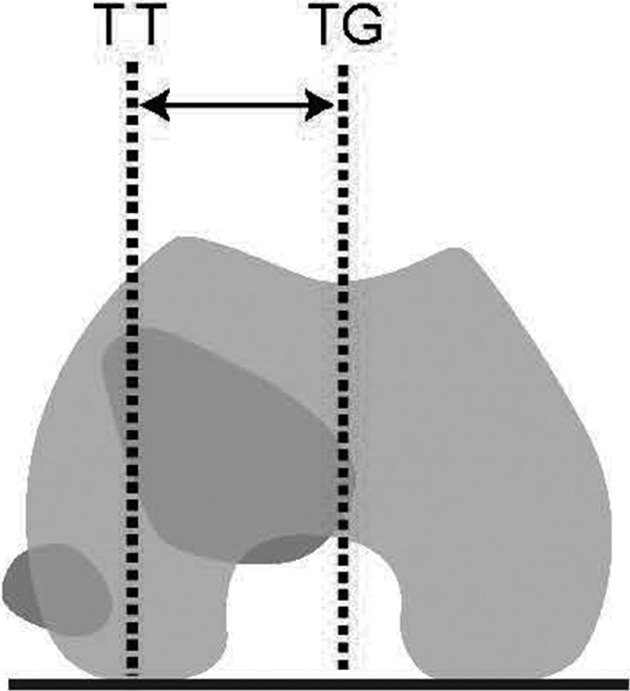
Schematic drawings of the method used to measure tibial tubercle (TT)–trochlear groove (TG) offset distance on axial 2-dimensional computed tomography images.
Analysis
Descriptive statistics were computed for patient demographic factors including age, sex, race, and body mass index (BMI, kg/m2). Paired t tests were used to compare TT-TG offset at time 1 and time 2 for both raters. Interrater reliability for TT-TG offset at time 1 and time 2 was assessed using a 2-way mixed-effects model intraclass correlation coefficient (ICC) with corresponding 95% CI. Intrarater reliability for rater 1 and rater 2 was also assessed using a 2-way mixed-effects model ICC with corresponding 95% CI. Based on an expected correlation of at least 0.50 between the TT-TG offset measures obtained from both raters, it was determined a priori that 20 patients were needed to obtain 80% power.34 SAS 9.4 (SAS Institute) and SPSS version 24 (SPSS Inc) were used for statistical analysis.
Results
Patient demographics are presented in Table 1. Mean age and BMI were 30.5 years and 25.9 kg/m2, respectively, and the entire sample was white.
TABLE 1.
Participant Demographics (N = 20)
| Age, y, mean ± SD | 30.5 ± 3.1 |
| Sex, n (%) | |
| Male | 10 (50) |
| Female | 10 (50) |
| Race, n (%) | |
| White | 20 (100) |
| Body mass index, kg/m2, mean ± SD | 25.9 ± 3.5 |
TT-TG offset is presented by rater and time of read in Table 2. There were no statistically significant differences in TT-TG offset between raters (P rater1 = .70; P rater2 = .49) and time of read (P time1 = .83; P time2 = .19). The mean TT-TG offset distance was 2.7 mm.
TABLE 2.
TT-TG Offset by Rater and Time of Reada
| Time 1 | Time 2 | P Valueb | |
|---|---|---|---|
| Rater 1 | 2.8 ± 4.3 | 3.4 ± 4.8 | .70 |
| Rater 2 | 2.5 ± 5.0 | 1.5 ± 4.1 | .49 |
| P valuec | .83 | .19 |
aData are means ± SD. TT-TG, tibial tubercle–trochlear groove.
bPaired t tests were used to calculate P values to examine the difference in TT-TG offset between time 1 and time 2.
cPaired t tests were used to calculate P values to examine the difference in TT-TG offset between rater 1 and rater 2.
Good to moderate interrater reliability was found at the time of both reads, and good intrarater reliability was found for both raters (Table 3).
TABLE 3.
