Abstract
Understanding statistical differences in states’ percentages and ranks of adolescents meeting health behavior guidelines can guide policymaking. Data came from 531,777 adolescents (grades 9–12) who completed the Youth Risk Behavior Surveillance System survey in 2011, 2013, or 2015. We measured the percentage of adolescents in each state that met guidelines for physical activity, fruit and vegetable (F&V) consumption, and healthy weight status. Then we ranked states and calculated the ranks’ 95% CI’s using a Monte Carlo method with 100,000 simulations. We repeated these analyses stratified by sex (female or male) or race/ethnicity (non-Hispanic white, non-Hispanic black, Hispanic/Latino, or other). Pearson’s and Spearman’s correlation coefficients examined consistency in the percentages and ranks (respectively) across behaviors and subgroups. Meeting the physical activity and F&V consumption guidelines was relatively rare among adolescents (25.8% [95% CI=25.2%–26.4%] and 8.0% [95% CI=7.6%–8.3%], respectively), while meeting the healthy weight guideline was common (71.5% [95% CI=70.7%–72.3%]). At the state level, percentages of adolescents meeting these guidelines were statistically similar; states’ ranks had wide CI’s, resulting in considerable overlap (i.e., statistical equivalence). For each behavior, states’ percentages and ranks were moderately to highly correlated across adolescent subgroups (Pearson’s r=0.33–0.96; Spearman’s r=0.42–0.96), but across behaviors, only F&V consumption and healthy weight were correlated (Pearson’s r=0.34; Spearman’s r=0.37). Adolescents in all states could benefit from initiatives to support cancer prevention behaviors, especially physical activity and F&V consumption. Programs in states that ranked highly on all assessed health behaviors could be adapted for dissemination in lower-performing states.
Keywords: adolescent health, cancer prevention, geographic disparities, physical activity, fruit and vegetable consumption, healthy weight, nutrition, body mass index, overweight/obesity, energy balance
Health behaviors related to energy balance, including physical activity and dietary intake, contribute to undue morbidity and mortality.1,2 Several types of cancer have been linked to poor physical activity3 and diet (including low fruit and vegetable (F&V) consumption).4 Overweight and obesity are closely related to these health behaviors5 and also have been associated with increased cancer risk.6 These behaviors each cause 2–3% of all cancers diagnosed in high-income countries such as the United States.7
Healthy People 2020 sets objectives for these behaviors based on guidelines from public health organizations, but many people in the U.S., including adolescents, fail to reach these objectives.8 In 2015, for example, 16% of high school students were overweight and another 14% were obese.9 Health during adolescence sets a foundation for health trajectories throughout the lifetime.10,11 For example, BMI during childhood is positively correlated with BMI during adulthood.11 In addition, health behaviors during adolescence may confer independent risks for chronic disease beyond health behaviors during adulthood10,12, although this evidence is mixed.11
Adolescent physical activity, diet, and overweight/obesity vary not only by important sociodemographic factors such as sex and race/ethnicity9, but also by contextual factors such as social norms13 and the built environment.14 Striking differences in these behaviors have emerged across states.9,15 As noted above, nationally, 14% of high school students were obese in 2015, but this percentage ranged almost two-fold across states, from 10% in Montana to 19% in Mississippi.9
Comparing and ranking states on their performance on health indicators may motivate policies and programs to improve public health16,17, but often such ranks ignore error in estimates derived from survey data.18–20 This practice can lead to over-interpretation of ranks that do not differ statistically.19,21 Our study aimed to examine the percentages of cancer-preventing energy balance indicators among adolescents across states and to evaluate differences in their ranks, using several years of population-based data.
Materials and Methods
Data source
Data came from the Youth Risk Behavior Surveillance System (YRBSS), a biennial, school-based survey coordinated by the Centers for Disease Control and Prevention (CDC) to monitor adolescent health behaviors.22 YRBSS surveys representative samples of students in grades 9–12 in each state using a three-stage clustered sampling design.23 In states with ≥60% response rates, YRBSS staff produce survey weights to account for student non-response and to increase generalizability of the findings.23
The present study analyzed data from 531,777 respondents in the 2011, 2013, and 2015 YRBSS surveys to estimate state-specific percentages of adolescent energy balance behaviors. Forty-seven states completed a YRBSS survey with an adequate response rate during at least one of these years (see Supplementary Table S1 for sample sizes across years and subgroups).22
Measures
We measured adherence to behavioral guidelines8 about physical activity, F&V consumption, and weight status among adolescents. State YRBSS surveys used the items quoted below or slight variations.
Physical activity
The Physical Activity Guidelines for Americans from the U.S. Department of Health and Human Services (DHHS) recommend that adolescents engage in at least 60 minutes of aerobic physical activity per day.24 YRBSS survey items read: “During the past 7 days, on how many days were you physically active for a total of at least 60 minutes per day?”23 We coded respondents as meeting the guideline if they were active for at least 60 minutes during 7 of the past 7 days.
F&V consumption
The Dietary Guidelines for Americans, 2015–2020, from the U.S. DHHS recommend that adolescents eat at least two servings of fruits and three servings of vegetables every day.25 Six YRBSS survey items assessed F&V consumption; all items began with “During the past 7 days, how many times did you…” and finished with “drink 100% fruit juices such as orange juice, apple juice, or grape juice?,” “eat fruit?,” “eat green salad?,” “eat potatoes?,” “eat carrots?,” and “eat other vegetables?”23 YRBSS staff calculated the number of servings of fruits and vegetables respondents ate per day. We coded respondents as meeting the guideline if they consumed the recommended amount of fruits and vegetables.
