Abstract
The Marine Resiliency Study-II examined changes in symptomatology across a deployment cycle to Afghanistan. U.S. Servicemembers (N = 1041) received clinical testing at two time points either bracketing a deployment (855) or not (186). Factor analyses were used to generate summary and change scores from Time 1 to Time 2. A between-subject design was used to examine changes across the deployment cycle with deployment (low-trauma, high-trauma, and non-deployed) and social support (low vs. high) as the grouping variables. Insomnia increased post-deployment regardless of deployment trauma (std. effect for high-trauma and low-trauma = 0.39 and 0.26, respectively). Only the high-trauma group showed increased PTSD symptoms and non-perspective-taking (std. effect = 0.40 and 0.30, respectively), while low-trauma showed decreased anxiety symptoms after deployment (std. effect = −0.17). These associations also depend on social support, with std. effects ranging from −0.22 to 0.51. When the groups were compared, the high-trauma deployed group showed significantly worse PTSD and non-perspective-taking than all other groups. Similar to studies in other military divisions, increased clinical symptoms were associated with high deployment stress in active duty Servicemembers, and social support shows promise as a moderator of said association.
Keywords: Marine Resiliency Study 2, Posttraumatic Stress Disorder, Computerized Neurocognitive Battery, Psychometrics, Social Support
The importance of US Servicemembers’ mental health has become increasingly apparent with the recent rise in suicide rates, reported post-traumatic stress disorder (PTSD) symptoms, and other psychopathologies (Hoge et al., 2006; Hoge et al., 2004; Kang et al., 2003; Prigerson et al., 2002; Ramchand et al., 2015). For example, in a large sample of active duty and reserve Servicemembers returning from Iraq in 2005–2006 (n = 88,235), 17–35% were determined to have a mental health risk, defined as endorsement of low-threshold levels of depression, PTSD, suicide ideation, interpersonal conflict, or aggressive ideation depending on the instrument used (Milliken et al., 2007). Examination of individual mental illnesses paints largely the same picture; in a sample of 1032 men returning from Iraq and Afghanistan, 33%, 39%, and 62% screened positive for PTSD, depression, and pain, respectively (Haskell et al., 2010). Lapierre, Schwegler, & LaBauve (2007) report similar numbers, with 44% of 4,089 soldiers returning from Iraq and Afghanistan reporting clinically significant levels of depression, PTSD, or both.
A primary approach to understanding mental health costs of combat deployment has been to document the prevalence or incidence of post-deployment psychiatric disorders. However, several researchers pursue a more detailed understanding of combat sequelae by examining phenomena such as symptom clusters embedded within psychiatric disorders, or trans-diagnostic symptom clusters that help understand comorbidities and tailor therapeutic interventions. To our knowledge, no study has examined symptom level data using a large combat deployed cohort assessed longitudinally on a diverse battery of psychiatric and psychosocial measures. Here we provide such data from a large deployed cohort, stratified by level of combat intensity and social support. The latter are considered key covariates when analyzing post-deployment outcomes. Combat exposure is known to predict PTSD, and in cross sectional research social support moderated (and perhaps mediated) effects of combat intensity on PTSD severity after deployment (Dirkzwager et al., 2003; Fontana et al., 1997; Han et al., 2014; Kaspersen and Matthiesen, 2003; King et al., 1998; Pietrzak et al., 2009; Polusny et al., 2011; Schnurr et al., 2004; Solomon et al., 1988). However, a recent longitudinal study suggests that social support perception changes post-trauma in relation to PTSD severity, and that social support does not influence subsequent PTSD symptoms (Nickerson et al., 2016). The combat intensity and social support data used were subscales of the Deployment Risk and Resilience Inventory (DRRI) (Vogt et al., 2013; Vogt et al., 2008).
We examined the overall change in mental health in Servicemembers deployed to Afghanistan between 2011–2013. The goal was to present unified overarching “profiles” of U.S. Servicemembers who were not deployed, deployed with low trauma exposure, or deployed with high trauma exposure. We distinguished among clinical associations stratified by, 1) deployment, 2) trauma, 3) military service with neither deployment nor trauma, and 4) perceived social support at follow-up. We have two hypotheses. First, trauma events produce changes in perception, biology, and behavior, predicting that traumatic deployment will be associated with negative outcomes across clinical dimensions, especially those related to dysregulated arousal (PTSD, anxiety, and insomnia) and interpersonal relationships (lack of perspective-taking). Second, the well-documented tendency of social support to abate negative trauma-related outcomes predicts that negative outcomes will be less severe among those who perceive strong social support upon returning from deployment.
Methods
Participants
The participants in MRS-II have been described in depth previously (Acheson et al., 2015). Briefly, 1444 U.S. Servicemembers (3 battalions; mean age = 21.9 ± 2.7 years, range 18 to 43) were assessed before and after a 7-months deployment to Afghanistan. Two battalions were assessed 1–2 weeks pre-deployment and 4–6 months post-deployment. To control for deployment effects, a third battalion was assessed at the same time points but was not deployed in the interim. Out of 1444 total infantry participating in the study, 1387 had valid measures at pre-deployment (deployed = 1192, not-deployed = 195) and 1033 had valid measures at post-deployment (deployed = 871, not-deployed = 162). There were no exclusion criteria beyond what is enforced by the U.S. Marine Corps upon joining the Service. The institutional review boards of the University of California San Diego and the University of Pennsylvania, VA San Diego Research Service, and Naval Health Research Center approved the study. Written informed consent was obtained from all participants.
Supplementary Table S1 shows the demographic sample characteristics, separated by deployment group. Groups differ significantly on only three characteristics. Years spent in the Marines thus far for the non-deployed (ND) group was significantly lower than that for the low-trauma (DLT) and high-trauma (DHT) deployed groups (|t| = 3.49 and 3.33, respectively; p < 0.005 for both). The proportion who had been on a previous operational deployment in the ND group was significantly higher than that for the DLT and DHT groups (χ2(1) = 43.6 and 41.4, respectively; p < 0.005). The effects mean that the ND group has spent longer in the military, during which time they were often deployed. Finally, the proportion who reported being a current cigarette smoker in the DLT group was significantly higher than that for the ND and DHT groups (χ2(1) = 6.3 and 3.9, respectively; p < 0.05 for both). This effect was examined to allow comparison of our sample with that of Vasterling et al. (2006).
