Abstract
Objectives:
The study was aimed at assessing adherence to prescribed antihypertensive medications and its associated factors.
Methodology:
Institutional-based cross-sectional study was conducted in four public hospitals which were selected by lottery method. Systematic random sampling was used to select the study subjects. Data were checked, cleaned, and entered into Epidata software version 3.1 and were imported to SPSS version 21 software for analysis. The results of the descriptive statistics were expressed as percentages and frequencies. Associations between independent variables and dependent variable were analyzed using bivariate and multivariate analysis. The study was conducted from February 15 to April 15, 2016.
Results:
The study included 404 respondents with 97% response rate. 210 (52%) were male and mean age was 54 ± 10.77 years. The respondents’ adherence to antihypertensive medications was 66.8%. The medication-related adherences were found to be better in females, patients who had comorbidities and have been knowledgeable about the disease and was poor among young adult respondents.
Conclusion:
This study found out a 66.8% adherence to prescribed antihypertensive medications. This figures show that medication adherence (MA) rates are low. The factors impeding or enhancing the outcome variable was thoroughly analyzed. Sex, age, number of types of medications, and knowledge were associated with MA. Educational sessions that especially focus on MA and ongoing support for patients should be designed. Studies which assess all the components of self-management should be conducted for comparison among different subgroups.
Keywords: Adherence, antihypertensive medications, hypertension, Morisky scale
Introduction
Hypertension (HTN) is one of the most prevalent noncommunicable diseases affecting a large number of people worldwide.1-4 It is one of the modifiable risk factors for cardiovascular and renal diseases.5 In developing nations like Ethiopia, the once thought rare disease; HTN is becoming a serious cause of morbidity and mortality.3 Even though there is undeniable threat imposed by non-communicable diseases such as HTN, communicable diseases still take the lion’s share in getting the attention from policymakers and foreign aid institutions.6 Globally, it is also one of the major causes of premature death, and 7.1 million of people die from HTN related diseases annually and the problem is still growing.3 HTN is one of the most common non-communicable diseases globally. More than 26% of the adult populations worldwide have been diagnosed as having HTN, and the prevalence of HTN increases with age.4
Poor adherence to medications is a major public health challenge. Adherence to medication has been defined as the extent to which patients’ behaviors coincide with health-care providers’ recommendations for health and medical advice.1 Self-management is a concept that emerged in the 1960’s as part of the chronic care model. Its purpose was highlighting the active participation of patients in their chronic disease management and minimizing the impact on their physical health status and functioning.7 Accumulated evidence showed that self-management activities are effective in terms of minimizing morbidity and mortality of HTN. One of the key components of HTN self-management is intake of prescribed anti-hypertensive medications.8-12
Although effective antihypertensive medications are available, control of HTN still remains minimal.13 A survey done in Iran to assess the risk factors of non-communicable diseases revealed 94% of hypertensive cases were not controlled.14 Another local study conducted in Bedele town revealed, control rate of HTN was only 22.4%.15 The rationale for these and other findings of uncontrolled HTN direct toward poor adherence to prescribed antihypertensive medications.13
The WHO recommends proper attention to be given toward adherence issues more than the development of new treatment regimens. On average, the overall adherence to long-term therapies for chronic illnesses is 50% among the developed countries. In developing countries, the rates are thought to be lower.2 Consequences of non-adherence would be catastrophic as they would cause poor blood pressure (BP) control and emergence of irreversible pathological complications. Additional to the impacts on personal health, they would have societal and economic influences, as management of the crisis caused by these diseases would increase the use of complicated and costly health services.13
Researchers tried to predict, factors that could impede or enhance adherence to self-management behaviors. Barriers to drug adherence consist of multiple factors that include complex medication regimens, dosing frequency, behavioral factors, and side effects of treatment. The most typical barriers to drug adherence are under the patient’s control, including patient’s knowledge and attitudes toward medications. Therefore, attention to these barriers is a necessary and important step to improve adherence.16-20 Even though sociodemographic factors have major impact on how patients deal with their illness, multiple independent factors that could influence patients’ adherence to taking anti-hypertensive medications are hardly studied.