Four states did not include comparable survey items on F&V consumption (Delaware, Hawaii, Maine, and New York); thus analyses of this outcome are restricted to 43 states.23
Weight status
The CDC recommends that adolescents maintain a normal weight, defined as below the 85th percentile of age- and sex-specific BMI.26 YRBSS respondents self-reported height and weight (biologically-implausible responses for height or weight were recoded to missing), and YRBSS staff calculated their BMI percentile.23 We coded respondents as meeting the guideline if they were below the 85th percentile of age- and sex-specific BMI.
Other variables
Respondents self-reported their sex (male; female; or missing). In addition, they self-reported their race and ethnicity, which YRBSS classified as non-Hispanic white, non-Hispanic black, Hispanic/Latino, other, or missing. Respondent state came from YRBSS records.
Statistical analysis
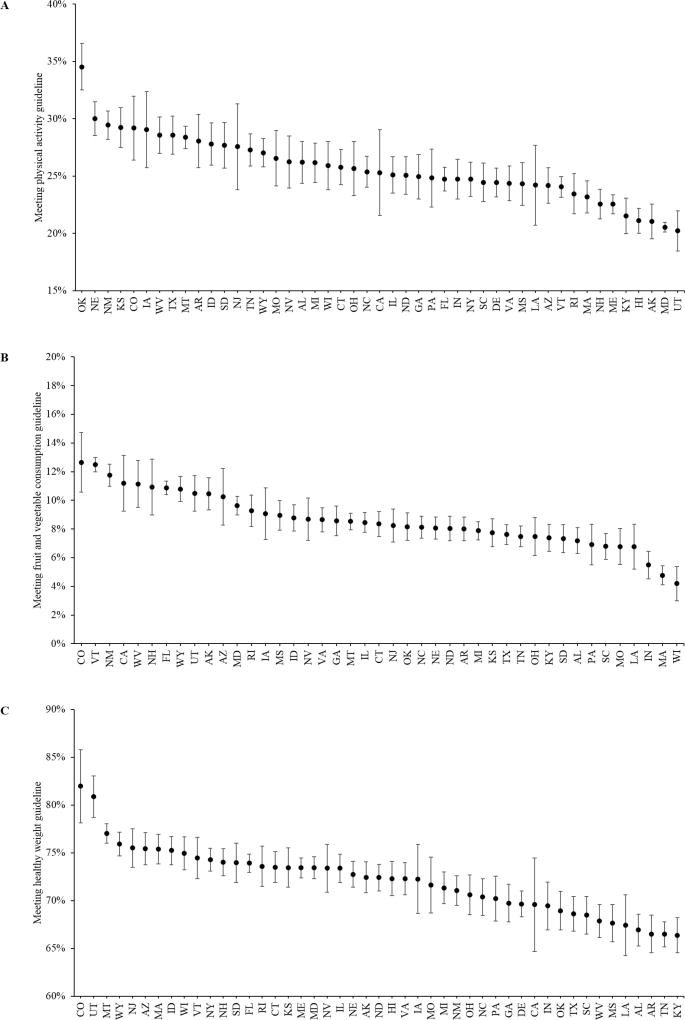
First, we calculated the percentage of respondents adhering to each of the guidelines described above for the overall population, by demographic subgroup, and by state. We used chi-squared tests to compare the percentages of adolescents meeting these guidelines across subgroups. Scatterplots depict the observed percentages and 95% confidence intervals (CI’s) for states’ adherence to each behavioral guideline. As a supplementary figure, we include choropleths to depict the states’ adherence levels.
Next, we ranked states according to their observed percentages and estimated the error around the ranks via a Monte Carlo method to generate simultaneous CI’s for each state’s rank for each indicator.19,27 This approach used 100,000 replications assuming a normal distribution of percentages across states. For each replication, we simulated the percentage of adolescents meeting each guideline in each state given the observed percentage and standard error. Then we ranked the states in each replication and calculated each state’s median rank and the 95% CI. We iteratively compared each state to all other states to examine their ranks. Scatterplots depict the ranks and associated CI’s for states’ adherence to each behavioral guideline. To gain further understanding of how these patterns vary by adolescent subgroups, we repeated these analyses stratifying by adolescent sex and by adolescent race/ethnicity.
Finally, we examined the consistency in percentages and ranks across subgroups and outcomes to estimate the similarity of these behaviors for different subgroups; marked differences in percentages and ranks could indicate states’ failure to address a given behavior for a given subgroup. We used Pearson’s correlation coefficients to measure the association between percentages and Spearman’s rank correlation coefficients to measure the association between ranks for the overall population compared to each of the subgroups (female; male; non-Hispanic white; non-Hispanic black; Hispanic/Latino; other race/ethnicity). In addition, for the overall population, we examined pairwise comparisons between physical activity, F&V consumption, and healthy weight guidelines; similarities in percentages and ranks could indicate a common cause underpinning engagement in these behaviors that could be examined in future research.
