Abstract
Objectives:
To determine the factors closely correlated with the unhealthy psychological status of patients with lung cancer and to ascertain whether the unhealthy psychology adversely affects their quality-of-life (QOL).
Methods:
Patients newly diagnosed with lung cancer between May 2013 and December 2015 in the Department of Thoracic Surgery, Tianjin 4th Centre Hospital, Tianjin, China were enrolled in this cross-sectional study. Patients were asked to complete the Symptom Checklist 90 (SCL-90) and Quality of Life Questionnaire (QLQ-C30) survey. From the responses, the correlation between the patient’s psychological status and QOL were analyzed with respect to several variables.
Results:
From the total of 258 patients subjected to the test, 168 belonged to the unhealthy psychology group and 90 to the healthy psychology group. Multiple regression analysis revealed that significant factors related to poor QOL among the 2 groups are gender (p=0.02), younger age (p=0.001), surgical history (p=0.04), employment status (p=0.03), and medical insurance (p=0.01) significantly predicted the severity of unhealthy psychology in lung cancer patients. A significantly negative correlation was noted between the points of SCL-90 and the general QOL in all included patients (p=0.03).
Conclusion:
Gender, younger age, surgical history, employment status, and medical insurance significantly predicted the severity of unhealthy psychology in lung cancer patients.
Lung cancer is the second most common cancer1 accounting for the largest number of cancer-related deaths worldwide. Limited improvements have been achieved in this cancer by therapy over the past decades, with the 5-year survival rate being only 16%.2 Patients with lung cancer may suffer from variable degrees of functional impairments that affect their quality-of–life (QOL) adversely. In addition, the negative cancer experiences and the side effects associated with cancer treatments such as pain, fatigue, nausea, and vomiting can also result in a wide range of health problems, bringing about not only physical issues, but also psychological and emotional distresses, including depression and anxiety.3 The severity of cancer-related symptoms has been strongly related to the psychological symptoms in the patients,4 and the unhealthy psychological status has been shown to be associated with a significantly increased frequency of cancer-related mortality.5 Of 102 lung cancer patients treated by chemotherapy, Baczewska found6 that 51.5% showed symptoms of severe depression, suggesting that depression occurs more frequently and with greater intensity in lung cancer patients as compared with that in healthy individuals. In another study of 1334 consecutively recruited lung cancer patients, Shimizu7 reported 440 with significant anxiety issues. The QOL, which is described as an individual response to the physical, mental, and social effects of diseases toward individual satisfaction in the daily life, has been emphasized for chronic disease.8 We believe that the negative mental status of lung cancer patients affects their QOL adversely. A detailed study in this respect may provide the physicians with better insights toward understanding the importance of psychotherapy for patients with lung cancer. In this study, 258 patients with lung cancer who were admitted to the Department of Thoracic Surgery from May 2013 to December 2015 were questioned with the following objective: 1) to determine the factors closely correlated with the unhealthy psychological status, and 2) to ascertain whether the unhealthy psychological status affects the QOL of lung cancer patients.
Methods
In this study, a total of 325 patients who were newly diagnosed with lung cancer between May 2013 and December 2015 in the Department of Thoracic surgery, Tianjin 4th Centre Hospital were recruited to participate in a questionnaire survey. The participants were asked to complete questionnaires on their psychological status and QOL prior to their cancer treatment. Age, gender, marital status, employment status, medical insurance condition, education condition, surgical history, smoking history, and the duration from the first visit of all the participants were recorded.
Inclusion and exclusion criteria
The patients who met the following criteria were included in the study: 1) patients diagnosed with lung cancer; 2) patients who have not received any type of medical treatment such as chemotherapy, radiation therapy, or surgery; 3) patients who have signed a written informed consent. The patients who preferred not to participate in the study or those with mental disorders were excluded from the study. This study was approved by the Ethics Committee of Tianjin 4th Centre Hospital and was conducted in accordance with the Principles of Helsinki Declaration, and written informed consents were signed by all participants. To find previous related researches, the literatures existing on MEDLINE from December 1986 through December 2016 were searched using the words “lung cancer” “lung carcinoma,” “lung tumor,” “quality of life,” and “psychology” by physicians.