Intraclass Correlation Coefficient (ICC) for Interrater and Intrarater Reliability
| ICC (95% CI) | |
|---|---|
| Interrater reliability | |
| Time 1 | 0.72 (0.42-0.88) |
| Time 2 | 0.66 (0.32-0.85) |
| Intrarater reliability | |
| Rater 1 | 0.92 (0.82-0.97) |
| Rater 2 | 0.77 (0.51-0.90) |
Discussion
Our study was designed to evaluate the feasibility, reproducibility, and results of TT-TG measures when obtained on a prototype portable cone-beam CT scanner that allowed simultaneous weightbearing and knee flexion. Since each condition is known to independently decrease TT-TG offset distance, our hypothesis was that their effect would be additive. Our results showed a mean TT-TG offset distance of 2.7 mm, with good to moderate interrater reliability and good intrarater reliability, thus proving our hypothesis.
Patellar instability is a significant clinical problem, with a multifactorial etiology that includes anatomic bony abnormalities of patellofemoral alignment. Many measures of patellofemoral alignment on CT scan, including tilt angle, congruence angle, and especially TT-TG offset, have been considered risk factors in patients who suffer from recurrent lateral patellar instability.1,10 The established normal value for TT-TG offset has been reported by multiple studies to be between 10 and 15 mm.8–10,15,25,30 Most agree that a TT-TG offset distance of greater than 20 mm is abnormal, but many patients are indicated for realignment surgery in the form of tibial tubercle transfer when a 15-mm threshold is exceeded.7,10,20,23,36 Previous studies have documented excellent interrater and intrarater reliability for CT measurements of TT-TG offset, but there is at least 1 study that shows an interrater difference of 3.2 mm on consecutive reads.20,21,24,29,31 Our reliability was somewhat less than that reported by others, which we attribute to the subjectivity that comes with deciding which CT slice is most appropriate at each level for measuring TT-TG offset.
When imaged by conventional CT scan technique, the patient is relaxed, lying supine on the examination table with the knee fully extended. A potential problem with this standard method of imaging is the static nature of the imaging position in an otherwise dynamic articulation, which is affected by many forces during normal activities. Others have shown that patellofemoral kinematics measured while supine do not accurately represent joint characteristics during weightbearing activities.13,19 This issue has been addressed in some imaging studies by modifying the scanner to simulate weightbearing using a shoulder or pelvic harness, pulleys, and weights.35
A prototype cone-beam CT scanner has been engineered, with one of its unique capabilities being the ability to acquire images while the patient is standing, weightbearing, and in various positions of knee joint flexion.5,38 Since patellar instability occurs with the knee flexed, and with the patient fully weightbearing, this “functional” CT scan provides an opportunity to obtain more physiologically relevant images of the knee and other joints.
The TT-TG offset distance (2.7 mm) that we found for healthy knees when images are obtained in this way is closer to zero and represents a patella that is well-centered in the trochlea. This makes biomechanical and intuitive sense for the trochlea and tibial tubercle to be collinear during activities of human function. Despite the goniometer being fixed at 30°, when we retrospectively measured the degree of knee flexion on sagittal 2-dimensional CT scans, the mean tibiofemoral flexion angle was 22°. It is plausible that if the knees were at 30° of flexion as intended, the trochlea and tibial tubercle would be collinear and the TT-TG offset distance would be even closer to zero. We suggest that this “near-zero point” may be the desired value of the TT-TG offset after tibial tubercle or other boney corrective surgery for patellar malalignment. The significantly lower value of the TT-TG offset raises the question of establishing a new threshold for CT examinations under physiological, upright weightbearing and functional positioning when evaluating patellofemoral diseases and contemplating surgery for malalignment.16,22
Previous studies using CT measures have shown a uniform decrease in TT-TG offset as the knee is flexed.4,22,32,37 Similar results have been reported in the magnetic resonance imaging (MRI) literature, and the effect is equal in healthy patients and in patients with symptomatic patellar instability.2,12,17,24,29 This is thought to be a result of the normal kinematics of the screw home mechanism of the knee joint.39 Flexion of the knee from full extension (unlocking of the screw home mechanism) causes an obligatory external rotation of the femur on the tibia, with the result being a decrease in the distance between the tibial tubercle and center of the trochlear groove. An MRI study by Izadpanah et al17 showed decreases in TT-TG of 4.3 mm at full extension and 2.4 mm at 30° of flexion as an effect of weightbearing alone. Another MRI study, however, showed no effect from weightbearing.2 Previous CT studies have shown a decrease in TT-TG of 3.3 mm at full extension and 2.2 mm at 30° of flexion as an effect of weightbearing alone.16,22 Our methods allow a direct comparison to the study of Marzo et al,22 where a group of patients with patellar instability were imaged supine by conventional CT scan and then during weightbearing by cone-beam CT with the knee held at 30° of flexion. The patients with patellar instability had a TT-TG of 20.1 mm on CT and 12.3 mm on cone-beam CT, as compared to the normal group imaged by cone-beam CT and reported here, where TT-TG offset was 2.7 mm.
