Abstract
Objective
Research suggests that being unable to generate solutions to problems in times of distress may contribute to suicidal thoughts and behavior, and that depression is associated with problem solving deficits. This study examined active and passive problem solving as moderators of the association between depressive symptoms and future suicidal ideation (SI) among suicide attempters and non-attempters.
Method
Young adults (n = 324, 73% female, Mage = 19, SD = 2.22) with (n = 78) and without (n = 246) a suicide attempt history completed a problem-solving task, self-report measures of hopelessness, depression, and SI at baseline, and also completed a self-report measure of SI at 6-month follow-up.
Results
Passive problem solving was higher among suicide attempters but did not moderate the association between depressive symptoms and future SI. Among attempters, active problem solving buffered against depressive symptoms in predicting future SI.
Conclusions
Suicide prevention should foster active problem solving, especially among suicide attempters.
Keywords: active problem solving, passive problem solving, depression, suicidal ideation, suicide attempts
Suicide is the 2nd leading cause of death among individuals 15–24 and 25–34 years of age in the United States, with over 11,000 suicides combined in these age groups in the year 2012 (CDC, 2014). Among the best-studied predictors of suicide are a history of previous suicide attempts and history of depression (see Miranda & Shaffer, 2013). Previous research suggests that individuals engage in suicidal behavior when they are unable to think of alternatives to cope with their distress – i.e., when they are unable to generate solutions to their problems (Williams, Crane, Barnhofer, & Duggan, 2005a). Understanding how problem solving interacts with depressive symptoms to affect risk for suicidal thoughts and behavior is one important step in improving interventions to reduce suicide risk among vulnerable individuals. The present study sought to better understand how different forms of problem solving impact the relation between depressive symptoms and future suicidal ideation among young adults as an important step in identifying points of intervention in problem-solving-focused treatments for suicidal behavior.
Social Problem Solving, Depression, and Suicidal Behavior
Previous research suggests that social problem solving deficits are associated with depression, suicidal ideation, and suicide attempts (Jollant, Lawrence, Olie, Guillaume, Courtet, 2011; Priester & Clum, 1993; Speckens & Hawton, 2005). Earlier research on problem solving and depression suggested not only that depressed individuals solve problems more poorly than non-depressed individuals (e.g., Priester & Clum, 1993) but that problem solving may have an the impact on the effect of life stress on depressive symptoms (Goodman, Gravitt, & Kaslow, 1995; Nezu & Ronan, 1988). For instance, in a study investigating the associations among problem solving, depression, hopelessness, and suicidal behavior, the amount of relevant and irrelevant solutions to problems people generated predicted levels of depressive symptomatology and hopelessness prospectively (Priester & Clum, 1993). At the same time, effective problem solving has been found to buffer against the prospective impact of life stress on depressive symptoms among adults (Nezu & Ronan, 1988) and children (Goodman et al., 1995). Later research has examined social problem solving deficits in relation to both depression and suicidal behavior (Williams, Barnhofer, Crane & Beck, 2005b; Grover et al., 2009). For instance, a study that investigated the effect of a negative mood induction on the problem solving ability of formerly depressed individuals with or without a history of suicidal ideation found that post-mood induction, only formerly depressed participants with a history of suicidal ideation generated less effective solutions to problems than before the mood induction (Williams et al., 2005b). Participants who were never depressed or who were depressed but did not have a history of suicidal ideation did not experience a significant change in problem solving (Williams et al., 2005b). Furthermore, in a study investigating the interaction of stress and problem solving skills in predicting suicidal behaviors in adolescents, individuals with high levels of life event stress and lower problem solving skills were at a greater risk of attempting suicide, but not after adjusting for depression and hopelessness (Grover et al., 2009). These findings suggest that social problem solving and depression may interact to influence suicidal thinking and behavior.
Research has also suggested that problem solving may protect against suicidal thinking and behavior (Fried, Williams, Cabral & Hacker, 2013; Khurana & Romer, 2012; Schotte, Cools & Payvar, 1990). For instance, a study examining risk and protective factors for suicide attempts among 9th and 11th graders found that addressing problems systematically was associated with lower risk of suicide attempts among 11th graders (Fried et al., 2013). Another study found that improvement in interpersonal problem solving skills on the Means-Ends Problem Solving (MEPS) task (Platt et al., 1975) was associated with a reduction of self-reported symptoms of depression and suicidal intent among inpatient suicide ideators (Schotte et al., 1990). Furthermore, in a study investigating the effects of different coping strategies on suicidal ideation over 1 year follow up, problem solving predicted decreases in suicidal ideation through a reduction in depressive symptoms (Khurana & Romer, 2012). These studies suggest that knowing how to effectively solve problems may decrease risk for future suicidal ideation and attempts by impacting depressive symptoms.