Methodology
Study design and setting
Institutional-based cross sectional study was conducted from February 15 to April 15, 2016. The study was conducted in chronic follow-up units of Dagmawi Menilik, Tirunesh Beijing, Yekatit 12, and Zewditu Memorial Hospitals. The size of study participants who were recruited into the research was calculated using the single population proportion formula separately. After comparing P values for diet-related adherence, medication adherence (MA) and exercise adherence, sample size was calculated considering an exercise adherence proportion 0.437,9 level of confidence of 95%, and margin of error 5%: The sample size is estimated to be 378. Adding non response rate of 10%, the final sample size was 416. The target populations were all hypertensive patients who were on follow-up at public health hospitals in Addis Ababa, Ethiopia, and the study populations were selected patients who fulfilled the inclusion criteria and were available during the time of data collection.
Sampling technique
There are 12 public health hospitals that give chronic follow-up services in Addis Ababa city. Out of these, 4 were selected using lottery method (simple random sampling). The study was conducted on the selected public hospitals’ chronic follow-up units. The number of study units for each unit was proportionally allocated (based on case load per month), and those who were part of the final sample size were selected using systematic random sampling.
Inclusion and exclusion criteria
Inclusion criteria
All hypertensive patients who were 18 years and older and were on medical treatment (antihypertensive) at least for 6 months period before commencement of the study.
Exclusion criteria
Patients with cognitive impairment and those who refused to participate were immediately excluded from the study.
Data collection and data quality assurance
Structured interviewer-administered questionnaire was used to collect data on adherence to medication and associated factors. Questionnaire was prepared in English and was translated to Amharic language of by experts who are fluent in both language and back translated to English to see its consistency. Data were collected using face-to-face interview. The investigators were responsible for the overall management of the project; the development of the final questionnaire; securing participation of selected patients; identifying, training and assignment of data collectors and supervisors. The data collectors were four trained diploma nurses who were assigned at each of the four hospitals’ chronic follow-up units and were supervised by three BSc. nurse professionals. The purpose of the training was to ensure that all the data collectors had the same information about the study instrument and followed the same interview procedures. The training dealt with the purpose of the study, confidentiality and how to approach and forward questions to clients. Both the data collectors and supervisors were trained for 2 days on the objective and methodology of the research, data collection approach.
Variables and measurement
Dependent variable
The dependent variable was adherence to prescribed antihypertensive medications.
Independent variables
Sociodemographic factors-age, sex, marital status, religion, ethnicity, level of education. Personal factors: Comorbidities, knowledge about the disease, duration of HTN.
Morisky MA scale (MMAS) (alpha-reliability = 0.61, and concurrent validity; Pearson correlation = 0.64; P < 0.05) was used to assess patients’ MA, where total scores of ≥3 indicated low adherence; 1 or 2 = medium adherence and 0 = high adherence.21
Data analysis
Data were checked, cleaned, and entered into Epi-data version 3.1 software, then was imported to SPSS version 21.0 software for the analysis. Incomplete and inconsistent data were excluded from the analysis. Descriptive statistics was used to describe the sample. The results of the descriptive statistics were expressed as percentages and frequencies. Associations between independent and dependent variables were analyzed first using bivariate analysis to identify factors which were associated with the outcome variable. Those variables which were found to have an association with the outcome variable at P < 0.2 were entered to multivariate logistic regression to test for independent association. The magnitude of the association between the different independent variables in relation to dependent was measured using odds ratios and 95% confidence interval (CI) and P values below 0.05 were considered to be statistically significant.
Ethical considerations
The Institutional Health Research Ethics Review Committee of Addis Ababa University approved the research for scientific and ethical integrity. Clients were provided with information about the objective of the study, privacy, and confidentiality.
Results
Adherence to antihypertensive medications
The study included 404 respondents from 416 calculated sample size. The response rate was 97%. 210 (52%) were male and mean age was 54 ± 10.77 years. Out of the total 404 participants, 270 (66.8%) were adherent to regimens whereas the remaining 134 (33.2%) were not adherent to prescribed antihypertensive medications (Figure 1).
Figure 1.
