In this prospective study, we explore the role of social intuition and social information in the evaluation and diagnosis of physical child abuse.
Abstract
BACKGROUND:
Poor and minority children with injuries concerning for abuse are evaluated and diagnosed for abuse differentially. We hypothesized that 2 steps in the decision-making process would influence evaluation and diagnosis: social intuition from meeting the family and objective social information associated with child abuse risk.
METHODS:
Between 2009 and 2013, 32 child abuse pediatricians (CAPs) submitted 730 child abuse consultations including original medical evaluations and diagnoses. CAPs evaluated and diagnosed each other’s cases. Comparisons of evaluations and diagnoses were made by levels of social understanding available to the CAP: meeting the family (social intuition and information), reading the case (social information), and reading the case without social information. Evaluations were compared with a consensus gold standard by using logistic regression modeling adjusting for child and CAP characteristics. Diagnostic categories were compared by level of social understanding and diagnostic certainty by using contingency tables.
RESULTS:
CAPs without access to social intuition were approximately twice as likely to perform gold standard evaluations for neurotrauma and long bone fracture compared with CAPs who met families. Diagnostic agreement fell from 73.3% (95% confidence interval [CI]: 70.1%–76.5%) when social information was present to 66.5% (95% CI: 63.1%–70.0%) when social information was restricted. In cases with less certainty, agreement dropped to 51.3% (95% CI: 46.0%–56.7%).
CONCLUSIONS:
Social intuition and information play a role in the physical child abuse decision-making process, which may contribute to differential diagnosis. Simple interventions including decision tools, check lists, and peer review may structure evaluations to ensure children’s equal treatment.
What’s Known on This Subject:
Disparities in diagnosis and evaluation of injured children for suspected abuse differ by the child’s race and socioeconomic status.
What This Study Adds:
Child abuse pediatricians use of social intuition from meeting families and social information from review of risk indicators influences their evaluations and diagnoses of injured children. Social information and intuition have a stronger influence in cases with less diagnostic certainty.
Poor children and minority children who have injuries concerning for physical abuse are evaluated differently than children with higher socioeconomic or nonminority status.1,2 Physicians are more willing to entertain the diagnosis of abuse in poor children than children with higher socioeconomic status with the same injury, and more likely to seek occult injuries associated with abuse in minority children than in white children with the same presentation.3,4 Why physicians evaluate and offer diagnoses for children from these groups differently is not well described but may be related to the process of decision-making. Clinical decision-making relies on 2 cognitive processes: intuitive thinking that is fast and automatic and analytic thinking that requires focused attention.5 Intuitive thinking is used for complicated everyday decisions because it increases cognitive efficiency; as a subconscious process, however, it may cause diagnostic error.6
To characterize the role of social understanding in diagnostic decision-making in suspected physical abuse, we invited a group of child abuse pediatricians (CAPs) to participate in a study of physical child abuse diagnosis. For this study, we considered 2 steps in the decision-making process: the medical evaluation and the medical diagnosis. We hypothesized that change in physician perception of a child’s social risk would change CAP evaluation and diagnosis of children with injuries suspicious for physical abuse. We further hypothesized that changes in medical diagnosis observed with changes in perceived social risk would be more common in difficult cases in which the medical history and physical findings were concerning but not specific for a diagnosis of abuse. We considered 2 levels of social understanding that may influence CAP evaluation and diagnosis of a child referred for suspected physical abuse. The first level is social intuition, the subconscious, intuitive perception or “gut” feel associated with a face-to-face meeting between CAP, child, and family. The second level is social information or knowledge of risk indicators and social cues in the consultation note that might sway a difficult diagnostic decision.
Methods
Study Context
We collected inpatient medical consultation notes by CAPs for 3 types of injury cases referred for child physical abuse consultation from 2009 to 2013. The study was approved by the Institutional Review Board for the University of Utah and each participant’s institution. A Certificate of Confidentiality was obtained from the National Institute of Child Health and Human Development.
