Abstract
Sleep patterns have been associated with the development of cancers, although the association between sleep duration and breast cancer remains controversial. The purpose of our study was to explore the relationship between sleep duration and breast cancer risk. The PubMed and Web of Science databases were searched, and restricted cubic splines were used to explore the dose-response relationship. Data from 415,865 participants were derived from 10 studies. A J-shaped nonlinear trend was found between sleep duration and breast cancer incidence (Pnon-linear = 0.012); compared with the reference hours (6 h or 7 h), with increasing sleep hours, the risk of breast cancer increased (Ptrend = 0.028). Moreover, a nonlinear relationship was found between sleep duration and estrogen receptor-positive breast cancer (Pnon-linear = 0.013); the risk of estrogen receptor-positive breast cancer increased with increasing sleep hours compared to the reference hours (Ptrend = 0.024). However, no nonlinear relationship was found between sleep duration and estrogen receptor-negative breast cancer; the risk of estrogen receptor-negative breast cancer was 1.035 for every additional sleep hour. Compared to women with the reference number of sleep hours, women with a longer sleep duration might have a significantly increased risk of breast cancer, especially estrogen receptor-positive breast cancer.
1. Introduction
Globally, breast cancer is the most frequently diagnosed cancer and the leading cause of cancer mortality among women. The incidence of breast cancer increases by 5 percent each year in low- and middle-income countries and thus represents an increasingly urgent public health problem [1, 2]. Many studies have focused on risk factors for breast cancer. For instance, the commentary by Colditz established reproductive characteristics, growth, obesity, and postmenopausal hormones as significant etiological factors, although these variables accounted for just a small proportion of breast cancer risk [3]. With societal development, attention has increasingly been turned to quality of life and lifestyle factors, such as sleep patterns, night-shift work, alcohol consumption, and weight gain, as important influencing factors that may provide additional clues for efforts to prevent breast cancer.
Recently, sleep patterns (including sleep duration or sleep quality) and their relationships with related health outcomes have been studied, mostly regarding chronic diseases such as cardiovascular diseases, diabetes, obesity, and metabolic syndrome [4–7]. As a possible mechanism, sleep might affect the levels of circulating hormones, such as melatonin, cortisol, growth hormone, prolactin, glucose, and insulin, which are key factors involved in many disease processes, including breast cancer [8]. Thus, a growing number of epidemiologic studies have examined the association between sleep duration and breast cancer incidence; however, the results have been inconsistent [9–12]. Therefore, we performed this updated dose-response meta-analysis to explore the association between sleep duration and breast cancer incidence, which might provide some insight and evidence for efforts to prevent breast cancer in women.
2. Materials and Methods
This meta-analysis was conducted according to the meta-analysis of observational studies in epidemiology (MOOSE) checklist [19].
2.1. Literature Search Strategy
Two authors (Chunyang Lu and Hao Sun) conducted a computerized search for published articles in the PubMed and Web of Science databases from inception to September 2nd, 2016, without language restrictions. Discrepancies were resolved through discussion with other authors (Jinyu Huang and Songcheng Yin). The following search terms were used: (1) breast cancer OR mammary cancer OR breast neoplasms OR mammary neoplasms; (2) sleep OR sleep duration OR sleep pattern. We also screened the reference lists of relevant review articles and included studies for additional information.
2.2. Selection Criteria
Studies were included only if they met all the following criteria: (1) the study was an observational study (case-control study or cohort study); (2) the outcome was the first incidence of breast cancer; (3) the exposure was sleep duration with at least three categories; and (4) there were available effect estimates (risk ratios (RRs)) or odds ratios (ORs) and 95% confidence intervals and the corresponding number of cases and person-years or subjects for each category of sleep duration. Comments, reviews, letters, animal experiments, and studies involving other cancers were excluded. If multiple publications were available for a study, data from the most recent and complete publication were included.
2.3. Data Extraction
Two authors (Chunyang Lu and Hao Sun) evaluated study eligibility and conducted data extraction independently using a predefined standardized data extraction form. The variables in the form included the following: name of the first author, publication year, study country, study name, study design, follow-up year (if cohort study), investigation year (if case-control study), age at baseline, the proportion of postmenopausal participants, method of sleep data collection, the ascertainment of breast cancer, sample size (numbers of participants and incident cases) in each category, covariates adjusted in the multivariable analysis, and effect size (RRs or ORs) with a 95% CI for all categories of sleep duration.
2.4. Quality Assessment
Quality assessment was performed according to the Newcastle-Ottawa Quality Assessment Scale (NOS) [20], which is a validated scale for nonrandomized studies in three areas: the selection of exposed and unexposed participants; the comparability of the groups; and the assessment of the outcome. This tool contains nine items, with each item being assigned a star if a study meets the criteria for the item. We considered a study as high-quality if it received 7 or more stars.
