Abstract
Objective:
Percutaneous coronary intervention has been effective in increasing longevity of patients with cardiovascular disease. However, the evidence shows that the quality of life after the intervention is still lower than optimal level. The quality of life can be affected by various factors. The aim of this study is to determine the quality of life and its related factors in patients undergoing coronary angioplasty.
Methods:
This cross-sectional study was performed on 106 patients undergoing coronary angioplasty during 2015-2016. This study population included all patients who referred to a cardiac clinic in Rasht, Iran, were passed 3 months after their angioplasty. Research samples met the inclusion criteria and were willing to participate to the study, were selected gradually (continually). Research tools were a self-structured questionnaire regarding factors associated with the quality of life and the MacNew quality of life questionnaire. Data were collected through asking patients questions and using patient’s medical records. Data analysis was conducted using descriptive and inferential statistics.
Results:
The results of multivariate linear regression analysis showed that independent variables of age (P = 0.0001), the number of diseased vessels (P = 0.0001), and the number of comorbidities (P < 0.05) were the most important factors associated with the quality of life.
Conclusion:
Health-care professionals can play an effective role in promoting the quality of life of patients undergoing coronary angioplasty by modifying lifestyle based on the related factors and to provide comprehensive care programs, especially for elderly.
Keywords: Cardiovascular disease, percutaneous coronary artery intervention, quality of life
Introduction
Cardiovascular diseases (CVDs (have still remained the most common diseases and the leading cause of death worldwide. It has been predicted to be the cause of 30.5% of the world death toll by the year 2030.1 In Iran, CVD is one of the main causes of mortality and morbidity and the first cause of death in people over 45 years (26% of the total deaths).2
Nowadays, there are valuable therapeutic strategies such as medication and coronary artery bypass grafting surgery for the treatment of coronary heart disease as the main manifestation of CAD. However, angioplasty is still the most common method of treatment.3 Evidences have shown improved cardiovascular events with early percutaneous coronary intervention (PCI).4 However, what eventually is obtained and remained for the patient following a medical or surgical treatment, is the best and major criterion for judging the effectiveness of that treatment. Health-related quality of life assessment of patients is an indicator for evaluating the effectiveness of medical interventions.5
The World Health Organization defines the quality of life as “individual’s perception of their position in life in the context of the culture and value systems in which they live and in relation to their goals, ambitions, standards and interests.”6 Person’s position is influenced by physical health, psychological status, personal beliefs, social communications, and relationships with important people in a complex way. The quality of life reflects secondary psycho-emotional benefits for the patient. The decrease in physical limitations, improvement of perception, and health status are the benefits of a successful coronary angioplasty.7 Therefore, it is expected that the quality of life will be promoted in the patients with coronary artery after PCI.
Although PCI is an effective method in the treatment of heart disease, health-related quality of life after angioplasty seems not to be desirable.8 In fact, treatment in the patients with coronary artery problems is not considered a real and achievable goal; because the disease is debilitating with a progressive course, and multiple internal and external factors have impact on the escalation and improvement of the disease. These characteristics obviously influence the patients’ quality of life.9 The literature review is showed disparate results regarding some of the factors related to the quality of life in the patients undergoing angioplasty.10-12 Therefore, this study was performed to determine factors associated with quality of life in these patients. Identifying these factors can help to design education programs and appropriate interventions to promote the quality of life in the patients undergoing angioplasty.