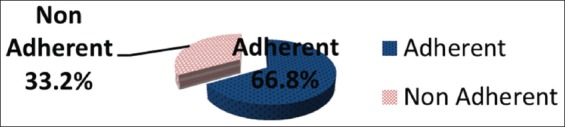
Antihypertensive medication adherence among hypertensive patients attending chronic follow up units of selected public hospitals in Addis Ababa, Ethiopia, 2016
MMAS was used to assess participant’s response about their MA level. This scale revealed that, out of the 404 respondents, 22.8% forgot taking medicines regularly, 12.6% were careless about taking their medications, 18.8% stopped medication on feeling worse, and 9.2% stopped on feeling better (Figure 2).
Figure 2.
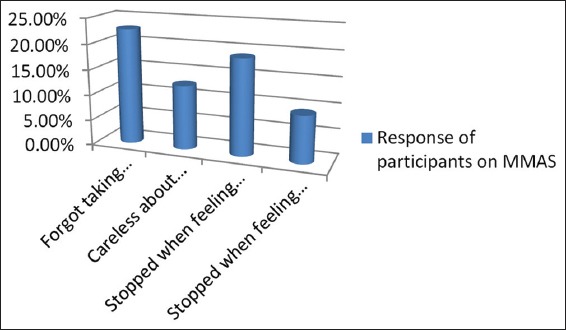
Response of study participants on the Morisky medication adherence scale attending follow-up at selected public hospitals of Addis Ababa, Ethiopia, 2016
Factors associated with adherence to antihypertensive medication
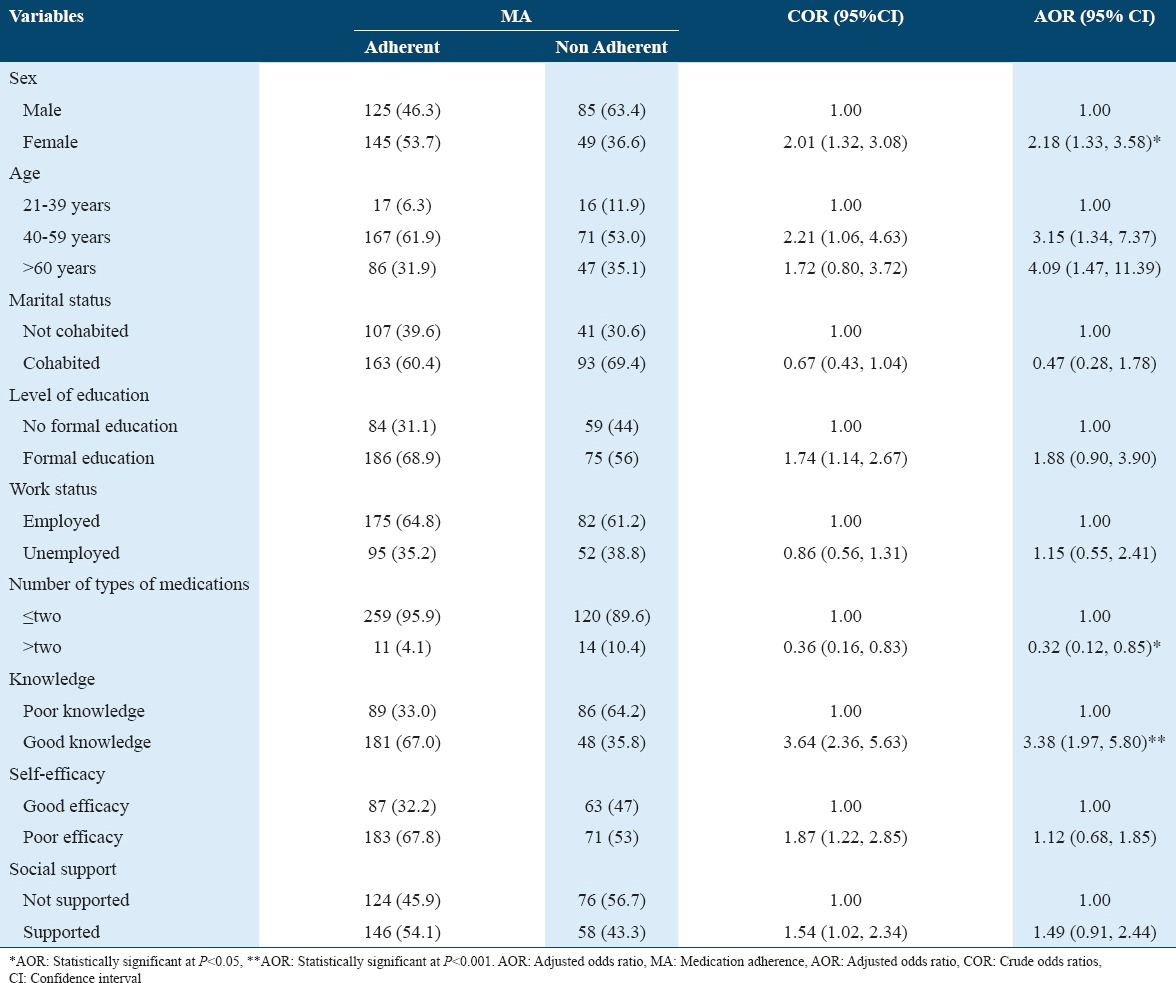
After controlling possible confounding effects of other covariates, sex, age, number of types of medications, and knowledge about HTN were independently associated with antihypertensive MA. Female respondents were 2 times more likely to be adherent than their male counterparts (adjusted odds ratio [AOR] = 2.18, 95% CI = 1.33, 3.58). With regard to age group, middle aged (AOR = 3.15, 95% CI = 1.34, 7.37) and older adults (AOR = 4.09, 95% CI = 1.47, 11.39) were found more likely to be adherent than young adults. Respondents who were taking more than two types of antihypertensive medications were found less likely to be adherent than those who took less types of medications (AOR = 0.315, 95% CI = 0.118, 0.845). Knowledge about the disease was found to be a significantly associated factor, as the respondents who had good knowledge were found 3 times more likely to be adherent to prescribed medication regimens (AOR = 3.378, 95% CI: 1.971, 5.789, P = 0.000) (Table 1).
Table 1.
Associations between sociodemographic, personal, social and behavioral factors and adherence to antihypertensive medications among patients attending follow up at selected public hospitals in Addis Ababa, Ethiopia, 2016