2.5. Statistical Analysis
First, we conducted restricted cubic splines with five knots at the 1st, 25th, 50th, 75th, and 99th percentiles of exposure distribution to fit the potential nonlinear trend between sleep duration and incidence of breast cancer. In this method, the distributions of cases and participants and the fully adjusted RRs or ORs and 95% CIs in each sleep duration category were required. For studies that did not report the numbers of breast cancer cases for each category of sleep duration, these numbers were inferred based on the total numbers of cases and the reported risk estimates. Additionally, for each of the included studies, we assigned the reported median or mean sleep duration of each category as the category sleep duration. When a study reported only the range of sleep duration for a category, we used the average value of the lower and upper bounds of that category. When the shortest or the longest category was open-ended, we assumed that the open-ended interval length had the same length as the adjacent interval. The reference category was set to 6 h (the lowest risk of breast cancer in our study based on the dose-response curve) or 7 h (international sleep duration recommendation) [21]. A P value for nonlinearity was calculated by testing the null hypothesis that the coefficient of the second and third spline was equal to 0. If the hypothesis did not hold, we conducted a linear dose-response meta-analysis to test the risk of breast cancer with each additional hour of sleep. Otherwise, the nonlinear dose-response meta-analysis was conducted to show each hour's risk of breast cancer (from 4 h to 10 h). We also performed subgroup analyses stratified by menopausal status (postmenopausal or premenopausal) and estrogen receptor (ER) status (ER+ or ER−). All analyses were performed with STATA version 12.0 (StataCorp, College Station, TX), and all tests were two-sided with a significance level of 0.05.
3. Results
3.1. Literature Search and Characteristics of the Included Studies
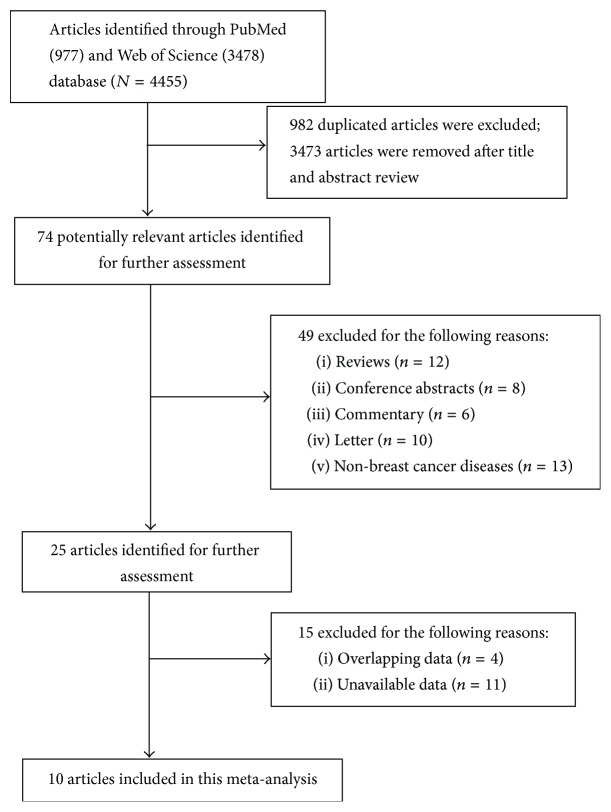
A total of 10 studies [9–18] composed of six cohort studies [9, 10, 12, 15, 16, 18], three case-control studies [11, 14, 17], and one nested case-control study [13] were included in our final meta-analysis. The details of how we selected relevant studies are shown in Figure 1.
Figure 1.
Flow diagram for studies selection.
The characteristics of the studies and participants included in this study were presented in Tables 1 and 2. Of these studies, five were conducted in America [9, 10, 12, 16, 17], three were conducted in Asia [11, 13, 15], one was conducted in Australia [14], and one was conducted in Europe [18]. The sample sizes ranged from 1,454 to 110,011, and the proportion of postmenopausal women in most of the studies was over 50%, except one study with 37.14% [11] and one study that did not report menopausal status [18]. The sleep durations were all self-reported via questionnaire or interview; the sleep reference categories in each study were set to ≤6 h [13], 7 h [12, 15, 16], 8 h [9, 18], 6.1 to 8.9 h [11], 7 to 7.9 h [17], 7 to 8 h [14], and 7 to 9 h [10]. The ascertainment of breast cancer was mostly through cancer registry or medical records. Most studies were adjusted for a wide range of potential confounders, such as menopausal status, body mass index (BMI), smoking, and alcohol drinking. The qualities of the individual studies were listed in Table 2.
Table 1.
