Abstract
Background:
India continues to contribute disproportionately to the global burden of disease and public health research output from India is also known to be not commensurate with her healthcare needs. We carried out the present study to assess if clinical trials were in line with the health care needs of the country by auditing the clinical trials registry of India.
Materials and Methods:
All the clinical studies registered in CTRI between July 20, 2007 and December 31, 2015 were searched in the “Trial Search” section. The total number of studies, their phases of development, and therapeutic areas were assessed. Trials in each therapeutic area was compared with the disease burden (DALYs) in that area taken from Global Health Estimates [2014] Summary Tables of the WHO. The number of trials conducted per state in India was also compared with the population of that state [Census 2011].
Results:
A total of 6474 studies were registered of which 3325 (51.4%) were clinical trials. The state of Maharashtra had the highest number trials [16.4%] followed by Karnataka (11.6%) and Tamil Nadu (10%). Populous states like Uttar Pradesh (5.3%) and Bihar (1.4%) had far fewer trials. The largest number of trials was in the area of cancer (16.4%), followed by diabetes (12.1%) and cardiovascular diseases (10.1%). Infectious and parasitic diseases had the highest DALYs (82,681) and ranked first in disease burden but accounted for only 5% of the total trials and ranked 7th according to number of trials. Cancer ranked first in the number of trials (16.4%), but ranked 6th based on DALYs.
Conclusion:
Clinical trials conducted in India are not in consonance with her health care needs. Strengthening the capacity for conducting trials in the populous states and the north-eastern part of the country is necessary to allow a more equitable selection of participants. The government should introduce policies to encourage new drug development in areas where needed the most.
Keywords: Clinical trials, disability-adjusted life-years, India
BACKGROUND
Over the past 10 years, although India has seen significant improvements in some health indicators (for example, increased life expectancy at birth, decreased under-five mortality rate, and decreased maternal mortality ratio),[1] the country still contributes disproportionately to the global burden of disease. In addition, large health disparities exist between states, across social classes with a significant rural-urban divide.[2] India accounts for 18% of global deaths and 20% of disability-adjusted life-years (DALYs) (WHO 2009).[3]
One of the ways to improve the health status of a country is to generate objective and locally relevant evidence about various interventions being researched or developed globally so that they can be applied to the country's needs. It was encouraging that India became one of the preferred destinations for the conduct of global clinical trials after a series of regulatory reforms from 2005 onward. The conduct of these trials was helped by the fact that the country had a treatment naïve patient pool, a large disease burden, experienced and English-speaking investigators, and relatively low costs of trial conduct.[4,5]
It has been stated earlier that the public health research output from India has not been commensurate with her healthcare needs.[6] In view of the surge in clinical research and the concomitant regulatory reforms, we wanted to find out if this research was in line with the health care needs of the country. We did this by evaluating studies registered in the Clinical Trials Registry of India (CTRI) between 2007 and 2015 and compared them with the disease burden in the country. Further, because health disparities are known to exist between states, social classes, and rural and urban India, we also assessed whether there were inequities in distribution of clinical trials across the country.
METHODS
Search strategy
All the clinical studies registered in CTRI between July 20, 2007, and December 31, 2015, were searched in the “Trial Search” section with the keywords CTRI/year (being 2007/08/09/10/11/12/13/14/15) and Phase I/II/III/IV in the “Trial Phase” section for each year.
Data extraction and analysis strategy
The total number of clinical trials (studies in various phases of drug development) per year and their development phase was determined
The number of trials conducted per state in India was calculated and compared with the population of that state based on the 2011 census of India
The trials were then classified into 15 different therapeutic areas: Cancers, cardiovascular diseases, diabetes mellitus, digestive diseases, endocrine, blood- and immune-related disorders, genitourinary diseases, infectious and parasitic diseases, mental and behavioral disorders, musculoskeletal diseases, neonatal conditions, neurological conditions, nutritional deficiencies, respiratory diseases, sense organ diseases, and skin diseases. The total number of trials and their phases in each therapeutic area was also calculated
The number of trials in each therapeutic area was compared with the disease burden (expressed in DALYs) in that area taken from Global Health Estimates 2014 Summary Tables, WHO.[7] Further, the DALYs were ranked in ascending order and compared to the rank that the therapeutic area got when classified by a number of trials.