Measures
Measures were collected using well-established instruments. Because factor analyses were performed at the item-level (see below), items from a scale designed to measure one construct were “allowed” to contribute (often solely) to a different construct if indicated by the analysis. Supplementary Table S2 shows the item text of these scales, and Supplementary Table S3 shows their means and standard deviations. The scales included: Clinician Administered PTSD Scale (CAPS) (Blake et al., 1995); PTSD Checklist (PCL) (Weathers et al., 1993); Beck Depression Inventory 2 (BDI) (Beck et al., 1996); Beck Anxiety Inventory (BAI) (Beck et al., 1993); Alcohol Use Disorders Identification Test (AUDIT) (Saunders et al., 1993); SF-12 Health Survey (Ware et al., 1996); Interpersonal Reactivity Index (IRI) (Davis, 1980, 1983); Army STARRS New Soldier Study Sleep Scale (NSSS) (Kessler et al., 2013; Ursano et al., 2014), and Deployment Risk and Resilience Inventory-2 (DRRI) (Vogt et al., 2013). Due to research goals of the workgroups who designed MRS-II, only one sub-scale of the IRI was collected: perspective-taking. This was because empathic processes have both cognitive (perspective-taking) and affective components (Davis, 1980, 1983), and social cognition was the primary research interest, more so than affect. Perspective-taking is foundational—i.e. if the cognitive stage of empathic responding is erroneous, subsequent affective responses are also impaired, and because perspective-taking is foundational, its assessment is suggestive regarding overall empathic tendencies as well as specific perspective-taking skills. One sees this empirically, in that perspective-taking is consistently shown to be correlated with all other subscales of the IRI and loads highly on IRI hierarchical factors (Pulos et al., 2004). Finally, one relevant question about perspective-taking in this context is, how much does it differ from social support, one of the primary independent variables used in this study. The correlation between perspective-taking and social support in the present sample is −0.21, suggesting that they are mostly unique phenomena. The Supplement contains further description of these measures, and to allow comparison with previous and subsequent studies, Table 1 contains the means and standard deviations of the raw scores of all scales used here.
Table 1.
Mean Raw Score (and SD) for all Clinical and DRRI Scales Used, for Full Sample and by Deployment Category
| Full Sample | Baseline (Time Point = 1) | Full Sample | Follow-up (Time Point = 2) | |||||
|---|---|---|---|---|---|---|---|---|
| By Deployment Status | By Deployment Status | |||||||
| Deployed (High-Trauma) | Deployed (Low-Trauma) | Not Deployed | Deployed (High-Trauma) | Deployed (Low-Trauma) | Not Deployed | |||
| CAPS Total | 13.39 (13.97) | 12.61 (13.38) | 12.68 (13.52) | 14.61 (14.71) | 16.05 (16.61) | 19.34 (17.63) | 13.32 (15.27) | 15.72 (16.35) |
| PCL | 22.46 (8.43) | 21.82 (7.77) | 22.10 (8.11) | 23.26 (9.10) | 23.94 (9.44) | 25.75 (9.96) | 22.57 (8.73) | 23.46 (9.36) |
| IRI | 15.99 (5.29) | 15.92 (5.20) | 15.92 (5.20) | 16.10 (5.43) | 15.53 (5.51) | 14.89 (5.37) | 15.97 (5.53) | 15.82 (5.65) |
| BDI | 5.66 (6.59) | 5.33 (6.16) | 5.40 (6.32) | 6.15 (7.09) | 5.19 (6.70) | 5.60 (6.61) | 4.55 (6.38) | 5.88 (7.50) |
| BAI | 4.49 (6.26) | 4.67 (6.66) | 4.27 (5.77) | 4.55 (6.37) | 3.73 (6.39) | 4.42 (7.36) | 2.87 (5.45) | 4.35 (6.08) |
| SF12 (Physical) | 54.46 (6.04) | 54.44 (5.66) | 54.96 (5.64) | 54.04 (6.61) | 52.96 (7.29) | 52.50 (7.64) | 53.13 (7.04) | 53.52 (7.14) |
| SF12 (Mental) | 50.25 (9.27) | 50.91 (8.63) | 50.25 (9.07) | 49.73 (9.88) | 50.43 (9.28) | 50.10 (9.11) | 51.16 (9.09) | 49.36 (9.98) |
| AUDIT | 7.27 (5.64) | 7.80 (6.01) | 6.24 (5.38) | 7.76 (5.47) | 6.67 (5.25) | 7.38 (5.63) | 5.82 (4.78) | 7.23 (5.24) |
| Insomnia† | 2.11 (4.60) | 2.11 (4.68) | 1.71 (4.13) | 2.45 (4.91) | 2.95 (4.83) | 3.63 (5.12) | 2.46 (4.52) | 2.67 (4.80) |
| PTSD Criteria Met | 4.52% | 2.78% | 5.70% | 4.81% | 4.30% | 6.27% | 2.18% | 5.29% |
| DRRI CES‡ | 13.14 (8.99) | 20.67 (7.07) | 6.50 (3.72) | |||||
| DRRI GPDS‡ | 54.26 (9.54) | 53.90 (9.07) | 54.56 (9.94) | |||||
Note. SD = standard deviation; CAPS = Clinician Administered PTSD Scale; PCL = PTSD Checklist; IRI = Interpersonal Reactivity Index; BDI = Beck Depression Inventory; BAI = Beck Anxiety Inventory; SF12 = SF-12 Health Survey; AUDIT = Alcohol Use Disorders Identification Test; DRRI = Deployment Risk and Resiliency Inventory-2; CES = Combat Experience Scale; GPDS = General Post-Deployment Support;
there is no standard insomnia total score for this scale, so the score listed is a sum of all NSSS items listed in Supplementary Table S2;
DRRI scale scores not available at baseline or for non-deployed servicemembers at follow-up.
One necessary step in the analysis process described below was to decide how best to utilize the myriad psychological measures (described above) administered to the Service Member cohort. Due to the large number of clinical scales, many of which measure similar pathologies and domains, we were presented with the problem of familywise error and possibly redundant results. As described below, our approach was to use exploratory factor analysis (EFA) (Kim et al., 1978) to reduce the data to latent dimensions, and as we demonstrate, this empirically driven approach yielded interpretable scores that are well-determined (see Grice, 2001).
Data Analysis
Missing data were confirmed missing completely at random (MCAR) using the MissMech package (Jamshidian et al., 2014) in R, and imputed using the Amelia package (Honaker et al., 2011) in R.
Factor analyses
We performed exploratory item factor analyses (itemwise EFAs) using the psych package in R. Because we did not necessarily expect simple-structure a priori, we used iterated-target rotation (Moore et al., 2015), which can detect complex structure. The number of factors was determined by examination of the scree plot. Because the clinical data were items1, the polychoric correlation matrix was analyzed, a common procedure in item factor analysis (Wirth and Edwards, 2007).
Based on the consistent clinical results, we opted to calculate factor scores (Thurstone, 1935) for these data. Itemwise EFAs were calculated separately for T1 and T2, and then to assure the scores at the two time points were on the same scale, we estimated a model to be used for both time points. This was done by rotating the T2 model to the T1 model using procrustean rotation (Browne, 1967; Schönemann, 1966), sometimes called target rotation (Browne, 2001). The process involves attempting to get one factor pattern matrix as close to another as possible, resulting in a pattern matrix that is “in between” the two pattern matrices. Here, it resulted in one model that could be used to calculate scores at both time points simultaneously, ensuring that they are on the same scale and can therefore be used for change scores.
