Abstract
Patient: Male, 51
Final Diagnosis: Liver cirrhosis by hepatitis virus C and hepatocellular carcinoma
Symptoms: Ascites
Medication: —
Clinical Procedure: Liver transplantantion
Specialty: Surgery
Objective:
Rare co-existance of disease or pathology
Background:
Adequate portal venous flow is required for successful liver transplantation. Reduced venous flow and blood flow ‘steal’ by collateral vessels are a concern, and when there is a prominent splenorenal shunt present, ligation of the left renal vein has been recommended to improve portal venous blood flow.
Case Report:
A 51-year-old man who had undergone right nephrectomy in childhood required liver transplantation for liver cirrhosis and hepatocellular carcinoma due to hepatitis C virus (HCV) infection. The patient had no other comorbidity and no history of hepatorenal syndrome. At transplantation surgery, portal venous flow was poor and did not improve with ligation of shunt veins, but ligation of the left renal vein improved portal venous flow. On the first and fifth postoperative days, the patient was treated with basiliximab, a chimeric monoclonal antibody to the IL-2 receptor, and methylprednisolone. The calcineurin inhibitor, tacrolimus, was introduced on the fifth postoperative day. On the sixteenth postoperative day, renal color Doppler ultrasound showed normal left renal parenchyma; hepatic Doppler ultrasound showed good portal vein flow and preserved hepatic parenchyma in the liver transplant.
Conclusions:
This case report has shown that in a patient with a single left kidney, left renal vein ligation is feasible and safe in a patient with no other risk factors for renal impairment following liver transplantation. Modification of postoperative immunosuppression to avoid calcineurin inhibitors in the very early postoperative phase may be important in promoting good recovery of renal function and to avoid the need for postoperative renal dialysis.
MeSH Keywords: Acute Kidney Injury, Immunosuppression, Liver Transplantation, Portal Vein, Renal Veins
Background
During preoperative evaluation of patients who require liver transplantation, portal vein patency, and portal venous blood flow is an important factor that predicts patient survival following transplantation [1]. Compromise of portal venous blood flow can be due to vein thrombosis or to ‘steal’ of venous blood flow through portosystemic shunts and can lead to postoperative liver failure due to portal hypoperfusion [2,3]. Preoperative imaging studies can be helpful in identifying compromise to portal venous blood flow.
Previously published studies have shown the safety and utility of left renal vein ligation in the treatment of portal venous blood flow ‘steal’ through a large splenorenal shunt [4–6]. Left renal vein ligation can be combined with thrombectomy in cases of portal vein thrombosis, and the procedure allows redirection of the splanchnic blood flow through the portal vein graft [4–6]. Left renal vein ligation should be performed at the confluence with the inferior vena cava (IVC), and has been reported to be a safe procedure that allows for continued renal function [6,7]. There are additional veins connected to the left kidney that include the gonadal, adrenal, lumbar and splenorenal veins.
However, it is unclear whether or not patients with only a left kidney can undergo left renal vein ligation while maintaining good long-term renal function [6,7].
Case Report
A 51-year-old man who had undergone right nephrectomy in childhood required liver transplantation for liver cirrhosis and hepatocellular carcinoma due to hepatitis C virus (HCV) infection. The patient had no other comorbidity and no history of hepatorenal syndrome or ascites.
On examination on hospital admission, the patient’s Child– Pugh score was A, and the Model of End-Stage Liver Disease (MELD) score was 14, with a serum albumin of 3.0 g/dl and an international normalized ratio (INR) of 1.78 (N range=2.0–3.0). During the pre-transplantation evaluation, the abdominal scan showed a very thin portal vein, with cavernous transformation (Figure 1).
Figure 1.