Participants
Thirty-two CAPs were recruited from 2 professional physician child maltreatment groups: the Ray E. Helfer Society and the American Academy of Pediatrics, Section on Child Abuse and Neglect. To be eligible, CAPs were required to have 5 years in pediatric practice postresidency, pediatric board certification, spend at least 50% of their clinical time evaluating possible child abuse cases including physical abuse, and have access to an institutional review board. Participants provided basic demographic information about themselves.
Overview
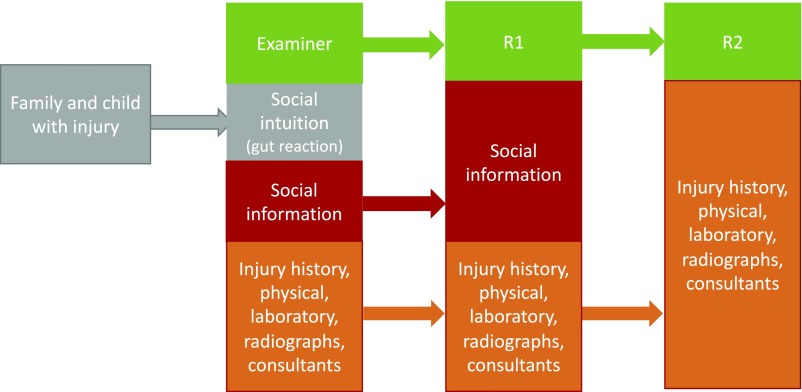
To test whether evaluation or diagnosis of physical child abuse might differ on the basis of 2 levels of social understanding, we systematically decreased the amount of information that CAPs had about a case. The examining CAP met the family, examined the child, and had access to social intuition and information. Social information included risk indicators (eg, child poverty) and social cues (eg, mom appeared disheveled). A second CAP reviewed the examiner’s written report and had knowledge of available social information but no intuitive perceptions from meeting the family or information about race. A third CAP reviewed the written report from which social information had been removed, unlinking medical decision-making from both levels of social understanding. All CAPs had the history of the injury event, past medical history, physical examination, laboratory and radiologic findings, and consultant reports. Each participant served as examiner, first reviewer (R1), and second reviewer (R2) throughout the study. As examiners, participating CAPs submitted deidentified medical consultation notes from their own clinical practices. In the R1 role, CAPs read unedited medical consultation notes submitted by their peers, but had no personal interaction with the patient or family, and thus no access to social intuition inherent to the examiner role. In the R2 role, CAPs read medical consultation notes scrubbed of all social information removing access to both social intuition and social information (Fig 1).
FIGURE 1.
Model displays decreasing levels of social understanding and social information from the examining CAP through R2.
Study Procedures and Definitions
Social Risk Perception
For each case, CAPs rated the social risk of abuse for the child (perceived social risk) by using a sliding scale from 1 (low) to 100 (high). Social risk perception was used to test whether lower levels of social understanding affected CAP perception.
Decision-Making
We considered 2 distinct points of decision-making: the medical evaluation and the medical diagnosis.
Medical Evaluation
The required elements of a CAP medical evaluation for each injury type were defined through an online Delphi process previously described (Supplemental Table 5) and served as our gold standard for comparison.7 Complete evaluations included all elements of the gold standard. Incomplete evaluations missed 1 or more required elements. For example, the medical evaluation of a child presenting with neurotrauma required these elements to be complete: a head computed tomography or MRI, a skeletal survey, an ophthalmology examination, a complete blood count, a prothrombin time or partial thromboplastin time, and an aspartate aminotransferase or alanine aminotransferase.
Medical Diagnosis
CAPs indicated a diagnosis for each case, selecting probable abuse (abuse) or probable not abuse (not abuse) for cases in which an abuse determination could be reached on the basis of available medical information. For cases in which an abuse determination was not possible, CAPs could indicate an indeterminate diagnosis.
