Abstract
Poor health information system has been identified as a major challenge in the health-care system in many developing countries including sub-Saharan African countries. Electronic health record (EHR) has been shown as an important tool to improve access to patient information with attendance improved quality of care. However, EHR has not been widely implemented/adopted in sub-Saharan Africa. This study sought to identify factors that affect the adoption of an EHR in sub-Saharan Africa and strategies to improve its adoption in this region. A comprehensive literature search was conducted on three electronic databases: PubMed, Medline, and Google Scholar. Articles of interest were those published in English that contained information on factors that limit the adoption of an EHR as well as strategies that improve its adoption in sub-Saharan African countries. The available evidence indicated that there were many factors that hindered the widespread adoption of an EHR in sub-Saharan Africa. These were high costs of procurement and maintenance of the EHR system, lack of financial incentives and priorities, poor electricity supply and internet connectivity, and primary user’s limited computer skills. However, strategies such as implementation planning, financial supports, appropriate EHR system selection, training of primary users, and the adoption of the phased implementation process have been identified to facilitate the use of an EHR. Wide adoption of an EHR in sub-Saharan Africa region requires a lot more effort than what is assumed because of the current poor level of technological development, lack of required computer skills, and limited resources.
Keywords: Adoption, Africa, barriers, electronic health record, electronic medical records, implementation, sub-Saharan Africa
Introduction
Sub-Saharan Africa is a resource-constrained region that suffers a top-heavy share of the world’s burden of disease. According to the World Health Organization (WHO), about 12% of the world’s population live in sub-Saharan Africa, yet the region suffers 27% of the world’s total burden of disease.1 To make the situation worse, the same region with a high burden of disease still lags in health information technology (HIT) which is vital in ensuring improved patients care.2,3-7 Timely as well as accurate patient information is essential to meet the health-care needs of any patient in any population. Physicians and other care providers require high quality information to make sound clinical decisions; however, their information needs are often not met.6,8 This lack of high quality information often leads to lesser quality and inefficient patient care; reporting as well as clinical research is also affected adversely.9 The critical need for good health information systems in sub-Saharan Africa has become the current focus of attention.
In recent years, there has been a growing interest in electronic medical records (EMRs) or electronic health records (EHR) adoption in many countries this is due to an increasing recognition that a stronger HIT is crucial to achieving a higher quality care at lower costs.2,4,5,7 The International Organization for Standardization (ISO) defines an EHR as a “repository of patient data in digital form, stored and exchanged securely, and accessible by multiple authorized users. It contains retrospective, concurrent, and prospective information and its primary purpose is to support continuing, efficient, and quality integrated health care.”10
EHR has been identified to be an important integral part of an efficient health-care information system that guarantees positive health outcomes.3,5,7,11
Many studies conducted in different health-care settings have indicated that EHRs will assist health professionals to reduce medical errors, achieve better effective care coordination, improve safety and quality, and also, it can reduce health-care costs.2,4,6,7,12,13 Health-care systems, similar to other industries, are information-intensive organizations.14 Health-care workers need adequate data as well as information management tools to make accurate decisions, both during patient care and management of the health-care system, and to communicate and document patient care plans.14
At present, the use of an EHR includes clinical care application/functions, clinical research function, and administrative function. The Institute of Medicine highlights that a more immediate access to computer-based clinical information, such as laboratory and radiology results, can reduce redundancy and improves quality.15 Similarly, the availability of complete patient health information at the point of care delivery, together with clinical decision support systems such as those for medication order entry can prevent many medical errors and adverse events (injuries caused by medical management rather than by the underlying disease or condition of the patient) from occurring.15,16
In addition, through a secure EHR, patient health information can be shared among all authorized users in the health-care settings. Computer-based reminder systems for patients and clinicians can improve compliance with preventive service protocols. A more advanced EHR is also crucial for various forms of biomedical and health systems research, as well as educating patients and citizens about health.15 Furthermore, the study conducted by Hillestad et al. on the potential health benefits and cost savings benefit of EHR adoption revealed that broad implementation of EHR would reduce health-care costs by more than $81 billion yearly in the United States.17 Overall, the significance of EHR in improving patient safety and quality care, reducing medical errors and health-care costs cannot be overstressed so also the benefits of its broad adoption in sub-Saharan Africa.