Methods
This cross-sectional study was conducted on 106 patients referred to a cardiac clinic who attended the follow-up visit 3 months after coronary angioplasty during 2015-2016 in Rasht, Iran. 101 participants were calculated based on a previous study13 and considering σ = 3.6, α = 0.05, β =0.2, µ1-µ0 =1 as the following Formula:
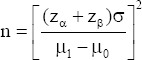
However, we recruited 110 participants to achieve more reliable results. The samples were selected through the consecutive convenience sampling with the inclusion criteria included age older than 18 years, the absence of mental disorders, being first-time angioplasty patient, and being candidate for receiving service from a certain specialist. The reason for selecting the patients of a specialist was to be control the possible effects of patient education after angioplasty and physician follow-up program on the patients’ quality of life. After obtaining ethical approval to conduct the study and getting permission from administrators, the researcher daily attended the clinic and extracted the list of patients referred to visit after 3 months of their angioplasty, and after self-introduction and assessing the samples in terms of the eligibility of inclusion criteria, provided the necessary explanations about the study to the participants in a peaceful place and separately. Furthermore, a written informed consent was obtained. Then, asking the participants questions, the questionnaires were completed. Using patients’ medical records and statements, information on the factors related to the disease was obtained. Of the 110 people who were on the initial list, 4 patients did not consent to complete the questionnaire. Therefore, the data of 106 people were analyzed. The MaCnew Heart Disease Health-related quality of life instrument was used to determine the participants’ quality of life. This instrument developed specifically to measure the quality of life of patients with heart disease, consists of 27 questions in three subscales: Emotional functioning, physical functioning, and social functioning. 14 questions are in the field of physical functioning, 14 questions are in the field of emotional functioning, and 13 questions are in the field of functioning. 