Two questionnaires were distributed among the patients for evaluation of their psychological status and QOL. The Symptom Checklist 90 (SCL-90), a 90-item self-reporting questionnaire, was used to evaluate the psychological status of the patients. The symptom severity of each item was assessed using a 5-Likert scale, in which “0” indicated “not at all” and “4” indicated “extremely.”9 The included patients were divided into the healthy and unhealthy psychology groups, according to their SCL-90 scores.10 The SCL-90 score exceeding 160 represented unhealthy status, while that of less than 160 represented the healthy status.11 The Quality of Life Questionnaire (QLQ-C30) was used to assess the QOL.12 In the questions regarding QOL, the answers are graded on the scale of 1-7, with the ascending values indicating increasing QOL.6 To facilitate the analysis, the points were standardized on the scale of 1 to 100 and assessed according to a 4-degree Likert scale, namely, 0–25 points indicated “very low QOL,” 26–50 points indicated “low QOL,” 51–75 points indicated “high QOL,” and 76–100 points indicated “very high QOL.6
Statistical analysis
For statistical analysis, The Statistical Package for the Social Sciences was performed (IBM Corp., Armonk, NY) version 21. Numerical data were compared by Student’s t-test. The categorical variables were evaluated by Chi-squared test or Rank sum test. The correlation analysis was performed by Pearson’s correlation analysis or by multiple regression analysis. A p-value of <0.05 was considered to be statistical significance.
Results
Of the 325 patients in the department, 258 patients were included in the current study according to the inclusion and exclusion criteria. Among the 258 patients, 162 were male and 96 were female (age ranged from 38 to 82 years). In the study, 168 patients belonged to the unhealthy psychology group and 90 to the healthy psychology group. The rate of unhealthy psychological status was 65%.
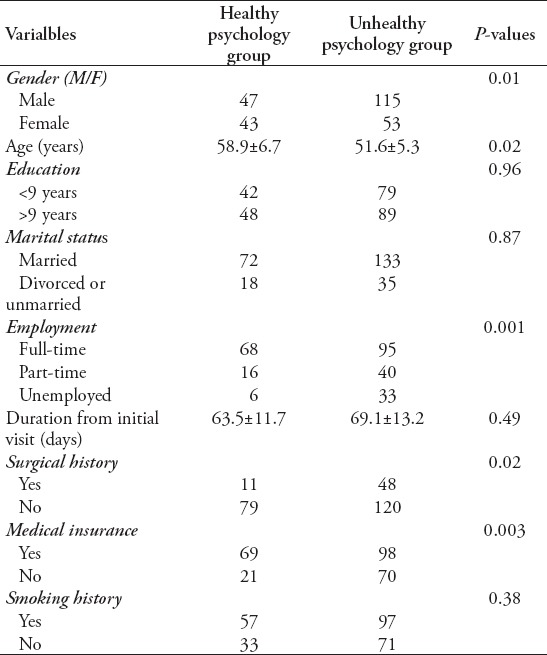
The comparison of QOL between the 2 groups are listed in Table 1. The percentage of low and very low QOL was 67.8% and 72.6% and that of high and very high QOL was 32.2% and 27.4% in the healthy and unhealthy psychology groups, respectively (Table 1).” In addition, significantly negative correlation was recorded between the SCL-90 scores and the general QOL in all patients (p=0.03). In addition, there was a significant difference in gender (p=0.01), younger age (p=0.02), surgical history (p= 0.02), employment status (p=0.001), and medical insurance (p=0.003) between the two groups (Table 2). The results of multiple regression analysis revealed that the above-mentioned variables were significantly predictive of the severity of unhealthy psychology among the included patients.
Table 1.
The comparison of general quality of life between the 2 groups.
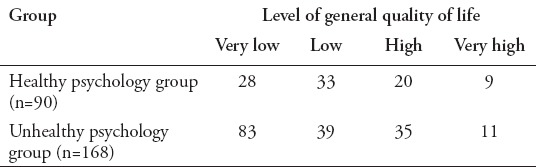
Table 2.
The comparison of demographics of 2 groups.
