Abstract
Pertussis is an acute respiratory illness caused by Bordetella pertussis, showing a re-emergence in developed countries. However, it is probably under-recognised and, as a consequence, its burden is underestimated. Here, we report the clinical case of an infant diagnosed with pertussis, despite a regular schedule of vaccination, thanks to a careful clinical evaluation, including personal and family history. In addition to pointing the attention on a precocious diagnosis of atypical cases of pertussis, this case report further raised the issue of modifying and/or implementing the immunisation strategy, considering the ongoing changes of social (eg, immigration) and sanitary (eg, vaccine coverage) background in Italy and all over the Europe.
Keywords: general practice / family medicine, global health, pneumonia (infectious disease), paediatrics
Background
Pertussis is an acute respiratory illness caused by Bordetella pertussis. Pertussis usually starts as an undifferentiated respiratory syndrome and, then, progresses to produce severe and paroxysmal attacks of ‘whooping’ cough. Vomiting, cyanosis and apnoea can occur as a result of these episodes of cough and, in infants and young children, complications have been described and may be life threatening, as impaired cerebral oxygenation may occur.1 Therefore, effective vaccines against pertussis have been developed and have been included in national immunisation programmes worldwide for several decades. In Italy, recommendations for pertussis immunisation were released in 1961 and the vaccination coverage increased substantially after 1995, corresponding to the introduction of acellular pertussis vaccines, which replaced whole-cell pertussis vaccine. As regards pertussis, Italy is currently reported as being a low incidence country: outbreaks or incidence peaks have been rarely reported after the achievement of high immunisation coverage. Although more than 90% of pertussis cases are currently reported in low-income and middle-income countries, actually a resurgence of such an infectious and preventable disease has been observed in Europe and USA. However, a precise estimate of the burden of pertussis is difficult, as under-recognition and/or under-reporting probably occur, as physicians, including paediatricians, have not been used to deal with such a disease in children for a long time.2
Here, we report the clinical case of an infant diagnosed with pertussis, despite a regular schedule of vaccination for age, consisting of the first two doses only, according to the Italian immunisation schedule for a child aged 8 months.
Case presentation
Recently, an 8-month-old infant was admitted to the Paediatric Department on the request of her general paediatrician. That was because she had suffered of persistent/recurrent cough and wheezing for more than 4 weeks, despite several therapies prescribed by the general paediatrician, including bronchodilator drugs, steroids and beta-lactam antibiotics; no macrolides had been prescribed until that point. When the infant was evaluated at the hospital, a careful clinical history and physical exam were obtained: she displayed mild wheezing with no relevant localised respiratory sounds. Her vital signs were normal (non-invasive oxygen saturation: 96%, normal values (nv): >95%; heart rate: 104 beats per minute, nv: 90–120; respiratory frequency: 34 breaths per minute, nv: 24–34; arterial blood pressure: 90/60 mmHg, nv: >80/>50 mmHg; capillary refilling <1 s, nv: <2 s). In the family history, an interesting data was that the father used to serve as a volunteer worker in hospital patients’ transportations and he had suffered of persistent cough for some weeks, too.
Investigations
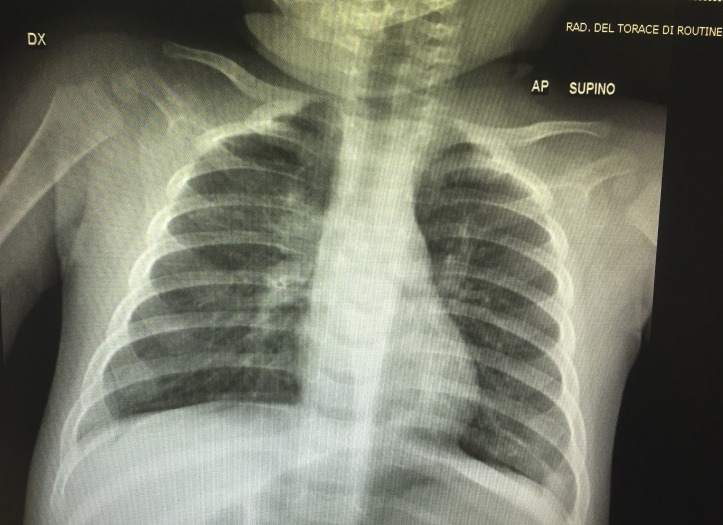
At the admission, the chest X-ray showed an interstitial pattern of lung inflammation, consolidating at the upper right lobe (figure 1).
Figure 1.
Chest X-ray: interstitial pneumonia associated to pertussis.