RESULTS
Demographics
The CTRI had a total of 6474 studies registered during the study period, of which 3325 (51.4%) were clinical trials. From 27 in 2007, the number of trials rose to a maximum of 550 in 2010. There was a fall over the next 2 years (363, 394, respectively) to rise again to 404 in 2015 [Figure 1]. Phase III trials were the largest group (1550/3325; 46.6%), followed by Phase IV (783/3325; 23.5%), Phase II (778/3325; 23.4%), and Phase I (214/3325; 6.5%). The year-wise trend for the various phases was similar to that seen with the total [Figure 1].
Figure 1.
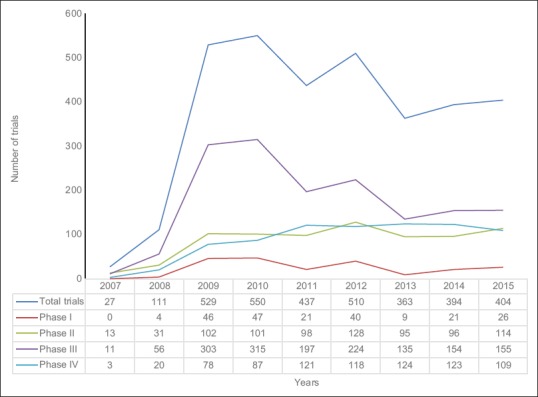
Year-wise trend of total trials and trials in different phases
State-wise distribution of trials
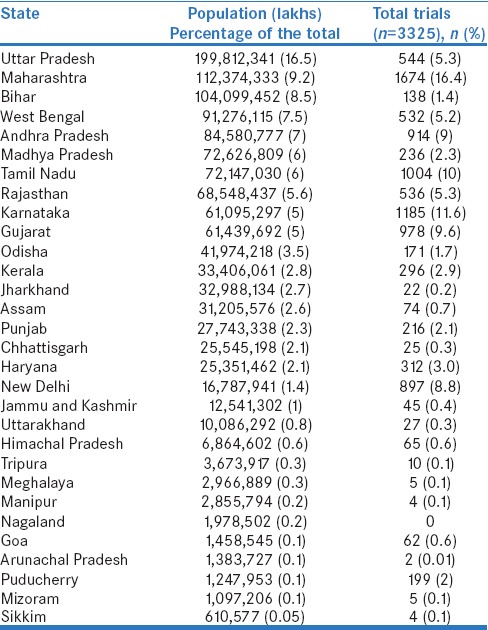
Maharashtra had the highest number trials registered (1674; 16.4%), followed by Karnataka (1185; 11.6%) and Tamil Nadu (1004; 10%). Populous states such as Uttar Pradesh (544; 5.3%) and Bihar (138; 1.4%) had far fewer trials. All the Northeastern states had only 109 (1.1%) trials over the entire 8-year period. Table 1 gives the state wise distribution of trials registered in CTRI between 2007 and 2015 and the corresponding population of the state.
Table 1.
