Abstract
Small bowel diverticulosis represents an uncommon pathology that is often misdiagnosed, since it causes non-specific gastrointestinal symptoms. It is defined by the existence of multiple diverticula, which are located most frequently in the jejunum. Diagnosis often occurs following the presentation of related complications such as diverticulitis, haemorrhage, perforation or obstruction. Intestinal obstruction can be caused by inflammatory stenosis due to repeated episodes of diverticulitis, volvulus, intussusception or the presence of enteroliths. Here, we report a case of multiple jejunal diverticula causing acute intestinal obstruction.
INTRODUCTION
Diverticulosis of the small intestine is characterized by the presence of multiple diverticula. Of these, 80% are found in the jejunum, 15% in the ileum and 5% in both [1]. Jejunal diverticulosis may be either congenital or acquired. Its incidence varies from 0.2 to 1.3% in autopsy studies and 2.3% in radiographic findings [1]. Prevalence increases with age, peaking in the sixth and seventh decades. Small bowel motility disorders with increased intraluminal pressure are considered to be the main aetiological factors for its development [2]. Although it is often asymptomatic, it can lead to severe complications including perforation, haemorrhage, enterolith formation, diverticulitis and intestinal obstruction [3].
We describe one such complication, acute bowel obstruction, and discuss the diagnostic and therapeutic approach.
CASE REPORT
A 72-year-old patient with hiatal hernia and colonic diverticulosis had a history of previous surgery for left inguinal hernia (10 years before), midline hernia and acute appendicitis (6 years before). He had recurrent bowel obstructions for a year that resolved spontaneously and were initially attributed to post-operative bands.
In the last episode, he was hospitalized. He had several episodes of vomiting without stopped transit. The abdomen was somewhat distended. There was no fever or signs of peritonitis. The supported diagnosis was small bowel obstruction caused by post-operative bands. Exploratory laparotomy was decided upon rather than laparoscopy as the patient had a history of abdominal surgery in addition to the context of acute intestinal obstruction. Intraoperatively, we noted the existence of jejunal, colonic and bladder diverticula. The obstruction was caused by adhesions and bands that had formed between the diverticula, the abdominal wall and the small intestine. We resected 60 cm of the proximal jejunum, removing all diverticula sized up to 5 cm (Fig. 1 ). Intestinal continuity was restored by a jejuno-jejunal anastomosis located 30 cm downstream of the duodeno-jejunal flexure. The post-operative course was uneventful.
Figure 1:
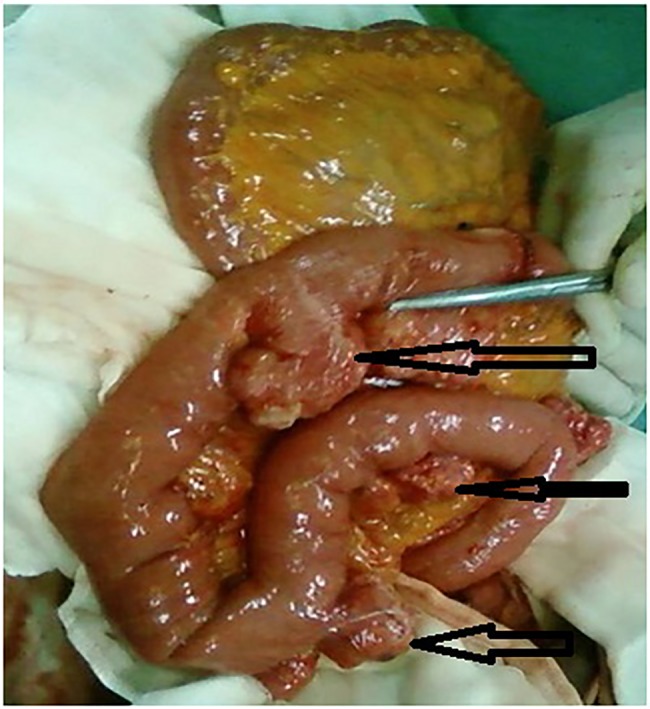
Intraoperative findings: multiple diverticula (arrows) arising at the mesenteric border of the jejunum.
DISCUSSION
Jejunal diverticulosis is a rare entity [1]. Jejunal diverticula are characterized by the herniation of mucosa and submucosa through the muscular layer at the point where blood vessels penetrate the intestinal wall [4]. This explains their typical location at the mesenteric side of the bowel [1]. Diverticula are more frequently found in the jejunum (80%) than other parts of the small bowel due to the greater diameter of the penetrating jejunal arteries [4]. Jejunal diverticula are usually multiple, in contrast to congenital Meckel's diverticulum, and tend to be larger and greater in number in the proximal jejunum.
The aetiology of jejunal diverticulosis is not fully understood. Krishnamurthy et al. [5] focussed on abnormalities of the smooth muscles and myenteric plexus in order to explain intestinal dyskinesia. Kongara et al. [2] performed manometric studies on the small bowel and described functional abnormalities in patients with small bowel diverticula. These facts support the hypothesis that irregular intestinal contractions generate increased segmental intraluminal pressure, favouring the formation of diverticula. A correlation between intestinal diverticulosis and rare neuromuscular disorders, such as mitochondrial neurogastrointestinal encephalomyopathy and Elhers–Danlos syndrome, has been described [6, 7]. In addition to jejunal diverticulosis, our patient had other ‘hernias’ such as inguinal hernia, midline hernia, hiatal hernia, colonic diverticulosis and gallbladder diverticulum. These findings favour the hypothesis that muscular disorders contribute to diverticula formation.