Discussion
HTN is a chronic condition that leads to serious complications if the person cannot control and manage the BP. HTN management consists of two main part: Pharmacological therapy and lifestyle modifications.1 The mean age of the participants in this study was 54 ± 10.77 years, which supports that the disease mostly affects those individuals in their late middle adulthood and above. Out of the 404 respondents, 52% were male consolidating the results of different studies that the prevalence of HTN is higher in males than females.8,15,22,23 This study tried to assess the prevalence of adherence to self-management activities among hypertensive patients in terms of adherence to antihypertensive medications.
Nonadherence to medication is a major factor that impedes control of BP in more than two-thirds of hypertensive individuals.2,22,23 Comparative to adherence to recommended lifestyle modifications, there are many studies done in different parts of the world assessing adherence to medications. There are different methods of adherence measurement, and there is no single measurement that can meet all gold standards since each has its own drawbacks. In this study, the Morisky 4-item self-reported MA scale was used to measure antihypertensive MA among hypertensive patients. the Morisky 4-item self-reported MA scale (alpha-reliability = 0.61, and concurrent validity; Pearson correlation = 0.64; P < 0.05) was used to assess patients’ MA, where total scores of >3 indicated low adherence; 1 or 2 = medium adherence, and 0 = high adherence. This study established that 66.8% of the respondents were found to be adherent to their HTN medication. These findings of other studies conducted in different parts of the world are varied; the UK (88%), the USA (77%), Kuwait (88.6%), and India (73%).24-26 Adherence in developed countries could be higher than developing countries probably due to the socioeconomic variations and better awareness about the disease.