As regards the laboratory investigations, the blood cell count was characterised with a prominent leucocytosis (White cell count: 27 600 109/L), whereas platelets were mildly increased for age (293 000 109/L) and haemoglobin was normal (12.6 mg/dL); however, there was no significant increase of neutrophils and, indeed, the leucocytosis was mainly driven by lymphocytes. Accordingly, the C-reactive protein was only moderately elevated (37 mg/L; nv: 0–5).
Although the mother confirmed that her daughter had received all the scheduled vaccinations for age, namely, the first two doses, the long-lasting personal history of cough and father’s persistent cough have made us consider a potential diagnosis of pertussis since the first evaluation. Thus, the dosage of serum IgM specific for B. pertussis was requested and, after 4 days, the result confirmed the presence of specific IgM, supporting a diagnosis of pertussis. Unfortunately, the father did not agree to check his serology status.
As an ancillary laboratory finding, it is useful to notice that total serum levels of all classes of immunoglobulin were quite elevated for age (IgG 1001 mg/dL, nv 450–850 mg/dL; IgA 135 mg/dL, nv 20–55 mg/dL; IgM 73 mg/dL, nv 30–70 mg/dL). In particular, a very high IgE level was detected, as it was 1417 UI/mL (nv <30 UI/mL).
Differential diagnosis
At this age, the differential diagnosis of persistent cough and/or recurrent wheezing is mainly represented by the occurrence of consecutive respiratory viral illnesses that may be complicated by a bacterial superimposition. In particular, syncytial respiratory virus must be considered and, interestingly, such an infection has been reported to elicit an elevation of total IgE, as well as it has been described during pertussis. Based on the clinical data and the results of all the laboratory investigations, such as normal values of all immunoglobulin classes, other pathological disorders, including allergy and some primary immunodeficiency diseases (eg, hyper-IgE syndromes, Wiskott-Aldrich disease, DiGeorge syndrome, etc) could be excluded.3 4 Moreover, total IgE levels showed a significant reduction at 4 weeks after the end of the antibiotic therapy.
Treatment
As soon as the patient was admitted to the hospital, the antibiotic therapy with clarithromycin was started, considering the clinical suspicion. Thus, once the diagnosis of pertussis was serologically confirmed, the antibiotic therapy was administered for 15 days and the infant recovered completely.
Discussion
Such a short clinical report highlighted that the occurrence of pertussis during the first year of life must be suspected and investigated in infants presenting persistent cough and/or recurrent wheezing, as the immunisation schedule has not been completed yet. The first doses of pertussis vaccine may mitigate the clinical expression of the disease, but cannot preserve completely from the infection in all cases. Unfortunately, in developed countries, the occurrence of pertussis is often underconsidered in infancy, especially when the typical clinical expression is lacking: thus, the diagnosis may be delayed and, as a consequence, the resolution of the clinical problem, too.
On the contrary, adolescents and adults are unlikely to experience severe complications from pertussis and they usually present persistent, but not specific, cough. As a consequence, those individuals can act as vectors of infection, when they get in contact with those who are more vulnerable, including unvaccinated or incompletely vaccinated infants and children.5 Interestingly, in our case, the most likely source of infection could have been a close relative, namely, the father, who had complained of persistent cough in the previous weeks and used to serve as a volunteer in an hospital setting. As well as in other unusual and/or disappeared infectious diseases in developed countries,6 7 the diagnosis of pertussis was significantly driven by a careful collection of the personal and family history.
In addition to pointing the attention on a precocious diagnosis of pertussis, this case report further raised the issue of modifying and/or implementing the immunisation strategy, considering the ongoing changes of social (eg, immigration) and sanitary (eg, vaccine coverage) background in Italy and all over the Europe.