Active versus Passive Problem Solving
In order to decipher how problem-solving deficits may lead to suicidal behavior, some researchers have more closely examined the solutions that individuals generate and the style of problem solving that they use (Linda, Marroquín, & Miranda, 2012; Pollock & Williams, 2004). Two styles of social problem solving have been conceptualized as active problem solving, which occurs when an individual takes discrete steps to solve his or her problem, and passive problem solving, which occurs when an individual relies on others to solve an interpersonal problem, or believes that the problem will be solved by fate, luck, or chance (Linehan, Camper, Chiles, & Strosahl, & Shearin, 1987). Previous research on passive versus active problem solving and suicidal behavior has been mixed (Linda et al., 2012; Pollock & Williams, 2004). For instance, in a study examining social problem solving skills among suicide attempters, a non-suicidal psychiatric control group, and a non-psychiatric control group, patients with a history of deliberate self-harm (i.e., drug-overdose, self-cutting, and attempted drowning) generated fewer active solutions to problems than did non-psychiatric controls, but no fewer than psychiatric controls (Pollock & Williams, 2004). In recent study examining the relation between type of social problem solving, life event stress, and suicidal ideation among college students, individuals with a history of suicide attempts generated more passive solutions to problems, compared to college students without a history of suicide attempts, but they did not differ in the number of active solutions they generated (Linda et al., 2012). However, among suicide attempters, generating passive means weakened the relation between life stress and suicidal ideation, suggesting that in the context of life stress, even passive problem solving may be adaptive for individuals with a history of suicide attempts (Linda et al., 2012). Thus, the role of active and passive problem solving in predicting suicidal ideation and behavior remains unclear.
The Present Study
The present study sought to examine whether active and passive problem solving would moderate the relation between depressive symptoms and future suicidal ideation. We hypothesized that active problem solving would buffer against the prospective relation between depressive symptoms and suicidal ideation, and that passive problem solving would exacerbate this relationship. Given previous research suggesting that passive problem solving may serve a buffering effect among individuals with a suicide attempt history, we also examined these questions separately for individuals with and without a history of suicide attempts.
Methods
Participants
Three hundred twenty-four college undergraduates (238 females and 86 males), ages 18-34 (M= 19.00, SD= 2.22) were recruited from a public college in New York City (via Introductory Psychology courses, electronic mail sent via the college registrar's office, or flyers; n = 300) and from other colleges in the surrounding metropolitan area (via Craigslist advertisements; n = 24). The participants from this sample were 33.3% Asian, 29.3% White, 17.6% Hispanic, 11.1% Black, 7.1% Biracial/Multiracial, and 1.5% of other races/ethnicities. These individuals originally took part in a larger study examining cognitive predictors of suicidal behavior (N = 2054). This subsample consisted of 78 individuals (24%) with a suicide attempt history (59 females, 19 males) and 246 individuals with no suicide attempt history (179 females, 67 males).
Measures
Depressive Symptoms
The Beck Depression Inventory, Second Edition (BDI-II; Beck, Steer & Brown, 1996) is a 21 item self-report questionnaire measuring depressive symptomatology (i.e. sadness, anhedonia, difficulty concentrating, appetite/ sleep disturbance, and psychomotor agitation) that participants have experienced during the previous two weeks. Scores for each item on the BDI-II can range from 0 to 3, and total scores on this measure can range from 0 to 63. A score of 20 or above is indicative of clinically significant depression. In the current sample, scores ranged from 0–56 (M = 16.15, SD = 10.83). Cronbach's alpha was .92 in the current sample. The BDI-II has shown high internal consistency, with a coefficient alpha of .89 for the total scale and alpha coefficients of .72 and .87 for the Somatic and Cognitive-Affective factors, respectively (Whisman, Perez, & Ramel, 2000).
Hopelessness
The Beck Hopelessness Scale (BHS; Beck & Steer, 1988) is a 20-item self-report measure designed to assess an individual's hopeless expectations about the future. Items included address general feelings about the future (e.g., “I look forward to the future with hope and enthusiasm”), loss of motivation (e.g., “I might as well give up because I can't make things better for myself”), and future expectations (e.g., “My future seems dark to me”). Responses are scored on a binary scale (true/false), and scores can range from 0 to 20, with some items reverse-scored. Scores ranged from 0–19 (M = 5.34, SD = 4.49), and the internal consistency reliability of the BHS was .88 in the present sample. The BHS has shown good internal consistency, test-retest reliability, and both concurrent and predictive validity (see Hilsenroth & Segal, 2004).
