Abstract
Situs inversus totalis is the mirror image of situs solitus, the normal position of abdominal and thoracic viscera. Many associated intraabdominal anomalies have been described with this condition. However, association of choledochal cyst with situs inversus has never been reported. Diagnosis and surgical procedures for abdominal pathology in patients with situs inversus totalis are technically more complicated and pose unique challenges because of left-right transposition of the visceral organs. The choledochal cyst is usually diagnosed in the neonatal period or during childhood. The clinical symptoms are nonspecific and usually include pain in the right upper quadrant and jaundice. The condition may also present with biliary colic, cholangitis, cholelithiasis or pancreatitis. In our case, the abdominal ultrasonography performed on a 55-year-old female who presented to us with jaundice, fever and pain in the left upper abdomen revealed presence of situs inversus with fusiform dilation of the common bile duct. Based on the magnetic resonance cholangiopancreatography (MRCP) images diagnosis of type I choledochal cyst was made. The aim of this case report is to illustrate an extremely rare association of situs inversus totalis with choledochal cyst along with the challenges faced in diagnosis and surgical management of this condition.
Keywords: Cholangiography, Choledochal cyst, Hepaticojejunostomy, Situs inversus totalis
Introduction
Situs inversus totalis (SIT) is the mirror image of normal anatomical position of both thoracic and abdominal viscera. Various anomalies have been described in association with SIT; however, association with choledochal cyst (CDC) has never been reported. Diagnosis and surgical technique for any abdominal pathology in patients with SIT are technically challenging because of altered anatomy of visceral organs [1].
Here, we describe a case of CDC with SIT that remained undiagnosed till late adulthood and was detected during workup for cholangitis.
Case Report
A 55-year-old female presented to us with 1-week history of constant, moderate to severe intensity, non-colicky pain in left hypochondrium. She also had complains of intermittent high-grade fever with chills, jaundice and pruritus for last 5 days. She was initially managed medically elsewhere with no significant response. Past medical and surgical history was unremarkable. At the time of admission, the patient had high-grade fever, tachycardia and icterus, though she was conscious and normotensive. Abdominal examination revealed tenderness over left hypochondrium.
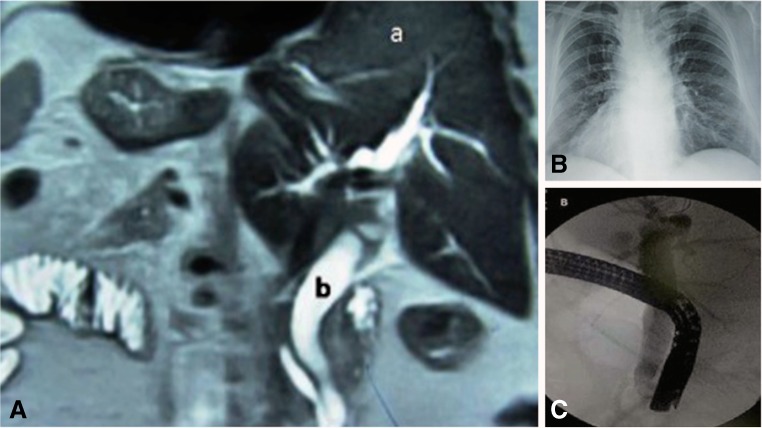
Laboratory work up showed leukocytosis with neutrophilia, elevated serum bilirubin (12.5 mg/dl), mildly raised alanine transaminase level (98 U/L, normal <40 U/L) and elevated alkaline phosphatase (508 U/L, normal <150 U/L). Renal function tests and coagulation profile were normal. Ultrasound (USG) abdomen and later magnetic resonance cholangiopancreaticography (MRCP) revealed SIT with cholelithiasis and dilated, anechoic extra-hepatic bile duct (Fig. 1A). X-ray of the chest showed dextrocardia and clear lung fields (Fig. 1B).
Fig. 1.
A MRI showing complete situs inversus with fusiform dilatation of bile duct (a liver, b common bile duct). B X-ray of the chest showing dextrocardia. C Endoscopic retrograde cholangiogram showing fusiform dilatation of the bile duct
On the basis of above findings, diagnosis of SIT with type I CDC complicated by cholangitis was made. The patient was started empirically on intravenous imipenem, at the dose of 2 g/day in divided doses. Fever failed to resolve after 48 h of antibiotic treatment; so an urgent endoscopic biliary drainage was planned. Endoscopic retrograde cholangopancreaticography (ERCP) was first tried in usual left lateral position but papilla could not be localised. Then procedure was attempted in right lateral position with endoscopist standing on the right side. Successful cannulation of papilla and biliary stenting could be performed in this adjusted position (Fig. 1C). She responded rapidly following biliary decompression and became afebrile within 24 h.