Limitations of this study are the relatively low number of patients evaluated with this technique, and further studies are needed to establish threshold values in a larger population, in healthy volunteers, and in patients with specific patellofemoral diseases. While our subjects were screened for patellofemoral disease, some may have had asymptomatic patellar malalignment. A potential problem with this study is that we used an elastic wrap to hold a 30° fixed-angle goniometer to the leg, which could have acted as a source of influence on patellar alignment.3,14 In addition, we showed that the goniometer did not hold the knee in the desired position of 30° of knee flexion. The muscle force used by our patients was only enough to maintain single-leg weightbearing for the duration of the cone-beam CT, likely to have been far less than the force required for activities such as running, jumping, pivoting, and other higher-energy activities where patellar instability is known to occur. It is likely, however, that higher muscle forces would have acted to further decrease TT-TG distance. Determination of precise axial images for assessment of the trochlear groove, as well as the tibial tuberosity, is challenging, although we found good to moderate interrater reliability and good intrarater reliability. This can be an even greater issue when TT-TG is assessed by MRI because of the variability in cartilage coverage of the trochlea and whether one uses the tibial tubercle cortex or patellar tendon insertion distally.10,16,17,20,27,28
Conclusion
Patellofemoral instability is a very common clinical problem, often dealt with by corrective surgery guided by radiographic studies that have quantified the pattern and degree of malalignment. Our study has shown that CT scans, when used to evaluate the offset between the tibial tubercle and the trochlear groove, may be best obtained with the subject weightbearing on a flexed knee because it represents a more functional position. The prototype scanner used in this study has been approved by the United States Food and Drug Administration and is commercially available for this application. Measurements of TT-TG offset can be expected to be reproducible and less than previously reported in a healthy population and may represent a better evaluation of the degree of centralization of the patella on the distal femur. For image assessment of patellofemoral alignment in general, and for measuring TT-TG offset specifically, the novel abilities of the cone-beam CT scanner described in this study may provide specific advantages over conventional CT.
Footnotes
One or more of the authors has declared the following potential conflict of interest or source of funding: This study was funded by Carestream Health, Inc.
Ethical approval for this study was obtained from the University at Buffalo Institutional Review Board (IRB ID: STUDY00000568).
References
- 1. Balcarek P, Oberthur S, Hopfensitz S, et al. Which patellae are likely to redislocate? Knee Surg Sports Traumatol Arthrosc. 2014;22(10):2308–2314. [DOI] [PubMed] [Google Scholar]
- 2. Becher C, Fleischer B, Rase M, et al. Effects of upright weight bearing and the knee flexion angle on patellofemoral indices using magnetic resonance imaging in patients with patellofemoral instability. Knee Surg Sports Traumatol Arthrosc. 2017;25(8):2405–2413. [DOI] [PubMed] [Google Scholar]
- 3. Callaghan MJ, Guney H, Bailey D, et al. The effect of a patellar brace on patella position using weight bearing magnetic resonance imaging. Osteoarthritis Cartilage. 2014;22:S55. [DOI] [PubMed] [Google Scholar]
- 4. Camathias C, Pagenstert G, Stutz U, Barg A, Muller-Gerbl M, Nowakowski AM. The effect of knee flexion and rotation on the tibial tuberosity-trochlear groove distance. Knee Surg Sports Traumatol Arthrosc. 2016;24(9):2811–2817. [DOI] [PubMed] [Google Scholar]