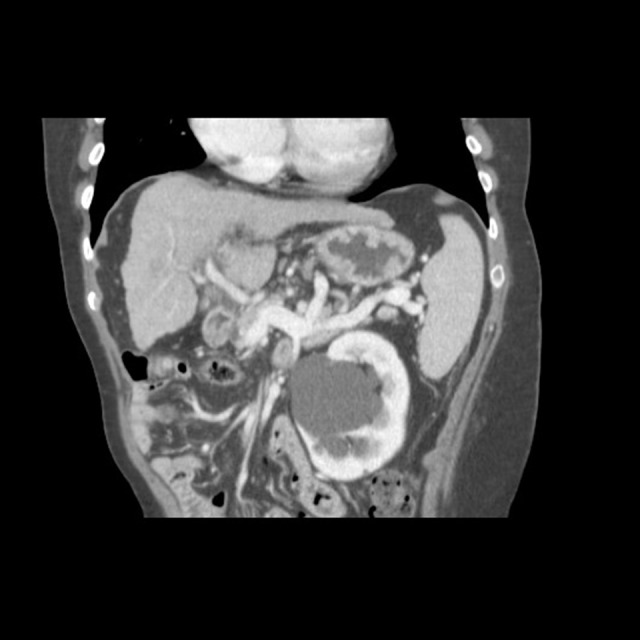
A thin portal vein is seen in the hepatic hilum.
Splenic and superior mesenteric veins were patent with increased caliber. The presence of spontaneous splenorenal shunt and signs of right nephrectomy were also observed. The single kidney (left kidney) measured 13.1 cm and had preserved parenchyma with good concentration of contrast and contained a cyst measuring 6.1×6.0 cm on the largest axis and some nephrolithiasis (Figure 2). The creatinine level was 0.82 mg/dL.
Figure 2.

A splenorenal shunt is seen in the left single kidney with a large renal vein.
The patient underwent liver transplantation, receiving a whole deceased donor graft. The piggyback technique was applied. A cava-cava anastomosis was carried out between the cava vein of the graft and the left/medium vein trunk ostium extended to the right side of the recipient. A temporary portocaval shunt was performed before the hepatectomy, as this is a routine procedure in our service. At transplantation surgery, portal venous flow was poor and did not improve with ligation of shunt veins, but ligation of the left renal vein improved portal venous flow. A collateral vein was found to the pancreatic tail, but when clamped there was no improvement of the portal flow. The left renal vein was dissected through the anterior inferior vena cava (IVC), and when it was clamped, the portal vein flow increased significantly to a normal flow. The total ischemia time was eight hours, and the warm ischemia time was 33 minutes. The patient remained stable throughout the procedure. The strategy of left renal vein ligation, by a simple 2.0 suture, in its confluence with the cava vein resulted in a significant increase in portal vein flow and better reperfusion of the liver.
On the first and fifth postoperative days, the patient was treated with basiliximab, a chimeric human/murine monoclonal antibody to the IL-2 receptor, and also treated with methylprednisolone. The calcineurin inhibitor, tacrolimus, was introduced on the fifth postoperative day. On the sixteenth postoperative day, renal color Doppler ultrasound showed normal left renal parenchyma, and hepatic Doppler ultrasound showed good portal vein flow and preserved hepatic parenchyma in the liver transplant. During this period, creatinine levels ranged from 0.98 mg/dL to 2.06 mg/dL up to the sixth day. The patient reported macroscopic hematuria on the first postoperative day, which remained for 48 hours. Urine output was good during the whole hospital stay. During the first ten days of tacrolimus treatment, the creatinine levels ranged from 1.27 mg/dL to 2.56 mg/dL (Figure 3).
Figure 3.