To assess whether our target-rotated EFA model was invariant across the two time points, we performed confirmatory factor analyses (CFAs) in Mplus (Muthén and Muthén, 2012) where each item was assigned only to factors on which it loaded at least 0.25 in the EFA. First, the models for the two time points were estimated freely (no constraints). Then, the same models were estimated but with the added constraints that the factor loadings and thresholds be equal across the two time points. These two sets of models (constrained and unconstrained) were then compared using a χ2-difference test (DIFFTEST; see Muthén & Muthén, 2012, pp. 485–487).
Trauma and social support group assignment
Trauma was determined by a section of the DRRI that probes combat experiences during the last deployment—e.g., “I saw the bodies of dead Americans or allies.” Scores on this 19-item scale were split at the median (13) to categorize those who were deployed into “low” (N = 458; 53.4% of deployed) and “high” (N = 399; 46.6% of deployed) trauma. Note that this categorization is related purely to combat experiences and not to signs or symptoms of PTSD. Social support was measured by a section of the DRRI that probes post-deployment support from family and friends—e.g., “When I am ill, friends or family members will help out until I am well.” Scores on this 15-item scale were split at the median (55) to create two social support categories for deployed marines, low (N = 428) and high (N = 428). Marines who were not deployed (N = 186; 17.8% of total) were not administered the DRRI.
The above group-assignment resulted in three deployment groups [“Not Deployed”, “Deployed (Low-Trauma)”, and “Deployed (High-Trauma)”], which were then further broken down by social support category (“Strong Social Support” vs. “Weak Social Support”). This resulted in four social support groups: 1) High-Trauma with Strong Support (N = 196; 22.9% of deployed), 2) High-Trauma with Weak Support (N = 203; 23.7% of deployed), 3) Low-Trauma with Strong Support (N = 232; 27.1% of deployed), and 4) Low-Trauma with Weak Support (N = 225; 26.3% of deployed).
Mean comparisons
Change in clinical symptomatology (measured by the factor scores) was assessed using linear mixed models to account for both within- and between-subject effects. The independent variable of interest was time point, and the following were entered into the model as covariates: years in the military, history of TBI (yes/no; see below for definition), having been on a previous deployment before Time 1 (yes/no), and, to account for regression to the mean, T1 clinical score. Groups were then compared to each other using analysis of covariance (ANCOVA) where the dependent variables were change scores. To account for regression to the mean, T1 score was always included as a covariate, along with years in the military, history of TBI (yes/no), and having been on a previous deployment before Time 1 (yes/no). For significant ANCOVA results, post hoc t-tests were performed. Again, T1 clinical score, years in the military, history of TBI (yes/no), and having been on a previous deployment before Time 1 (yes/no) were all regressed out of all change scores before conducting t-tests.
All p-values were corrected for multiple comparisons using the Holm method (Holm, 1979). Due to the well-documented association of TBI with psychological outcomes (Hibbard et al., 1998; Hoofien et al., 2001; Rao and Lyketsos, 2000), analyses for clinical change were also performed on a sub-group of Marines who reported no TBI during deployment (and TBI was therefore not used as a covariate for these analyses). These results were then compared to the full-sample to examine any discrepancy. TBI was defined using the Department of Defense protocol for mild TBI/concussion—specifically, a head injury event accompanied by an alteration of consciousness and at least one of the following symptoms immediately after the injury event: feeling dazed or confused, experiencing loss of consciousness, or experiencing loss of memory of the injury event (Conaton et al., 2012). This reduced the N to 860, with 273 still remaining in the high-trauma group.
Results
Factor Analyses
Supplementary Table S4 shows the results of the EFA of 113 clinical items from the MRS. Factor 1 comprises items mostly from the BDI, CAPS, and SF12, and appears to represent anhedonic depression. The two highest loading items are BDI #4 (“I don’t enjoy things the way I used to.”) and #12 (“I am less interested in other people or things than before.”). Factor 2 comprises items mostly from the PCL and CAPS, and appears to represent PTSD. The two highest loading items are PCL #1 (“Repeated, disturbing memories, thoughts, or images of the event?”) and #5 (“Having physical reactions - e.g., heart pounding, trouble breathing, sweating - when something reminded you of the event?”). Factor 3 comprises items mostly from the BAI, and appears to represent anxiety. The two highest loading items are BAI #20 (“Face flushed”) and #3 (“Wobbliness in legs”). Factor 4 comprises items mostly from the NSSS, and appears to represent insomnia. The two highest loading items are NSSS #2 (“Have you had a whole month or longer when you had insomnia at least three nights a week?”) and #1 (“Have you ever had insomnia?”). Factor 5 is composed entirely of AUDIT items, and appears to represent alcohol use/abuse. The two highest loading items are AUDIT #8 (“How often during the last year have you been unable to remember what happened the night before because you had been drinking?”) and #3 (“How many times have you had 8 or more units of alcohol on a single occasion in the last year?”). Factor 6 is composed entirely of SF12 items, and appears to represent subjective physical and emotional health. The two highest loading items are SF12 #5 (“During the past 4 weeks, how much of the time were you limited in the kind of work or other regular activities as a result of your physical health?”) and #2 (“Does your health now limit you in moderate activities, such as moving a table, pushing a vacuum cleaner, bowling or playing golf?”). Finally, Factor 7 is composed entirely of IRI items, and appears to represent lack of perspective-taking, which we will call non-perspective-taking (NPT). The two highest loading items are IRI #6 (“When I’m upset at someone, I usually try to ‘put myself in his shoes’ for a while.”) and #3 (“I sometimes try to understand my friends better by imagining how things look from their perspective.”). To keep the IRI score in the negative direction (higher = worse), we multiplied it by negative one. That is, whereas a high score on the perspective-taking section of the IRI usually indicates a positive (good) outcome, a high score on our reversed IRI indicates a lack of perspective-taking. Supplementary Table S5 shows the means and standard deviations of the seven factors described above, separated by time point.
The test of measurement invariance across the two time points provided somewhat mixed results. When both T1 and T2 models were fit with the constraint that factor loadings be equal, joint-estimated model fit was good (comparative fit index = 0.93; RMSEA = 0.025 ± 0.001). However, when this model was compared to the model in which loading were freely estimated at the two time points, the less constrained model fit significantly better (Δχ2 = 253.5; Δdf = 136; p < 0.01). This suggests some violation of the measurement invariance assumption; however, note that factor scores used here were calculated from an EFA that was identical at the two time points.