Diagnostic Certainty
CAPs rated certainty for each diagnosis of abuse or not abuse on a scale of 1 (not certain) to 100 (very certain). Certainty for indeterminate cases was not requested. Difficult cases included determinate cases with certainty falling below the median level of certainty for examiners across all cases.
Case Preparation
Each CAP submitted completed consultation notes every 3 months. CAPs selected notes at random from their clinical consultations to reduce selection bias. Injury types were limited to neurotrauma, long bone fracture, or skull fracture in children up to 4 years old. A secure, Web-based interface prompted CAPs to enter the original text of their consultation notes in a standard medical format including the history of presenting illness, past medical history, review of systems, family history, social history, and physical examination. CAPs entered their requested laboratory studies with results, uploaded radiographs with interpretations, and uploaded consultants requested and the consultant reports. The interface then prompted the CAP to rate their perception of social risk for abuse, their diagnosis, and diagnostic confidence.
The investigators prepared 2 versions of each case for CAPs to review. (Process shown in Supplemental Information.) For R1, the investigators deidentified the case and removed race and/or ethnicity, leaving all other textual elements unchanged. For R2, investigators removed social information not needed to understand the injury mechanism from the R1 deidentified cases. For this step, a second investigator reviewed the altered R2 case to ensure removal of all risk indicators except for retention of the mechanism of injury. For example, in a case of a 2-year-old who sustained a skull fracture after falling from a shopping cart, the description of the injury mechanism and witness statements would be preserved, but information about parental employment, living situation, and marital status would be removed. Cases were randomly assigned to CAPs to review, ensuring that the case was not assigned back to the examining CAP or the CAP’s institution.
Analysis
Differences in the level of diagnostic certainty were compared by using the Wilcoxon rank test. Stratified tests based on the diagnosis were performed to account for potential interaction between diagnosis and diagnostic certainty. Risk perception was compared by using the Mann–Whitney U test.
Medical Evaluation
To understand if medical evaluations differed among examiners R1 and R2, we compared the relationship between CAP role and requesting a complete evaluation by using the McNemar test for paired data. A logistic regression model with an outcome of complete evaluation request (yes or no) was developed by using general estimating equations to account for clustering within cases and clustering of cases within reviewers. Covariates included child age and physician characteristics including physician experience (<10 vs 10+ years), sex, and whether the physician was a self-identified underrepresented minority.8 Models were stratified by age when the requirements for a complete evaluation differed by age category. Because an insufficient number of required elements were identified for children with skull fractures and children over 2 years of age with long bone fractures, analyses of complete evaluations exclude these cases; however, they are included in the analysis of diagnosis.
Medical Diagnosis
Percent diagnostic agreement was calculated with 95% confidence intervals (CIs) between the examiner and R1 and R1 and R2 for all cases and difficult cases. Contingency tables were generated to calculate percent change in diagnostic categories (abuse, not abuse, indeterminate).
Results
The 32 CAP participants contributed 730 cases of children with suspected physical abuse. CAPs were experienced (63% with 10 years or more experience), primarily women (84%), and nonminority (81%). Children identified in CAP consultations had a median age of 7 months (interquartile range [IQR]: 3–13 months), were majority boys (58.5%), minority (51.0%), and publicly insured (74.5%). The cases, by design, were divided almost equally into neurotrauma (33%), long bone fracture (39%), and skull fracture (28%).
Perception of Social Risk
CAP risk perception decreased from R1 to R2, demonstrating that our method of removing risk indicators was effective (Table 1).
TABLE 1.