Several industrialized nations such as Canada, United Kingdom, and the United States of America have either implemented or are in the process of implementing an EHR system because of its possible benefits.6,7,11 However, there is a limited adoption of EHR in sub-Saharan African countries, despite the huge benefits arising from its usage. The study conducted by Akanbi et al. on the use of EHR in sub-Saharan Africa showed that the use of EHRs in sub-Saharan Africa is largely driven by HIV treatment international programs such as President’s Emergency Plan for AIDS Relief HIV program.18 Implementation is still, however, very low.5,7,18 In addition, many of the most commonly available electronic functionalities with EHR in this region are more administrative, rather than clinical.18
The factors that limit the implementation of EHR in different health-care settings in this region have not been widely studied. Therefore, to bridge this gap, this paper reviewed both the challenges that hinder its wider adoption in the region and the factors that facilitate its implementation in the few piloted projects or few sub-Saharan countries that have minimally adopted it. Identifying factors that affect EHR adoption in this part of the world is essential to inform all health stakeholders, policy makers, researchers, and academic health institutions that train medical doctors, pharmacist, nurses, laboratory scientists, and just to mention a few. To answer the question of why low adoption of EHR in this region, it is imperative to identify and understand the factors that limit broad adoption of EHR. Besides, to accelerate wider implementation of EHR, there is a need to have a better understanding of the EHR adoption facilitating factors.
Methods
A comprehensive literature search was conducted on two electronic databases: PubMed and Medline. The Google Scholar search engine was also utilized as well as organizations’ websites such as those of the WHO and ISO. To facilitate the search, the following keywords were used: Sub-Saharan Africa, EHR, Africa, EMR, developing countries, names of each country in the sub-Saharan African region, facilitating factors, barriers, EHR adoption, and implementation.
Inclusion and exclusion criteria
Publications of interest were those published in English and with information on factors that limit the implementation/adoption of EHR as well as factors/strategies that improve its adoption in sub-Saharan Africa. Exclusion criteria were studies that were not published in English as well as those that were not related to sub-Saharan African countries.
Search outcomes
About 47 papers were retrieved. Duplicate papers in the databases were deleted. After screening of abstracts and application of the inclusion and exclusion criteria, 15 papers were included in the final review. Figure 1 summarizes the search strategies and search outcomes. Inclusion and exclusion criteria were based on matching types of evidence to research purposes on the basis of their relevance and quality of individual studies.
Figure 1.
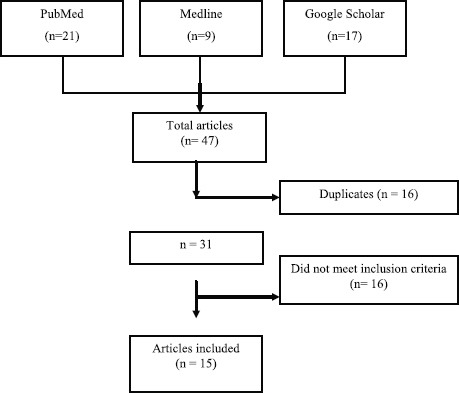
Search strategies and search outcomes
In assessing the quality of the included studies, the criteria from Dixon-Woods et al. were adopted, so as to exclude the papers that are fatally flawed.19 The appraisal prompts for informing judgments about the quality of papers are as follows:
Are the aims and objectives of the research clearly stated?
Is the research design clearly specified and appropriate for the aims and objectives of the research?
Do the researchers display enough information to support their interpretations and conclusions?
Is the method of analysis appropriate and adequately explicated?