Mean Comparisons
Table 2 shows the results of the linear mixed models, by deployment category and social support category. All T1-to-T2 effects are standardized such that they indicate standard deviations of change (positive or negative), controlling for covariates. Starting with deployment category, those who were deployed with high trauma showed significant and substantial increases in PTSD symptoms, insomnia, and NPT. Those who were deployed with low trauma showed significant increase in insomnia but significant improvement (decrease) in anxiety symptoms. Those who were not deployed showed no significant change from T1 to T2. When social support group is considered (last two columns of Table 2), the high-trauma/strong-support group showed significant increases in PTSD symptoms, insomnia, and NPT. The low-trauma/strong-support group showed significant improvement in anxiety and alcohol use. The high-trauma/weak-support group showed significant increases in PTSD symptoms, insomnia, and NPT. Finally, those in the low-trauma/weak-support group showed significant increases in insomnia and NPT. For convenient visualization of these effects, Supplementary Figures S1 and S2 show the mean raw change scores for the seven groups in Table 2, along with 95% confidence intervals.
Table 2.
Linear Mixed Model Results for MRS Clinical T1-to-T2 Change by Deployment Category and Social Support Category, with TBI History, Years in the Military, and Deployment History as Covariates.
| DV (change in) | Deployment category | Std. Effect | By social support | |
|---|---|---|---|---|
| Strong | Weak | |||
| Std. Effect | Std. Effect | |||
| Anhedonic depression | Deployed HT | −0.03 | −0.11 | 0.04 |
| PTSD | Deployed HT | 0.40*** | 0.28** | 0.51*** |
| Insomnia | Deployed HT | 0.39*** | 0.32** | 0.46*** |
| Physical health | Deployed HT | 0.12 | 0.00 | 0.25 |
| Anxiety | Deployed HT | −0.12 | −0.19 | −0.05 |
| Alcohol use/abuse | Deployed HT | −0.17 | −0.19 | −0.15 |
| Non-Perspective-Taking | Deployed HT | 0.30*** | 0.22* | 0.38*** |
| Anhedonic depression | Deployed LT | −0.08 | −0.15 | −0.01 |
| PTSD | Deployed LT | 0.06 | −0.02 | 0.14 |
| Insomnia | Deployed LT | 0.26*** | 0.18 | 0.34*** |
| Physical health | Deployed LT | 0.14 | 0.07 | 0.22 |
| Anxiety | Deployed LT | −0.17* | −0.22* | −0.13 |
| Alcohol use/abuse | Deployed LT | −0.12 | −0.18* | −0.07 |
| Non-Perspective-Taking | Deployed LT | 0.11 | −0.10 | 0.33*** |
| Anhedonic depression | Not deployed | −0.18 | ||
| PTSD | Not deployed | −0.17 | ||
| Insomnia | Not deployed | −0.02 | ||
| Physical health | Not deployed | 0.06 | ||
| Anxiety | Not deployed | −0.07 | ||
| Alcohol use/abuse | Not deployed | −0.08 | ||
| Non-Perspective-Taking | Not deployed | −0.03 | ||
Note.
p < 0.05;
p < 0.01;
p < 0.001;
DV = dependent variable; n.s. = not significant; HT = high-trauma; LT = low-trauma; p-values were adjusted for multiple comparisons separately for the analyses including and not including social support (with social support adjusted for 28, without social support adjusted for 21).
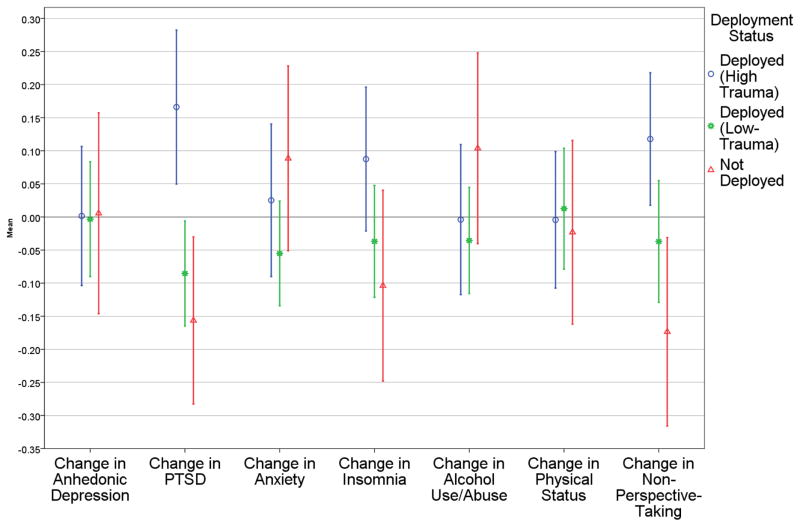
Table 3 shows the results of the ANCOVAs and post hoc t-tests used to compare the deployment categories to each other. PTSD, insomnia, and NPT showed significance at the omnibus level (adjusted p < 0.001 for all three). For PTSD, the high-trauma group showed significantly worse change than both the low-trauma and the non-deployed group (adjusted p < 0.01 for both). For insomnia, none of the between-group contrasts was significant after correction for multiple comparisons. For NPT, the high-trauma group showed significantly worse change than the non-deployed group (adjusted p < 0.01). Figure 1 shows the groups’ mean changes relative to each other (note that unlike Figure S1, the mean overall change in Figure 1 is zero because the change scores are residuals).
Table 3.
ANOVAs and post hoc t-tests Comparing Clinical Change Scores Across Deployment Categories.
| DV (Change in) | ANOVAs | Post hoc t-tests | |
|---|---|---|---|
| F | Comparison | |t| | |
| Anhedonic depression | 1.51 | ||
|
| |||
| PTSD | 22.09*** | ND vs DHT | 3.70** |
| ND vs DLT | 0.94 | ||
| DLT vs DHT | 3.51** | ||
|
| |||
| Insomnia | 9.29*** | ND vs DHT | 2.09 |
| ND vs DLT | 0.79 | ||
| DLT vs DHT | 1.77 | ||
|
| |||
| Physical health | 0.38 | ||
|
| |||
| Anxiety | 0.72 | ||
|
| |||
| Alcohol use/abuse | 0.67 | ||
|
| |||
| Non-Perspective-Taking | 8.10*** | ND vs DHT | 3.30** |
| ND vs DLT | 1.59 | ||
| DLT vs DHT | 2.24 | ||
Note.
p < 0.05;
p < 0.01;
p < 0.001;
DV = dependent variable; ND = not deployed; DHT = deployed (high-trauma); DHT = deployed (low-trauma); post hoc t-test p-values were adjusted for multiple comparisons (9 tests) using the Holm method.
Figure 1.
Change in Clinical Symptoms by Deployment Category, Controlling for Time 1 Symptom Levels, Previous Deployment, Years in the Marine Corps, and history of TBI.