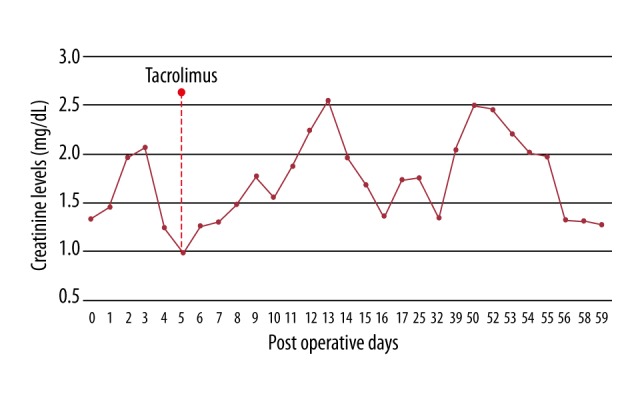
The creatinine levels following left renal vein ligation during liver transplantation in the patient siwth a single left kidney.
On the sixteenth postoperative day, a renal color Doppler ultrasound was performed, in which normal renal parenchyma with slightly increased echogenicity and a good corticomedullary differentiation was observed. Hepatic Doppler ultrasound showed good portal vein flow and preserved hepatic parenchyma.
The patient presented with a transient acute renal injury in the early postoperative days, which recovered to preoperative levels, so that the patient was discharged on the sixteenth day with good hepatic and renal function. Eight months following liver transplant surgery, the patient was still on tacrolimus and steroid immunosuppression with good renal and hepatic function.
Discussion
The present case is the second case of left renal vein ligation in a patient with a solitary left kidney and liver transplantation to improve portal venous flow, described in the literature, and the first to use immunosuppression induction with basiliximab in this context. This case report describes the management of a challenging surgical situation with a good outcome.
Portal venous blood flow is important to a good outcome in liver transplantation, and splenorenal shunt and ‘steal’ of portal venous blood flow has to be identified and properly managed during the operative procedure.
Ligation of the left renal vein close to the inferior vena cava (IVC) has been proposed as an effective approach that can lead to a redirection of the splanchnic flow through the graft portal vein, without damage to the venous drainage of the left kidney drainage [3,5]. Ligation of the left renal vein has previously shown to be a safe procedure, as shown by renal function measurements three months after transplantation, including urine output, proteinuria, hematuria, serum creatinine or blood urea nitrogen [3]. Recently, Golse et al. found no difference between short-term and long-term results that compared left renal vein ligation with reno-portal anastomosis in patients with spontaneous splenorenal shunt undergoing liver transplantation [5]. In two published studies, when left renal vein ligation was compared with splenectomy, to avoid vascular ‘steal,’ left renal vein ligation was found to be the safer and less technically demanding procedure [6,7].
From the published literature, left renal vein ligation has been shown to be a safe procedure when the patient had two functioning kidneys. However, in this case, the surgical team performed liver transplantation for a patient with a single left kidney, and the decision to ligate the left renal vein was not easy because only one similar case had been previously reported in the literature [8].
However, the previously published literature supports that the left renal vein can drain both kidneys through its branches in the event of vena cava resections [9]. Also, reports of end-to-end renal vein anastomosis were not in patients with cirrhosis, where the left renal vein receives larger collateral vessels and probably has better drainage [9].
Concerns about postoperative renal function led to the decision to modify our immunosuppression strategy. Basiliximab induction was used to avoid further injury to the kidney caused by calcineurin inhibitors in the very early postoperative phase. We believe that this treatment strategy was important in promoting good recovery of renal function and avoided the need for postoperative renal dialysis.
Despite the patient’s previous history of hepatitis C virus infection (HCV) in this case, no other preoperative risk factors for acute kidney injury were identified, such as kidney dysfunction, hepatorenal syndrome, hypoalbuminemia, hypovolemia, ascites, or concomitant chronic disease (diabetes mellitus or hypertension) [10]. Ligation of the left renal vein is an approach that should be performed only when the patient does not present with any pre-existing condition that may impair renal function.
Even during the operative procedure, there was no need for blood transfusion or persistent use of vasoactive drugs, and the vena cava was not clamped. Although a large splenorenal shunt was present, we decided to cut the portal vein early to test the portal flow, and then performed a portocaval shunt to be sure about the effectiveness of the ligating the left renal vein. Clamping the other collateral veins close to the pancreatic tail was not effective.