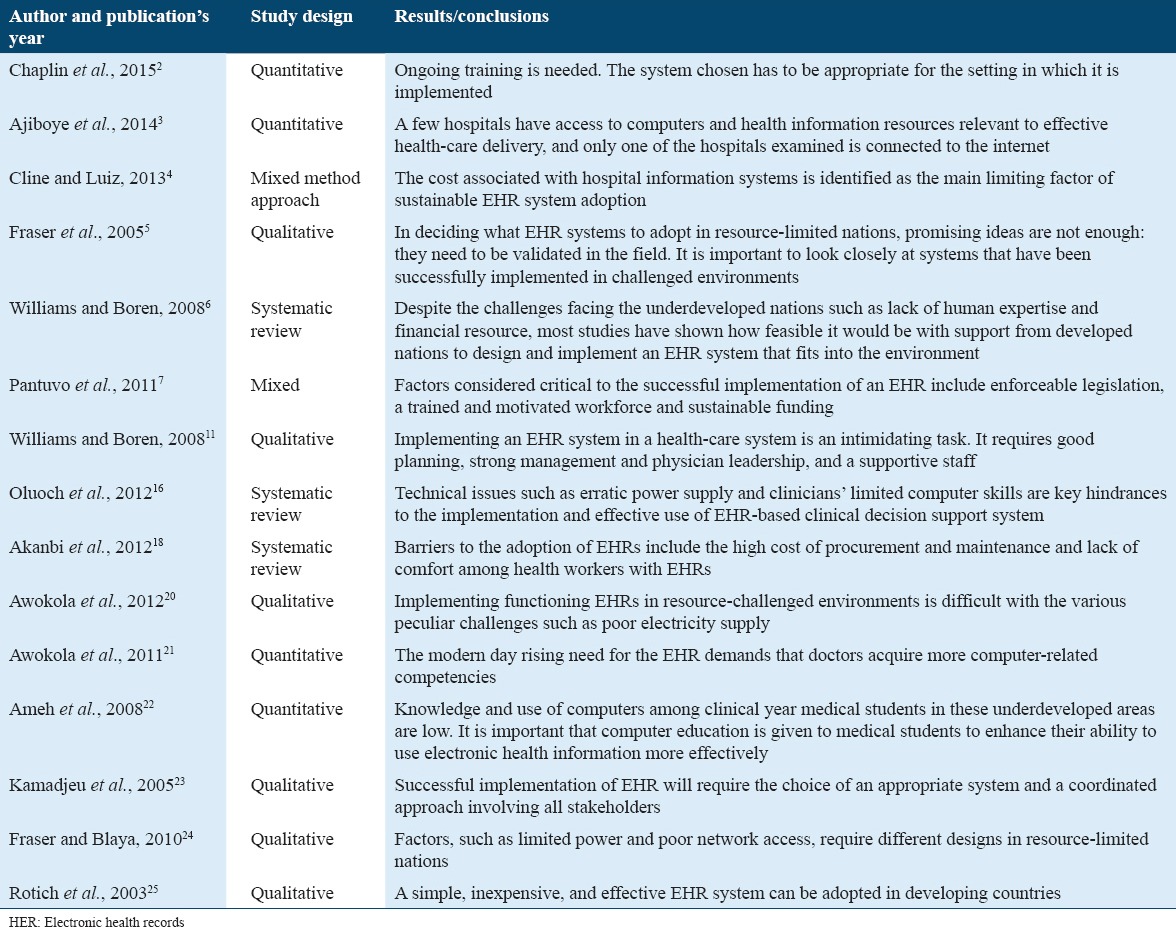
No papers were excluded in respect of quality. 15 studies included were of different study designs ranging from quantitative to qualitative to systematic review to mixed designs. Table 1 summarizes a list of the 15 articles included in the review.
Table 1.
List of reviewed articles
Results
The following section presents the findings from the reviewed articles.
The main barriers to adoption of the EHR in sub-Saharan Africa that emerged from the studies reviewed are grouped under four themes.