Perceived Social Risk and Degree of Certainty by Examiner, R1, and R2
| Perceived Social Riska | |||
|---|---|---|---|
| Abuse (n = 379) | Not Abuse (n = 241) | Indeterminate (n = 106) | |
| Median (IQR) | Median (IQR) | Median (IQR) | |
| Examiner | 70 (50–80) | 30 (20–55) | 50 (25–65) |
| R1 | 75 (50–90) | 30 (15–60) | 53 (25–75) |
| R2 | 50 (25–72) | 26 (11–50) | 38 (18–50) |
| Certainty of diagnosisb | |||
| Examiner | 95 (86–100) | 85 (80–90) | — |
| R1 | 90 (80–99) | 81 (80–90) | — |
| R2 | 91 (80–98) | 81 (70–90) | — |
| Certainty of diagnosis in cases in which examiner and reviewers all performed complete examinationb | |||
| Abuse (n = 205) | Not Abuse (n = 149) | ||
| Examiner | 95 (89–100) | 85 (80–91) | — |
| R1 | 95 (82–100) | 80 (71–90) | — |
| R2 | 90 (80–98) | 82 (70–90) | — |
—, not applicable.
Examiner to R1 comparison statistically important (P < .05) for abuse cases; examiner to R2 and R1 to R2 statistically important (P < .01) for all case types.
Comparison statistically important among examiner to R1 and examiner to R2 (P < .001) in abuse and not abuse cases. Certainty not assessed in indeterminate cases.
Certainty of Diagnosis
CAPs rated their diagnostic certainty differently depending on level of social information. The examiner was more confident than either reviewer in all diagnostic categories (Table 1). The examiner median level of certainty for all cases was 90 (IQR: 80–98) and for difficult cases was 83 (IQR: 68–92). To account for the possibility that reviewers were less certain because a complete examination was not performed, certainty was assessed for cases in which the examiner, R1, and R2 all performed a complete examination. Examiners remained more certain than R1 or R2 (Table 1).
Medical Evaluation: Neurotrauma
Whether a complete evaluation was performed differed by level of social information (examiner, R1, or R2) (Table 2). For neurotrauma (N = 239 cases) examiners were least likely to perform a compete evaluation (59.4%), whereas R1 and R2 were similar (76.2% and 74.4%, respectively) and statistically different from the examiner (P < .001 and P = .001, respectively). After adjustment, R1 was 2.2 (95% CI: 1.5–3.2) times more likely to perform a complete evaluation than the examiner. Similarly, R2 was 2.0 (95% CI: 1.1–2.9) times as likely to perform a complete evaluation. Older children (who have fewer requirements) and greater CAP experience were associated with a complete evaluation. Results were similar when cases were stratified by diagnostic category; however, small sample size limited precision for not abuse and indeterminate cases.
TABLE 2.
Adjusted Odds of Examiner, R1, and R2 Performing a Complete Neurotrauma Evaluation
| All Cases N = 239 Cases | Probable Abuse N = 195 Cases | Probable Not Abuse N = 56 Cases | Indeterminate N = 66 Cases | |||||
|---|---|---|---|---|---|---|---|---|
| Odds Ratio | 95% CI | Odds Ratio | 95% CI | Odds Ratio | 95% CI | Odds Ratio | 95% CI | |
| R1 vs examiner | 2.23 | 1.51–3.29 | 2.25 | 1.35–3.76 | 1.60 | 0.73–3.51 | 2.35 | 0.91–6.04 |
| R2 vs examiner | 2.03 | 1.41–2.92 | 2.09 | 1.30–3.34 | 1.29 | 0.47–3.52 | 4.04 | 1.43–11.39 |
| Age (referent ≤5 mo) | ||||||||
| 6–11 mo | 0.71 | 0.45–1.12 | 0.83 | 0.48–1.44 | 0.30 | 0.08–1.10 | 1.08 | 0.35–3.34 |
| 12–23 mo | 1.12 | 0.62–1.99 | 1.42 | 0.68–2.96 | 0.57 | 0.13–2.41 | 1.99 | 0.30–13.14 |
| 24+ mo | 3.45 | 1.94–6.13 | 3.63 | 1.70–7.75 | 4.18 | 1.03–17.00 | 2.21 | 0.45–10.92 |
| CAP experience (10+ y) | 1.7 | 1.24–2.42 | 2.08 | 1.36–3.19 | 0.78 | 0.34–1.78 | 1.61 | 0.81–3.18 |
| Reviewer nonminority | 1.16 | 0.68–1.98 | 1.54 | 0.81–2.90 | 0.25 | 0.06–0.97 | 0.70 | 0.05–9.84 |
| Reviewer male | 0.69 | 0.43–1.11 | 0.67 | 0.37–1.24 | 0.74 | 0.25–2.24 | 0.77 | 0.15–3.92 |
Each case has three observations.