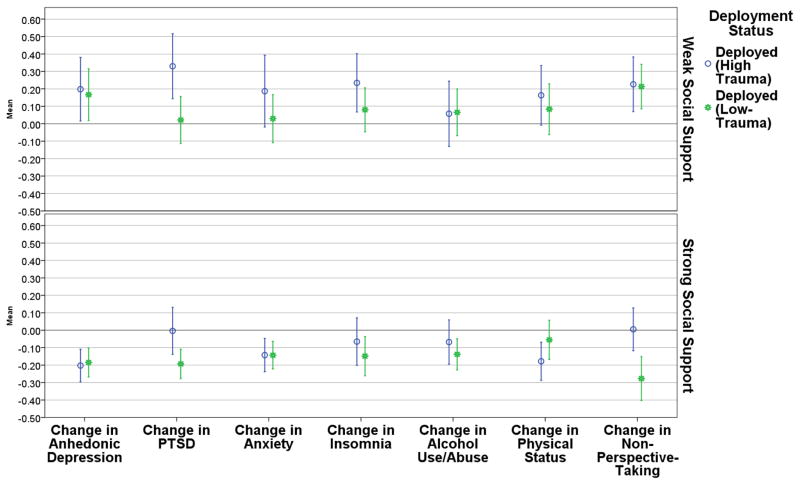
Table 4 shows the results of the ANCOVAs and post hoc t-tests examining clinical change by deployment category and social support. Five of the seven omnibus ANOVA effects were significant: Anhedonic depression differed between social support categories (p < 0.05); PTSD differed between deployment categories (p < 0.001) and social support categories (p < 0.01); insomnia differed between social support categories (p < 0.05); reported psycho-physical health differed between social support categories (p < 0.05); and NPT differed between deployment categories (p < 0.01) and social support categories (p < 0.001). Post hoc t-tests revealed that, for Anhedonic depression, all six groups differed from each other (and in the expected direction) with two exceptions: the high-trauma/strong-support (HTSS) and low-trauma/strong-support (LTSS) groups did not differ (adjusted p ≈ 1.0), and the high-trauma/weak-support (HTWS) and low-trauma/weak-support (LTWS) groups did not differ (adjusted p ≈ 1.0). For PTSD, the largest difference was between HTWS and LTSS (adjusted p < 0.001). For insomnia, the only groups that differed were HTWS and LTSS (p < 0.001). For physical health, HTSS and HTWS differed (p < 0.05). Finally, for NPT, the largest differences were between LTSS and LTWS, and between HTWS and LTSS (p < 0.001 for both). The HTSS and LTSS groups also differed (p < 0.05). Figure 2 shows these results graphically, where the y-axis is mean change score with all covariates regressed out, and therefore has the same interpretation as in Figure 1.
Table 4.
ANOVAs and post hoc t-tests Comparing Clinical Change Scores Across Deployment and Social Support Categories.
| DV (Change in) | ANOVAs | Post hoc Contrasts | ||
|---|---|---|---|---|
| Deployment Cat. | Social Support Cat. | |||
| F | F | Comparison | t | |
| Anhedonic depression | 0.58 | 5.73* | HTSS vs HTWS | 3.85** |
| HTSS vs LTSS | −0.38 | |||
| HTSS vs LTWS | 4.23*** | |||
| HTWS vs LTSS | 3.69** | |||
| HTWS vs LTWS | 0.20 | |||
| LTSS vs LTWS | 4.07** | |||
|
| ||||
| PTSD | 22.30*** | 7.65** | HTSS vs HTWS | 2.88 |
| HTSS vs LTSS | 2.25 | |||
| HTSS vs LTWS | 0.33 | |||
| HTWS vs LTSS | 4.99*** | |||
| HTWS vs LTWS | 2.60 | |||
| LTSS vs LTWS | 2.65 | |||
|
| ||||
| Insomnia | 3.29 | 4.38* | HTSS vs HTWS | 2.71 |
| HTSS vs LTSS | 0.81 | |||
| HTSS vs LTWS | 1.61 | |||
| HTWS vs LTSS | 3.60** | |||
| HTWS vs LTWS | 1.36 | |||
| LTSS vs LTWS | 2.62 | |||
|
| ||||
| Physical health | 0.07 | 5.95* | HTSS vs HTWS | 3.34* |
| HTSS vs LTSS | −1.63 | |||
| HTSS vs LTWS | 2.88 | |||
| HTWS vs LTSS | 2.07 | |||
| HTWS vs LTWS | 0.68 | |||
| LTSS vs LTWS | 1.47 | |||
|
| ||||
| Anxiety | 0.60 | 2.32 | ||
|
| ||||
| Alcohol use/abuse | 0.50 | 1.56 | ||
|
| ||||
| Non-Perspective-Taking | 8.02** | 21.33*** | HTSS vs HTWS | 2.16 |
| HTSS vs LTSS | 3.12* | |||
| HTSS vs LTWS | 2.32 | |||
| HTWS vs LTSS | 4.86*** | |||
| HTWS vs LTWS | 0.09 | |||
| LTSS vs LTWS | 5.35*** | |||
Note.
p < 0.05;
p < 0.01;
p < 0.001; interaction between Deployment Category and Social Support Category was significant for Non-Perspective-Taking (p = 0.042); all other interactions were non-significant; DV = dependent variable; Cat. = category; HTSS = high-trauma with strong social support; HTWS = high-trauma with weak social support; LTSS = low-trauma with strong social support; LTWS = low-trauma with weak social support.
Figure 2.
Change in Clinical Symptoms by Deployment Category and Social Support Category, Controlling for Time 1 Symptom Levels, Previous Deployment, Years in the Marine Corps, and history of TBI.
When these analyses were repeated excluding participants who had experienced a TBI (reducing the sample to N = 860), some of the results became non-significant. Specifically, when deployment and social support were examined together (corresponding to Table 4), there was no longer an association between social support and anhedonic depression (p > 0.05), between social support and insomnia (p > 0.05), and between social support and physical complaints (p > 0.05).
Discussion
The well-known association between heavy combat during deployment with increases in PTSD symptoms (Vasterling et al., 2010) was fully replicated in the present study. Non-Deployed participants and participants with relatively low combat exposure showed little change from pre-deployment symptom levels. Research suggesting that social support moderates the effect of combat intensity on PTSD symptom severity after deployment (Han et al., 2014; Schnurr et al., 2004) was also replicated. Non-Deployed participants and participants with relatively low combat exposure showed little change from pre-deployment symptom levels. We also found that social support at Time 2 was associated with changes in perspective taking only in low trauma or non-deployed groups, while high trauma groups showed reduced perspective taking regardless of social-support status. Note, however, that because perceived social support was assessed only post-deployment (and not assessed at all in non-deployed servicemembers), our claims about social support are limited to its potential associations post-deployment. For example, while we did find that the relationship of deployment with change in symptoms depends on post-deployment social support—thus meeting the statistical definition of moderation—we cannot rule out the possibility that pre-deployment social support is just as (if not more) important as post-deployment social support. It might be that servicemembers with strong social support in general are simply less vulnerable to trauma-related symptom change.