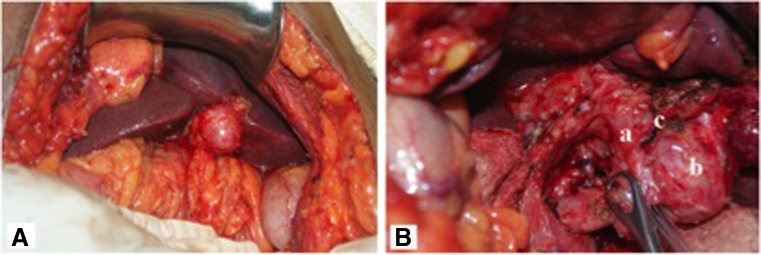
Four weeks after resolution of cholangitis, the patient was taken up for CDC excision with Roux-en-Y hepaticojejunostomy. The abdominal cavity was accessed through extended left subcostal incision with the patient placed in the supine position. Dense adhesions were present in the subhepatic area. The gallbladder was first dissected from the liver. The CDC was then meticulously mobilised from the underlying portal vein, hepatic arteries, duodenum and pancreas. The tapered end of the cyst was transected and ligated just proximal to the common bilio-pancreatic channel. The proximal mobilisation of cyst was done till the hilum. The anterior cyst wall was split opened from below upwards and hepatic duct openings were identified. The proximal transection was done 1 cm below the hilum and the cyst was excised out. The bilio-enteric continuity was restored with single layer, interrupted hepaticojejunostomy using a 50-cm-long jejunal Roux limb. A small drain was placed in the region at the end of the procedure. Unlike ERCP, surgery could be performed successfully without any modification in the position of the surgical team; the operating surgeon remained on the right side of the patient with first and second assistants on the left side (Fig. 2).
Fig. 2.
A Operative image showing the liver and gallbladder in the left upper quadrant with dense pericholecystic adhesions. B CDC (a) and inflamed and distended gallbladder (b) with frozen Calot’s triangle (c)
Post-operative hospital course was uneventful. Histopathology was suggestive of chronic cholecystitis with bile duct examination consistent with CDC. The patient is doing well after a follow-up of 18 months.
Discussion
SIT is a rare congenital anomaly. It has been found to be associated with genetic diseases like Kartagener’s syndrome as well as other anomalies such as polysplenia, asplenia, duodenal atresia, biliary atresia, gastroschisis, congenital hepatic fibrosis, tracheoesophageal fistula, diaphragmatic hernia and pheochromocytoma [2, 3]. However, till date, association of SIT with CDC has not been reported in the medical literature.
SIT poses diagnostic and therapeutic challenge due to altered visceral position. Our patient too had pain over the left upper abdomen, which initially caused diagnostic dilemma. The diagnosis could be established only after abdominal USG examination. Performing ERCP may be difficult in the usual left lateral position and specific maneuvers have been described for successful cannulation in patients with SIT [4, 5]. In the present case too, ERCP was possible only in modified right lateral position.
The position of the gallbladder and the branching patterns of the biliary tract are mirror image in situs inversus relative to normal. Mayo et al. reported hepatobiliary anomalies in their series of 76 patients with situs inversus [2]. Associated abdominal anomalies include biliary atresia, lobulation of liver, absent gallbladder, portal vein hypoplasia, absence of suprarenal venacava and quadruplication anomaly of the bile ducts [6, 7]. Our patient had no anomaly other than CDC that remained asymptomatic till the sixth decade of life. Although commonly diagnosed in early childhood, CDC presenting in adulthood is not unusual. The symptoms of CDC in adults are often vague and nonspecific. Several studies have reported higher association of cirrhosis, pancreatitis, choledocholithiasis and cholangitis in adult CDC cases as compared to pediatric cases [8, 9]. Complete cyst excision may be challenging in view of pericystic inflammation and adhesion. Although mortality rate is low, morbidity associated with surgical cyst excision may be significant [10]. Bile leak and surgical site infections are common early complications. Patients also remain at risk for developing anastomotic stricture and cholangiocarcinoma in the long run. Our patient had uneventful recovery after surgery and remained healthy till her last follow-up.