Characteristics of studies and participants included in meta-analysis.
| Author | Year | Country | Study | Number of participants | Follow-up/investigated years | Age at baseline | Postmenopausal (%) | Study design |
|---|---|---|---|---|---|---|---|---|
| Xiao et al. [9] | 2016 | America | Southern community cohort study | 42953 | 2002–2009 | 52.18 | 66.70% | Cohort study |
|
| ||||||||
| Hurley et al. [10] | 2015 | America | California teachers study | 101609 | “1995-1996” to 2011 | 52.00 | 58.28% | Cohort study |
|
| ||||||||
| Wang et al. [11] | 2014 | China | Guangzhou breast cancer study | 1454 | 2010–2012 | 47.50 | 37.14% | Case-control study |
|
| ||||||||
| Vogtmann et al. [12] | 2013 | America | Women's health initiative | 110011 | 1992–2007 | 62.91 | 100% | Cohort study |
|
| ||||||||
| Wu et al. [13] | 2012 | Singapore | Singapore Chinese health study | 34028 | “1993–1998” to 2010 | 45–74 | 92.73% | Nested case-control study |
|
| ||||||||
| Girschik et al. [14] | 2012 | Australia | Breast cancer environment and employment study | 2828 | 2009–2011 | 18–80 | 88.79% | Case-control study |
|
| ||||||||
| Kakizaki et al. [15] | 2008 | Japan | Ohsaki national health insurance cohort study | 23995 | 1994 to “1995–2003” | 60.76 | 65.42% | Cohort study |
|
| ||||||||
| Pinheiro et al. [16] | 2006 | America | Nurses' health study | 77418 | “1986, 2000” to “1986, 2002” | 52.94 | 56.87% | Cohort study |
|
| ||||||||
| McElroy et al. [17] | 2005 | America | US case-control study | 9347 | 1997–1999 | 20–69 | 54.98% | Case-control study |
|
| ||||||||
| Verkasalo et al. [18] | 2005 | Finland | Finnish twin cohort | 12222 | “1975, 1981” to “1976–1996” | 36.50 | — | Cohort study |
Table 2.
The outcome and related information included in this meta-analysis.
| Author | Year | Data collection | Breast cancer ascertainment | Sleep duration (h/d) and risk (95% CI) | Adjusted variable | Quality assessment |
|---|---|---|---|---|---|---|
| Xiao et al. [9] | 2016 | Questionnaire | State cancer registries; pathology reports; medical records |
<6: 1.09 (0.83–1.44) 6: 1.01 (0.78–1.30) 7: 1.19 (0.92–1.53) 8: reference ≥9: 1.07 (0.80–1.43) |
Age, enrollment year, enrollment state, race, education, income, marital status, BMI, physical activity, overall sitting, smoking, pack-year, number of live birth, age at first birth, length of breastfeeding, age at menarche, menopause status, hormone therapy, multivitamin, aspirin, diabetes, family history of cancer, alcohol consumption, and dietary intakes of total fat, fiber, folate and total calories | 8 |
|
| ||||||
| Hurley et al. [10] | 2015 | Questionnaire | California cancer registry | 3–6: 0.97 (0.91–1.04) 7–9: reference ≥10: 1.13 (0.86–1.50) |
Race/ethnicity, alcohol consumption, menopausal status, hormone therapy use | 6 |
|
| ||||||
| Wang et al. [11] | 2014 | Face-to-face interview | Medical records | ≤6: 1.62 (1.18–2.21) 6.1–8.9: reference ≥9: 1.58 (1.18–2.12) |
Age, education, BMI, age at menarche, menopausal status, parity, physical activity, breastfeeding, family history of breast cancer, other sleep factors | 7 |
|
| ||||||
| Vogtmann et al. [12] | 2013 | Interview | Pathology reports; medical records | ≤5: 0.89 (0.80–1.00) 6: 0.92 (0.85–0.98) 7: reference 8: 1.00 (0.93–1.07) ≥9: 1.05 (0.92–1.20) |