Social Problem Solving
The Means-Ends Problem-Solving (MEPS; Platt et al., 1975) task, administered via computer, was used to measure social problem solving. In the task, participants are presented with the beginning of a story that states an interpersonal problem, and the end of a story that states the resolution. Participants are asked to imagine themselves experiencing the situation and to explain in one paragraph what they would do to solve the problem in order to get to the stated end. The scenarios included: being new to a neighborhood and wanting to make friends, wanting to resolve an argument with a friend who is ignoring you, wanting to resolve an argument with a significant other, and trying to take a leadership role at a meeting. The scenarios were coded for active and passive means by three coders who were blind to participants' status as an attempter or non-attempter. The coding scheme used was adapted from Lyubomirsky and Nolen-Hoeksema (1995; see also Linda et al., 2012). Active means were conceptualized as the steps the protagonist takes to solve the problem, while passive means were conceptualized as the steps that another character in the story takes to solve the problem, or solutions that occur by fate, luck, or chance. One coder (VQ) scored all of the scenarios for active and passive means and two other coders (JJ and EF) scored different halves of the scenarios for active and passive means, in order to measure interrater reliability. Coders met regularly to discuss and resolve discrepancies in order to yield final scores for analysis. The interrater reliabilities were .79 and .80 for active means and .75 and .80 for passive means, for each pair of coders, respectively. The total number of active and passive means generated for each of the four scenarios was summed. Scores for active means ranged from 0 to 13 (M = 5.38, SD = 2.21), and scores for passive means ranged from 0 to 7 (M = 1.38, SD = 1.22). The MEPS task has been reported to have adequate construct, content, discriminant, concurrent, and predictive validity, satisfactory levels of test-retest reliability, and high levels of internal consistency (Platt et al., 1975).
Suicide Attempt History
The Suicidal Behavior Screening (SBS) is a questionnaire containing 6 questions derived from the Diagnostic Interview Schedule for Children (Shaffer et al., 2000). In the present study, this measure was used to screen for lifetime history of suicide attempts. Participants responded “yes” or “no” to the question: “Have you ever, in your whole life, tried to kill yourself or made a suicide attempt?” This response was used to divide the sample into individuals with and without a suicide attempt history. A similar procedure has been used in prior research with young adults (Linda et al., 2012).
Suicidal Ideation
The Beck Scale for Suicide Ideation (BSS; Beck & Steer, 1991) is a 21-item self-report questionnaire that measures active (e.g., “I have a moderate to strong desire to kill myself”) and passive suicidal thoughts (e.g., “I would not take the steps necessary to avoid death if I found myself in a life-threatening situation”) that an individual has experienced within the past week. Items on the BSS are measured on a 0 to 2 point Likert Scale, with higher scores representing more active thoughts about attempting suicide. Scores on the BSS can range from 0 to 38. Scores ranged from 0–29 (M = 2.64, SD = 5.13) at baseline, and from 0–25 (M= 1.08, SD = 3.06) at 6-month follow-up. Cronbach's alpha was .97 at baseline and .97 at follow-up. The BSS has shown to be a valid and reliable measure of suicidal ideation in inpatient and outpatient samples. It demonstrated strong concurrent validity (greater than .90) with clinical ratings of suicidal ideation and high internal consistency, with Cronbach coefficient alpha above .90 (Beck, Steer, &Ranieri, 1988).
Procedure
Participants were recruited for a study examining cognitive predictors of suicidal ideation and behavior. In the first study session, participants provided informed consent and, in groups of 4–8, completed a packet of self-report questionnaires – arranged in a random order – that included the BDI, BHS, SBS, and the BSS. After taking part in this study, participants were debriefed and asked for their consent to be contacted for future studies. Participants who gave their consent were randomly selected (via a random number generator) so that about two-thirds of the sample for the next study session would consist of individuals without a history of suicidal ideation or a suicide attempt and one-third of the sample would consist of individuals with a history of either suicidal ideation in the previous 6 months or a lifetime suicide attempt history. They were invited to participate in a longitudinal study that involved a 2-hour study session, followed by 3 hour-long assessments, each separated by 6 months. Of those who were invited, 354 participated in the 2-hour session approximately one month after the initial screening. They completed several tasks, including the MEPS task, and other self-report questionnaires that were not included in the present study. Participants had the option to be compensated $50, to be granted 2 research credits for their Introduction to Psychology course, or to receive a combination of $25 and one credit. They also scheduled a tentative appointment for their 6-month follow-up session. The final sample consisted of 324 participants (92% retention) who returned approximately six months later for a follow-up assessment. They completed the BSS and other self-report measures for the second time and were compensated $30 for their participation. After each study session, research assistants with at least a Bachelor's degree reviewed participants' responses on the BDI, BSS, and SBS as part of a risk assessment. Individuals who reported current suicidal ideation or a suicide attempt that occurred within the previous two weeks were interviewed by a licensed clinical social worker or a licensed clinical psychologist. If deemed necessary, participants were escorted to the counseling center on campus. All participants were debriefed and received a list of local treatment referrals at the end of each study session. The study received full-board approval by an Institutional Review Board.