There has been little research on the effects of trauma and deployment on social habits and attitudes, notwithstanding the social withdrawal and dysfunction commonly reported in trauma survivors (Maercker et al., 1999; Schnurr et al., 2004). PTSD patients show reduced perspective taking on the IRI, attributed to the emotional numbing and avoidance components of PTSD (Nietlisbach and Maercker, 2009; Nietlisbach et al., 2010; Parlar et al., 2014). Our findings suggest that perspective taking is reduced with trauma exposure, rather than changing only in those with a PTSD diagnosis. This conclusion is supported by the low correlation (r = 0.06) between change in PTSD symptoms and change in perspective taking among the high-trauma group. Furthermore, analysis of IRI stratified by perceived social support, showed that perceived social support moderated perspective taking only in low trauma or non-deployed groups, while the high trauma groups showed reduced perspective taking regardless of perceived social-support. A recent longitudinal study showed that post-trauma social support perception was related to PTSD development and severity. Our finding of reduced perspective taking regardless of perceived social-support status in our high trauma group lends additional support to perspective taking being related to trauma exposure, and not specifically PTSD-related (Nickerson et al., 2016). Further research can determine whether trauma effects on perspective taking resolve with time in traumatized individuals or after treatment in those who develop PTSD. There is another notable point about our perspective-taking findings. Since perspective-taking is largely conceptualized as a dispositional trait, one would not expect it to change at all. That perspective taking does appear to be affected by deployment trauma suggests that either, a) the view of empathic tendency as a trait might be problematic, or b) battle trauma is psychologically powerful enough to change even deeply rooted personality traits.
We observed increased sleep problems in participants that experienced significant combat exposure (Figure 1). This association was maintained when controlling for PTSD and depression symptoms, thus it is not simply related to other mental health symptoms experienced after deployment. Sleep disruption after deployment predicts subsequent development of depression and PTSD symptoms, suggesting that deployment-related sleep problems may precede other signs of clinical dysfunction (Wright et al., 2011).
In summary, participants were relatively resilient to significant deployment-related changes in most mental health indices. The group with high combat exposure showed increased PTSD and insomnia symptoms and reductions in perspective-taking scores compared to low-exposure or non-deployed groups. Notably, the decrease in perspective taking was one of the least sensitive to social support, with no significant difference between the HTSS and HTWS groups. Associations related to sleep problems and non-perspective-taking could inform post-deployment mental healthcare. First, clinicians and family members should be particularly watchful for insomnia symptoms. These symptoms could represent a unique clinical phenomenon that could best be palliated with therapy targeted specifically toward sleep disturbance. Alternatively, they could portend other symptoms. The decreased perspective-taking of Servicemembers after experiencing a traumatic deployment seems to improve minimally from social support. Clinicians and family should be aware of the apparent counter-intuitive possibility that increasing social support might not help with the Servicemember’s non-perspective-taking and perhaps more individualized therapies such as cognitive-behavioral treatment are needed.
The clinical EFAs suggest clean measurement of well-established psychopathologies at both time points. This finding is encouraging, because it means the combined (target-rotated) model likely comes close to both individual time points’ structures, and scores generated from it can therefore safely be used to calculate change. Notably, although some of the clinical measures formed their corresponding factor in the EFA (e.g. AUDIT), this was not always the case. For example, factors 1 and 2 (“Anhedonic Depression” and “PTSD”, respectively) are a blend of the BDI, CAPS, SF-12, and PCL. This underlines the potential benefit of empirically derived measures, as some items from one measure are better indicators of a construct other than the one for which they were developed. Methods such as principal components analysis and factor analysis (used here) allow assignment of items to constructs based on what the data suggest rather than on theoretical expectations.
Overall the present study found that significant combat experience resulted in a specific pattern of changes in mental health, namely in increased PTSD and insomnia symptoms, as well as reductions in perspective-taking. Limitations to the study include a restricted assessment of psychiatric symptoms, a highly homogenous study population (male, infantry Marine battalions) that reduces generalizability, and a relatively long time span (4–6 months) between return from deployment and assessment of symptoms. This renders us unable to parse effects of deployment from effects of other experiences that occurred in the 4–6 months after deployment. An additional limitation is the single (post-deployment) collection of social support. Pre- as well as post-deployment social support would have permitted evaluation of change in social support in relation to combat exposure and PTSD and a choice of using social support for stratification. Finally, formal CFA testing of measurement invariance across the two time points suggested some violation of the measurement invariance assumption. Nonetheless, the present findings move us toward a fuller psychological profile of US Marines, whether non-deployed, deployed with low trauma exposure, or deployed with substantial trauma exposure.
Supplementary Material
Acknowledgments
This work was supported by the Navy Bureau of Medicine and Surgery N62645-11-C-4037; the VA Center of Excellence for Stress and Mental Health; NIMH grants MH089983, MH019112, MH096891, MH042228; and the Dowshen Program for Neuroscience.
Footnotes
The only exception was the CAPS variables, which were total scores on each section ranging from 0 to 7 or 0 to 8. To make them consistent with the remaining items, these were made ordinal by discretizing such that scores of 0–1 were coded a 0, scores of 2–5 were coded a 1, and score of 6 or greater were coded a 2.
CONFLICTS OF INTEREST: NONE
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Acheson DT, Geyer MA, Baker DG, Nievergelt CM, Yurgil K, Risbrough VB, Team MI. Conditioned fear and extinction learning performance and its association with psychiatric symptoms in active duty Marines. Psychoneuroendocrinology. 2015;51:495–505. doi: 10.1016/j.psyneuen.2014.09.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beck AT, Steer RA, Antonio TX. Beck Anxiety Inventory Manual. San Harcourt Brace and Company; 1993. [Google Scholar]
- Beck AT, Steer RA, Brown GK, Antonio TX Inventory II. Manual for Beck Depression (BDI-II) San Psychological Corp; 1996. [Google Scholar]
- Blake DD, Weathers FW, Nagy LM, Kaloupek DG, Gusman FD, Charney DS, Keane TM. The development of a clinician-administered PTSD scale. Journal of traumatic stress. 1995;8(1):75–90. doi: 10.1007/BF02105408. [DOI] [PubMed] [Google Scholar]
- Browne MW. On oblique procrustes rotation. Psychometrika. 1967;32(2):125–132. doi: 10.1007/BF02289420. [DOI] [PubMed] [Google Scholar]
- Browne MW. An Overview of Analytic Rotation in Exploratory Factor Analysis. Multivariate Behavioral Research. 2001;36(1):111–150. [Google Scholar]
- Conaton, E., D., Washington, D.C., 2012. DoD policy guidance for management of mild traumatic brain injury/concussion in the deployed setting (Do[DoDI] Number 6490. 11 Department of Defense b17.