Age, clinical trial arm assignment, number of live births, age at menarche, age at menopause, BMI, energy expenditure, education, income, race/ethnicity, marital status, age at first birth, use of hormone therapy, history of benign breast disease, family history of breast cancer, alcohol consumption, smoking status | 8 |
|
| ||||||
| Wu et al. [13] | 2012 | In-person interview | National cancer registry | ≤6: reference 7: 1.00 (0.84–1.19) 8: 1.00 (0.84–1.21) ≥9: 0.89 (0.64–1.22) |
Age, year, dialect group, education, parity, BMI, menopausal status | 8 |
|
| ||||||
| Girschik et al. [14] | 2012 | Self-administered postal questionnaire | Western Australian cancer registry | <6: 1.04 (0.83–1.32) 6-7: 0.95 (0.79–1.14) 7-8: reference >8: 1.05 (0.83–1.33) |
Age, number of children, age at first birth, breastfeeding, menopausal status, use and duration of hormone therapy, alcohol consumption, comparative weight at the age of 30 years, melatonin, physical activity | 8 |
|
| ||||||
| Kakizaki et al. [15] | 2008 | Questionnaire | Miyagi prefectural cancer registry | ≤6: 1.67 (1.002–2.78) 7: reference 8: 0.99 (0.59–1.65) ≥9: 0.29 (0.09–0.98) |
Age, BMI, history of disease, family history of cancer, marital status, education, alcohol consumption, time spent walking, caloric intake, menopausal status, age at menarche, age at first delivery, number of deliveries, oral contraceptive drugs, hormone drug | 8 |
|
| ||||||
| Pinheiro et al. [16] | 2006 | Mailed questionnaire | Blinded medical chart review | ≤5: 0.93 (0.79–1.09) 6: 0.98 (0.91–1.06) 7: reference 8: 1.05 (0.97–1.13) ≥9: 0.95 (0.82–1.11) |
Age, BMI, height, history of benign breast disease, family history of breast cancer, parity and age at first birth, age at menarche, postmenopausal hormone use, physical activity, alcohol, caloric intake, smoking | 7 |
|
| ||||||
| McElroy et al. [17] | 2005 | Telephone interviews | State cancer registries | <5: 0.94 (0.62–1.44) 5–5.9: 0.82 (0.65–1.05) 6–6.9: 0.89 (0.79–1.01) 7–7.9: reference 8–8.9: 1.01 (0.91–1.11) ≥9: 1.01 (0.84–1.23) |
Age, state, parity, age at first full-term pregnancy, family history of breast cancer, alcohol consumption, BMI, menopause status, age at menopause, postmenopausal hormone use, marital status | 8 |
|
| ||||||
| Verkasalo et al. [18] | 2005 | Questionnaires | Finnish cancer registries | ≤4: 0.88 (0.11–6.91) 5: 0.91 (0.36–2.32) 6: 0.74 (0.44–1.27) 7: 0.81 (0.60–1.10) 8: reference 9: 0.64 (0.40–1.02) ≥10: 0.65 (0.24–1.75) |
Age, zygosity, social class, number of children, use of oral contraceptives, BMI, alcohol use, smoking, physical activity | 8 |
3.2. Association between Sleep Duration and Breast Cancer
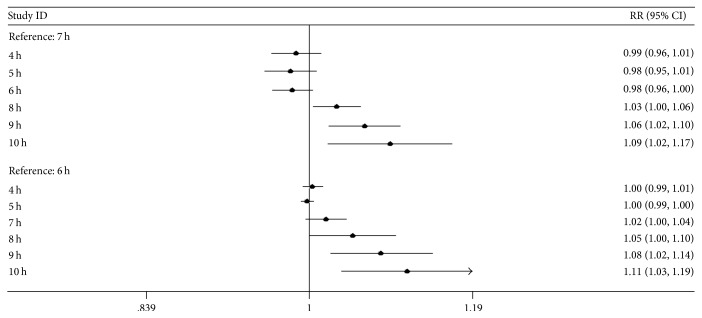
A J-shaped nonlinear trend between sleep duration and breast cancer incidence was shown in Figure 2 (Pnon-linear = 0.012). For the overall analysis, we used a fixed-effects model because there was no significant within-study heterogeneity (Pheterogeneity = 0.064). Because there was a nonlinear trend, we conducted a nonlinear dose-response meta-analysis to evaluate each additional sleep hour's risk of breast cancer. As Table 3 and Figure 3 show, compared with the reference hours (6 h or 7 h), with increasing sleep hours, the risk of breast cancer increased, and the increasing trend was significant (Ptrend = 0.028).
Figure 2.
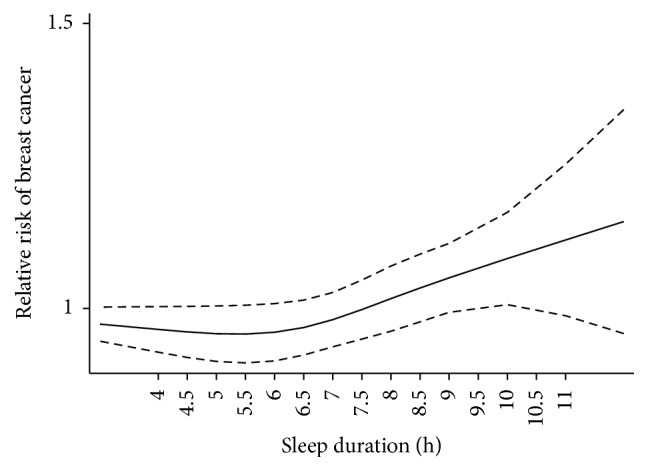
The plot of dose-response relationship between sleep duration and breast cancer risk.
Table 3.