High implementation and maintenance costs
The cost of EHR implementation is one of the most frequently identified factors that limit EHR adoption. Studies have shown that low adoption of EHR in sub-Saharan Africa can be linked to high costs of implementation and maintenance due to hardware, software, training, and support costs.18,20 Many hospitals and physicians in sub-Saharan African countries were mainly concerned about the large capital outlay5-7,11,18,20 associated with hardware, software, and installation; broadband connection costs; the cost of accessories such as scanners, printers, paper, and ink; and recurring expenses for system maintenance. Furthermore, Akanbi et al. stated that lack of robust/poor infrastructure in developing nations also increased both the costs of setting up EHR and costs of maintenance.6,11,18 Awokola et al. pointed out that the software used in health-care establishments is very expensive and that a basic EHR costs about $32,000 excluding technical support and ongoing maintenance.20 As a result of high costs of EHR procurement, many hospitals, though beneficial in a number of other ways, did not see EHR implementation as a priority.20
Limited computer skills
Low computer literacy level is another variable that clearly emerged from the articles reviewed as one of the potent factors that limit the wider adoption of EHR in sub-Saharan African countries. Physicians reported a series of skill-related factors that they believe would make it difficult to use an EHR. These included lack of typing proficiency, low/no understanding of how to use a computer, lack of understanding of how to use the EHR system, and inability to type while talking with patients.4,21,22 The study conducted on computer and internet use by doctors in one of the sub-Saharan African countries showed that the overall proficiency of the respondents in computer based competencies was below average. Only 32 (26.7%) were sufficiently familiar with computer tools to perform advanced tasks.21 The researchers stated further that the Appalachian Regional Informatics Consortium Survey of 2005 in Ohio, United States, showed that 91.4% of doctors could use an EHR. In the Canadian Medical Association physician resource survey of 2000, 84% of doctors showed computer use proficiency. Similarly, higher values were seen in a study of student doctors in Malaysia in 2002, where 94.4% of the subjects could use a computer well.21 As a result, of low-level computer literacy in the sub-Saharan African countries, many physicians and other key end users are not eager/willing to adopt an EHR and ultimately low EHR adoption in the region.
Poor electricity supply and lack of constant internet connectivity
Lack of constant supply of electricity has also been identified by many researchers as a major barrier to a successful wider implementation and adoption of EHR in this region.7,11,16,20 For instance, Awokola et al., reported that for many months, they could not use the EHR consistently because of the constant power outage. In addition, Pantuvo et al. stated that many hospitals in this region do not have access to constant electricity supply.7 In fact, many hospitals depend mainly on the alternative power supply commonly called “generator” for their operations. Due to the infrastructure issues all through the nation and absence of guaranteed internet connection or even uncertain continuous power supply,2,7,11 a wider implementation of EHR in some sub-Saharan nations may not be conceivable.
Furthermore, the study conducted on the use of health information and communication technologies by health workers in seven state hospitals and a private hospital in the North Eastern Zone, Ogun State, Nigeria, reported that only one of the hospitals examined was connected to the internet, and none of them had a website.3 Jimoh et al. noted that the internet penetration was very low. For instance, the internet penetration of <16% and average broadband download speed of 1.38 mbps (compared with 10.1 mbps the United States.26 Overall, poor electricity supply and lack of constant internet connectivity have been reported as strong barriers to EHR adoption in this region.
Lack of prioritization of EHR
Studies have shown that most developing countries face many challenges ranging from disease epidemics to civil wars to disasters so EHR implementation may seem outside the priority agenda in this region.6,11,17 Akanbi et al. revealed that most EHRs in this region were sustained by funding from foreign partnerships, thereby raising the question about the sustainability of these systems by the domestic institutions. Many countries in sub-Saharan Africa did not have a specific policy in place on EHR adoption and no financial incentives for adoption.6,11,17,18
Factors Facilitating EHR Implementation in sub-Saharan Africa
The following section presents the strategies that enabled the adoption of EHR in the few piloted projects or few sub-Saharan countries that have minimally adopted it.