- 5. Carrino JA, Al Muhit A, Zbijewski W, et al. Dedicated cone-beam CT system for extremity imaging. Radiology. 2014;270(3):816–824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Caton JH, Dejour D. Tibial tubercle osteotomy in patello-femoral instability and in patellar height abnormality. Int Orthop. 2010;34(2):305–309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Colvin AC, West RV. Patellar instability. J Bone Joint Surg Am. 2008;90(12):2751–2762. [DOI] [PubMed] [Google Scholar]
- 8. Dandy DJ. Chronic patellofemoral instability. J Bone Joint Surg Br. 1996;78(2):328–335. [PubMed] [Google Scholar]
- 9. Dejour D, Le Coultre B. Osteotomies in patello-femoral instabilities. Sports Med Arthrosc. 2007;15(1):39–46. [DOI] [PubMed] [Google Scholar]
- 10. Dejour H, Walch G, Nove-Josserand L, Guier C. Factors of patellar instability: an anatomic radiographic study. Knee Surg Sports Traumatol Arthrosc. 1994;2(1):19–26. [DOI] [PubMed] [Google Scholar]
- 11. Demehri S, Muhit A, Zbijewski W, et al. Assessment of image quality in soft tissue and bone visualization tasks for a dedicated extremity cone-beam CT system. Eur Radiol. 2015;25(6):1742–1751. [DOI] [PubMed] [Google Scholar]
- 12. Dietrich T, Betz M, Pfirrmann C, Koch P, Fucentese S. End-stage extension of the knee and its influence on tibial tuberosity-trochlear groove distance (TTTG) in asymptomatic volunteers. Knee Surg Sports Traumatol Arthrosc. 2014;22(1):214–218. [DOI] [PubMed] [Google Scholar]
- 13. Draper CE, Besier TF, Fredericson M, et al. Differences in patellofemoral kinematics between weight-bearing and non-weight-bearing conditions in patients with patellofemoral pain. J Orthop Res. 2011;29(3):312–317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Draper CE, Besier TF, Santos JM, et al. Using real-time MRI to quantify altered joint kinematics in subjects with patellofemoral pain and to evaluate the effects of a patellar brace or sleeve on joint motion. J Orthop Res. 2009;27(5):571–577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Goutallier D, Bernageau J, Lecudonnec B. The measurement of the tibial tuberosity. Patella groove distanced technique and results [in French]. Rev Chir Orthop Reparatrice Appar Mot. 1978;64(5):423–428. [PubMed] [Google Scholar]
- 16. Hirschmann A, Buck FM, Fucentese SF, Pfirrmann CW. Upright CT of the knee: the effect of weight-bearing on joint alignment. Eur Radiol. 2015;25(11):3398–3404. [DOI] [PubMed] [Google Scholar]
- 17. Izadpanah K, Weitzel E, Vicari M, et al. Influence of knee flexion angle and weight bearing on the tibial tuberosity-trochlear groove (TTTG) distance for evaluation of patellofemoral alignment. Knee Surg Sports Traumatol Arthrosc. 2014;22(11):2655–2661. [DOI] [PubMed] [Google Scholar]
- 18. Jones RB, Barlett EC, Vainright JR, Carroll RG. CT determination of tibial tubercle lateralization in patients presenting with anterior knee pain. Skeletal Radiol. 1995;24(7):505–509. [DOI] [PubMed] [Google Scholar]
- 19. Kim TH, Sobti A, Lee SH, Lee JS, Oh KJ. The effects of weight-bearing conditions on patellofemoral indices in individuals without and with patellofemoral pain syndrome. Skeletal Radiol. 2014;43(2):157–164. [DOI] [PubMed] [Google Scholar]
- 20. Koeter S, Horstmann WG, Wagenaar FCBM, Huysse W, Wymenga AB, Anderson PG. A new CT scan method for measuring the tibial tubercle trochlear groove distance in patellar instability. Knee. 2007;14(2):128–132. [DOI] [PubMed] [Google Scholar]
- 21. Lustig S, Servien E, Ait Si Selmi T, Neyret P. Factors affecting reliability of TT-TG measurements before and after medialization: a CT-scan study [in French]. Rev Chir Orthop Reparatrice Appar Mot. 2006;92(5):429–436. [DOI] [PubMed] [Google Scholar]