The relative risks (RRs) for nonlinear and linear model.
| Number of studies | P heterogeneity | P non-linear | RR | P trend | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Nonlinear | Linear | ||||||||||||
| 4 h | 5 h | 6 h | 7 h | 8 h | 9 h | 10 h | 1 h increment | ||||||
| All | 10 | 0.064 | 0.012 | 0.986 | 0.980 | 0.982 | 1.000 | 1.03 | 1.061 | 1.091 | — | 0.028 | |
| 1.004 | 0.998 | 1.000 | 1.018 | 1.049 | 1.08 | 1.111 | |||||||
| Premenopausal | 4 | 0.132 | 0.139 | — | 1.012 | 0.198 | |||||||
| Postmenopausal | 5 | 0.241 | 0.298 | — | 1.003 | 0.506 | |||||||
| ER+ | 3 | 0.705 | 0.013 | 0.971 | 0.966 | 0.974 | 1.000 | 1.042 | 1.096 | 1.16 | — | 0.024 | |
| 0.997 | 0.992 | 1.000 | 1.027 | 1.070 | 1.126 | 1.192 | |||||||
| ER− | 3 | 0.018 | 0.139 | — | 1.035 | 0.352 | |||||||
Figure 3.
The trend of relationship between sleep duration and breast cancer risk.
3.3. Association between Sleep Duration and Breast Cancer according to Menopausal Status
Four studies [11, 14–16] and five studies [11, 13–16] reported the dose-response data in premenopausal and postmenopausal populations, respectively. For the nonlinear tests, we did not find nonlinear relationships between sleep duration and breast cancer risk in either premenopausal women or postmenopausal women (Pnon-linear = 0.139; Pnon-linear = 0.298). Therefore, we conducted a linear dose-response meta-analysis. The results showed that the relative risk (RR) of breast cancer was 1.012 in the premenopausal population and 1.003 in the postmenopausal population for every additional sleep hour; however, neither showed statistical significance (Ptrend = 0.198; Ptrend = 0.506).
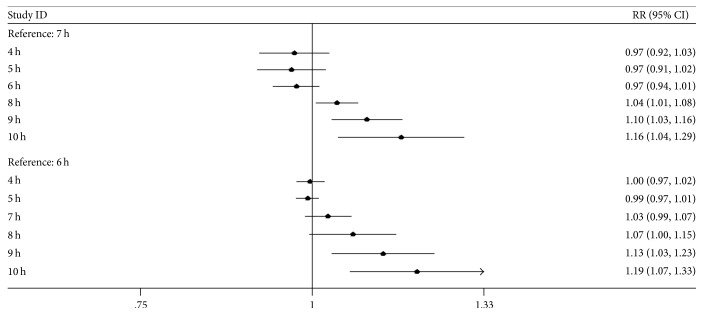
3.4. Association between Sleep Duration and Breast Cancer according to Estrogen Receptor (ER) Status
Three studies [9, 11, 12] reported dose-response data on ER+ and ER− breast cancer. According to the nonlinear test, there was a nonlinear relationship between sleep duration and ER+ breast cancer (Pnon-linear = 0.013) and a linear relationship between sleep duration and ER− breast cancer (Pnon-linear = 0.139). As shown in Table 3 and Figure 4, the risk of ER+ breast cancer increased with increasing sleep hours compared with the reference hours, and the increasing trend was significant (Ptrend = 0.024). Regarding ER− breast cancer, a linear dose-response meta-analysis showed that the RR of ER− breast cancer was 1.035 for every additional sleep hour (Ptrend = 0.352).
Figure 4.
The trend of relationship between sleep duration and ER+ breast cancer risk.
4. Discussion
Our meta-analysis included 10 studies involving 415,865 participants to reliably quantify the association between sleep duration and breast cancer risk. An increased risk trend was found between sleep duration and breast cancer; our study also indicated that, compared to women with a normal sleep duration, women with a longer sleep duration might have a significantly increased risk of breast cancer; this was not observed among women with a shorter sleep duration. Subgroup analysis for breast cancer by ER status also showed a positive association between sleep duration and the risk of ER+ breast cancer, although this was not observed for ER− breast cancer.
Before 2008, most published articles involving sleep duration and breast cancer risk reported null findings [15–18] or that shorter sleep duration might be a risk factor [15] and longer sleep duration might be a preventative factor for breast cancer [15, 16, 18], which is inconsistent with our findings. However, after 2008, an increasing number of studies have reported slightly positive associations between longer sleep hours and breast cancer, in agreement with the findings in our meta-analysis. In the US case-control study, a positive trend for breast cancer was found for every additional sleep hour (OR = 1.06, 95% CI = 1.01~1.11) [13], and another study observed a positive association between sleep duration and breast cancer incidence with a RR of 1.58 (95% CI = 1.18~2.12) for 9 h or more compared to the reference hours (6.1 h to 8.9 h) [11]. Among the studies of breast cancer by ER status, Vogtmann et al.'s study observed a positive trend for increasing sleep duration with the risk of ER+ breast cancer [12], and Wang et al.'s study reported that longer sleep might be a risk factor for ER+ breast cancer compared to reference hours [11], which is consistent with our findings. Due to controversial results, four meta-analyses of the relationship between sleep duration and breast cancer have been previously published [22–25]; most of these articles pooled the results using a traditional two-category model. The most recent meta-analysis was published in 2012 with only six original articles included (four articles published before 2008) and found no significant association between either short or long sleep duration and breast cancer risk [22]. Therefore, our study might provide the most comprehensive assessment and robust evidence to evaluate the relationship between sleep duration and breast cancer risk.