Long Bone Injury
For long bone injury (N = 232), the examiner performed a complete evaluation (70.2%) less often than R1 (84.2%) or R2 (85.2%) (P = .001, P = .001 respectively). In the adjusted analysis, R1 (odds ratio 2.17; 95% CI: 1.38–3.42) and R2 (odds ratio 2.60; 95% CI: 1.55–4.38) were more likely to perform a complete evaluation (Table 3). Similar to neurotrauma evaluations, older children were more likely to have a complete evaluation. Minority physicians were more likely to perform a complete evaluation. Results were similar when cases were stratified by diagnostic category. There were insufficient cell sizes to model indeterminate cases.
TABLE 3.
Adjusted Odds of Examiner, R1, and R2 Performing a Complete Long Bone Fracture Evaluation
| All Cases N = 232 Cases | Probable Abuse n = 169 Cases | Probable Not Abuse n = 87 Cases | ||||
|---|---|---|---|---|---|---|
| Odds Ratio | 95% CI | Odds Ratio | 95% CI | Odds Ratio | 95% CI | |
| R1 vs examiner | 2.17 | 1.38–3.42 | 2.03 | 1.23–3.67 | 2.16 | 0.81–5.76 |
| R2 vs examiner | 2.60 | 1.55–4.38 | 2.11 | 1.12–3.97 | 3.05 | 0.98–9.44 |
| Age (6–23 vs 0–5 mo) | 6.09 | 3.00–12.37 | 9.36 | 2.81–31.24 | 3.96 | 1.22–12.74 |
| CAP experience ≥10 y | 1.47 | 0.97–2.23 | 1.15 | 0.66–2.01 | 3.48 | 1.38–8.76 |
| Reviewer nonminority | 0.27 | 0.12–0.62 | 0.24 | 0.07–0.73 | 0.58 | 0.17–1.98 |
| Reviewer male | 0.79 | 0.44–1.39 | 1.33 | 0.60–2.97 | 0.24 | 0.09–0.64 |
Each case has three observations.
Medical Diagnoses: Examiner to R1
The examiner agreed with R1 in 73.3% (95% CI: 70.1%–76.5%) of all cases (Table 4). Of determinant cases, diagnoses by R1 changed from abuse to not abuse or from not abuse to abuse between the examiner and R1 in 33 cases (11.6%), with the remainder changing to indeterminate. Of indeterminate cases, 21 (19.8%) changed to abuse and 35 (33.0%) changed to not abuse.
TABLE 4.
Percent Diagnostic Agreement and Percent Diagnostic Change in All Cases and Difficult Cases
| Examiner to R1a (Testing Intuition) | All Cases N = 726 | Difficult Cases n = 337 |
|---|---|---|
| Percent (95% CI) | Percent (95% CI) | |
| Percent agreement | 73.3 (70.1–76.5) | 56.7 (51.4–62.0) |
| Percent change in diagnosis | ||
| Abuse | 15.5 (11.9–19.2) | 34.3 (24.9–43.7) |
| Not abuse | 32.7 (26.8–38.7) | 42.8 (34.4–51.2) |
| Indeterminate | 52.8 (43.2–62.3) | 52.3 (42.7–61.9) |
| R1 to R2a (testing social information) | ||
| Percent agreement | 66.5 (63.1–70.0) | 51.3 (46.0–56.7) |
| Percent change in diagnosis | ||
| Abuse | 22.5 (18.2–26.8) | 44.4 (34.7–54.2) |
| Not abuse | 25.6 (19.7–31.4) | 34.7 (26.2–43.2) |
| Indeterminate | 69.7 (62.4–76.9) | 66.7 (58.1–75.2) |
Statistical significance is indicated by nonoverlapping CIs.