The intraoperative approach to liver transplantation in the case of a patient with a solitary left kidney and reduced portal venous blood flow required the use of maneuvers to preserve renal function, including minimizing blood loss, avoidance of total vena cava clamping, and temporary portocaval anastomosis. Furthermore, in the postoperative period, we had to be aware of the risk of renal impairment caused by vasoactive drugs, antibiotics, or immunosuppressive drugs.
Conclusions
This case report has shown that in a patient with a single left kidney, left renal vein ligation is feasible and safe in a patient with no other risk factors for renal impairment following liver transplantation. Modification of postoperative immunosuppression to avoid calcineurin inhibitors in the very early postoperative phase may be important in promoting good recovery of renal function and to avoid the need for postoperative renal dialysis.
References:
- 1.Spitzer AL, Dick AA, Bakthavatsalam R, et al. Intraoperative portal vein blood flow predicts allograft and patient survival following liver transplantation. HPB (Oxford) 2010;12:166–73. doi: 10.1111/j.1477-2574.2009.00137.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gontarczyk GW, Łagiewska B, Pacholczyk M, et al. Intraoperative blood flow measurements and liver allograft function: preliminary results. Transplant Proc. 2006;38:234–36. doi: 10.1016/j.transproceed.2005.12.086. [DOI] [PubMed] [Google Scholar]
- 3.Lee SG, Moon DB, Ahn CS, et al. Ligation of left renal vein for large spontaneous splenorenal shunt to prevent portal flow steal in adult living donor liver transplantation. Transpl Int. 2007;20:45–50. doi: 10.1111/j.1432-2277.2006.00392.x. [DOI] [PubMed] [Google Scholar]
- 4.Golse N, Mohkam K, Rode A, et al. Surgical management of large spontaneous portosystemic splenorenal shunts during liver transplantation: Splenectomy or left renal vein ligation? Transplant Proc. 2015;47:1866–76. doi: 10.1016/j.transproceed.2015.06.019. [DOI] [PubMed] [Google Scholar]
- 5.Golse N, Bucur PO, Faitot F, et al. Spontaneous splenorenal shunt in liver transplantation: results of left renal vein ligation versus renoportal anastomosis. Transplantation. 2015;99:2576–85. doi: 10.1097/TP.0000000000000766. [DOI] [PubMed] [Google Scholar]
- 6.Slater RR, Jabbour N, Abbass AA, et al. Left renal vein ligation: A technique to mitigate low portal flow from splenic vein siphon during liver transplantation. Am J Transplant. 2011;11:1743–47. doi: 10.1111/j.1600-6143.2011.03578.x. [DOI] [PubMed] [Google Scholar]
- 7.Elsharawy MA, Cheatle TR, Clarke JM, et al. Effect of left renal vein division during aortic surgery on renal function. Ann R Coll Surg Engl. 2000;82:417–20. [PMC free article] [PubMed] [Google Scholar]
- 8.Genzini T, Trevizol AP, Yamashita ET, et al. Left renal vein ligation during liver transplantation in a recipient with a single kidney. Liver Transplant. 2013;19:563–64. doi: 10.1002/lt.23636. [DOI] [PubMed] [Google Scholar]
- 9.Araujo RL, Gaujoux S, D’Albuquerque LA, et al. End-to-end renal vein anastomosis to preserve renal venous drainage following inferior vena cava radical resection due to leiomyosarcoma. Ann Vasc Surg. 2014;28(4):1048–51. doi: 10.1016/j.avsg.2013.08.027. [DOI] [PubMed] [Google Scholar]
- 10.Wiesen P, Massion PB, Joris J, et al. Incidence and risk factors for early renal dysfunction after liver transplantation. World J Transplant. 2016;6:220–32. doi: 10.5500/wjt.v6.i1.220. [DOI] [PMC free article] [PubMed] [Google Scholar]