Sample weights were used to obtain population estimates that accounted for student nonresponse23, and design information was incorporated to calculate standard errors accounting for the complex survey design.20 Below, we present unweighted frequencies and weighted percentages. Analyses were conducted in SAS version 9.3 (Cary, NC) with an alpha value of .05.
Results
Across survey years, 531,777 adolescents participated in YRBSS. Of these, about half were female (48.8%) and half male (50.7%) (0.5% missing). More than half of participants were non-Hispanic white (52.5%), with smaller groups of non-Hispanic blacks (15.3%), Hispanics/Latinos (21.2%), or other race/ethnicity (8.5%) (2.5% missing).
Meeting the adolescent physical activity guideline
Altogether, 491,093 participants from 47 states reported their physical activity, and 25.8% (95% CI=25.2%–26.4%) of adolescents met this guideline (Table 1). Meeting this guideline was higher among males than females (χ2=16,568, p<.0001) and among non-Hispanic whites than other races/ethnicities (χ2=989, p<.0001).
Table 1.
Frequencies and percentages of adolescents meeting guidelines for physical activity, fruit and vegetable consumption, and healthy weight status, 2011–2015 Youth Risk Behavior Surveillance System.
| n | N | % | (95% CI) | p | |
|---|---|---|---|---|---|
| Physical activity | |||||
| Total | 118,167 | 491,093 | 25.8% | (25.2%–26.4%) | |
| Sex | |||||
| Female | 42,533 | 249,715 | 17.7% | (17.1%–18.3%) | |
| Male | 75,036 | 237,957 | 33.8% | (33.1%–34.6%) | <.0001 |
| Race/ethnicity | |||||
| Non-Hispanic white | 66,265 | 256,967 | 27.7% | (27.0%–28.4%) | |
| Non-Hispanic black | 12,887 | 60,859 | 23.6% | (22.7%–24.5%) | |
| Hispanic/Latino | 16,978 | 77,819 | 23.7% | (22.6%–24.7%) | |
| Other | 19,216 | 82,448 | 24.1% | (22.2%–26.0%) | <.0001 |
| Fruit and vegetable consumption | |||||
| Total | 37,809 | 488,149 | 8.0% | (7.6%–8.3%) | |
| Sex | |||||
| Female | 17,623 | 248,831 | 7.1% | (6.8%–7.5%) | |
| Male | 19,822 | 236,173 | 8.7% | (8.2%–9.1%) | <.0001 |
| Race/ethnicity | |||||
| Non-Hispanic white | 18,210 | 250,077 | 7.1% | (6.8%–7.4%) | |
| Non-Hispanic black | 4,650 | 64,463 | 8.2% | (7.7%–8.8%) | |
| Hispanic/Latino | 6,254 | 78,444 | 9.0% | (8.4%–9.7%) | |
| Other | 7,537 | 82,367 | 9.8% | (8.3%–11.4%) | <.0001 |
| Healthy weight status | |||||
| Total | 355,603 | 490,919 | 71.5% | (70.7%–72.3%) | |
| Sex | |||||
| Female | 188,033 | 248,691 | 74.8% | (74.1%–75.6%) | |
| Male | 167,570 | 242,228 | 68.3% | (67.2%–69.3%) | <.0001 |
| Race/ethnicity | |||||
| Non-Hispanic white | 194,365 | 257,731 | 75.0% | (74.4%–75.6%) | |
| Non-Hispanic black | 42,983 | 64,712 | 65.8% | (64.9%–66.7%) | |
| Hispanic/Latino | 52,572 | 77,613 | 65.1% | (63.6%–66.6%) | |
| Other | 58,179 | 80,264 | 76.1% | (73.3%–78.8%) | <.0001 |
Note. Frequencies are unweighted, and percentages are weighted. P-values indicate results of chi-square tests of independence of health behaviors for sex or race/ethnicity subgroups.
CI=confidence interval.
Across states, the percentage of adolescents meeting this guideline ranged from 20.2% (Utah) to 34.6% (Oklahoma) (Table 2, Figure 1A). Thus, Oklahoma was ranked first (1, 95% CI=1–1) and Utah last (47, 95% CI=43–47). The CI’s for the percentages and ranks of meeting the physical activity guideline overlapped for many states. For example, the CI for California’s rank, 25th (8–42; Supplementary Table S2), overlapped 33 other ranks.
Table 2.
Percentages of adolescents meeting guidelines for physical activity, fruit and vegetable consumption, and healthy weight status by state, 2011–2015 Youth Risk Behavior Surveillance System.