- 22. Marzo J, Kluczynski M, Notino A, Bisson L. Comparison of a novel weightbearing cone beam computed tomography scanner versus a conventional computed tomography scanner for measuring patellar instability. Orthop J Sports Med. 2016;4(12):2325967116673560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. McNally EG, Ostlere SJ, Pal C, Phillips A, Reid H, Dodd C. Assessment of patellar maltracking using combined static and dynamic MRI. Eur Radiol. 2000;10(7):1051–1055. [DOI] [PubMed] [Google Scholar]
- 24. Miyanishi K, Nagamine R, Murayama S, et al. Tibial tubercle malposition in patellar joint instability: a computed tomograpy study in full extension and at 30 degree flexion. Acta Orthop Scand. 2000;71(3):286–291. [DOI] [PubMed] [Google Scholar]
- 25. Monk AP, Doll HA, Gibbons CL, et al. The patho-anatomy of patellofemoral subluxation. J Bone Joint Surg Br. 2011;93(10):1341–1347. [DOI] [PubMed] [Google Scholar]
- 26. Pennock AT, Alam M, Bastrom T. Variation in tibial tubercle-trochlear groove measurement as a function of age, sex, size, and patellar instability. Am J Sports Med. 2014;42(2):389–393. [DOI] [PubMed] [Google Scholar]
- 27. Pfirrmann CW, Zanetti M, Romero J, Hodler J. Femoral trochlear dysplasia: MR findings. Radiology. 2000;216(3):858–864. [DOI] [PubMed] [Google Scholar]
- 28. Schoettle PB, Zanetti M, Seifert B, Pfirrmann CWA, Fucentese SF, Romero J. The tibial tuberosity-trochlear groove distance: a comparative study between CT and MRI scanning. Knee. 2006;13(1):26–31. [DOI] [PubMed] [Google Scholar]
- 29. Seitlinger G, Scheurecker G, Högler R, Labey L, Innocenti B, Hofmann S. The position of the tibia tubercle in 0°-90° flexion: comparing patients with patella dislocation to healthy volunteers. Knee Surg Sports Traumatol Arthrosc. 2014;22(10):2396–2400. [DOI] [PubMed] [Google Scholar]
- 30. Sherman SL, Erickson BJ, Cvetanovich GL, et al. Tibial tuberosity osteotomy: indications, techniques, and outcomes. Am J Sports Med. 2014;42(8):2006–2017. [DOI] [PubMed] [Google Scholar]
- 31. Skelley N, Friedman M, McGinnis M, Smith C, Hillen T, Matava M. Inter- and intraobserver reliability in the MRI measurement of the tibial tubercle-trochlear groove distance and trochlea dysplasia. Am J Sports Med. 2015;43(4):873–878. [DOI] [PubMed] [Google Scholar]
- 32. Tanaka MJ, Elias JJ, Williams AA, Carrino JA, Cosgarea AJ. Correlation between changes in tibial tuberosity-trochlear groove distance and patellar position during active knee extension on dynamic kinematic computed tomographic imaging. Arthroscopy. 2015;31(9):1748–1755. [DOI] [PubMed] [Google Scholar]
- 33. Tuominen EK, Kankare J, Koskinen SK, Mattila KT. Weight-bearing CT imaging of the lower extremity. AJR Am J Roentgenol. 2013;200(1):146–148. [DOI] [PubMed] [Google Scholar]
- 34. Walter SD, Eliasziw M, Donner A. Sample size and optimal designs for reliability studies. Stat Med. 1998;17(1):101–110. [DOI] [PubMed] [Google Scholar]
- 35. Ward SR, Terk MR, Powers CM. Patella alta: association with patellofemoral alignment and changes in contact area during weight-bearing. J Bone Joint Surg Am. 2007;89(8):1749–1755. [DOI] [PubMed] [Google Scholar]
- 36. Weber AE, Nathani A, Dines JS, et al. An algorithmic approach to the management of recurrent lateral patellar dislocation. J Bone Joint Surg Am. 2016;98(5):417–427. [DOI] [PubMed] [Google Scholar]
- 37. Williams AA, Elias JJ, Tanaka MJ, et al. The relationship between tibial tuberosity-trochlear groove distance and abnormal patellar tracking in patients with unilateral patellar instability. Arthroscopy. 2016;32(1):55–61. [DOI] [PubMed] [Google Scholar]
- 38. Zbijewski W, De Jean P, Prakash P, et al. A cone-beam CT system for musculoskeletal extremities with advanced multi-mode imaging capabilities. Int J Comput Assist Radiol Surg. 2011;6:S19–S21. [Google Scholar]
- 39. Zhang LK, Wang XM, Niu YZ, Liu HX, Wang F. Relationship between patellar tracking and the “screw-home” mechanism of tibiofemoral joint. Orthop Surg. 2016;8(4):490–495. [DOI] [PMC free article] [PubMed] [Google Scholar]