Implementation Planning
Comprehensive planning before implementation was frequently cited in literature. Planning steps included setting realistic goals and expectations, involving EHR users early in the planning process, determining how current workflows will be redefined with EHRs, system selection, staged implementation processes, and learning from facilities that have implemented EHR systems.7,11,24
Training and Education
Training of EHR users was also reported in studies to be an effective strategy for getting end users’ acceptance. Training should be both initial and ongoing.2,11,24 Physicians and other EHR end users have to set time aside to study how the system is operated and how their workflow should be redesigned to allow for an efficient use of the system. Training, however, should commence with the most interested EHR users, the so-called local champions who will subsequently be used to motivate the others and developed to “super users” to handle most basic hardware and software problems locally.24 Equally, incorporation of health informatics into the school curriculum by the academic health institutions that train medical doctors, pharmacist, nurses, laboratory scientists, and other health workers were frequently mentioned by researchers.7,13
Financial Supports
In addition, literature supports the notion that financial assistance from the government to cover implementation costs. This can be in the form of grants or one-time payments for infrastructure and hardware costs, reimbursement incentives. Many researchers pointed out that some form of government incentives would be required to see substantial adoption and meaningful use of EHR in sub-Saharan African countries.7,12
Appropriate EHR System Selection
Studies have shown that while it is true that the cost of implementation of an EHR can be prohibitive for most developing countries, the use of low-cost technologies has been demonstrated to be sustainable in many such countries.5,7,12,23,25 “The functionality of EHR systems varies across multiple settings. To be most useful, a functional model of an EHR system must reflect a balance between what is desirable and what can feasibly be implemented immediately or within a short time frame.”15
Phased Implementation
Another strategy that facilitates EHR adoption in sub-Saharan Africa is the embracing of phased implementation. According to Pantuvo et al., a phased implementation involves implementing one unit at a time. The author stated that “a phased implementation is preferred for resource-constrained areas where the resources to tackle all the issues that implementation will raise are not readily available. This gives room to manage changes in small units and transfer lessons learned to other units.”7
Discussion
There are many reasons why hospitals/clinics in sub-Saharan African countries might not be adopting EHRs despite the immense benefits of improving patient safety and quality of care, reduce medical errors, decrease health-care cost, greater efficiency, and enhanced care coordination.27 The most frequently reported major factors that limit EHR implementation in sub-Saharan African countries are as follows: High initial and ongoing maintenance costs, lack of financial incentives for adoption, lack of priorities, poor electricity supply, lack of internet connectivity, low computer literacy level, and some of these identified factors are similar to findings in developed part of the world. For instance, the study conducted by Abramson et al. in the United States reported that major barriers to EHR adoption are the initial cost of IT, lack of fiscal incentives for EHR adoption, lack of interoperability with current systems, ongoing maintenance costs, and competing priorities.28
However, it should be noted that some of the most important barriers to EHR adoption in sub-Saharan African countries identified are typical to this region, and other developing countries. For example, poor electricity supply, inadequate/lack of internet connectivity, and lower computer literacy level issues that are identified in the reviewed research studies in this region, but these factors have not been identified as barriers to EHR adoption in many developed countries. Identifying factors that affect EHR adoption in this part of the world is essential to inform all health stakeholders, policy makers, researchers, and academic health institutions. The findings in this review have provided valuable information in this regard. This review is very useful, given that poor resource-constrained countries are traditionally described as lagging behind other developed countries in the health-care sector so having a better understanding of the limiting factors of EHR adoption in the sub-Saharan Africa will serve as a platform for improvement to achieve the desired goals and objectives of wider EHR implementation in the region.
As with any study, this review has limitations. The available evidence does not represent all countries in sub-Saharan African region equally, thereby limiting generalization of the findings. Due to the heterogeneity of the study design of the reviewed articles, no statistical analysis was conducted. The major strength of this desk study is that it comprises studies which have used different study designs to triangulate the result to provide knowledge about factors affecting and promoting EHR adoption. This effort of triangulation results in deeper and better understanding of these factors.
Conclusions
EHR has been shown to play significant roles in improving health-care information system. The main drivers for the increasing interest in EHR include the need to improve efficiency in health-care service delivery, improve patient safety, increase access to health-care services, and more importantly, the need to reduce the costs of medical expenditures. However, there are many factors that limit broad adoption of EHR in sub-Saharan Africa. These include high initial costs of procurement of EHR system and ongoing maintenance costs, lack of financial incentives for adoption, lack of priorities, poor electricity supply, lack of internet connectivity, primary user’s limited computer skills, and lack of robust health-care infrastructure.