5 questions on the physical functioning subscale evaluate the symptoms of the disease. Allocation of questions in the questionnaire is in a way that each question can be considered in one, two, or all three domains. The total score is calculated by calculating the scores of all questions. Each of the questions of the questionnaire has a 7-point scale ranging from “always” to “never.” The highest score on each question is seven, and the lowest score is one which represents the best condition and the worst condition, respectively. The scores of physical functioning domain and emotional functioning domain, each one are between 14 and 98, the score of social functioning domain is between 13 and 91 and the total score of questionnaire is between 27 and 189. The questionnaire has been translated into Persian and localized by Asadi-Lari et al. Its validation was conducted through the face validity and content validity, and its reliability was calculated by Cronbach’s alpha coefficient that was 0.95.14 Charlson comorbidity questionnaire was used to determine number of comorbidities on the basis of medical diagnosis.15 Factors associated with disease were selected through the literature review. After collecting data, the descriptive (mean, standard deviation, and frequency distribution table) and inferential statistics (t-test, ANOVA, Pearson’s correlation coefficient, and linear regression) were used to determine factors related to the quality of life in patients undergoing angioplasty.
Results
Most of patients were in the age group over 60 years (39.6%), male (67.9%), married (88.7%), resident in urban area (84%), and under diploma (62.3%) (Table 1).
Table 1.
Patients’ characteristics
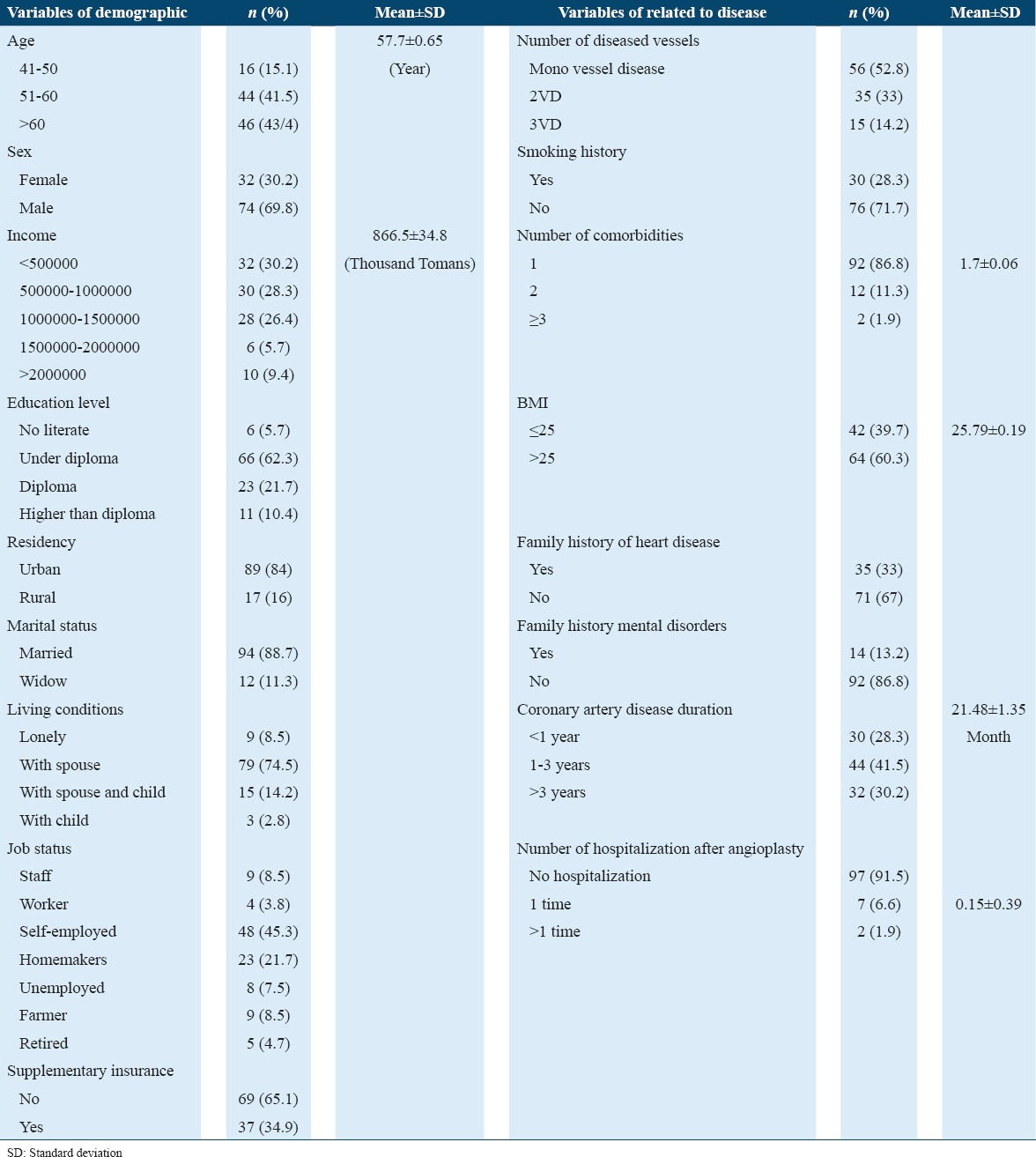
The mean score of the patients’ quality of life was 67.16 ± 12.04 (social functioning), 64.33 ± 8.73 (physical functioning), 65.45 ± 9.31 (emotional functioning), and 126.6 ± 15.99 (total quality of life). Furthermore, the mean score of quality of life was higher in the age group 41-50 years (129.59 ± 12.74), men (131.46 ± 15.31), those earning more than two million Tomans (137.66 ± 15.85), level of education of higher than diploma (142.63 ± 9.38), resident in urban area (127.46 ± 15.95), married (130.0 ± 19.2), self-employed people (138.88 ± 15.48), those living with their wives and children (136.66 ± 16.77), and those with supplementary insurance (129.45 ± 17.44). There was a statistically significant relationship between scores of quality of life and age (P = 0.0001), gender (P = 0.039), and level of education (P = 0.004) (Table 2).
Table 2.