| State | Physical activity |
Fruit and vegetable consumption |
Healthy weight status |
|---|---|---|---|
| Alabama | 26.2% | 7.2% | 66.9% |
| Alaska | 21.1% | 10.5% | 72.4% |
| Arizona | 24.2% | 10.2% | 75.4% |
| Arkansas | 28.1% | 8.0% | 66.5% |
| California | 25.3% | 11.2% | 69.6% |
| Colorado | 29.2% | 12.6% | 82.0% |
| Connecticut | 25.8% | 8.4% | 73.5% |
| Delaware | 24.4% | -- | 69.6% |
| Florida | 24.7% | 10.9% | 73.9% |
| Georgia | 24.9% | 8.6% | 69.7% |
| Hawaii | 21.1% | -- | 72.3% |
| Idaho | 27.8% | 8.8% | 75.2% |
| Illinois | 25.1% | 8.5% | 73.4% |
| Indiana | 24.7% | 5.5% | 69.4% |
| Iowa | 29.1% | 9.1% | 72.3% |
| Kansas | 29.2% | 7.8% | 73.5% |
| Kentucky | 21.5% | 7.4% | 66.4% |
| Louisiana | 24.2% | 6.8% | 67.4% |
| Maine | 22.5% | -- | 73.4% |
| Maryland | 20.5% | 9.6% | 73.4% |
| Massachusetts | 23.2% | 4.8% | 75.4% |
| Michigan | 26.2% | 7.9% | 71.3% |
| Mississippi | 24.3% | 8.9% | 67.7% |
| Missouri | 26.6% | 6.8% | 71.6% |
| Montana | 28.4% | 8.5% | 77.0% |
| Nebraska | 30.0% | 8.1% | 72.8% |
| Nevada | 26.2% | 8.7% | 73.4% |
| New Hampshire | 22.6% | 10.9% | 74.0% |
| New Jersey | 27.6% | 8.2% | 75.5% |
| New Mexico | 29.4% | 11.8% | 71.1% |
| New York | 24.7% | -- | 74.3% |
| North Carolina | 25.4% | 8.1% | 70.4% |
| North Dakota | 25.1% | 8.0% | 72.4% |
| Ohio | 25.6% | 7.5% | 70.6% |
| Oklahoma | 34.6% | 8.2% | 68.9% |
| Pennsylvania | 24.8% | 6.9% | 70.2% |
| Rhode Island | 23.5% | 9.3% | 73.6% |
| South Carolina | 24.5% | 6.8% | 68.5% |
| South Dakota | 27.7% | 7.3% | 74.0% |
| Tennessee | 27.3% | 7.5% | 66.5% |
| Texas | 28.6% | 7.6% | 68.6% |
| Utah | 20.2% | 10.5% | 80.9% |
| Vermont | 24.1% | 12.5% | 74.5% |
| Virginia | 24.4% | 8.6% | 72.3% |
| West Virginia | 28.6% | 11.1% | 67.9% |
| Wisconsin | 25.9% | 4.2% | 75.0% |
| Wyoming | 27.0% | 10.8% | 75.9% |
Note. Percentages are weighted.
Figure 1.
State percentages of adolescents meeting guidelines for (A) physical activity, (B) fruit and vegetable consumption, and (C) healthy weight status, 2011–2015 Youth Risk Behavior Surveillance System.
In stratified analyses, states’ percentages and ranks for meeting physical activity guidelines across subgroups were fairly consistent. Percentages in the overall population were correlated with those observed in subgroups (females: r=0.84; males: r=0.93; non-Hispanic white: r=0.88; non-Hispanic black: r=0.54; Hispanic/Latino: r=0.62; other race/ethnicity: r=0.65; all p<.05). Similarly, ranks were correlated for the overall population versus subgroups (females: r=0.84; males: r=0.91; non-Hispanic white: r=0.88; non-Hispanic black: r=0.45; Hispanic/Latino: r=0.63; other race/ethnicity: r=0.63; all p<.05) (Supplementary Table S2). For example, Oklahoma was ranked in the top five states for meeting the physical activity guideline, and Utah in the bottom three, across most subgroups.
Meeting the adolescent F&V consumption guideline
Altogether, 488,149 participants from 43 states reported their F&V consumption, and 8.0% (95% CI=7.6%–8.3%) of adolescents met this guideline (Table 1). Meeting this guideline was higher among males than females (χ2=387, p<.0001) and varied by race/ethnicity (χ2=665, p<.0001).
Across states, the percentage of adolescents meeting this guideline ranged from 4.2% (Wisconsin) to 12.6% (Colorado) (Table 2, Figure 1B). Thus, Colorado was ranked first (1, 95% CI=1–8) and Wisconsin last (43, 95% CI=41–43). The CI’s for the percentages and ranks of meeting the F&V consumption guideline overlapped for many states. For example, the CI for Connecticut’s rank, 22nd (14–33; Supplementary Table S3), overlapped 18 others.
In stratified analyses, states’ percentages and ranks for meeting F&V consumption guidelines across adolescent subgroups were fairly consistent. Percentages in the overall population were highly correlated with those observed in subgroups (females: r=0.92; males: r=0.94; non-Hispanic white: r=0.95; non-Hispanic black: r=0.75; Hispanic/Latino: r=0.70; other race/ethnicity: r=0.67; all p<.05). Similarly, ranks were highly correlated for the overall population versus subgroups (females: r=0.90; males: r=0.92; non-Hispanic white: r=0.94; non- Hispanic black: r=0.59; Hispanic/Latino: r=0.68; other race/ethnicity: r=0.62; all p<.05) (Supplementary Table S3). For example, Colorado was ranked in the top four states for meeting the F&V consumption guideline, and Wisconsin in the bottom two, across most subgroups.
Meeting the adolescent healthy weight status guideline
Altogether, 490,919 participants from 47 states reported on their weight status, and 71.5% (95% CI=70.7%–72.3%) of adolescents met this guideline (Table 1). Meeting this guideline was higher among females than males (χ2=2,589, p<.0001) and varied by race/ethnicity (χ2=5,249, p<.0001).