In most western countries, the ‘acellular’ pertussis vaccine is currently used: it consists of several purified and inactivated bacterial components and it is usually combined with tetanus and diphtheria toxoids. Importantly, two different formulations are available, according to the amount antigenic components, being 25 µg (Pa) and 8 µg (pa), respectively: the former is used in children younger than 7 years, whereas the latter is used to provide the booster doses in adolescents and adults. According to the Italian immunisation schedule, children are supposed to receive four doses of DTaP vaccine, exactly at 3 months, 5 months, 11 months and 6 years of life. Eventually, a booster dose (Tdap) is scheduled at the age of 12 years and, after that, it should be administered every 10 years.8 Thanks to such an immunisation policy, in Italy pertussis vaccine coverage increased dramatically, until reaching 96.2% in 2010: importantly, from 1995 to 2001, only one pertussis death per year was reported and no deaths had been reported at all since 2002; unfortunately, in October 2015 a newborn died of pertussis. Currently, the vaccine coverage for pertussis within the age of 2 years in Italy is estimated to be around 93.3%, as the trend has been reducing since 2012.2
Lowering the time points of the three vaccine doses during the first year of life could help to improve the coverage in infants, but it is not enough, as evidenced by the model of disease prevalence provided by Bento et al in USA.9 Indeed, an important window of susceptibility persists during the first year of life and, in particular, in the first 2 months, if the environmental circulation of the bacterium is not interrupted by minimising also the number of susceptible adults, representing the weakest link in the ‘prevention chain’. However, pertussis can be mitigated and manifest through an atypical course of disease in infants, if the infection occurs when the immunisation schedule has started regularly, but not completed yet.1 9 10 It is well known that there is a lack of long-term persistence of pertussis immunity after the completion of the scheduled immunisations in the paediatric age and, therefore, the protection against pertussis wanes if booster doses are not administered every 10 years,9 as occurs too frequently in Italy, despite the aforementioned recommendation. Indeed, our common experience with the medical activities at the Emergency Department is that most adults evaluated because of contaminated wounds need the vaccination against tetanus, meaning that they have not repeated Tdap booster for more than 10 years and, as a consequence, they are very likely to be susceptible to the infection with B. pertussis, too. Thus, ‘cocoon’ vaccination strategy, which consists of immunising family members and close contacts of the neonate, and mother’s prenatal vaccination have been recently proposed in order to reduce the risk of pertussis in younger infants.9 11
Learning points.
Pertussis can manifest through atypical course of disease in infants: it may be mitigated by an uncompleted immunisation programme.
Recurrent and persisting cough in infancy, despite several therapies, should raise the clinical suspicion of pertussis.
A report of a close relative complaining of persisting cough should alert the physician about a potential diagnosis of pertussis in an infant who has not received all the vaccinations yet.
Footnotes
Contributors: DP diagnosed and managed the clinical case. MGN, NM and PB provided contribution to the clinical management. DP conceived and wrote the paper.
Competing interests: None declared.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Ebell MH, Marchello C, Callahan M. Clinical diagnosis of Bordetella pertussis infection: a systematic review. J Am Board Fam Med 2017;30:308–19. 10.3122/jabfm.2017.03.160330 [DOI] [PubMed] [Google Scholar]
- 2.Gonfiantini MV, Carloni E, Gesualdo F, et al. Epidemiology of pertussis in Italy: disease trends over the last century. Euro Surveill 2014;19:20921 10.2807/1560-7917.ES2014.19.40.20921 [DOI] [PubMed] [Google Scholar]
- 3.Marseglia GL, Caimmi S, Marseglia A, et al. Rhinosinusitis and asthma. Int J Immunopathol Pharmacol 2010;23(1 Supp):29–31. [PubMed] [Google Scholar]
- 4.Poddighe D, Virginia E, Nedbal M, et al. Postnatal cytomegalovirus infection in an infant with congenital thrombocytopenia: how it can support or mislead the diagnosis of Wiskott-Aldrich syndrome. Infez Med 2016;24(3):237–240. [PubMed] [Google Scholar]
- 5.Chiappini E, Stival A, Galli L, et al. Pertussis re-emergence in the post-vaccination era. BMC Infect Dis 2013;13:151 10.1186/1471-2334-13-151 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Poddighe D. Letter to the editor: the measles outbreak in Bulgaria, 2009–2011: an epidemiological assessment and lessons learnt – but not completely yet. Euro Surveill 2016;21(13) 10.2807/1560-7917.ES.2016.21.13.30178 [DOI] [PubMed] [Google Scholar]
- 7.Poddighe D, Bonomelli I, Giardinetti S, et al. Paediatric dengue fever diagnosed through parents' epidemiologic report and preventive strategy during the acute phase of infection. J Travel Med 2016;23(1):tav013 10.1093/jtm/tav013 [DOI] [PubMed] [Google Scholar]
- 8.Le vaccinazioni in Italia: copertura vaccinale in Italia Pertosse. http://www.epicentro.iss.it/temi/vaccinazioni/dati_Ita.asp#pertosse (accessed 29 May 2017).
- 9.Bento AI, King AA, Rohani P. Maternal pertussis immunisation: clinical gains and epidemiological legacy. Euro Surveill 2017;22 10.2807/1560-7917.ES.2017.22.15.30510 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Poddighe D. Re: clinical diagnosis of Bordetella pertussis infection: a systematic review. J Am Board Fam Med 2017;30(5):681 10.3122/jabfm.2017.05.170221 [DOI] [PubMed] [Google Scholar]
- 11.Rossmann Beel E, Rench MA, Montesinos DP, et al. Acceptability of immunization in adult contacts of infants: possibility of expanding platforms to increase adult vaccine uptake. Vaccine 2014;32:2540–5. 10.1016/j.vaccine.2014.03.056 [DOI] [PubMed] [Google Scholar]