State-wise distribution of trials registered in Clinical Trials Registry of India between 2007 and 2015
Distribution of trials based on therapeutic area
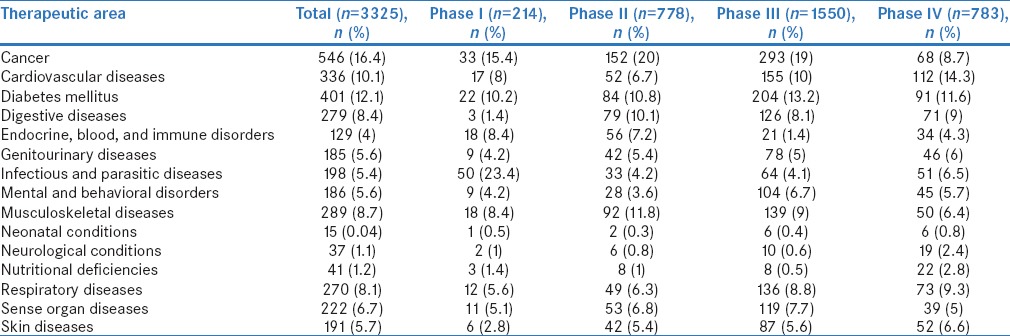
The largest number of trials was in the area of cancer (546; 16.4%), followed by diabetes (401; 12.1%) and cardiovascular diseases (336; 10.1%). Most Phase I trials were in infectious and parasitic diseases (50/214; 23.4%) and 76% (38/50) of these Phase I trials were vaccine trials. Most Phase II (152/778; 20%) and Phase III (293/1550; 19%) trials were in cancers while the maximum Phase IV trials were in cardiovascular diseases (112/783; 14.3%). Table 2 shows the distribution of trials across therapeutic areas and phases of drug development.
Table 2.
Distribution of trials registered in Clinical Trials Registry of India between 2007 and 2015 according to therapeutic area and phase of drug development
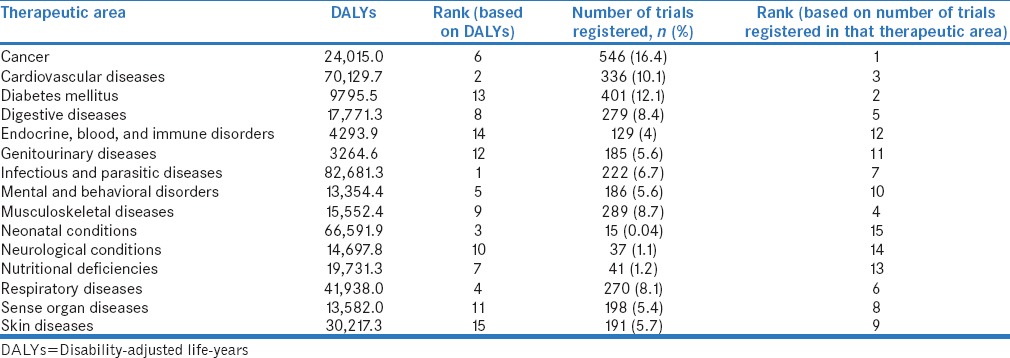
Comparison of number of trials conducted with the disease burden in India by ranking of health conditions according to the number of trials in that condition and the disease burden in that area (expressed as DALYs).
We found that infectious and parasitic diseases had the highest DALYs (82,681) and ranked first in disease burden but accounted for only 5% of the total trials ranking 7th according to number of trials. Cancer was ranked first in the number of trials (546/3325; 16.4%) but was ranked 6th based on DALYs (24,015). Neonatal conditions (DALY rank 3) and nutritional deficiencies (DALY rank 7) also with high DALYs had far fewer trials (trial rank 15 and 13, respectively). Table 3 shows the number of trials in each therapeutic area and the disease burden in that area (expressed as DALYs) in India.
Table 3.
Number of clinical trials in each therapeutic area and the disease burden (expressed as disability-adjusted life-years) in India with ranking
DISCUSSION
In this 8-year analysis of studies registered with the CTRI, we found that 51% of the total studies registered were clinical trials. The total number of trials registered, first increased from 2007 to 2010, after which the numbers began to fall to rise again in 2015. The fall in number of trials after 2010 can be attributed to the global financial crisis that occurred in 2008–2009. Almost half of the trials in India registered during the study period were Phase III studies, reflecting the fact that India had become an attractive hub for clinical research. The small number of Phase I trials (7%) indicates that not enough indigenous research is occurring in India. On the other hand, it is encouraging that a large number of these Phase I studies are being conducted on vaccines suggesting that efforts are being made in the country to reduce large infectious disease burden.