Therefore, any efforts that will be directed toward widespread adoption of EHR in this region by any stakeholders must be tackled at a much more fundamental level within the context of sub-Saharan African region and uniqueness of the region’s present situation. The following strategies have been shown to promote EHR adoption: Proper and adequate implementation planning, financial supports from the government, appropriate EHR selection, training of primary users, and adoption of the phased implementation process. Improved efforts such as the inclusion of the biomedical informatics program in medicine, pharmacy, nursing, and other potential users of EHR curricular and establishment of computer laboratories are required to increase the student’s access to computers and the internet. Early involvement of stakeholders to build up the requirements of end users and reduce resistance to change is highly recommended. The perceived benefits of EHR should be identified and communicated to stakeholders as much as possible. The building of robust health-care infrastructures should be taken more seriously in this region.
References
- 1.World Health Organization. Core Health Indicators. 2008. [[Last accessed on 2015 Sep 02]]. Available from: http://www.apps.who.int/whosis/database/core/core_select_process.cfm .
- 2.Chaplin B, Meloni S, Eisen G, Jolayemi T, Banigbe B, Adeola J, et al. Scale-up of networked HIV treatment in Nigeria: Creation of an integrated electronic medical records system. Int J Med Inform. 2015;84:58–68. doi: 10.1016/j.ijmedinf.2014.09.006. [DOI] [PubMed] [Google Scholar]
- 3.Ajiboye BA, Adekoya AJ, Alawiye MK, Oyedipe WJ. Knowledge and utilization of health information and communication technologies (HICTs) by health workers of the North-Eastern health zone of Ogun State, Nigeria. Inform Health Soc Care. 2014;39:104–23. doi: 10.3109/17538157.2013.858044. [DOI] [PubMed] [Google Scholar]
- 4.Cline GB, Luiz JM. Information technology systems in public sector health facilities in developing countries: The case of South Africa. BMC Med Inform Decis Mak. 2013;13:13. doi: 10.1186/1472-6947-13-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Fraser HS, Biondich P, Moodley D, Choi S, Mamlin BW, Szolovits P. Implementing electronic medical record systems in developing countries. Inform Prim Care. 2005;13:83–95. doi: 10.14236/jhi.v13i2.585. [DOI] [PubMed] [Google Scholar]
- 6.Williams F, Boren SA. The role of the electronic medical record (EMR) in care delivery development in developing countries: A systematic review. Inform Prim Care. 2008;16:139–45. doi: 10.14236/jhi.v16i2.685. [DOI] [PubMed] [Google Scholar]
- 7.Pantuvo JS, Naguib R, Wickramasinghe N. Towards implementing a nationwide electronic health record system in Nigeria. Int J Healthc Deliv Reform Initiatives. 2011;3:39–55. [Google Scholar]
- 8.Simba DO, Mwangu M. Application of ICT in strengthening health information systems in developing countries in the wake of globalisation. Afr Health Sci. 2004;4:194–8. [PMC free article] [PubMed] [Google Scholar]
- 9.Monda J, Keipeer J, Were MC. Data integrity module for data quality assurance within an e-health system in sub-Saharan Africa. Telemed J E Health. 2012;18:5–10. doi: 10.1089/tmj.2010.0224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.International Organization for Standardization ISO/DTC 20514. Health Informatics-Electronic Health Record-Defination, Scope, and Context 2005. [[Last accessed on 2015 Apr 03]]. Available from: https://www.iso.org/obp/ui/#iso:std:39525:en .