Discussion
In our study, 65% lung cancer patients presented with unhealthy psychological status; the multiple regression analysis of the data revealed that gender, age, surgical history, employment status, and medical insurance factors were significantly predictive of the severity of unhealthy psychology of the patients. Male patients are more likely to suffer from unhealthy psychology as they also have to bear the heavy burdens of family life and several kinds of pressures from the society as compared with the female patients. Pain resulting from the surgery may also produce psychological stress, affecting the psychological status of the patients. Thus, the history of surgery can adversely aggravate the depression and anxiety in lung cancer patients. The employment and medical insurance also affects the psychological status of patients as the fatal disease burdens the patients’ economy. As a result, the financial situation may become difficult if a patient does not have a job and medical insurance. In these aspects, most authors hold the same viewpoints.10,13
In the present study, no significant difference was noted in the marital conditions between the healthy and unhealthy psychology groups. The multiple regression analysis revealed that marital condition was not a significant predictive factor of the severity of unhealthy psychology. This result is in concordance with that of Park,14 who made a similar conclusion in his study of 278 patients, while, Wang et al15 suggested a different viewpoint, advocating that marital conditions are closely correlated with the psychological status of lung cancer patients. In this regard, we believe that a more focused and detailed study is warranted for confirmation and clarification of the viewpoint.
Some authors worked on the relationship between psychotherapy and the clinical outcomes of lung cancer patients. Zhao et al16 studied 124 lung cancer patients treated surgically, in whom psychological intervention was performed in the experimental group, while conventional nursing intervention was performed in a control group. They reported that, as compared with the control group, the Visual Analogue Scale (VAS) was significantly decreased and immune function was significantly increased in patients of the experimental group. In another study of a total of 684 lung cancer patients, Vodermaier17 found that anxiety is associated with increased mortality. Some other authors have also advocated the same viewpoints.18 These studies demonstrate that psychotherapy plays an important role in the management of lung cancer patients.
In terms of the predictive factors of unhealthy psychological status, some of our viewpoints were consistent with those of previous studies, but some differed. Thus, further studies are warranted to clarify these issues.
In conclusion, we found the percentage of patients with low and very low QOL was high and very near in both healthy and unhealthy psychological status. Therefore, psychotherapy has to be recommended to all lung cancer patients felt in need, not only for those patients with unhealthy psychology status. Nevertheless, we believe that poor QOL may further worsen the unhealthy psychological status, and this vicious circle inevitably influences the final clinical outcomes of the lung cancer patients. In addition, other criteria for selecting patients has to be looked for and studied. Subsequently, we suggest that psychological intervention should be emphasized in all patients with lung cancer, especially in young and unemployed male patients, who have no medical insurance, because these factors are the independent risk factors that have been identified to be closely correlated with unhealthy psychology.
Footnotes
References
- 1.Aldarouish M, Wang C. Trends and advances in tumor immunology and lung cancer immunotherapy. J Exp Clin Cancer Res. 2016;35:157. doi: 10.1186/s13046-016-0439-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Del Mar Valenzuela-Membrives M, Perea-Garcia F, Sanchez-Palencia A, Ruiz-Cabello F, Gomez-Morales M, Miranda-Leon MT, et al. Progressive changes in composition of lymphocytes in lung tissues from patients with non-small-cell lung cancer. Oncotarget. 2016;7:71608–71619. doi: 10.18632/oncotarget.12264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wang T, Deng R, Tan JY, Guan FG. Acupoints Stimulation for Anxiety and Depression in Cancer Patients: A Quantitative Synthesis of Randomized Controlled Trials. Evid Based Complement Alternat Med. 2016;2016:5645632. doi: 10.1155/2016/5645632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Walker MS, Pohl GM, Houts AC, Peltz G, Miller PJE, Schwartzberg LS, et al. Analysis of the psychological impact of cancer-related symptoms on patients with non-small cell lung cancer. Psychooncology. 2017;26:755–762. doi: 10.1002/pon.4071. [DOI] [PubMed] [Google Scholar]