Relation demographic factors with QOL score of the patients
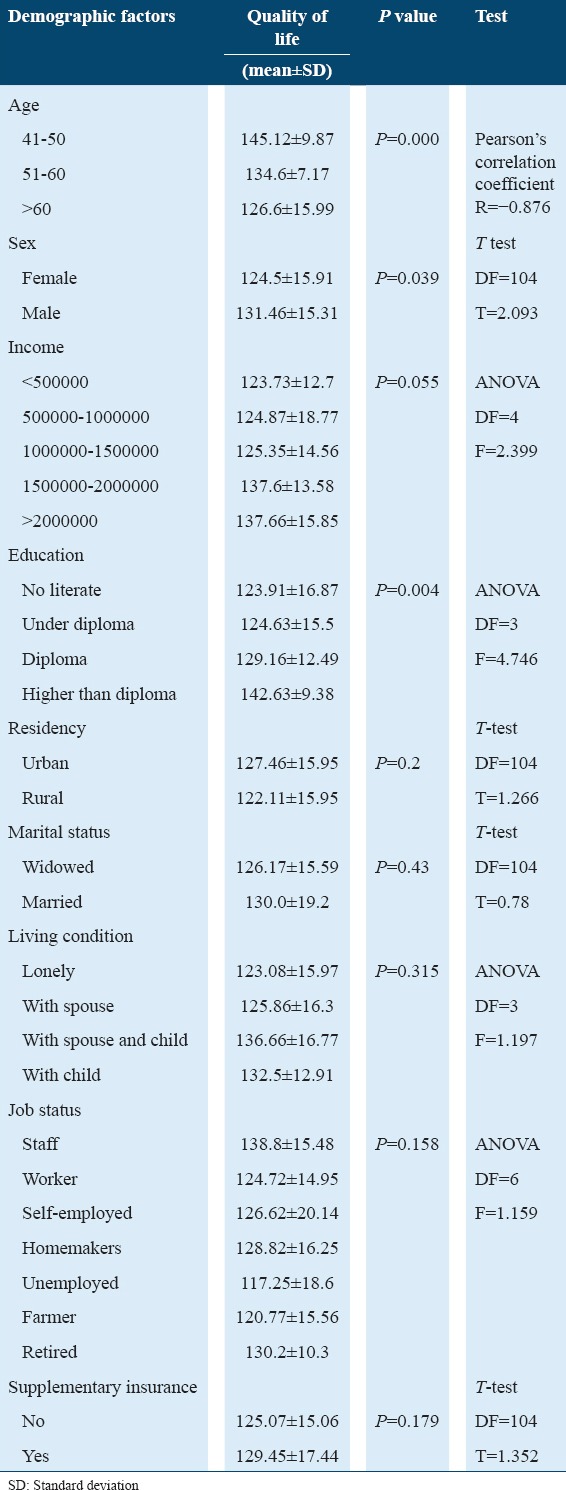
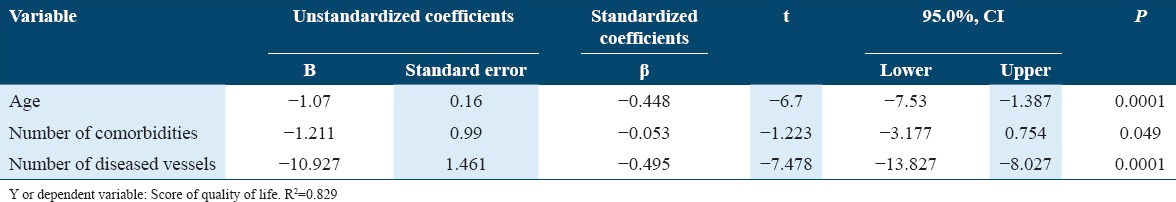
Mean score of patients’ quality of life was higher in non-smokers (128.72 ± 16.71), non-obese people (130.05 ± 15.17), mono vessel disease (VD) (138.3 ± 8.88), a history of 1-3-year heart disease (126.95 ± 16.11), those with no history of hospitalization after angioplasty (133.75 ± 11.16), those with the least number in the comorbidity (131.28 ± 12.93), history of heart disease (129.22 ± 14.67), and those with no mental disorders in the family (133.92 ± 13.5). There was statistically significant relationship between score of quality of life and smoking history (P = 0.029), body mass index (P = 0.018), number of diseased vessels (P = 0.0001), comorbidities (P = 0.012), and a family history of heart disease (P = 0.024) (Table 3). Results of multivariate linear regression showed that age (P = 0.0001), the number of diseased vessels (P = 0.0001), and the number of comorbidities (P < 0.05) are the most important factors associated with the quality of life in patients undergoing angioplasty (Table 4).