African studies done to assess adherence to antihypertensive medications found out different adherence figures. A Kenyan study with 327 respondents found out a 64.2% adherence level while a Nigerian and Tanzanian studies found the adherence rates to be 51% and 56%, respectively.27-29 This discrepancy could be explained by methodological variations among these studies. A similar study conducted in Addis Ababa, Ethiopia found out an approximately similar proportion of respondents who were adherent to their antihypertensive medications (69.2%).9 Other local studies conducted in Adama and Jimma towns found 59.5% and 52.9% adherence rates, respectively.30,31 The variation between this particular study and the other local studies could be explained by the higher number of respondents in this study, and the urban residency of study participants which allowed them to be more aware about MA.
The findings of this study show that female respondents were found more likely to be adherent to HTN treatment than their male counterparts due to the fact that females are more careful naturally. This is in line with a study from Kenya where female respondents were found to be more adherent than males.29 A Bangladesh study also found that more men were nonadherent to antihypertensive treatment than women.32 This study found that respondents who were taking less than two types of antihypertensive medications were more adherent than those who were taking more than two types of medications due to pill burden that affects adherence negatively. A similar Kenyan study consolidates the findings of this study, as it found that those who took one or two antihypertensive medications were about 2.2 times more adherent than those who took three or more antihypertensive medications.33
Participants who were found to have good knowledge about HTN and its management were also found more likely to be adherent to their treatment compared to those who were found to be poorly knowledgeable. This is due to the fact that patients’ knowledge and understanding about disease improve adherence to prescribed drug. Other studies from Kuwait and Kenya support the finding of this study, in that they found a positive association between lack of knowledge about HTN and noncompliance to treatment.29,34 In this study, middle and old aged adults were found more likely to be adherent to antihypertensive medications compared to young adults. This finding is similar to the results of studies carried out in different parts of the world which found out that age increment was associated with better adherence.32-36
Conclusion
This study found out a 66.8% adherence to prescribed antihypertensive medications. Our study demonstrated that MA rates are low. The factors impeding or enhancing the outcome variable was thoroughly analyzed. Sex, age, number of types of medications, and knowledge were associated with MA. Educational sessions that especially focus on MA and ongoing support for patients should be designed. MA counseling regarding the benefit of adhering to antihypertensive medications should be focused by health-care provider. Studies which assess all the components of self-management should be conducted for comparison among different subgroups.
Acknowledgments
We would like to thank the participants of this study for their cooperation and AA University, School of Nursing and Midwifery for the support they provided us.
References
- 1.Ogah OS, Rayner BL. Recent advances in hypertension in Sub-Saharan Africa. Heart. 2013;99:1390–7. doi: 10.1136/heartjnl-2012-303227. [DOI] [PubMed] [Google Scholar]
- 2.Alwan A. Global Status Report on Noncommunicable Diseases. World Health. 2010. [[Last accessed on 2016 Jul 09]]. pp. 16–28. Available from: http://www.whqlibdoc.who.int/publications/2011/97892406⇅8_eng.pdf .