Difficult Cases
Diagnostic agreement between the examiner and R1 fell to 56.7% (95% CI: 51.4%–62.0%) in cases with examiner certainty rated <90. The diagnosis changed from abuse to not abuse (and vice versa) in 20.6% of cases. Indeterminate cases changed to abuse 19% of the time and to not abuse 33% of the time.
R1 to R2
In the R1 to R2 comparison, the influence of social information on medical diagnosis was assessed. R1 and R2 agreed in 66.5% of cases (95% CI: 63.1%–70.0%) (Table 4). In the R1 to R2 comparison, cases changed from abuse to not abuse (or vice versa) 13.9% of the time as classified by R1. Indeterminate cases changed to abuse (30.3%) and to not abuse (39.3%). Social information was more influential in difficult cases, with R1 to R2 agreement dropping to 51.3% (95% CI: 46.0%–56.7%) of cases. Abuse diagnoses changed to not abuse (or vice versa) 26.2% of the time, and indeterminate diagnoses changed to abuse 26.5% of the time and not abuse 40.2% of the time.
Discussion
Our results are consistent with the hypothesis that medical evaluation and diagnosis of child physical abuse are influenced at 2 points: an intuitive reaction from meeting the family and a knowledge of social information unlinked to meeting the family.
The influence of social intuition is shown in differences of complete evaluations. CAPs who met the family performed a less complete evaluation than both CAPs (R1 and R2) who did not meet the family, whereas R1 and R2 performed similar evaluations. This may reflect that meeting the family encourages an intuitive thinking pathway (“gut feeling”), allowing an examining CAP to skip elements of a diagnostic evaluation deemed required by expert consensus. This intuitive leaning toward a leading diagnosis may distort subsequent decisions.9 Croskerry10,11 proposed a 2 pathways model of decision-making: a rapid intuitive pathway and a more deliberative analytic pathway. Physicians use the intuitive pathway because it is efficient and frequently correct12; however, if intuition is based on characteristics of the child and family that are associated with but not causal for abuse, it may lead to overevaluation of some groups and underevaluation of other groups. This evaluation pattern is reported in the literature with overevaluation of African American children in the emergency department for fractures and underevaluation of white children for abusive head trauma.1,2,4 CAPs who are not informed by meeting the family may be forced to use the analytic pathway, as reflected in their adherence to the gold standard evaluation. Evaluations of suspected child physical abuse might be improved by interventions that switch CAPs from intuitive to analytic thinking. Simple interventions (such as checklists that require physicians to opt out of elements of a gold standard evaluation) encourage analytic thinking while preserving physician judgement in individual cases.13 A pilot study of a checklist revealed a decrease in disparities of evaluations for abusive head trauma, lending support to this idea.14
Our second hypothesis was that social information might influence medical diagnosis and that this influence would be more apparent in less certain cases. Our results reveal that among all cases, the examiner and R1 have good diagnostic agreement at 73%, similar to diagnostic agreement in expert review of child sex abuse.15 There is significantly less agreement between R1 and R2. The fact that R2 rated social risk lower than R1 supports the idea that eliminating social risk indicators affected R2 perceptions. Agreement decreased in difficult cases for both comparisons (examiner to R1 and R1 to R2), suggesting that social information is more influential in formulating a diagnosis under conditions of medical uncertainty.16
CAP certainty of diagnosis decreased from the examiner to R1 and from R1 to R2, suggesting that social intuition from meeting the family and social information may act through increased confidence, potentially decreasing deliberative thinking. Of interest, confidence and diagnostic accuracy correlate only when all information is aligned but not when information is discrepant.17
There is no diagnostic gold standard in child physical abuse; therefore, our results cannot determine if inclusion of social intuition or social information in medical decision-making strengthens or weakens accuracy in cases of suspected child physical abuse. However, reliance on a child’s social risks in medical decision-making may open the diagnostic process to bias.18 Laskey et al’s3 study revealed that physicians are more willing to consider a diagnosis of abuse among poor children, suggesting that some bias exists. It is concerning that knowledge of social information reversed 1 in 5 diagnoses when all other information was held constant. Although social information may be critical to recognizing and responding to child abuse risk, our findings suggest that CAPs must be mindful of how this information is used to shape a diagnosis of child abuse.