Table 3.
Relation-related disease factors with QOL score of the patients
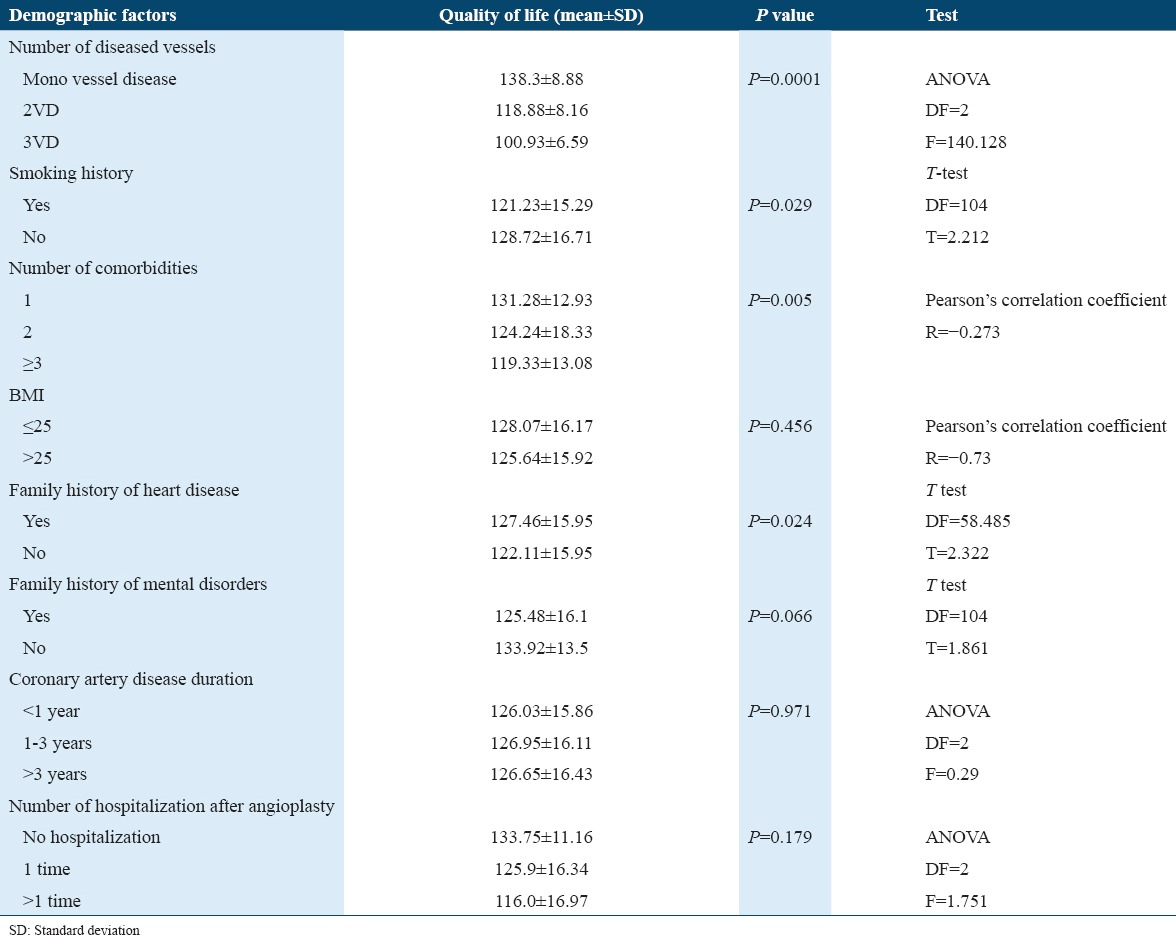
Table 4.
Estimated regression coefficients from the multiple linear regression models to predict quality of life from related factors
Discussion
The quality of life in the women was lower than men. Similarly, a study has reported the relationship between gender and the quality of life.12 It is not clearly recognized that why the quality of life between men and women is different. Psychological factors, different women’s perceptions of the symptoms, and health indicators have been considered as the causes of this difference.16
People with higher level of education had the better quality of life. This relationship has been shown in many studies.17,18 Education changes people’s attitude and knowledge to health and can lead to improve the quality of life.