The altered anatomy in SIT demands a careful preoperative planning for operating room setup and surgical team positioning. A right-handed surgeon may be comfortable to operate from the right side of the patient with SIT. The abdomen can be approached through a midline or another suitable incision. In the present case, an extended left subcostal incision was given to expose the gallbladder and CDC. Due to the mirror image of the anatomy, operating surgeon should reorient him/herself repetitively during the procedure to avoid misperception of the pathological anatomy and thus iaterogenic injury. Vascular anatomy of the pericholedochal region also requires specific attention while dissecting the cyst. The right-sided orientation of the pancreatic duct and its orifice places it at danger while dissecting the intrapancreatic portion of the cyst.
Conclusion
Individuals with SIT pose unique diagnostic and management problems when they present with abdominal symptoms. Proper assessment and planning is important to ensure safety and success of surgery. Technical difficulties may arise due to the contralateral disposition of the viscera; hence, meticulous dissection and exposure of the biliary structures are required to avoid iatrogenic injury.
Contribution of Authors
APM, SK, VG, AC: concept and design
APM, SK, AC: drafting the manuscript and critical revision
The manuscript has been read and approved by all the authors, the requirements for authorship as stated earlier in this document have been met, and each author believes that the manuscript represents honest work, if that information is not provided in another form.
Compliance with Ethical Standards
Redundant or Duplicate Publication
No
Presentation at a Meeting
None
Conflict of Interest
The authors declare that they have no conflicts of interest.
Ethical Approval
Obtained by institutional ethical committee
Patient’s Consent
Obtained
Copyright Assignment
Yes
Source(s) of Support
Nil
References
- 1.Blegen HM. Surgery in situs inversus. Ann Surg. 1949;129:244–259. doi: 10.1097/00000658-194902000-00009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Mayo CW, Rice RG. Situs inversus totalis; a statistical review of data on 76 cases with special reference to disease of the biliary tract. Arch Surg. 1949;58:724–730. doi: 10.1001/archsurg.1949.01240030734014. [DOI] [PubMed] [Google Scholar]
- 3.Lee SE, Kim HY, Jung SE, Lee SC, Park KW, Kim WK. Situs anomalies and gastrointestinal abnormalities. J Pediatr Surg. 2006;41:1237–1242. doi: 10.1016/j.jpedsurg.2006.03.045. [DOI] [PubMed] [Google Scholar]
- 4.McDermott JP, Caushaj PF. ERCP and laparoscopic cholecystectomy for cholangitis in a 66-year-old male with situs inversus. Surg Endosc. 1994;8:1227–1229. doi: 10.1007/BF00591057. [DOI] [PubMed] [Google Scholar]
- 5.Fiocca F, Donatelli G, Ceci V, Cereatti F, Romagnoli F, Simonelli L, et al. ERCP in total situs viscerum inversus. Case Rep Gastroenterol. 2008;2:116–120. doi: 10.1159/000119713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Fulcher AS, Turner MA. Abdominal manifestations of situs anomalies in adults. Radiographics. 2002;22:1439–1456. doi: 10.1148/rg.226025016. [DOI] [PubMed] [Google Scholar]
- 7.Gagner M, Munson JL, Scholz FJ. Hepatobiliary anomalies associated with polysplenia syndrome. Gastrointest Radiol. 1991;16:167–171. doi: 10.1007/BF01887336. [DOI] [PubMed] [Google Scholar]
- 8.Ouaissi M, Kianmanesh R, Ragot E, Belghiti J, Wildhaber B, Nuzzo G, et al. Congenital bile duct cyst (BDC) is a more indolent disease in children compared to adults, except for Todani type IV-A BDC: results of the European multicenter study of the French Surgical Association. HPB: the official journal of the International Hepato Pancreato Biliary Association. 2016;18(6):529–539. doi: 10.1016/j.hpb.2016.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Park SW, Koh H, Oh JT, Han SJ, Kim S. Relationship between anomalous pancreaticobiliary ductal union and pathologic inflammation of bile duct in choledochal cyst. Pediatr Gastroenterol Hepatol Nutr. 2014;17(3):170–177. doi: 10.5223/pghn.2014.17.3.170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gadelhak N, Shehta A, Hamed H. Diagnosis and management of choledochal cyst: 20 years of single center experience. World J Gastroenterol. 2014;20(22):7061–7066. doi: 10.3748/wjg.v20.i22.7061. [DOI] [PMC free article] [PubMed] [Google Scholar]