Many child abuse programs employ a peer review process to review each case. Although the peer review process has not been studied in CAP, multidisciplinary review boards in oncology do affect diagnostic decision-making.19 Our results suggest that peer review of child abuse cases, which includes experts without personal perceptions of the family to weigh in on cases, should be a focus for future CAP research. A combination of intuitive and deliberative thinking may minimize bias and improve accuracy in the diagnostic process.20
This study must be viewed in the light of its limitations. The experimental conditions created for the study do not replicate actual practice. The CAP diagnosis of abuse is the first step in the social response to child abuse and not the last step. Results of child welfare investigations that occurred after the CAP evaluation were not included in our cases because we were interested in the CAP decision-making process. Additionally, although we can say that the use of social intuition and information change diagnosis, we cannot say which diagnosis was correct when there was diagnostic disagreement because no diagnostic gold standard exists. Finally, a small sample of CAPs participated, so results may not be broadly generalizable.
Conclusions
Reliance on social intuition and social information for the evaluation and diagnosis of children with physical abuse may lead CAPs astray when all information is not aligned. Methods to encourage analytic thinking in conjunction with intuitive thinking may provide insurance that all children are evaluated and diagnosed for abuse in an equivalent manner. Researchers for future studies should evaluate tools including decision aides, checklists, and peer review that promote analytic thinking in the evaluation and diagnosis of suspected physical abuse.
Glossary
- CAP
child abuse pediatrician
- CI
confidence interval
- IQR
interquartile range
- R1
first reviewer
- R2
second reviewer
Footnotes
Dr Keenan conceptualized and designed the study and drafted the initial manuscript; Dr Cook and Mr Bardsley conducted the analyses and reviewed and revised the manuscript; Dr Olson contributed to the design of the study and the analysis and reviewed and revised the manuscript; Dr Campbell contributed to the design and analysis of the study and reviewed and revised the manuscript; and all authors approved the final manuscript as submitted.
FINANCIAL DISCLOSURE: Dr Campbell’s institution receives financial compensation for expert witness testimony provided in cases of suspected child abuse for which she is subpoenaed to testify; the other authors have indicated they have no financial relationships relevant to this article to disclose.
FUNDING: Supported by the Eunice Kennedy Shriver Institute of Child Health and Human Development of the National Institutes of Health grant R01 HD061373 (principal investigator Dr Keenan). Funded by the National Institutes of Health (NIH).
POTENTIAL CONFLICT OF INTEREST: The authors have indicated they have no potential conflicts of interest to disclose.