The quality of life in married people was higher than widows. However, there was no association between marital status and quality of life. A study has reported a relationship between these two variables.19 Using different tools in the studies may be a reason for the differences.
People living with their spouses and children had the highest level of quality of life, and lonely individuals had the lowest level of quality of life. Evidences have shown that lonely people have lower level of quality of life than people with sources of support, such as spouse and children.17,19
People who were unemployed had lower quality of life. However, a significant relationship was not observed between job status and quality of life. While a study was reported the relationship between job status and quality of life.20 Perhaps, the reason is related to low number of unemployed people, and larger sample size is needed to assess this association.
Non-smokers had higher level of quality of life, and there was a relationship between smoking and the quality of life. Smoking increases the risk of myocardial infarction and death in patients with heart disease, especially after angioplasty. Smoking limits vascular reconstruction and the maintenance of coronary blood flow by creating microvascular endothelial dysfunction. Furthermore, smoking reduces the ability of individuals to exercise after angioplasty.21 Thus, smoking can reduce the quality of life of patients after angioplasty.
People with mono-VD had higher quality of life than others. This finding is consistent with a study.22 Number of vessels affected, as a reflection of disease severity, is the most important determinant of the quality of life.23
Patients with more comorbidities had worse quality of life. This finding is compatible with many studies.17,22 Comorbidities are the most powerful predictors of mental and physical health and therefore quality of life in the patients with heart disease.11
There was an association between family history of heart disease and quality of life. In a study, individuals who had a positive family history of the disease had better physical functioning.24 Knowledge of patients with positive family history of the disease concerning self-care and the importance of self-care can affect their quality of life.
People with hospitalization after angioplasty had a lower level of quality of life than others. However, there was a relationship between the history of hospitalization after angioplasty and quality of life. In contrast, a study has reported an association between the quality of life and the number of hospitalization after therapeutic interventions (surgery).20 Differences in results may be explained by the difference in type of intervention and the fact that the majority of our participants in this study were not readmitted after angioplasty. However, according to Johansson’s results, the patients with undesirable quality of life are more likely to be readmitted frequently because over time, they experience multiple and severe symptoms leading to urgent readmission.25
People, who had a family history of mental disorder, had lower score of quality of life than those who had no family history of mental disorder. However, there was no significant relationship between these two variables. Family support influences individuals’ quality of life.26 Therefore, it is expected that if family members have mental disorders, person will not receive the necessary support resulting in reduced quality of life.
People with a higher body mass index had lower level of quality of life. However, a significant association was not observed between the quality of life and body mass index. This finding is consistent with results of Martin’s study.27 However, in a study, the score of quality of life obtained through EuroQOL-5D instruments, significantly decreased only in those who had a high BMI.28 The instruments that were used in these studies to measure the quality of life were different from each other and from our study. Contradictory results observed in terms of the relationship between two variables may be related to difference in the quality of life assessment instruments. Therefore, it is required to design and develop a more comprehensive tool for measuring the quality of life in patients with heart disease. Participants’ fatigue resulting from the waiting time for follow-up visit, could affect their responses to the questions. Hence, we tried to be completed questionnaires in the early hours of entering the clinic and in a quiet environment.
Conclusion
In general, at this study, age, the number of comorbidities, and the number of diseased vessels were determined as the most important factors associated with patients’ quality of life after angioplasty. Accordingly, it seems to be necessary to pay special attention to the elderly people when planning the self-care educational programs after angioplasty. Health-care professionals can play an effective role in promoting the quality of life of patients undergoing coronary angioplasty through raising awareness creating health beliefs in the field of a healthy lifestyle as well as, taking into account the specific circumstance of each individual in terms of the number of comorbidities and the number of diseased vessels to develop the self-care and educational programs. Desirable quality of life is an inalienable individuals’ right in any society, and health-care professionals have a vital role in achieving this through awareness of factors associated with the quality of life.