Results
Statistical Analysis
Chi-square analyses were conducted to test for gender and ethnic differences by suicide attempt history, and independent samples t-tests were conducted to examine differences in depressive symptoms, hopelessness, baseline and future suicidal ideation, active means, and passive means by suicide attempt history. Correlational analyses were used to examine the relations among study variables. Baseline active and passive problem solving, depressive symptoms, suicide attempt history, the two-way interactions between problem solving and depressive symptoms (Active × Depression, Passive × Depression), and the three-way interactions among problem solving, depressive symptoms, and suicide attempt history (Active × Depression × Attempt History, Passive × Depression × Attempt History) were entered into a linear regression analysis to predict suicidal ideation at 6-month follow up, adjusting for baseline suicidal ideation and hopelessness. Continuous variables that were included in interactions were centered around their means (Jacard, 2001). Simple effects for significant interactions between problem solving and depression were tested separately for individuals with and without a suicide attempt history using the PROCESS computational tool for interactions (Hayes, 2013).
Group Differences
There were no significant group differences in gender, χ2 (1, N = 324) = 0.25, p = .62, or ethnicity, χ2 (5, N = 324) = 2.86, p = .72. Suicide attempters had significantly higher depressive symptoms, t(322) = −4.42, p < .01, hopelessness, t(113.75) = −3.63, p < .01, baseline suicidal ideation, t(102.68) = −3.20, p < .01, future suicidal ideation, t(89.95) = −2.89, p < .01, and passive means, t(322) = −2.43, p < .05, than did non-attempters. Attempters and non-attempters did not differ on active means, t(322) = 0.37, p = .71, or age, t(105.01) = −1.72, p = .09. See Table 1 for means and standard deviations.1
Table 1.
Means for Study Measures by Suicide Attempt History
| No Past Suicide Attempt
|
Past Suicide Attempt
|
||||
|---|---|---|---|---|---|
| M | SD | M | SD | Effect size d | |
| Active (1) | 5.40 | 2.14 | 5.29 | 2.42 | 0.05 |
| Passive (1) | 1.28* | 1.20 | 1.67* | 1.26 | 0.32 |
| Depression (1) | 14.70** | 10.24 | 20.74** | 11.42 | 0.57 |
| Hopelessness (1) | 4.80** | 4.19 | 7.06** | 4.99 | 0.49 |
| Baseline SI (1) | 2.05** | 4.52 | 4.54** | 6.38 | 0.45 |
| Future SI (2) | 0.73** | 2.32 | 2.28** | 4.56 | 0.43 |
Note.
p < .05,
p < .01
Participants with no past suicide attempt, n = 246; Participants with past suicide attempt, n = 78.
(1) Assessed at baseline
(2) Assessed at follow up
Associations among Study Variables by Suicide Attempt History
Among individuals without a suicide attempt history, passive problem solving was significantly and negatively associated with age, r(244) = −.13, p < .05, while active problem solving was not significantly associated with age. Neither active nor passive problem solving was significantly associated with depressive symptoms, hopelessness, baseline suicidal ideation, or future suicidal ideation. Depressive symptoms were significantly and positively associated with hopelessness, baseline suicidal ideation, and future suicidal ideation, and hopelessness was also significantly and positively associated with baseline and future suicidal ideation. Among individuals with a suicide attempt history, active and passive problem solving were not significantly associated with any other study variables. Depression was significantly and positively associated with hopelessness, baseline suicidal ideation, and future suicidal ideation. Hopelessness was significantly and positively associated with baseline and future suicidal ideation. See Table 2 for correlations.
Table 2.