Some diseases, such as progressive systemic sclerosis and amyloidosis, are associated with jejuno-ileal diverticulosis. Indeed, lesions of the extracellular matrix lead to intestine dysmotility disorders that cause an increase in intraluminal pressure and, therefore, the formation of bowel diverticula.
The prevalence of jejunal diverticulosis is difficult to ascertain because it is often asymptomatic, symptoms are not specific (e.g. discomfort, dyspepsia) and little clinical significance has been attributed to these symptoms. Although no studies published to date have analysed age group incidence in large populations, we have noted an increase in incidence with age. The disease presents a peak incidence in the sixth and seventh decades, with male predominance [4, 8]. The size of small bowel diverticula varies from a few millimetres up to >3 cm.
The disease is usually asymptomatic. Symptoms are noted in 29% of cases, but many are misdiagnosed as dyspepsia or irritable bowel syndrome. A symptom triad observed in these patients has been described as ‘flatulent dyspepsia', associating epigastric pain, abdominal discomfort and flatulence 1–2 h after meals [8].
Complications of jejunal diverticulosis include obstruction, haemorrhage, diverticulitis and perforation [3], and occur in 10–30% of the cases. The incidence of each complication is variable and difficult to assess due to the small sample sizes of most studies. However, it seems that diverticulitis and perforation are the most common complications (2–6%), followed by bleeding and obstruction (2%). Mechanical obstruction can be caused by adhesions and peritoneal bands developing after many episodes of diverticulitis, as was the case with our patient. In addition, sizeable stones enclosed in the diverticula may apply pressure to the adjacent bowel wall or may escape from the diverticulum causing intestinal occlusion.
Diagnosis is usually made when the disease becomes symptomatic or complicated as simple radiographs are not sufficient for diagnosis to be made. In cases of complicated jejunal diverticulosis, a series of plain abdominal X-ray may demonstrate distension of the small bowel, air–fluid levels and pneumoperitoneum. Barium follow-through studies and enteroclysis are more specific, although their utility is limited in emergency situations. Computed tomography may show focal areas of out-pouching on the mesenteric side of the bowel, localized intestinal wall thickening due to inflammation or oedema, abscesses, free abdominal fluids and pneumoperitoneum. Multi-slice computed tomography seems to be promising and more specific. Laparoscopy is a valid diagnostic approach for complicated cases, and total laparoscopic treatment of a sizeable jejunal diverticulum was recently reported [9].
Asymptomatic jejunal diverticulosis does not require bowel resection. Some authors believe that patients with chronic symptoms can be treated conservatively. Resection becomes imperative only when symptoms are persistent or refractory to treatment. Others who have based their research on data demonstrating that jejuno-ileal diverticula (compared with diverticula of the duodenum) potentially perforate and develop abscesses, recommend a more aggressive surgical approach in view of the lower post-operative morbidity of elective bowel resection [10]. Exploratory laparotomy and resection of the affected intestinal segment with primary anastomosis are mandatory in cases of perforation, abscesses or obstruction. The extent of the segmental resection depends on the length of the bowel affected by diverticula. If diverticula involve a long intestinal segment, as is commonly found, resection should be limited to the perforated or inflamed part in order to avoid short bowel syndrome.
CONFLICT OF INTEREST STATEMENT
None declared.
REFERENCES
- 1. Kassahun WT, Fangmann J, Harms J, Bartels M, Hauss J. Complicated small-bowel diverticulosis: a case report and review of the literature. World J Gastroenterol 2007;13:2240–2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Kongara KR, Soffer EE. Intestinal motility in small bowel diverticulosis: a case report and review of the literature. J Clin Gastroenterol 2000;30:84–6. [DOI] [PubMed] [Google Scholar]
- 3. Natarajan K, Phansalkar M, Varghese RG, Thangiah G. Jejunal diverticulosis with perforation – a challenging differential diagnosis of acute abdomen: case report. J Clin Diagn Res 2015;9:ED03–ED04. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Kouraklis G, Glinavou A, Mantas D, Kouskos E, Karatzas G. Clinical implications of small bowel diverticula. IMAJ 2002;4:431–3. [PubMed] [Google Scholar]
- 5. Krishnamurthy S, Kelly MM, Rohrmann CA, Schuffler MD. Jejunal diverticulosis. A heterogeneous disorder caused by a variety of abnormalities of smooth muscle or myenteric plexus. Gastroenterology 1983;85:538–47. [PubMed] [Google Scholar]
- 6. Aksoy F, Demirel G, Bilgiç T, Güngör IG, Ozçelic A. A previously diagnosed mitochondrial neurogastrointestinal encephalomyopathy patient presenting with perforated ileal diverticulitis. Turk J Gastroenterol 2005;16:228–31. [PubMed] [Google Scholar]
- 7. Shapira O, Mavor E, Simon D, Rothstein H, Pfeffermann R. Multiple giant gastrointestinal diverticula complicated by perforated jejunoileal diverticulitis in Marfan syndrome. Dig Surg 1992;9:58–60. [Google Scholar]
- 8. Falidas E, Vlachos K, Mathioulakis S, Archontovasilis F, Villias C. Multiple giant diverticula of the jejunum causing intestinal obstruction: report of a case and review of the literature. World J Emerg Surg 2011;6:8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Cang N, Khullar R, Sharma A, Soni V, Baijal M, Chowbey P. Total laparoscopic management of large complicated jejunal diverticulum. J Minim Access Surg 2009;5:115–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Bitterling H, Rock C, Reiser M. Computed tomography in the diagnosis of inflammatory bowel disease-methodology of MSCT and clinical results. Radiologe 2003;43:17–25. [DOI] [PubMed] [Google Scholar]