The positive association between sleep duration and risk of breast cancer and ER+ breast cancer in our study was unexpected, as the melatonin hypothesis suggests that a short sleep duration is associated with decreased levels of melatonin, and melatonin is known to regulate susceptibility to cancer and to have antiproliferative activity [26]. However, Wu et al.'s research suggested that sleep duration might be inversely associated with urinary melatonin levels (aMT6s levels were 1.88, 1.85, 1.23, and 1.32 for ≤6, 7, 8, and ≥9 h of sleep, resp.; Ptrend = 0.018) [13]. In addition, lower melatonin levels were correlated with higher estrogen levels [27], and increased estrogen exposure has been strongly linked to ER+ breast cancer [28, 29], which indicates that a link between longer sleep and breast cancer is biologically plausible. Additionally, inflammation was also considered to initiate and promote breast cancer development. Indeed, some authors believed that excessive sleep might lead to elevated levels of systemic inflammation and increase some inflammatory biomarkers, such as CRP and IL-6, which might predispose an individual to breast cancer [30, 31]. Furthermore, longer sleep might also increase the breast cancer risk through increased levels of cortisol and reductions in natural killer cell activity [32, 33].
There were several limitations of our study. First, misclassification bias might exist in our study because sleep duration was self-reported in the included studies. Compared with wrist actigraphy, which was an objective measure of sleep, self-reported sleep duration showed poor validation, and the sleep duration reported in questionnaires tended to be longer than the measured duration [34, 35]. However, subjectively measured sleep is the only practical option in large population studies. Second, the assessment of sleep duration in most studies was based on different time scales, which might influence the accuracy of our results. Third, other aspects of sleep such as snoring, sleep quality, and sleep disorder diseases that might influence breast cancer were not considered in our included studies. Indeed, studies have reported that long-term sleep duration might reflect poor sleep quality [36], and poor sleep quality might be related to cancer development. Even with the above-mentioned limitations, our study had several strengths. The mean Newcastle-Ottawa Scale (NOS) score of our study was 7.6, which means that the quality of the included studies was high and the results were reliable. Moreover, most included studies had adequately adjusted for potential confounders to reduce their possible impact on the association between sleep duration and breast cancer. Third, we used restricted cubic splines to fit potential dose-response trends, which made full use of the available data and had higher statistical power than traditional binary meta-analysis. Therefore, our meta-analysis might provide useful and robust evidence to evaluate the relationship between sleep duration and breast cancer.
5. Conclusions
In conclusion, our dose-response meta-analysis indicates that women with longer sleep durations might have a significantly increased risk of breast cancer, especially of ER+ breast cancer, compared to that of women with a normal sleep duration.
Acknowledgments
This work was supported by the National Natural Science Foundation of China (81000943) and Key Laboratory Programme of Education Department of Liaoning Province (LS2010165).
Contributor Information
Yingying Xu, Email: lovecmustar@yahoo.com.
Huimian Xu, Email: xuhuimian@126.com.
Conflicts of Interest
The authors declare no conflicts of interest.
Authors' Contributions
Yingying Xu, Huimian Xu, and Chunyang Lu conceived and designed the experiments; Chunyang Lu, Hao Sun, Jinyu Huang, and Songcheng Yin performed the experiments; Hao Sun, Chunyang Lu, Jinyu Huang, and Songcheng Yin analyzed the data; Wenbin Hou, Junyan Zhang, and Yanshi Wang contributed reagents/materials/analysis tools; Chunyang Lu, Hao Sun, and Yingying Xu wrote the paper. Chunyang Lu and Hao Sun contributed equally to this work.