Correlations among Study Variables by Suicide Attempt History.
| 1 | 2 | 3 | 4 | 5 | 6 | |
|---|---|---|---|---|---|---|
| 1. Active (1) | - | −0.27* | −0.06 | −0.04 | 0.02 | −0.13 |
| 2. Passive (1) | −0.23** | - | 0.03 | −0.04 | −0.04 | 0.07 |
| 3. Depression (1) | −0.09 | 0.03 | - | 0.71** | 0.58** | 0.48** |
| 4. Hopelessness (1) | −0.02 | 0.06 | 0.66** | - | 0.55** | 0.36** |
| 5. Baseline SI (1) | 0.02 | 0.00 | 0.53** | 0.50** | - | 0.53** |
| 6. Future SI (2) | 0.06 | −0.07 | 0.21** | 0.26** | 0.46** | - |
p < .01;
p <.05
Correlations for suicide attempters (n = 78) are reported above the diagonal and for non-attempters (n = 246) are reported below the diagonal. SI = Suicidal ideation.
(1) Assessed at baseline
(2) Assessed at 6-month follow up
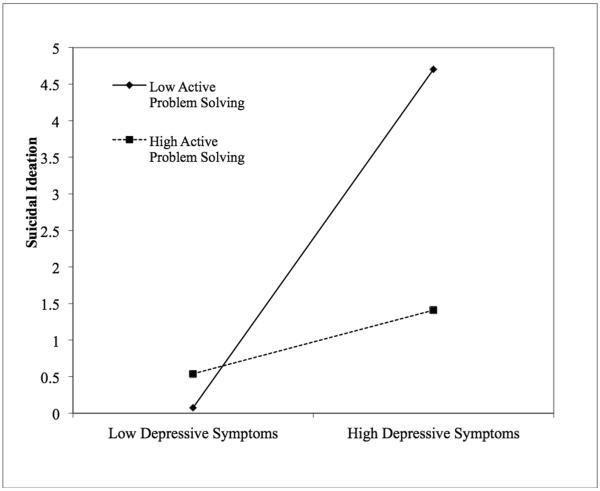
Moderating role of Problem Solving
Results from a multiple linear regression analysis examining predictors of future suicidal ideation indicated that only the three-way interaction among active problem solving, depressive symptoms, and suicide attempt history predicted suicidal ideation at 6-month follow up, b = −0.06, s.e. = 0.02, partial r = −.19, p< .01, adjusting for baseline hopelessness and baseline suicidal ideation (with baseline ideation also a predictor of future ideation, b = 0.25, s.e. = 0.04, partial r = .37, p < .01; all other partial rs in the model ranged from −.09 to 0.07). Tests of simple effects revealed that among individuals without a suicide attempt history, there was no statistically significant relation between depressive symptoms and future suicidal ideation at low (1 SD below the mean), b = −0.02, p = .27, average, b = −0.02, p = .28, or high (1 SD above the mean), b = −0.02, p = .49, levels of active problem solving, after adjusting for baseline suicidal ideation, hopelessness, and passive problem solving. Among individuals with a suicide attempt history, there was a statistically significant relation between depressive symptoms and future suicidal ideation at low (1 SD below the mean), b = 0.20, p = .01, and average, b = 0.12, p < .05, levels of active problem solving but not at high (1 SD above the mean), b = 0.04, p = .61, levels of active problem solving, adjusting for baseline ideation, hopelessness, and passive problem solving (See Figure 1).
Figure 1.
Interaction between depressive symptoms and active problem solving among individuals with a suicide attempt history.
Discussion
This study sought to examine whether active and passive problem solving would differentially influence the prospective relation between baseline depressive symptoms and future suicidal ideation (adjusting for baseline suicidal ideation) among young adults with and without a history of suicide attempts, beyond the influence of hopelessness. We hypothesized that passive problem solving would increase, whereas active problem solving would decrease, the strength of the relation between depressive symptoms and future suicidal ideation. Our hypotheses were partially supported only among individuals with a suicide attempt history. Whereas active problem solving buffered against the relation between depressive symptoms and future suicidal ideation among suicide attempters, passive problem solving did not moderate the relation between depressive symptoms and future suicidal ideation.
Among non-attempters, active problem solving did not influence the relation between depression and future suicidal ideation. This is surprising, because prior research indicates that more active forms of social problem solving decrease risk for suicidal thinking and behavior in clinical and non-clinical samples (Fried et al., 2013; Khurana & Romer, 2012). For instance, in a study examining risk and protective factors for suicide attempts in 9th and 11th grade students, problem solving emerged as a protective factor (Fried et al., 2013). Similarly, in a study examining the relation between coping strategies and suicidal ideation, the use of problem solving coping predicted reduction in suicidal ideation at 1-year follow-up (Khurana & Romer, 2012). Given previous research suggesting that social problem solving deficits interact with depression to increase risk for suicidal behavior (e.g., Grover et al., 2009), it was not surprising that active problem solving did buffer against the relation between depressive symptoms and future suicidal ideation among individuals with a suicide attempt history. Given that both depression and a suicide attempt history increase risk for future suicidal thinking and behavior (Fried et al., 2013; O'Connor et al., 2013), these findings may indicate that the ability to generate active solutions to problems may be more beneficial for those individuals who are most vulnerable – i.e., those who have a history of suicide attempts and report high levels of depressive symptoms. Fostering active problem solving may protect against not only future suicidal ideation but also future suicide attempts among these individuals.