- 11.Williams F, Boren SA. The role of electronic medical record in care delivery in developing countries. Int J Inf Manage. 2008;28:503–7. doi: 10.1016/j.ijinfomgt.2008.01.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Blaya JA, Fraser HS, Holt B. E-health technologies show promise in developing countries. Health Aff (Millwood) 2010;29:244–51. doi: 10.1377/hlthaff.2009.0894. [DOI] [PubMed] [Google Scholar]
- 13.Castelnuovo B, Kiragga A, Afayo V, Ncube M, Orama R, Magero S, et al. Implementation of provider-based electronic medical records and improvement of the quality of data in a large HIV program in Sub-Saharan Africa. PLoS One. 2012;7:e51631. doi: 10.1371/journal.pone.0051631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Shortliffe EH, Cimino JJ. Biomedical Informatics: Computer Applications in Healthcare and Biomedicine. New York, NY: Springer; 2014. pp. 1–43. [Google Scholar]
- 15.Institute of Medicine. Key Capabilities of an Electronic Health Record System: Letter Report. Washington, DC: The National Academies Press; 2003. pp. 1–36. [PubMed] [Google Scholar]
- 16.Oluoch T, Santas X, Kwaro D, Were M, Biondich P, Bailey C, et al. The effect of electronic medical record-based clinical decision support on HIV care in resource-constrained settings: A systematic review. Int J Med Inform. 2012;81:e83–92. doi: 10.1016/j.ijmedinf.2012.07.010. [DOI] [PubMed] [Google Scholar]
- 17.Hillestad R, Bigelow J, Bower A, Girosi F, Meili R, Scoville R, et al. Can electronic medical record systems transform health care? Potential health benefits, savings, and costs. Health Aff (Millwood) 2005;24:1103–7. doi: 10.1377/hlthaff.24.5.1103. [DOI] [PubMed] [Google Scholar]
- 18.Akanbi MO, Ocheke AN, Agaba PA, Daniyam CA, Agaba EI, Okeke EN, et al. Use of electronic health records in sub-Saharan Africa: Progress and challenges. J Med Trop. 2012;14:1–6. [PMC free article] [PubMed] [Google Scholar]
- 19.Dixon-Woods M, Cavers D, Agarwal S, Annandale E, Arthur A, Harvey J, et al. Conducting a critical interpretive synthesis of the literature on access to healthcare by vulnerable groups. BMC Med Res Methodol. 2006;6:35. doi: 10.1186/1471-2288-6-35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Awokola BI, Abioye-Kuteyi EA, Otoru OO, Oyegbade OO, Awokola EO, Awokola OA, et al. Practical challenges of setting up an electronic medical record system in a Nigerian tertiary hospital: The wesley guild hospital experience. Middle East J Fam Med. 2012;7:37–42. [Google Scholar]
- 21.Awokola BI, Abioye-Kuteyi EA, Ogundele OA, Awokola EO. Computer and internet use by doctors in a Nigerian Teaching Hospital: A survey of the wesley guild unit of Obafemi Awolowo University Teaching Hospitals complex. Middle East J Fam Med. 2011;9:17–21. [Google Scholar]
- 22.Ameh N, Kene TS, Ameh EA. Computer knowledge amongst clinical year medical students in a resource poor setting. Afr Health Sci. 2008;8:40–3. [PMC free article] [PubMed] [Google Scholar]
- 23.Kamadjeu RM, Tapang EM, Moluh RN. Designing and implementing an electronic health record system in primary care practice in sub-Saharan Africa: A case study from Cameroon. Inform Prim Care. 2005;13:179–86. doi: 10.14236/jhi.v13i3.595. [DOI] [PubMed] [Google Scholar]
- 24.Fraser HS, Blaya J. Implementing medical information systems in developing countries, what works and what doesn't. AMIA Annu Symp Proc. 2010;2010:232–6. [PMC free article] [PubMed] [Google Scholar]
- 25.Rotich JK, Hannan TJ, Smith FE, Bii J, Odero WW, Vu N, et al. Installing and implementing a computer-based patient record system in sub-Saharan Africa: The Mosoriot Medical Record System. J Am Med Inform Assoc. 2003;10:295–303. doi: 10.1197/jamia.M1301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Jimoh L, Pate MA, Lin L, Schulman KA. A model for the adoption of ICT by health workers in Africa. Int J Med Inform. 2012;81:773–81. doi: 10.1016/j.ijmedinf.2012.08.005. [DOI] [PubMed] [Google Scholar]
- 27.Odekunle FF. Current roles and applications of electronic health record in the healthcare system. [[Last accessed on 2016 Dec 11]];Int J Med Res Health Sci. 2016 5:48–51. Available from: http://www.ijmrhs.com/current-roles-and-applications-of-electronic-health-record-in-the-healthcare-system . [Google Scholar]
- 28.Abramson EL, McGinnis S, Moore J, Kaushal R. A statewide assessment of electronic health record adoption and health information exchange among nursing homes. Health Serv Res. 2014;49:361–72. doi: 10.1111/1475-6773.12137. [DOI] [PMC free article] [PubMed] [Google Scholar]