References
- 1.Anderson B. O., Lipscomb J., Murillo R. H., Thomas D. B. Breast cancer. In: Gelband H., Jha P., Sankaranarayanan R., Horton S., editors. Cancer: Disease Control Priorities. 3rd. Vol. 3. Washington, DC, USA: The International Bank for Reconstruction and Development / The World Bank; 2015. [PubMed] [Google Scholar]
- 2.Colditz G. A. Epidemiology and prevention of breast cancer. Cancer Epidemiology Biomarkers and Prevention. 2005;14(4):768–772. doi: 10.1158/1055-9965.EPI-04-0157. [DOI] [PubMed] [Google Scholar]
- 3.Cappuccio F. P., Cooper D., Delia L., Strazzullo P., Miller M. A. Sleep duration predicts cardiovascular outcomes: a systematic review and meta-analysis of prospective studies. European Heart Journal. 2011;32(12):1484–1492. doi: 10.1093/eurheartj/ehr007. [DOI] [PubMed] [Google Scholar]
- 4.Shan Z., Ma H., Xie M., et al. Sleep duration and risk of type 2 diabetes: a meta-analysis of prospective studies. Diabetes Care. 2015;38(3):529–537. doi: 10.2337/dc14-2073. [DOI] [PubMed] [Google Scholar]
- 5.Wu Y., Zhai L., Zhang D. Sleep duration and obesity among adults: A meta-analysis of prospective studies. Sleep Medicine. 2014;15(12):1456–1462. doi: 10.1016/j.sleep.2014.07.018. [DOI] [PubMed] [Google Scholar]
- 6.Xi B., He D., Zhang M., Xue J., Zhou D. Short sleep duration predicts risk of metabolic syndrome: Asystematic review and meta-analysis. Sleep Medicine Reviews. 2014;18(4):293–297. doi: 10.1016/j.smrv.2013.06.001. [DOI] [PubMed] [Google Scholar]
- 7.Blask D. E. Melatonin, sleep disturbance and cancer risk. Sleep Medicine Reviews. 2009;13(4):257–264. doi: 10.1016/j.smrv.2008.07.007. [DOI] [PubMed] [Google Scholar]
- 8.Morris C. J., Aeschbach D., Scheer F. A. J. L. Circadian system, sleep and endocrinology. Molecular and Cellular Endocrinology. 2012;349(1):91–104. doi: 10.1016/j.mce.2011.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Xiao Q., Signorello L. B., Brinton L. A., Cohen S. S., Blot W. J., Matthews C. E. Sleep duration and breast cancer risk among black and white women. Sleep Medicine. 2016;20:25–29. doi: 10.1016/j.sleep.2015.11.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hurley S., Goldberg D., Bernstein L., Reynolds P. Sleep duration and cancer risk in women. Cancer Causes and Control. 2015;26(7):1037–1045. doi: 10.1007/s10552-015-0579-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wang P., Ren F.-M., Lin Y., et al. Night-shift work, sleep duration, daytime napping, and breast cancer risk. Sleep Medicine. 2015;16(4):462–468. doi: 10.1016/j.sleep.2014.11.017. [DOI] [PubMed] [Google Scholar]
- 12.Vogtmann E., Levitan E. B., Hale L., et al. Association between sleep and breast cancer incidence among postmenopausal women in the Women's Health Initiative. Sleep. 2013;36(10):1437–1444. doi: 10.5665/sleep.3032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wu A. H., Stanczyk F. Z., Wang R., Koh W.-P., Yuan J.-M., Yu M. C. Sleep duration, spot urinary 6-sulfatoxymelatonin levels and risk of breast cancer among Chinese women in Singapore. International Journal of Cancer. 2012;132(4):891–896. doi: 10.1002/ijc.27653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Girschik J., Heyworth J., Fritschi L. Self-reported sleep duration, sleep quality, and breast cancer risk in a population-based case-control study. American Journal of Epidemiology. 2013;177(4):316–327. doi: 10.1093/aje/kws422. [DOI] [PubMed] [Google Scholar]
- 15.Kakizaki M., Kuriyama S., Sone T., et al. Sleep duration and the risk of breast cancer: the Ohsaki Cohort Study. British Journal of Cancer. 2008;99(9):1502–1505. doi: 10.1038/sj.bjc.6604684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Pinheiro S. P., Schernhammer E. S., Tworoger S. S., Michels K. B. A prospective study on habitual duration of sleep and incidence of breast cancer in a large cohort of women. Cancer Research. 2006;66(10):5521–5525. doi: 10.1158/0008-5472.CAN-05-4652. [DOI] [PubMed] [Google Scholar]
- 17.McElroy J. A., Newcomb P. A., Titus-Ernstoff L., Trentham-Dietz A., Hampton J. M., Egan K. M. Duration of sleep and breast cancer risk in a large population-based case-control study. Journal of Sleep Research. 2006;15(3):241–249. doi: 10.1111/j.1365-2869.2006.00523.x. [DOI] [PubMed] [Google Scholar]
- 18.Verkasalo P. K., Lillberg K., Stevens R. G., et al. Sleep duration and breast cancer: a prospective cohort study. Epidemiology. 2005;16(5):p. S115. doi: 10.1097/00001648-200509000-00288. [DOI] [PubMed] [Google Scholar]
- 19.Stroup D. F., Berlin J. A., Morton S. C., et al. Meta-analysis of observational studies in epidemiology: a proposal for reporting. Journal of the American Medical Association. 2000;283(15):2008–2012. doi: 10.1001/jama.283.15.2008. [DOI] [PubMed] [Google Scholar]
- 20.Wells G. A., Shea B. J., O'Connell D., et al. The Newcastle–Ottawa Scale (NOS) for Assessing the Quality of Non-Randomized Studies in Meta-Analysis (vol. 2000)
- 21. https://sleepfoundation.org/how-sleep-works/how-much-sleep-do-we-really-need.