- 3.Nshisso LD, Reese A, Gelaye B, Lemma S, Berhane Y, Williams MA. Prevalence of hypertension and diabetes among Ethiopian adults. Diabetes Metab Syndr. 2012;6:36–41. doi: 10.1016/j.dsx.2012.05.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Warren-Findlow J, Seymour RB, Shenk D. Intergenerational transmission of chronic illness self-care: Results from the caring for hypertension in African American families study. Gerontologist. 2011;51:64–75. doi: 10.1093/geront/gnq077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Awoke A, Awoke T, Alemu S, Megabiaw B. Prevalence and associated factors of hypertension among adults in Gondar, Northwest Ethiopia: A community based cross-sectional study. [[Last accessed on 2016 Jun 09]];BMC Cardiovasc Disord. 2012 12:113. doi: 10.1186/1471-2261-12-113. Available from: http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=3519757&tool=pmcentrez&rendertype=abstract . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Angaw K, Dadi AF, Alene KA. Prevalence of hypertension among Federal Ministry Civil Servants in Addis Ababa, Ethiopia: A call for a workplace-screening program. BMC Cardiovasc Disord. 2015;15:76. doi: 10.1186/s12872-015-0062-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Southern Mallee Primary Care Partnership. Common Models of Chronic Disease Self-Management Support. Vol. 5. Australia, Victoria: Southern Mallee Primary Care Partnership; 2010. pp. 1–4. [Google Scholar]
- 8.Akhter V. Self-Management among Patients with Hypertension in Banagladesh. Vol. 21. Prince of Songkla University; 2010. pp. 10–23. [Google Scholar]
- 9.Hareri HA, Abebe M, Asefaw T. Assessments of adherence to hypertension managements and its influencing factors among hypertensive patients attending black lion hospital chronic follow up unit, Addis Ababa, Ethiopia - A cross-sectional study. [[Last accessed on 2016 Jun 23]];Int J Pharm Sci Res. 2013 4:1086–95. Available from: http://www.ijpsr.com/V4I3/26-27 . [Google Scholar]
- 10.Lynch EB, Liebman R, Ventrelle J, Avery EF, Richardson D. A self-management intervention for African Americans with comorbid diabetes and hypertension: A pilot randomized controlled trial. Prev Chronic Dis. 2014;11:E90. doi: 10.5888/pcd11.130349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.British Columbia Ministry of Health. [[Last accessed on 2015 Sep 15]];Self-management Support: A Health Care Intervention. 2011 34:89–90. Available from: http://www.selfmanagementbc.ca/uploads/WhatisSelf-Management/PDF/Self-ManagementSupportAhealthcareintervention2011.pdf . [Google Scholar]
- 12.Nakagawa-Kogan H, Garber A, Jarrett M, Egan KJ, Hendershot S. Self-management of hypertension: Predictors of success in diastolic blood pressure reduction. Res Nurs Health. 1988;11:105–15. doi: 10.1002/nur.4770110206. [DOI] [PubMed] [Google Scholar]
- 13.De Geest S, Sabaté E. Adherence to long-term therapies: Evidence for action. Eur J Cardiovasc Nurs. 2003;2:323. doi: 10.1016/S1474-5151(03)00091-4. [DOI] [PubMed] [Google Scholar]
- 14.Babaee Beigi MA, Zibaeenezhad MJ, Aghasadeghi K, Jokar A, Shekarforoush S, Khazraei H. The effect of educational programs on hypertension management. Int Cardiovasc Res J. 2014;8:94–8. [PMC free article] [PubMed] [Google Scholar]
- 15.Bonsa F, Gudina EK, Hajito KW. Prevalence of hypertension and associated factors in Bedele Town, Southwest Ethiopia. Ethiop J Health Sci. 2014;24:21–6. doi: 10.4314/ejhs.v24i1.3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.McEvoy LK, Kritz-Silverstein D, Barrett-Connor E, Bergstrom J, Laughlin GA. Changes in alcohol intake and their relationship with health status over a 24-year follow-up period in community-dwelling older adults. J Am Geriatr Soc. 2013;61:1303–8. doi: 10.1111/jgs.12366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Xin X, He J, Frontini MG, Ogden LG, Motsamai OI, Whelton PK. Effects of alcohol reduction on blood pressure: A meta-analysis of randomized controlled trials. Hypertension. 2001;38:1112–7. doi: 10.1161/hy1101.093424. [DOI] [PubMed] [Google Scholar]
- 18.Stevens VJ, Corrigan SA, Obarzanek E, Bernauer E, Cook NR, Hebert P, et al. Weight loss intervention in phase 1 of the trials of hypertension prevention. The TOHP Collaborative Research Group. Arch Intern Med. 1993;153:849–58. [PubMed] [Google Scholar]