The present study also found that individuals with a suicide attempt history had higher levels of passive problem solving than individuals without a suicide attempt history. This finding is consistent with previous research suggesting that individuals with a history of suicide attempts solve problems more passively, compared to individuals without a suicide attempt history (Linda et al., 2012; Pollock & Williams, 2004). Surprisingly, however, passive problem solving was not associated with increases in suicidal ideation over time, nor did it moderate the relation between depressive symptoms and suicidal ideation, even among individuals with a suicide attempt history. This is contrary to what was expected based on prior research, which has typically suggested that deficits in social problem solving are associated with suicidal thinking and behavior (Jollant et al., 2011; Pollock & Williams, 2004; Williams et al., 2005b). However, studies that have examined passive problem solving tend to be retrospective (e.g., Linda et el., 2012; Pollock & Williams, 2004). Few studies of which we are aware have examined the effects of problem solving style over time, or whether passive problem solving actually predicts suicidal ideation over time. Taking this previous research into consideration, the findings of the present study may suggest that passive problem solving is more predictive of actual suicide attempts, than suicidal ideation, per se. However, since passive problem solving did not predict increases in suicidal ideation, it is also possible that in certain contexts, passive problem solving is not maladaptive. For instance, in a study examining the interaction between life event stress and style of social problem solving in college students with and without a suicide attempt history, passive problem solving buffered against the relation between life event stress and suicidal ideation among individuals with a suicide attempt history (Linda et al., 2012). Therefore, the adaptive or maladaptive nature of passive problem solving may depend on the experience of life event stress.
Strengths and Limitations
Several limitations must be taken into consideration when interpreting these data. First, since the sample consisted mostly of female college undergraduates, the findings may generalize primarily to women between the ages of 18-34 who are college students rather than to the general population as a whole. Replication of these findings with a more proportionate number of male and female participants is therefore necessary. Another limitation is the use of self-report measures to assess suicidal ideation and history of suicidal behavior. History of suicide attempts was not verified via clinical interview. Finally, it is important to note that while the MEPS procedure has been widely used as a measure of problem solving ability, House and Scott (1996) point out several criticisms of the test. For instance, since MEPS scenarios are interpersonal in nature, they require an interaction or a behavioral response from the protagonist. Real-life problems, however, are often intrapersonal and may require a different set of problem-solving skills or emotion-focused responses (House & Scott, 1996). In addition, the third-person format, story-like narrative, and predetermined outcome may also elicit a different kind of response from the individual than if the story were presented in the second-person format and allowed participants to define the outcome of the problem for themselves (House & Scott, 1996).
Despite these limitations, the current study has important strengths to highlight. The study was prospective rather than cross-sectional, and the sample was ethnically diverse and included US-born (individuals born in the US) and non-US born individuals (individuals born outside of the US). This is particularly important given the scarcity of longitudinal research with diverse samples that also examines different types of problem solving. This study was also the first of which we are aware that examines the interaction between depressive symptoms and style of social problem solving (active and passive) in predicting future suicidal ideation. In addition, this study emphasizes the importance of an active problem solving style in buffering against future suicidal ideation in depressed individuals with a lifetime history of suicide attempts.
Conclusion
This study extends our knowledge of the adaptive nature of active problem solving by demonstrating that a high level of active problem solving buffers against the prospective relation between depressive symptoms and suicidal ideation. The present study also demonstrated that passive problem solving did not increase risk for future suicidal ideation in suicide attempters or non-attempters, suggesting that passive problem solving may be more predictive of suicide attempts, or that the maladaptive or adaptive effects of passive problem solving are dependent on situational factors (e.g., life event stress). Importantly, this study has valuable clinical implications. Intervention and prevention programs for suicidal behavior may utilize these findings to tailor therapies to individuals at higher risk for suicidal thinking and behavior (i.e., depressed individuals who have a history of suicide attempts). Groups of individuals who are more vulnerable to suicidal thinking or behaviors may benefit more from problem solving therapies in which individuals are taught how to generate active, constructive solutions to their interpersonal problems.