Acknowledgments
This project was funded by the Research and Technology Deputy of Guilan University of Medical Sciences. We thank colleagues in Heshmat hospital and patients.
References
- 1.Lozano R, Naghavi M, Foreman K, Lim S, Shibuya K, Aboyans V, et al. Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: A systematic analysis for the global burden of disease study 2010. Lancet. 2012;380:2095–128. doi: 10.1016/S0140-6736(12)61728-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Saadat S, Yousefifard M, Asady H, Moghadas Jafari A, Fayaz M, Hosseini M. The most important causes of death in Iranian population;a retrospective cohort study. Emerg (Tehran) 2015;3:16–21. [PMC free article] [PubMed] [Google Scholar]
- 3.Sharif F, Moshkelgosha F, Molazem Z, Najafi Kalyani M, Vossughi M. The effects of discharge plan on stress, anxiety and depression in patients undergoing percutaneous transluminal coronary angioplasty: A randomized controlled trial. Int J Community Based Nurs Midwifery. 2014;2:60–8. [PMC free article] [PubMed] [Google Scholar]
- 4.Al Shammeri O, Garcia L. Thrombolysis in the age of primary percutaneous coronary intervention: Mini-review and meta-analysis of early PCI. Int J Health Sci (Qassim) 2013;7:91–100. doi: 10.12816/0006026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ruano-Rodríguez C, Serra-Majem L, Dubois D. Assessing the impact of dietary habits on health-related quality of life requires contextual measurement tools. Front Pharmacol. 2015;6:101. doi: 10.3389/fphar.2015.00101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sischo L, Broder HL. Oral health-related quality of life: What, why, how, and future implications. J Dent Res. 2011;90:1264–70. doi: 10.1177/0022034511399918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chaudhury S, Srivastava K. Relation of depression, anxiety, and quality of life with outcome after percutaneous transluminal coronary angioplasty. ScientificWorldJournal. 2013;2013:465979. doi: 10.1155/2013/465979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kim MJ, Jeon DS, Gwon HC, Kim SJ, Chang K, Kim HS, et al. Health-related quality-of-life after percutaneous coronary intervention in patients with UA/NSTEMI and STEMI: The Korean multicenter registry. J Korean Med Sci. 2013;28:848–54. doi: 10.3346/jkms.2013.28.6.848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lukkarinen H, Hentinen M. Treatments of coronary artery disease improve quality of life in the long term. Nurs Res. 2006;55:26–33. doi: 10.1097/00006199-200601000-00004. [DOI] [PubMed] [Google Scholar]
- 10.Dey S, Flather MD, Devlin G, Brieger D, Gurfinkel EP, Steg PG, et al. Sex-related differences in the presentation, treatment and outcomes among patients with acute coronary syndromes: The global registry of acute coronary events. Heart. 2009;95:20–6. doi: 10.1136/hrt.2007.138537. [DOI] [PubMed] [Google Scholar]
- 11.Wang W, Lau Y, Chow A, Thompson DR, He HG. Health-related quality of life and social support among Chinese patients with coronary heart disease in mainland China. Eur J Cardiovasc Nurs. 2014;13:48–54. doi: 10.1177/1474515113476995. [DOI] [PubMed] [Google Scholar]
- 12.Höfer S, Kullich W, Graninger U, Wonisch M, Gassner A, Klicpera M, et al. Cardiac rehabilitation in Austria: Long term health-related quality of life outcomes. Health Qual Life Outcomes. 2009;7:99. doi: 10.1186/1477-7525-7-99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Zeighami R, Heidari MA. The effect of continuous care model on quality of life of patients after coronary angioplasty in Bou Ali Sina hospital. Evid Based Care. 2014;4:61–70. [Google Scholar]