When we compared the number of trials per state in India with the population of that state, we found a skew in distribution. Populous states such as Uttar Pradesh and Bihar were found to have fewer trials and the topographically detached Northeastern states had the fewest. This likely stems from lack of trained workforce, infrastructure, and appropriate technology. The Declaration of Helsinki, 2013[8] specifies that research should be accessible to the population and it is an individual's right to participate in research. More training and infrastructure building efforts must thus be made in these states to reduce this inequity.
The top five health conditions contributing to the disease burden were infectious and parasitic disease, cardiovascular diseases, neonatal conditions, respiratory diseases, and mental and behavioral diseases, while the top five areas in which clinical trials were conducted included cancers, diabetes mellitus, cardiovascular diseases, musculoskeletal diseases, and digestive diseases. This shows a discrepancy in the areas in which the trials are being conducted and the areas contributing to significant disease burden in the country. A large number of trials on noncommunicable diseases lead to a possible conclusion that India is possibly contributing to global research, which may not entirely be necessary for the population. This shows a discrepancy in the areas in which research is being conducted and the health needs of the country. Other authors have noted that research outputs – publications in peer-reviewed journals are at a dismal low in the country.[9]
While communicable diseases still pose a very high risk on the health status of the Indian population, very little new research is being done on them. This clearly depicts that India is conducting more trials on lifestyle-related disorders while their major disease burden is still contributed by infectious diseases. Even drugs such as bedaquiline (for drug-resistant tuberculosis) and miltefosine (for leishmaniasis) which are lifesaving have been developed outside the country.
CONCLUSION
Thus, the present study shows that the clinical trials conducted in India are not in consonance with their health care needs. Strengthening the capacity for conducting trials in the populous states and the Northeastern part of the country is necessary to allow a more equitable selection of participants. We conclude that India must participate in more clinical trials, especially in areas relevant to its own disease burden and major public health problems. The government should introduce policies to encourage new drug development in areas where needed the most.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1. [Last accessed on 2016 Aug 01]. Available from: http://www.who.int/gho/countries/ind/en/
- 2.Patel V, Parikh R, Nandraj S, Balasubramaniam P, Narayan K, Paul VK, et al. Assuring health coverage for all in India. Lancet. 2015;386:2422–35. doi: 10.1016/S0140-6736(15)00955-1. [DOI] [PubMed] [Google Scholar]
- 3. [Last accessed on 2016 Aug 01]. Available from: http://www.who.int/countryfocus/cooperation_strategy/ccsbrief_ind_en.pdf .
- 4.Maiti R. MR. Clinical trials in India. Pharmacol Res. 2007;56:1–10. doi: 10.1016/j.phrs.2007.02.004. [DOI] [PubMed] [Google Scholar]
- 5.Gupta YK, Padhy BM. India's growing participation in global clinical trials. Trends Pharmacol Sci. 2011;32:327–9. doi: 10.1016/j.tips.2011.02.017. [DOI] [PubMed] [Google Scholar]
- 6.Dandona L, Sivan YS, Jyothi MN, Bhaskar VS, Dandona R. The lack of public health research output from India. BMC Public Health. 2004;4:55. doi: 10.1186/1471-2458-4-55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. [Last accessed on 2016 Aug 01]. Available from: http://www.who.int/healthinfo/global_burden_disease/estimates/en/index2.html .
- 8. [Last accessed on 2016 Aug 01]. Available from: http://www.wma.net/en/30publications/10policies/b3/
- 9.Ray S, Shah I, Nundy S. The research output from Indian medical institutions between 2005 and 2014. Curr Med Res Pract. 2016;2:49–58. [Google Scholar]