Acknowledgments
This research was funded by NIH Grant 5SC1 MH 091873 (Miranda) and by MBRS-RISE GRANT GM060665. Thanks to Alyssa Wheeler, Valerie Khait, Soumia Cheref, Kaerensa Craft, Nargus Harounzadeh, Matthew Kaplowitz, Amy Kephart, Giulia Landi, Robert Lane, Lisa Lerner, Wendy Linda, Russell Marks, Lillian Polanco-Roman, Jessica Silver, Lauren Uss, Jorge Valderrama, and Dalia Gefen for their assistance with data collection.
Footnotes
College students recruited from the community were significantly older (M = 20.4, SD = 3.5, vs. M = 18.9, SD = 2.1), t(24.3) = 2.14, p < .05, and had higher hopelessness scores (M = 7.3, SD = 5.1, vs. M = 5.2, SD = 4.4), t(320) = 2.22, p < .05, than did students recruited from the college where the study took place, but they showed no statistically significant differences on other measures, including suicide attempt history, χ2 (1, N = 324) = 0.37, p = .54.
Disclosures The authors have no conflicts of interest to disclose.
References
- Beck AT, Steer RA. Manual for the beck hopelessness scale. The Psychological Corporation; San Antonio, TX: 1988. [Google Scholar]
- Beck AT, Steer RA. Manual for the beck scale for suicide ideation. Psychological Corporation; San Antonio, TX: 1991. [Google Scholar]
- Beck AT, Steer RA, Brown GK. Manual for the beck depression inventory-II. Psychological Corporation; San Antonio, TX: 1996. [Google Scholar]
- Beck AT, Steer RA, Ranieri WF. Scale for suicide ideation: Psychometric properties of a self-report version. Journal of Clinical Psychology. 1988;44:499–505. doi: 10.1002/1097-4679(198807)44:4<499::aid-jclp2270440404>3.0.co;2-6. doi:10.1002/1097-4679(198807)44:4<499::AID-JCLP2270440404>3.0.CO;2-6. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention (CDC) Web-based Injury Statistics Query and Reporting System (WISQARS) 2014 [Online interactive database]. Retrieved on November 5, 2014, from http://www.cdc.gov/injury/wisqars/index.html.
- Fried LE, Williams S, Cabral H, Hacker K. Differences in risk factors for suicide attempts among 9th and 11th grade youth: A longitudinal perspective. The Journal of School Nursing. 2013;29:113–122. doi: 10.1177/1059840512461010. [DOI] [PubMed] [Google Scholar]
- Goodman SH, Gravitt GW, Kaslow NJ. Social problem solving: A moderator of the relation between life stress and depression symptoms in children. Journal of Abnormal Child Psychology. 1995;23:473–485. doi: 10.1007/BF01447209. [DOI] [PubMed] [Google Scholar]
- Grover KE, Green KL, Pettit JW, Monteith LL, Garza MJ, Venta A. Problem solving moderates the effects of life event stress and chronic stress on suicidal behaviors in adolescence. Journal of Clinical Psychology. 2009;65:1281–1290. doi: 10.1002/jclp.20632. doi:10.1002/jclp.20632. [DOI] [PubMed] [Google Scholar]
- Hayes AF. Introduction to mediation, moderation, and conditional process analysis: A regression-based approach. Guilford Press; New York, NY, US: 2013. [Google Scholar]
- Hilsenroth M, Segal D, editors. Personality assessment. Volume 2 in M. Hersen (Editor-in-Chief) Comprehensive handbook of psychological assessment. John Wiley & Sons; Hoboken, NJ: 2004. [Google Scholar]
- House R, Scott J. Problems in measuring problem-solving: The suitability of the means-ends problem solving (MEPS) procedure. International Journal of Methods in Psychiatric Research. 1996;6:243–251. 10.1002/(SICI)1234-988X(199612)6:4<243∷AID-MPR167>3.3.CO;2-5. [Google Scholar]
- Jacard J. Interactive effects in logistic regression. Sage; Thousand Oaks: 2001. [Google Scholar]
- Jollant F, Lawrence NL, Olié E, Guillaume S, Courtet P. The suicidal mind and brain: A review of neuropsychological and neuroimaging studies. The World Journal of Biological Psychiatry. 2011;12:319–339. doi: 10.3109/15622975.2011.556200. doi:10.3109/15622975.2011.556200. [DOI] [PubMed] [Google Scholar]