References
- 1.Lane WG, Rubin DM, Monteith R, Christian CW. Racial differences in the evaluation of pediatric fractures for physical abuse. JAMA. 2002;288(13):1603–1609 [DOI] [PubMed] [Google Scholar]
- 2.Jenny C, Hymel KP, Ritzen A, Reinert SE, Hay TC. Analysis of missed cases of abusive head trauma. JAMA. 1999;281(7):621–626 [DOI] [PubMed] [Google Scholar]
- 3.Laskey AL, Stump TE, Perkins SM, Zimet GD, Sherman SJ, Downs SM. Influence of race and socioeconomic status on the diagnosis of child abuse: a randomized study. J Pediatr. 2012;160(6):1003–1008.e1 [DOI] [PubMed] [Google Scholar]
- 4.Wood JN, Hall M, Schilling S, Keren R, Mitra N, Rubin DM. Disparities in the evaluation and diagnosis of abuse among infants with traumatic brain injury. Pediatrics. 2010;126(3):408–414 [DOI] [PubMed] [Google Scholar]
- 5.Ely JW, Graber ML, Croskerry P. Checklists to reduce diagnostic errors. Acad Med. 2011;86(3):307–313 [DOI] [PubMed] [Google Scholar]
- 6.Redelmeier DA. Improving patient care. The cognitive psychology of missed diagnoses. Ann Intern Med. 2005;142(2):115–120 [DOI] [PubMed] [Google Scholar]
- 7.Campbell KA, Olson LM, Keenan HT. Critical elements in the medical evaluation of suspected child physical abuse. Pediatrics. 2015;136(1):35–43 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Association of American Medical Colleges The status of the new AAMC definition of “underrepresented in medicine” following the Supreme Court’s decision in Grutter. 2004. Available at: https://www.aamc.org/download/54278/data/urm.pdf. Accessed August 21, 2015
- 9.Kostopoulou O, Russo JE, Keenan G, Delaney BC, Douiri A. Information distortion in physicians’ diagnostic judgments. Med Decis Making. 2012;32(6):831–839 [DOI] [PubMed] [Google Scholar]
- 10.Croskerry P. From mindless to mindful practice–cognitive bias and clinical decision making. N Engl J Med. 2013;368(26):2445–2448 [DOI] [PubMed] [Google Scholar]
- 11.Croskerry P. Perspectives on diagnostic failure and patient safety. Healthc Q. 2012;15(Spec No):50–56 [DOI] [PubMed] [Google Scholar]
- 12.Van den Bruel A, Thompson M, Buntinx F, Mant D. Clinicians’ gut feeling about serious infections in children: observational study. BMJ. 2012;345:e6144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Croskerry P, Singhal G, Mamede S. Cognitive debiasing 2: impediments to and strategies for change. BMJ Qual Saf. 2013;22(suppl 2):ii65–ii72 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Rangel EL, Cook BS, Bennett BL, Shebesta K, Ying J, Falcone RA. Eliminating disparity in evaluation for abuse in infants with head injury: use of a screening guideline. J Pediatr Surg. 2009;44(6):1229–1234; discussion 1234–1235 [DOI] [PubMed] [Google Scholar]
- 15.Starling SP, Frasier LD, Jarvis K, McDonald A. Inter-rater reliability in child sexual abuse diagnosis among expert reviewers. Child Abuse Negl. 2013;37(7):456–464 [DOI] [PubMed] [Google Scholar]
- 16.Chaiyachati BH, Asnes AG, Moles RL, Schaeffer P, Leventhal JM. Gray cases of child abuse: investigating factors associated with uncertainty. Child Abuse Negl. 2016;51:87–92 [DOI] [PubMed] [Google Scholar]
- 17.Cavalcanti RB, Sibbald M. Am I right when I am sure? Data consistency influences the relationship between diagnostic accuracy and certainty. Acad Med. 2014;89(1):107–113 [DOI] [PubMed] [Google Scholar]
- 18.Dovidio JF, Fiske ST. Under the radar: how unexamined biases in decision-making processes in clinical interactions can contribute to health care disparities. Am J Public Health. 2012;102(5):945–952 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Thenappan A, Halaweish I, Mody RJ, et al. . Review at a multidisciplinary tumor board impacts critical management decisions of pediatric patients with cancer. Pediatr Blood Cancer. 2017;64(2):254–258 [DOI] [PubMed] [Google Scholar]
- 20.Eva KW, Hatala RM, Leblanc VR, Brooks LR. Teaching from the clinical reasoning literature: combined reasoning strategies help novice diagnosticians overcome misleading information. Med Educ. 2007;41(12):1152–1158 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.