- 14.Asadi-Lari M, Javadi HR, Melville M, Oldridge NB, Gray D. Adaptation of the MacNew quality of life questionnaire after myocardial infarction in an Iranian population. Health Qual Life Outcomes. 2003;1:23. doi: 10.1186/1477-7525-1-23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: Development and validation. J Chronic Dis. 1987;40:373–83. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- 16.Kendel F, Dunkel A, Müller-Tasch T, Steinberg K, Lehmkuhl E, Hetzer R, et al. Gender differences in health-related quality of life after coronary bypass surgery: Results from a 1-year follow-up in propensity-matched men and women. Psychosom Med. 2011;73:280–5. doi: 10.1097/PSY.0b013e3182114d35. [DOI] [PubMed] [Google Scholar]
- 17.Taghadosi M, Aliakbarzade-Arani Z, Gilasi H. Quality of life in patients with ischemic heart disease. J Neuromuscul Syst. 2014;1:19–26. [Google Scholar]
- 18.Yazdani-Bakhsh R, Javanbakht M, Sadeghi M, Mashayekhi A, Ghaderi H, Rabiei K. Comparison of health-related quality of life after percutaneous coronary intervention and coronary artery bypass surgery. ARYA Atheroscler. 2016;12:124–31. [PMC free article] [PubMed] [Google Scholar]
- 19.Salazar A, Dueñas M, Fernandez-Palacin F, Failde I. Factors related to the evolution of health related quality of life in coronary patients. A longitudinal approach using weighted generalized estimating equations with missing data. Int J Cardiol. 2016;223:940–6. doi: 10.1016/j.ijcard.2016.08.300. [DOI] [PubMed] [Google Scholar]
- 20.Seyam S, Heidarnia AR, Tavafian SS. Quality of life and factors related to it in cardiovascular patients after heart surgery. J Birjand Univ Med Sci (Suppl Cardiovasc) 2013;19:33–41. [Google Scholar]
- 21.Control CfD Prevention. How Tobacco Smoke Causes Disease: The Biology and Behavioral Basis for Smoking-Attributable Disease: A Report of the Surgeon General. 2010 [PubMed] [Google Scholar]
- 22.Pocock S, Henderson R, Clayton T, Lyman G, Chamberlain D. Quality of life after coronary angioplasty or continued medical treatment for angina: Three-year follow-up in the RITA-2 trial. J Am Coll Cardiol. 2009;35:907–14. doi: 10.1016/s0735-1097(99)00637-3. [DOI] [PubMed] [Google Scholar]
- 23.Demircioglu DT, Paker N, Erbil E, Bugdayci D, Emre TY. The effect of neuromuscular electrical stimulation on functional status and quality of life after knee arthroplasty: A randomized controlled study. J Phys Ther Sci. 2015;27:2501–6. doi: 10.1589/jpts.27.2501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hatmi Z, Kazemi MS. Quality of life in patients hospitalized with heart failure: A novel two questionnaire study. Acta Med Iran. 2007;45:493–500. [Google Scholar]
- 25.Johansson P, Dahlström U, Broström A. Factors and interventions influencing health-related quality of life in patients with heart failure: A review of the literature. Eur J Cardiovasc Nurs. 2006;5:5–15. doi: 10.1016/j.ejcnurse.2005.04.011. [DOI] [PubMed] [Google Scholar]
- 26.Rahimi A, Taghipoor H, Ebadi A, Pourebrahimi M. Comparing patients'quality of life before and after Coronary Artery Bypass Graft surgery (CABG) Iran J Crit Care Nurs. 2014;7:194–9. [Google Scholar]
- 27.Martin B, Galbraith PD, Lewin AM, Anderson T, Rabi D, Knudtson ML, et al. 213 sex differences in the association between obesity and quality of life in patients with coronary artery disease. Can J Cardiol. 2011;27:S136–7. [Google Scholar]
- 28.Korhonen PE, Seppälä T, Järvenpää S, Kautiainen H. Body mass index and health-related quality of life in apparently healthy individuals. Qual Life Res. 2014;23:67–74. doi: 10.1007/s11136-013-0433-6. [DOI] [PubMed] [Google Scholar]