- 19.Appel LJ, Espeland MA, Easter L, Wilson AC, Folmar S, Lacy CR. Effects of reduced sodium intake on hypertension control in older individuals: Results from the Trial of Nonpharmacologic Interventions in the Elderly (TONE) Arch Intern Med. 2001;161:685–93. doi: 10.1001/archinte.161.5.685. [DOI] [PubMed] [Google Scholar]
- 20.Huang Z, Willett WC, Manson JE, Rosner B, Stampfer MJ, Speizer FE, et al. Body weight, weight change, and risk for hypertension in women. Ann Intern Med. 1998;128:81–8. doi: 10.7326/0003-4819-128-2-199801150-00001. [DOI] [PubMed] [Google Scholar]
- 21.Pedersini R, Vietri J. Comparison of the 4-item and 8-item Morisky medication adherence scale in patients with Type 2 diabetes. Kantar Health. 2014;10:85–9. [Google Scholar]
- 22.Whelton PK, He J, Muntner P. Prevalence, awareness, treatment and control of hypertension in North America, North Africa and Asia. J Hum Hypertens. 2004;18:545–51. doi: 10.1038/sj.jhh.1001701. [DOI] [PubMed] [Google Scholar]
- 23.Okwuonu CG, Ojimadu NE, Okaka EI, Akemokwe FM. Patient-related barriers to hypertension control in a Nigerian population. Int J Gen Med. 2014;7:345–53. doi: 10.2147/IJGM.S63587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Al-Mehza AM, Al-Muhailije FA, Khalfan MM, Al-Yahya AA, Care PH, Clinic H. Drug compliance among hypertensive patients; An area based study. Eur J Gen Med. 2009;6:6–10. [Google Scholar]
- 25.Bhandari S, Centre AM, Studies HS. Adherence to anti-hypertensive treatment and its determinants among the urban slum dwellers. Am J Hand Surg. 2009;12:98–120. [Google Scholar]
- 26.Grant S. Self-monitoring blood pressure in patients with hypertension: Who self-monitors and why? Int J Hypertens. 2013;34:45–78. [Google Scholar]
- 27.Alphonce JA. Factors affecting treatment compliance among hypertension patients in three district hospitals - Dar es Salaam. Muhimbili Univ Health Allied Sci. 2012;9:129–39. [Google Scholar]
- 28.Osamor PE, Owumi BE. Factors associated with treatment compliance in hypertension in southwest Nigeria. J Health Popul Nutr. 2011;29:619–28. doi: 10.3329/jhpn.v29i6.9899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kimuyu BM. Factors associated with adherence to anti-hypertensive treatment. Nairobi Univ. 2006;24:234–56. [Google Scholar]
- 30.Hareri HA, Gedefaw M, Simeng B. Original research article assessment of prevalence and associated factors of adherence to anti-hypertensive agents among adults on follow up in Adama Referal hospital, East Shoa, Ethiopia-cross sectional study. [[Last accessed on 2016 Jun 01]];Int J Curr Microbiol Appl Sci. 2014 3:60–70. Available from: http://www.ijcmas.com/vol-3-1/HabtamuAberaHarerietal.pdf . [Google Scholar]
- 31.Yenesew A, Gashi F, Tatiparthi R. Prevalence of non-adherance and its associated factors of hypertensive patients at Jimma University specialized hospital in southwest Ethiopia. Indian J Health Sci. 2015;8:40–7. [Google Scholar]
- 32.Nwankwo T, Yoon SS, Burt V, Gu Q. Hypertension among adults in the United States: National Health and Nutrition Examination Survey, 2011-2012. NCHS Data Brief. 2013;133:1–8. [PubMed] [Google Scholar]
- 33.Khanam MA, Lindeboom W, Perez TL, Alam DS, Niessen L, Milton AH. Hypertension: Adherence to treatment in rural Bangladesh findings from a population-based study. Glob Health Action. 2014;1:1–9. doi: 10.3402/gha.v7.25028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Lee GK, Wang HH, Liu KQ, Cheung Y, Morisky DE, Wong MC. Determinants of medication adherence to antihypertensive medications among a Chinese population using Morisky Medication Adherence Scale. PLoS One. 2013;8:e62775. doi: 10.1371/journal.pone.0062775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Hu H, Li G, Arao T. Prevalence rates of self-care behaviors and related factors in a rural hypertension population: A questionnaire survey. Int J Hypertens. 2013;2013:526949. doi: 10.1155/2013/526949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Hyre AD, Krousel-Wood MA, Muntner P, Kawasaki L, DeSalvo KB. Prevalence and predictors of poor antihypertensive medication adherence in an urban health clinic setting. J Clin Hypertens (Greenwich) 2007;9:179–86. doi: 10.1111/j.1524-6175.2007.06372.x. [DOI] [PMC free article] [PubMed] [Google Scholar]