- 5.Drageset J, Eide GE, Hauge S. Symptoms of depression, sadness and sense of coherence (coping) among cognitively intact older people with cancer living in nursing homes-a mixed-methods study. PeerJ. 2016;4:e2096. doi: 10.7717/peerj.2096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Baczewska B, Kaminska M, Ciszewski T, Kubiatowski T, Makara-Studzinska M, Sygit K, et al. Quality of life and occurrence of depression under chemotherapy in patients suffering from lung carcinoma. Ann Agric Environ Med. 2014;21:783–789. doi: 10.5604/12321966.1129933. [DOI] [PubMed] [Google Scholar]
- 7.Shimizu K, Nakaya N, Saito-Nakaya K, Akechi T, Ogawa A, Fujisawa D, et al. Personality traits and coping styles explain anxiety in lung cancer patients to a greater extent than other factors. Jpn J Clin Oncol. 2015;45:456–463. doi: 10.1093/jjco/hyv024. [DOI] [PubMed] [Google Scholar]
- 8.Duman E, Yildirim M, Kaya V, Ozturk D, Inal A, Akarsu Z, et al. Effects of Definitive Chemoradiotherapy on Respiratory Function Tests and Quality of Life Scores During Treatment of Lung Cancer. Asian Pac J Cancer Prev. 2015;16:6779–6782. doi: 10.7314/apjcp.2015.16.15.6779. [DOI] [PubMed] [Google Scholar]
- 9.Wongpakaran T, Wongpakaran N. Personality traits influencing somatization symptoms and social inhibition in the elderly. Clin Interv Aging. 2014;9:157–164. doi: 10.2147/CIA.S56246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wang F, Lu Z, Lu W, Zhang X, Mo X. Correlation Between Psychological Status and Quality of Life in Patients with Lung Cancer: A Control Study. Chin J Clin Thorac Cardiovasc Surg. 2016;23:1–4. [Google Scholar]
- 11.Liu Y, Song H, Wang T, Wang T, Yang H, Gong J, Shen Y, Dai W, Zhou J, Zhu S, et al. Determinants of tobacco smoking among rural-to-urban migrant workers: a cross-sectional survey in Shanghai. BMC Public Health. 2015;15:131. doi: 10.1186/s12889-015-1361-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Polanski J, Jankowska-Polanska B, Rosinczuk J, Chabowski M, Szymanska-Chabowska A. Quality of life of patients with lung cancer. Onco Targets Ther. 2016;9:1023–1028. doi: 10.2147/OTT.S100685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Trevino KM, Maciejewski PK, Fasciano K, Greer J, Partridge A, et al. Coping and psychological distress in young adults with advanced cancer. J Support Oncol. 2012;10:124–130. doi: 10.1016/j.suponc.2011.08.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Park S, Kang CH, Hwang Y, Seong YW, Lee HJ, Park IK, et al. Risk factors for postoperative anxiety and depression after surgical treatment for lung cancerdagger. Eur J Cardiothorac Surg. 2016;49:e16–e21. doi: 10.1093/ejcts/ezv336. [DOI] [PubMed] [Google Scholar]
- 15.Wang F, Lu Z, Lu W, Zhang X, Mo X. Survey and analysis on the changes and influence factors of psychological state of the patients with lung cancer. Prac J Med &Pharm. 2016;33:586–589. [Google Scholar]
- 16.Zhao X, Cui L, Wang W, Su Q, Li X, Wu J. Influence of psychological intervention on pain and immune functions of patients receiving lung cancer surgery. Pak J Med Sci. 2016;32:155–159. doi: 10.12669/pjms.321.8935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Vodermaier A, Lucas S, Linden W, Olson R. Anxiety After Diagnosis Predicts Lung Cancer-Specific and Overall Survival in Patients With Stage III Non-Small Cell Lung Cancer: A Population-Based Cohort Study. J Pain Symptom Manage. 2017;53:1057–1065. doi: 10.1016/j.jpainsymman.2016.12.338. [DOI] [PubMed] [Google Scholar]
- 18.Walker J, Hansen CH, Martin P, Symeonides S, Gourley C, Wall L, et al. Integrated collaborative care for major depression comorbid with a poor prognosis cancer (SMaRT Oncology-3): a multicentre randomised controlled trial in patients with lung cancer. Lancet Oncol. 2014;15:1168–1176. doi: 10.1016/S1470-2045(14)70343-2. [DOI] [PubMed] [Google Scholar]