Across states, the percentage of adolescents meeting this guideline ranged from 66.4% (Kentucky) to 82.0% (Colorado) (Table 2, Figure 1C). Thus, Colorado was ranked first (1, 95% CI=1–2) and Kentucky last (45, 95% CI=40–47; tied with two other states). The CI’s for the percentages and ranks of meeting the healthy weight guideline overlapped for many states. For example, the CI for North Dakota’s rank, 24th (15–30; Supplementary Table S4), overlapped 14 others.
In stratified analyses, states’ percentages and ranks for meeting healthy weight guidelines across adolescent subgroups were fairly consistent. Percentages in the overall population were correlated with those observed in subgroups (females: r=0.96; males: r=0.93; non-Hispanic white: r=0.84; non-Hispanic black: r=0.47; Hispanic/Latino: r=0.33; other race/ethnicity: r=0.53; all p<.05). Similarly, ranks were correlated for the overall population versus subgroups (females: r=0.96; males: r=0.92; non-Hispanic white: r=0.82; non-Hispanic black: r=0.53; Hispanic/Latino: r=0.42; other race/ethnicity: r=0.50; all p<.05) (Supplementary Table S4). For example, Colorado was ranked in the top two states for meeting the healthy weight guideline, and Kentucky in the bottom seven, across most subgroups.
Across behavioral indicators, states’ percentages and ranks were not highly correlated. States that had high percentages for the F&V consumption guideline tended to also have high percentages for the healthy weight guideline (r=0.34), but the associations were smaller for the physical activity and F&V consumption guidelines (r=−0.02) and for the physical activity and healthy weight guidelines (r=−0.09). Similarly, states that were ranked highly for F&V consumption tended to also rank highly for healthy weight (r=0.37), but the associations were smaller for physical activity and F&V consumption (r=−0.06) and for physical activity and healthy weight (r=−0.07).
Conclusions
Among more than half a million adolescents, we found considerable statistical overlap in states’ percentages and ranks of meeting guidelines for cancer prevention behaviors (physical activity, F&V consumption, and weight status). Overall, meeting guidelines for physical activity and F&V consumption was rare, but meeting healthy weight guidelines was more common. While ranking states on these indicators may galvanize public health action around a particular prevention behavior16,17, statistically, many states had equivalent ranks. Ranking smaller geographic areas (e.g., counties) with correspondingly smaller population and survey sample sizes would be prone to even more uncertainty. Rankings for each behavior were similar for the overall population and subgroups defined by sex; lower (but still statistically-significant) correlations observed for the overall population and subgroups defined by race/ethnicity could be explained by the smaller sample sizes. Additional research is needed to examine potential differences in adolescent cancer prevention behaviors across states to support interventions to improve these patterns.
These findings indicate that adolescents in all states would benefit from interventions to promote cancer prevention behaviors. States’ percentages and ranks for meeting guidelines were correlated only for F&V consumption and healthy weight. Some state-level conditions may similarly underpin these two behaviors (and therefore interventions may be able to target both simultaneously), but independent interventions may be needed for other adolescent health behaviors. Notably, Colorado was ranked first overall for F&V consumption and healthy weight, and sixth for physical activity. Future research should explore (1) the reliability of inter-state rankings on these health behaviors and (2) the characteristics of states with especially high performance on all three adolescent health indicators to understand which policies or programs can be implemented in other states.
However, at least four study limitations should be acknowledged when interpreting these findings. First, several states (and Washington, D.C.) were absent from this analysis.23 The consequence is that the range of ranks did not extend to 50 or 51, and none of the states can be designated as “best” or “worst,” even if they had the best or worst performance in this dataset. Second, due to differences in YRBSS sampling schemes and the availability of data, state sample sizes were quite variable and not necessarily what one would expect based on population.22 If sampling procedures had been identical across states, the CI’s would have been different, perhaps resulting in more precision and less overlap around states’ percentages and ranks; the influence of sample size on the width of the CI’s and, as a result, conclusions about statistical differences is crucial. However, in the current analysis states had samples between 1,125 and 112,301 participants, affording a great deal of precision (even among states with relatively small samples). However, the sample sizes for the supplementary analyses of adolescent subgroups were necessarily smaller, resulting in some instability in the estimates; caution should be used in interpreting these findings, particularly for non-Hispanic blacks. Third, YRBSS is cross-sectional and relies on self-reported data; biases in survey data are well-recognized.28 In particular, adolescents’ self-reported weight may be underestimated while self-reported height may be overestimated.29 Fourth, state-level estimates of percentages and ranks of adolescents engaging in these behaviors do not account for other individual- and area-level correlates of physical activity, F&V consumption, and healthy weight status; analyzing the influence of these correlates (and other excluded variables) was outside the scope of the current analysis.