- Davis MH. A multidimensional approach to individual differences in empathy 1980 [Google Scholar]
- Davis MH. Measuring individual differences in empathy: Evidence for a multidimensional approach. Journal of Personality and Social Psychology. 1983;44(1):113–126. [Google Scholar]
- Dirkzwager AJ, Bramsen I, Ploeg HM. Van Der Social support, coping, life events, and posttraumatic stress symptoms among former peacekeepers: a prospective study. Personality and Individual Differences. 2003;34(8):1545–1559. SRC - GoogleScholar. [Google Scholar]
- Fontana A, Rosenheck R, Horvath T. Social Support and Psychopathology in the War Zone. The Journal of Nervous & Mental Disease. 1997;185(11):675–681. doi: 10.1097/00005053-199711000-00004. [DOI] [PubMed] [Google Scholar]
- Grice JW. Computing and evaluating factor scores. Psychological methods. 2001;6(4):430–450. [PubMed] [Google Scholar]
- Han SC, Castro F, Lee LO, Charney ME, Marx BP, Brailey K, Vasterling JJ. Military unit support, postdeployment social support, and PTSD symptoms among active duty and National Guard soldiers deployed to Iraq. Journal of Anxiety Disorders. 2014;28(5):446–453. doi: 10.1016/j.janxdis.2014.04.004. [DOI] [PubMed] [Google Scholar]
- Haskell SG, Gordon KS, Mattocks K, Duggal M, Erdos J, Justice A, Brandt CA. Gender Differences in Rates of Depression, PTSD, Pain, Obesity, and Military Sexual Trauma Among Connecticut War Veterans of Iraq and Afghanistan. Journal of Women’s Health. 2010;19(2):267–271. doi: 10.1089/jwh.2008.1262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hibbard MR, Uysal S, Kepler K, Bogdany J, Silver J, Axis I. psychopathology in individuals with traumatic brain injury. The Journal of Head Trauma Rehabilitation. 1998;13(4):24–39. doi: 10.1097/00001199-199808000-00003. [DOI] [PubMed] [Google Scholar]
- Hoge CW, Auchterlonie JL, Milliken CS. Mental Health Problems, Use of Mental Health Services, and Attrition From Military Service After Returning From Deployment to Iraq or Afghanistan. JAMA. 2006;295(9):1023. doi: 10.1001/jama.295.9.1023. [DOI] [PubMed] [Google Scholar]
- Hoge CW, Castro CA, Messer SC, McGurk D, Cotting DI, Koffman RL. Combat Duty in Iraq and Afghanistan, Mental Health Problems, and Barriers to Care. New England Journal of Medicine. 2004;351(1):13–22. doi: 10.1056/NEJMoa040603. [DOI] [PubMed] [Google Scholar]
- Holm S. A simple sequentially rejective multiple test procedure. Scandinavian Journal of Statistics 6 SRC - GoogleScholar. 1979:65–70. [Google Scholar]
- Honaker J, King G, Blackwell M. Amelia II: A Program for Missing Data. Journal of Statistical Software. 2011;45(7) [Google Scholar]
- Hoofien D, Gilboa A, Vakil E, Donovick PJ. Traumatic brain injury (TBI) 10–20 years later: A comprehensive outcome study of psychiatric symptomatology, cognitive abilities and psychosocial functioning. Brain Injury. 2001;15(3):189–209. doi: 10.1080/026990501300005659. SRC - GoogleScholar. [DOI] [PubMed] [Google Scholar]
- Jamshidian M, Jalal S, Jansen C. MissMech : An R Package for Testing Homoscedasticity, Multivariate Normality, and Missing Completely at Random (MCAR) Journal of Statistical Software. 2014;56(6) [Google Scholar]
- Kang HK, Natelson BH, Mahan CM, Lee KY, Murphy FM. Post-traumatic stress disorder and chronic fatigue syndrome-like illness among Gulf War veterans: a population-based survey of 30,000 veterans. American journal of epidemiology. 2003;157(2):141–148. doi: 10.1093/aje/kwf187. [DOI] [PubMed] [Google Scholar]
- Kaspersen M, Matthiesen SB, Götestam KG. Social network as a moderator in the relation between trauma exposure and trauma reaction: A survey among UN soldiers and relief workers. Scandinavian Journal of Psychology. 2003;44(5):415–423. doi: 10.1046/j.1467-9450.2003.00362.x. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Colpe LJ, Fullerton CS, Gebler N, Naifeh JA, Nock MK, Sampson NA, Schoenbaum M, Zaslavsky AM, Stein MB. Design of the army study to assess risk and resilience in servicemembers (Army STARRS) International Journal of Methods in Psychiatric Research. 2013;22(4):267–275. doi: 10.1002/mpr.1401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim JO, Mueller CW, Hills CA. Factor analysis: Statistical methods and practical issues. Vol. 14. Beverly Sage; 1978. [Google Scholar]
- King LA, King DW, Fairbank JA, Keane TM, Adams GA. Resilience-recovery factors in post-traumatic stress disorder among female and male Vietnam veterans: Hardiness, postwar social support, and additional stressful life events. Journal of Personality and Social Psychology. 1998;74(2):420–434. doi: 10.1037//0022-3514.74.2.420. [DOI] [PubMed] [Google Scholar]
- Maercker A, Schützwohl M, Solomon Z. Posttraumatic stress disorder: A lifespan developmental perspective. Hogrefe & Huber; Seattle, WA: 1999. SRC - GoogleScholar. [Google Scholar]
- Milliken CS, Auchterlonie JL, Hoge CW. Longitudinal Assessment of Mental Health Problems Among Active and Reserve Component Soldiers Returning From the Iraq War. JAMA. 2007;298(18):2141. doi: 10.1001/jama.298.18.2141. [DOI] [PubMed] [Google Scholar]
- Moore TM, Reise SP, Depaoli S, Haviland MG. Iteration of Partially Specified Target Matrices: Applications in Exploratory and Bayesian Confirmatory Factor Analysis. Multivariate Behavioral Research. 2015;50(2):149–161. doi: 10.1080/00273171.2014.973990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muthén LK, Muthén BO. Mplus statistical modeling software: Release 7. Muthén & Muthén; Los Angeles, CA: 2012. SRC - GoogleScholar. [Google Scholar]
- Nickerson A, Creamer M, Forbes D, McFarlane AC, Donnell ML, Silove D, Bryant RA. The longitudinal relationship between post-traumatic stress disorder and perceived social support in survivors of traumatic injury. Psychological Medicine. 2016:1–12. doi: 10.1017/S0033291716002361. SRC - GoogleScholar. [DOI] [PubMed] [Google Scholar]