- 22.Yang W.-S., Deng Q., Fan W.-Y., Wang W.-Y., Wang X. Light exposure at night, sleep duration, melatonin, and breast cancer: a dose-response analysis of observational studies. European Journal of Cancer Prevention. 2014;23(4):269–276. doi: 10.1097/CEJ.0000000000000030. [DOI] [PubMed] [Google Scholar]
- 23.Qin Y., Zhou Y., Zhang X., Wei X., He J. Sleep duration and breast cancer risk: a meta-analysis of observational studies. International Journal of Cancer. 2014;134(5):1166–1173. doi: 10.1002/ijc.28452. [DOI] [PubMed] [Google Scholar]
- 24.Wang X., Cairns B. J., Travis R. C. Sleep duration and breast cancer risk: a meta-analysis. Journal of Epidemiology & Community Health. 2010;64, supplement 1:A32–A32. doi: 10.1136/jech.2010.120956.80. [DOI] [Google Scholar]
- 25.Zhao H., Yin J.-Y., Yang W.-S., et al. Sleep duration and cancer risk: A systematic review and meta-analysis of prospective studies. Asian Pacific Journal of Cancer Prevention. 2013;14(12):7509–7515. doi: 10.7314/APJCP.2013.14.12.7509. [DOI] [PubMed] [Google Scholar]
- 26.Vijayalaxmi, Thomas C. R., Jr., Reiter R. J., Herman T. S. Melatonin: from basic research to cancer treatment clinics. Journal of Clinical Oncology. 2002;20(10):2575–2601. doi: 10.1200/jco.2002.11.004. [DOI] [PubMed] [Google Scholar]
- 27.Schernhammer E. S., Rosner B., Willet W. C., Laden F., Colditz G. A., Hankinson S. E. Epidemiology of urinary melatonin in women and its relation to other hormones and night work. Cancer Epidemiology Biomarkers and Prevention. 2004;13(6):936–943. [PubMed] [Google Scholar]
- 28.Clemons M., Goss P. Estrogen and the risk of breast cancer. New England Journal of Medicine. 2001;344(4):276–285. doi: 10.1056/NEJM200101253440407. [DOI] [PubMed] [Google Scholar]
- 29.Huang W.-Y., Newman B., Millikan R. C., Schell M. J., Hulka B. S., Moorman P. G. Hormone-related factors and risk of breast cancer in relation to estrogen receptor and progesterone receptor status. American Journal of Epidemiology. 2000;151(7):703–714. doi: 10.1093/oxfordjournals.aje.a010265. [DOI] [PubMed] [Google Scholar]
- 30.Frydenberg H., Thune I., Lofterød T., et al. Pre-diagnostic high-sensitive C-reactive protein and breast cancer risk, recurrence, and survival. Breast Cancer Research and Treatment. 2016;155(2):345–354. doi: 10.1007/s10549-015-3671-1. [DOI] [PubMed] [Google Scholar]
- 31.Prather A. A., Vogelzangs N., Penninx B. W. J. H. Sleep duration, insomnia, and markers of systemic inflammation: results from the Netherlands Study of Depression and Anxiety (NESDA) Journal of Psychiatric Research. 2015;60:95–102. doi: 10.1016/j.jpsychires.2014.09.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Dettenborn L., James G. D., Van Berge-Landry H., Valdimarsdottir H. B., Montgomery G. H., Bovbjerg D. H. Heightened cortisol responses to daily stress in working women at familial risk for breast cancer. Biological Psychology. 2005;69(2):167–179. doi: 10.1016/j.biopsycho.2004.07.004. [DOI] [PubMed] [Google Scholar]
- 33.Strayer D. R., Carter W. A., Brodsky I. Familial occurrence of breast cancer is associated with reduced natural killer cytotoxicity. Breast Cancer Research and Treatment. 1986;7(3):187–192. doi: 10.1007/BF01806249. [DOI] [PubMed] [Google Scholar]
- 34.Girschik J., Fritschi L., Heyworth J., Waters F. Validation of self-reported sleep against actigraphy. Journal of Epidemiology. 2012;22(5):462–468. doi: 10.2188/jea.JE20120012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Lauderdale D. S., Knutson K. L., Yan L. L., Liu K., Rathouz P. J. Self-reported and measured sleep duration: how similar are they? Epidemiology. 2008;19(6):838–845. doi: 10.1097/EDE.0b013e318187a7b0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Bliwise D. L., Young T. B. The parable of parabola: what the U-shaped curve can and cannot tell us about sleep. Sleep. 2007;30(12):1614–1615. doi: 10.1093/sleep/30.12.1614. [DOI] [PMC free article] [PubMed] [Google Scholar]