Despite these limitations, this study has several strengths. Analyzing YRBSS data allowed us to examine behaviors among more than half a million adolescents. Samples of adolescents were representative of the populations in their respective states. We conducted rigorous statistical analysis of the error in states’ ranks; ranks are often presented as error-free (i.e., without confidence intervals), which could bias their interpretation.18,19 Finally, we evaluated adolescents’ behaviors in reference to nationally-established guidelines that promote public health.8,24–26
Overall, only a quarter of adolescents met the guideline for physical activity24, with higher levels among males than females (+15% points) and non-Hispanic whites than the other races/ethnicities (+4% points). These differences could reflect differential self-efficacy, beliefs, and attitudes about physical activity (by sex)30 or differential access to parks and recreational facilities (by race/ethnicity).30,31 At the state level, states in the middle part of the country (e.g., Oklahoma, Nebraska, New Mexico, Kansas, and Colorado; Supplementary Figure S1) had particularly high percentages of meeting the guideline (all >29%). States with especially low percentages were more dispersed. Differences across states may reflect variations in the natural and built environments14,32 or school policies33, and states with low adolescent physical activity may benefit from additional efforts to promote this behavior, such as school-based programming.34
Less than one-tenth of adolescents met the F&V consumption guideline, with slightly higher levels among males than females (+2% points) and minority racial/ethnic groups than non-Hispanic whites (+1–3% points). Previous studies have had mixed findings regarding differences in adolescent F&V consumption by sex and race/ethnicity, although the differences observed in the current study are quite small.35 At the state level, meeting this guideline ranged threefold from 4.2% to 12.6% (Supplementary Figure S1). State differences in this behavior could be attributable to differences in access to healthy foods35 and to school policies.36 Some of the states that performed poorly in the overall population had higher ranks for select subgroups (e.g., Louisiana ranked 38th overall but 5th for Hispanics/Latinos). These states may have characteristics or programs that are particularly supportive of F&V consumption among different adolescent subgroups.
Finally, almost two-thirds of adolescents met the healthy weight guideline, with higher levels among females than males (+7% points) and non-Hispanic whites and other races/ethnicities than non-Hispanic blacks and Hispanics/Latinos (+9–11% points). Differences in healthy weight by adolescent sex or race/ethnicity could reflect biases in self-reporting37 or maturational processes.38 At the state level, distinct clusters emerged of the highest-performing states (e.g., Colorado, Utah, Montana, and Wyoming, all ≥76%) and lowest-performing states (e.g., Kentucky, Tennessee, Arkansas, Alabama, and Louisiana, all <68%) (Supplementary Figure S1). As noted above, states’ performance on the healthy weight guideline was correlated with their performance on the F&V consumption guideline. Thus, geographic differences in healthy weight status may be driven by differences in F&V consumption and by factors such as the social environment.39
In conclusion, meeting the guidelines for adolescent physical activity and F&V consumption was relatively rare, although meeting the guideline for healthy weight was relatively common. However, the CI’s around many states’ percentages and ranks overlapped, indicating that they were statistically equivalent. The ranks were fairly consistent across adolescent sex or race/ethnicity, suggesting that the factors underpinning whether adolescents met these guidelines operated similarly across subgroups. Considerable room for improvement exists for (1) surveillance surveys, in terms of increasing overall sample sizes (and precision) and ensuring equivalence of procedures across sampling locations and, (2) cancer prevention efforts among all adolescents in all states, especially in promoting physical activity and F&V consumption. More research is needed on geographic differences in adolescent behaviors related to cancer prevention. A potentially promising next step is to adapt programs or policies in states with high ranks for all three health behaviors (e.g., Colorado) for implementation in states with low ranks to improve preventive health behaviors.
Supplementary Material
Supplementary Table S1. State sample sizes overall, by year, and by demographic subgroup, 2011–2015 Youth Risk Behavior Surveillance System.
Supplementary Table S2. State ranks and 95% confidence intervals for meeting physical activity guidelines, overall and stratified across demographic subgroups, 2011–2015 Youth Risk Behavior Surveillance System.
Supplementary Table S3. State ranks and 95% confidence intervals for meeting fruit and vegetable consumption guidelines, overall and stratified across demographic subgroups, 2011–2015 Youth Risk Behavior Surveillance System.
Supplementary Table S4. State ranks and 95% confidence intervals for meeting healthy weight status guidelines, overall and stratified across demographic subgroups, 2011–2015 Youth Risk Behavior Surveillance System.
Supplementary Figure S1. State percentages of adolescents meeting guidelines for (A) physical activity, (B) fruit and vegetable (F&V) consumption, and (C) healthy weight status.
Highlights.
Ranking states’ performance on adolescent cancer prevention can motivate change.
The prevalence of meeting some weight-related guidelines among adolescents was low.
States’ performance ranks varied across indicators and had considerable error.
States’ ranks for fruit/vegetable consumption and healthy weight were correlated.
Precise ranks could inform research and states’ policies for cancer prevention.
Acknowledgments
Funding source: This research was conducted as part of active duty at the National Cancer Institute. The National Cancer Institute was not involved in the study design; collection, analysis, and interpretation of data; writing of the report; or decision to submit the manuscript for submission.
The authors wish to acknowledge the assistance of the CDC and the state health agencies that conducted the YRBSS surveys and shared their data. This manuscript was prepared or accomplished by the authors in their personal capacity. The opinions expressed in this article are the authors’ own and do not reflect the view of the National Institutes of Health, the Department of Health and Human Services, or the United States government.
Abbreviations
- BMI
body mass index
- CDC
Centers for Disease Control and Prevention
- CI
confidence interval
- DHHS
Department of Health and Human Services
- F&V
fruit and vegetable
- YRBSS
Youth Risk Behavior Surveillance System.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflicts of interest: The authors have no potential conflicts of interest to disclose.