- Nietlisbach G, Maercker A. Social Cognition and Interpersonal Impairments in Trauma Survivors with PTSD. Journal of Aggression, Maltreatment & Trauma. 2009;18(4):382–402. [Google Scholar]
- Nietlisbach G, Maercker A, Haker H, Rössler W. Are empathic abilities impaired in posttraumatic stress disorder? Psychological Reports. 2010;106:832–844. doi: 10.2466/pr0.106.3.832-844. SRC - GoogleScholar. [DOI] [PubMed] [Google Scholar]
- Parlar M, Frewen P, Nazarov A, Oremus C, MacQueen G, Lanius R, McKinnon MC. Alterations in empathic responding among women with posttraumatic stress disorder associated with childhood trauma. Brain and Behavior. 2014;4(3):381–389. doi: 10.1002/brb3.215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pietrzak RH, Johnson DC, Goldstein MB, Malley JC, Southwick SM. Psychological resilience and postdeployment social support protect against traumatic stress and depressive symptoms in soldiers returning from Operations Enduring Freedom and Iraqi Freedom. Depression and Anxiety. 2009;26(8):745–751. doi: 10.1002/da.20558. [DOI] [PubMed] [Google Scholar]
- Polusny MA, Erbes CR, Murdoch M, Arbisi PA, Thuras P, Rath MB. Prospective risk factors for new-onset post-traumatic stress disorder in National Guard soldiers deployed to Iraq. Psychological Medicine. 2011;41(04):687–698. doi: 10.1017/S0033291710002047. SRC - GoogleScholar. [DOI] [PubMed] [Google Scholar]
- Prigerson HG, Maciejewski PK, Rosenheck RA. Population Attributable Fractions of Psychiatric Disorders and Behavioral Outcomes Associated With Combat Exposure Among US Men. American Journal of Public Health. 2002;92(1):59–63. doi: 10.2105/ajph.92.1.59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pulos S, Elison J, Lennon R. The hierarchical structure of the Interpersonal Reactivity Index. Social Behavior and Personality: an international journal. 2004;32(4):355–359. [Google Scholar]
- Ramchand R, Rudavsky R, Grant S, Tanielian T, Jaycox L. Prevalence of, Risk Factors for, and Consequences of Posttraumatic Stress Disorder and Other Mental Health Problems in Military Populations Deployed to Iraq and Afghanistan. Current Psychiatry Reports. 2015;17(5) doi: 10.1007/s11920-015-0575-z. [DOI] [PubMed] [Google Scholar]
- Rao V, Lyketsos C. Neuropsychiatric Sequelae of Traumatic Brain Injury. Psychosomatics. 2000;41(2):95–103. doi: 10.1176/appi.psy.41.2.95. [DOI] [PubMed] [Google Scholar]
- Saunders JB, Aasland OG, Babor TF, de la Fuente JR, Grant M. Development of the Alcohol Use Disorders Identification Test (AUDIT): WHO collaborative project on early detection of persons with harmful alcohol consumption-II. Addiction. 1993;88:791–804. doi: 10.1111/j.1360-0443.1993.tb02093.x. SRC - GoogleScholar. [DOI] [PubMed] [Google Scholar]
- Schnurr PP, Lunney CA, Sengupta A. Risk factors for the development versus maintenance of posttraumatic stress disorder. Journal of Traumatic Stress. 2004;17(2):85–95. doi: 10.1023/B:JOTS.0000022614.21794.f4. [DOI] [PubMed] [Google Scholar]
- Schönemann PH. A generalized solution of the orthogonal procrustes problem. Psychometrika. 1966;31(1):1–10. [Google Scholar]
- Solomon Z, Mikulincer M, Avitzur E. Coping, locus of control, social support, and combat-related posttraumatic stress disorder: A prospective study. Journal of Personality and Social Psychology. 1988;55(2):279–285. doi: 10.1037//0022-3514.55.2.279. [DOI] [PubMed] [Google Scholar]
- Thurstone LL. The vectors of mind. Chicago University of Chicago Press; 1935. [Google Scholar]
- Ursano RJ, Colpe LJ, Heeringa SG, Kessler RC, Schoenbaum M, Stein MB. The army study to assess risk and resilience in Servicemembers (Army STARRS) Psychiatry: Interpersonal and Biological Processes. 2014;77(2):107–119. doi: 10.1521/psyc.2014.77.2.107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vasterling JJ, Proctor SP, Amoroso P, Kane R, Heeren T, White RF. Neuropsychological outcomes of army personnel following deployment to the Iraq war. JAMA. 2006;296(5):519–529. doi: 10.1001/jama.296.5.519. [DOI] [PubMed] [Google Scholar]
- Vasterling JJ, Proctor SP, Friedman MJ, Hoge CW, Heeren T, King LA, King DW. PTSD symptom increases in Iraq-deployed soldiers: Comparison with nondeployed soldiers and associations with baseline symptoms, deployment experiences, and postdeployment stress. Journal of Traumatic Stress. 2010;23(1):41–51. doi: 10.1002/jts.20487. SRC - GoogleScholar. [DOI] [PubMed] [Google Scholar]
- Vogt D, Smith BN, King LA, King DW, Knight J, Vasterling JJ. Deployment Risk and Resilience Inventory-2 (DRRI-2): An updated tool for assessing psychosocial risk and resilience factors among service members and veterans. Journal of Traumatic Stress. 2013;26(6):710–717. doi: 10.1002/jts.21868. [DOI] [PubMed] [Google Scholar]
- Vogt DS, Proctor SP, King DW, King LA, Vasterling JJ. Validation of Scales From the Deployment Risk and Resilience Inventory in a Sample of Operation Iraqi Freedom Veterans. Assessment. 2008;15(4):391–403. doi: 10.1177/1073191108316030. [DOI] [PubMed] [Google Scholar]
- Ware J, Kosinski M, Keller SD. A 12-Item Short-Form Health Survey: construction of scales and preliminary tests of reliability and validity. Medical care. 1996;34(3):220–233. doi: 10.1097/00005650-199603000-00003. [DOI] [PubMed] [Google Scholar]
- Weathers FW, Litz BT, Herman DS, Huska JA, Keane TM, The P. checklist (PCL): Reliability, validity, and diagnostic utility. Paper presented at the Ninth Annual Conference of the ISTSS; San Antonio. 1993. [Google Scholar]
- Wirth RJ, Edwards MC. Item factor analysis: Current approaches and future directions. Psychological Methods. 2007;12(1):58–79. doi: 10.1037/1082-989X.12.1.58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wright KM, Britt TW, Bliese PD, Adler AB, Picchioni D, Moore D. Insomnia as predictor versus outcome of PTSD anvd depression among Iraq combat veterans. Journal of Clinical Psychology. 2011;67(12):1240–1258. doi: 10.1002/jclp.20845. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.