References
- 1.Mokdad AH, Marks JS, Stroup DF, Gerberding JL. Actual causes of death in the United States, 2000. JAMA. 2004;291(10):1238–1245. doi: 10.1001/jama.291.10.1238. [DOI] [PubMed] [Google Scholar]
- 2.Bauer UE, Briss PA, Goodman RA, Bowman BA. Prevention of chronic disease in the 21st century: Elimination of the leading preventable causes of premature death and disability in the USA. The Lancet. 2014;384(9937):45–52. doi: 10.1016/S0140-6736(14)60648-6. [DOI] [PubMed] [Google Scholar]
- 3.Moore SC, Lee I, Weiderpass E, et al. Association of leisure-time physical activity with risk of 26 types of cancer in 1.44 million adults. JAMA internal medicine. 2016;176(6):816–825. doi: 10.1001/jamainternmed.2016.1548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Marmot M, Atinmo T, Byers T, et al. Food, nutrition, physical activity, and the prevention of cancer: A global perspective. 2007 http://www.aicr.org/assets/docs/pdf/reports/Second_Expert_Report.pdf.
- 5.Sallis JF, Glanz K. Physical activity and food environments: Solutions to the obesity epidemic. Milbank Q. 2009;87(1):123–154. doi: 10.1111/j.1468-0009.2009.00550.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Calle EE, Kaaks R. Overweight, obesity and cancer: Epidemiological evidence and proposed mechanisms. Nature Reviews Cancer. 2004;4(8):579–591. doi: 10.1038/nrc1408. [DOI] [PubMed] [Google Scholar]
- 7.Danaei G, Vander Hoorn S, Lopez AD, Murray CJ, Ezzati M. Comparative Risk Assessment collaborating group (Cancers. Causes of cancer in the world: Comparative risk assessment of nine behavioural and environmental risk factors. The Lancet. 2005;366(9499):1784–1793. doi: 10.1016/S0140-6736(05)67725-2. [DOI] [PubMed] [Google Scholar]
- 8.U. S. Department of Health and Human Services. Healthy people 2020 cancer objectives. http://www.healthypeople.gov/2020/topicsobjectives2020/objectiveslist.aspx?topicid=5. Updated 2016.
- 9.Centers for Disease Control and Prevention (CDC) Adolescent obesity prevalence: Trends over time. http://www.cdc.gov/healthyschools/obesity/obesity-youth.htm. Updated 2016.
- 10.Fuemmeler BF, Pendzich MK, Tercyak KP. Weight, dietary behavior, and physical activity in childhood and adolescence: Implications for adult cancer risk. Obes Facts. 2009;2(3):179–186. doi: 10.1159/000220605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wright CM, Parker L, Lamont D, Craft AW. Implications of childhood obesity for adult health: Findings from thousand families cohort study. BMJ. 2001;323(7324):1280–1284. doi: 10.1136/bmj.323.7324.1280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Must A, Jacques PF, Dallal GE, Bajema CJ, Dietz WH. Long-term morbidity and mortality of overweight adolescents: A follow-up of the Harvard growth study of 1922 to 1935. N Engl J Med. 1992;327(19):1350–1355. doi: 10.1056/NEJM199211053271904. [DOI] [PubMed] [Google Scholar]
- 13.Koehly LM, Loscalzo A. Adolescent obesity and social networks. Prev Chronic Dis. 2009;6(3):A99. doi: A99. [PMC free article] [PubMed] [Google Scholar]
- 14.Papas MA, Alberg AJ, Ewing R, Helzlsouer KJ, Gary TL, Klassen AC. The built environment and obesity. Epidemiol Rev. 2007;29:129–143. doi: 10.1093/epirev/mxm009. doi: mxm009. [DOI] [PubMed] [Google Scholar]
- 15.Kramer MR, Raskind IG, Van Dyke ME, Matthews SA, Cook-Smith JN. Geography of adolescent obesity in the US, 2007− 2011. Am J Prev Med. 2016;51(6):898–909. doi: 10.1016/j.amepre.2016.06.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Peppard PE, Kindig DA, Dranger E, Jovaag A, Remington PL. Ranking community health status to stimulate discussion of local public health issues: The Wisconsin county health rankings. Am J Public Health. 2008;98(2):209–212. doi: 10.2105/AJPH.2006.092981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Oliver TR. Population health rankings as policy indicators and performance measures. Prev Chronic Dis. 2010;7(5):A101. doi: A101. [PMC free article] [PubMed] [Google Scholar]
- 18.Gerzoff RB, Williamson GD. Who's number one? the impact of variability on rankings based on public health indicators. Public Health Rep. 2001;116(2):158–164. doi: 10.1016/S0033-3549(04)50007-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Zhang S, Luo J, Zhu L, et al. Confidence intervals for ranks of age-adjusted rates across states or counties. Stat Med. 2014;33(11):1853–1866. doi: 10.1002/sim.6071. [DOI] [PubMed] [Google Scholar]
- 20.Wolter K. Introduction to variance estimation. Springer Science & Business Media; 2007. [Google Scholar]
- 21.Arndt S, Acion L, Caspers K, Blood P. How reliable are county and regional health rankings? Prev Sci. 2013;14(5):497–502. doi: 10.1007/s11121-012-0320-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Centers for Disease Control and Prevention (CDC) Youth risk behavior surveillance system (YRBSS) overview. http://www.cdc.gov/healthyyouth/data/yrbs/overview.htm. Updated 2016.
- 23.Centers for Disease Control and Prevention (CDC) 2015 YRBS data user’s guide. https://www.cdc.gov/healthyyouth/data/yrbs/pdf/2015/2015_yrbs-data-users-guide.pdf. Updated 2016.
- 24.Department of Health and Human Services. Physical activity guidelines for Americans: Active children and adolescents. https://health.gov/paguidelines/guidelines/chapter3.aspx. Updated 2016.
- 25.Department of Health and Human Services. Dietary guidelines for Americans, 2015–2020. 2015 https://health.gov/dietaryguidelines/2015/guidelines/
- 26.Centers for Disease Control and Prevention (CDC) About child & teen BMI. http://www.cdc.gov/healthyweight/assessing/bmi/childrens_bmi/about_childrens_bmi.html. Updated 2015.
- 27.Wright T, Klein M, Wieczorek J. Ranking populations based on sample survey data. Research Report Series. 2014 #2014-12. [Google Scholar]
- 28.Groves RM. Nonresponse rates and nonresponse bias in household surveys. Public Opin Q. 2006;70(5):646–675. [Google Scholar]
- 29.Elgar FJ, Roberts C, Tudor-Smith C, Moore L. Validity of self-reported height and weight and predictors of bias in adolescents. Journal of Adolescent Health. 2005;37(5):371–375. doi: 10.1016/j.jadohealth.2004.07.014. [DOI] [PubMed] [Google Scholar]
- 30.Sallis JF, Zakarian JM, Hovell MF, Hofstetter CR. Ethnic, socioeconomic, and sex differences in physical activity among adolescents. J Clin Epidemiol. 1996;49(2):125–134. doi: 10.1016/0895-4356(95)00514-5. [DOI] [PubMed] [Google Scholar]
- 31.Gordon-Larsen P, McMurray RG, Popkin BM. Determinants of adolescent physical activity and inactivity patterns. Pediatrics. 2000;105(6):E83. doi: 10.1542/peds.105.6.e83. [DOI] [PubMed] [Google Scholar]
- 32.Gordon-Larsen P, Nelson MC, Page P, Popkin BM. Inequality in the built environment underlies key health disparities in physical activity and obesity. Pediatrics. 2006;117(2):417–424. doi: 10.1542/peds.2005-0058. doi: 117/2/417. [DOI] [PubMed] [Google Scholar]
- 33.Story M, Nanney MS, Schwartz MB. Schools and obesity prevention: Creating school environments and policies to promote healthy eating and physical activity. Milbank Q. 2009;87(1):71–100. doi: 10.1111/j.1468-0009.2009.00548.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.van Sluijs EM, McMinn AM, Griffin SJ. Effectiveness of interventions to promote physical activity in children and adolescents: Systematic review of controlled trials. BMJ. 2007;335(7622):703. doi: 10.1136/bmj.39320.843947.BE. doi: bmj.39320.843947.BE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Rasmussen M, Krølner R, Klepp K, et al. Determinants of fruit and vegetable consumption among children and adolescents: A review of the literature. part I: Quantitative studies. International Journal of Behavioral Nutrition and Physical Activity. 2006;3(1):1. doi: 10.1186/1479-5868-3-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Chriqui JF, Pickel M, Story M. Influence of school competitive food and beverage policies on obesity, consumption, and availability: A systematic review. JAMA pediatrics. 2014;168(3):279–286. doi: 10.1001/jamapediatrics.2013.4457. [DOI] [PubMed] [Google Scholar]
- 37.Sherry B, Jefferds ME, Grummer-Strawn LM. Accuracy of adolescent self-report of height and weight in assessing overweight status: A literature review. Arch Pediatr Adolesc Med. 2007;161(12):1154–1161. doi: 10.1001/archpedi.161.12.1154. [DOI] [PubMed] [Google Scholar]
- 38.Wang Y. Is obesity associated with early sexual maturation? A comparison of the association in american boys versus girls. Pediatrics. 2002;110(5):903–910. doi: 10.1542/peds.110.5.903. [DOI] [PubMed] [Google Scholar]
- 39.Singh GK, Kogan MD, van Dyck PC. A multilevel analysis of state and regional disparities in childhood and adolescent obesity in the United States. J Community Health. 2008;33(2):90–102. doi: 10.1007/s10900-007-9071-7. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Table S1. State sample sizes overall, by year, and by demographic subgroup, 2011–2015 Youth Risk Behavior Surveillance System.
Supplementary Table S2. State ranks and 95% confidence intervals for meeting physical activity guidelines, overall and stratified across demographic subgroups, 2011–2015 Youth Risk Behavior Surveillance System.
Supplementary Table S3. State ranks and 95% confidence intervals for meeting fruit and vegetable consumption guidelines, overall and stratified across demographic subgroups, 2011–2015 Youth Risk Behavior Surveillance System.
Supplementary Table S4. State ranks and 95% confidence intervals for meeting healthy weight status guidelines, overall and stratified across demographic subgroups, 2011–2015 Youth Risk Behavior Surveillance System.
Supplementary Figure S1. State percentages of adolescents meeting guidelines for (A) physical activity, (B) fruit and vegetable (F&V) consumption, and (C) healthy weight status.