- Khurana A, Romer D. Modeling the distinct pathways of influence of coping strategies on youth suicidal ideation: A national longitudinal study. Prevention Science. 2012;13:644–654. doi: 10.1007/s11121-012-0292-3. doi:10.1007/s11121-012-0292-3. [DOI] [PubMed] [Google Scholar]
- Linda WP, Marroquín B, Miranda R. Active and passive problem solving as moderators of the relation between negative life event stress and suicidal ideation among suicide attempters and non-attempters. Archives of Suicide Research. 2012;16:183–197. doi: 10.1080/13811118.2012.695233. doi:10.1080/13811118.2012.695233. [DOI] [PubMed] [Google Scholar]
- Linehan MM, Camper P, Chiles JA, Strosahl K, Shearin E. Interpersonal problem solving and parasuicide. Cognitive Therapy and Research. 1987;11:1–12. doi:10.1007/BF01183128. [Google Scholar]
- Lyubomirsky S, Nolen-Hoeksema S. Effects of self-focused rumination on negative thinking and interpersonal problem solving. Journal of Personality and Social Psychology. 1995;69:176–190. doi: 10.1037//0022-3514.69.1.176. doi:10.1037/0022-3514.69.1.176. [DOI] [PubMed] [Google Scholar]
- Miranda R, Shaffer D. Understanding the suicidal moment in adolescence. Annals of the New York Academy of Sciences. 2013;1304:14–21. doi: 10.1111/nyas.12291. [DOI] [PubMed] [Google Scholar]
- Nezu AM, Ronan GF. Social problem solving as a moderator of stress-related depressive symptoms: A prospective analysis. Journal of Counseling Psychology. 1988;35:134–138. [Google Scholar]
- O'Connor RC, Smyth R, Ferguson E, Ryan C, Williams JMG. Psychological processes and repeat suicidal behavior: A four-year prospective study. Journal of Consulting and Clinical Psychology. 2013;81:1137–1143. doi: 10.1037/a0033751. doi:10.1037/a0033751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Platt JJ, Spivack G, Bloom W. Manual for the means-end problem-solving procedure (MEPS): A measure of interpersonal problem-solving. Hahneman Medical College and Hospital, Department of Medical Health Sciences, Hahneman Community MH/MR center; Philadelphia: 1975. [Google Scholar]
- Pollock LR, Williams JMG. Problem-solving in suicide attempters. Psychological Medicine. 2004;34:163–167. doi: 10.1017/s0033291703008092. doi:10.1017/S0033291703008092. [DOI] [PubMed] [Google Scholar]
- Priester MJ, Clum GA. The problem-solving diathesis in depression, hopelessness, and suicide ideation: A longitudinal analysis. Journal of Psychopathology and Behavioral Assessment. 1993;15:239–254. doi:10.1007/BF01371381. [Google Scholar]
- Schotte DE, Cools J, Payvar S. Problem-solving deficits in suicidal patients: Trait vulnerability or state phenomenon? Journal of Consulting and Clinical Psychology. 1990;58:562–564. doi: 10.1037//0022-006x.58.5.562. doi:10.1037/0022-006X.58.5.562. [DOI] [PubMed] [Google Scholar]
- Shaffer D, Fisher P, Lucas CP, Dulcan MK, Schwab-Stone ME. NIMH diagnostic interview schedule for children version IV (NIMH DISC-IV): Description, differences from previous versions, and reliability of some common diagnoses. Journal of the American Academy of Child and Adolescent Psychiatry. 2000;39:28–38. doi: 10.1097/00004583-200001000-00014. doi:10.1097/00004583-200001000-00014. [DOI] [PubMed] [Google Scholar]
- Speckens AEM, Hawton K. Social problem solving in adolescents with suicidal behavior: A systematic review. Suicide and Life-Threatening Behavior. 2005;35:365–387. doi: 10.1521/suli.2005.35.4.365. doi: 10.1521/suli.2005.35.4.365. [DOI] [PubMed] [Google Scholar]
- Whisman MA, Perez JE, Ramel W. Factor structure of the beck depression inventory – second edition (BDI-II) in a student sample. Journal of Clinical Psychology. 2000;56:545–551. doi: 10.1002/(sici)1097-4679(200004)56:4<545::aid-jclp7>3.0.co;2-u. doi:10.1002/(SICI)1097-4679(200004)56:4<545::AIDJCLP7>3.0.CO;2-U. [DOI] [PubMed] [Google Scholar]
- Williams JMG, Crane C, Barnhofer T, Duggan DS. Psychology and suicidal behaviour: Elaborating the entrapment model. In: Hawton K, editor. Prevention and treatment of suicidal behaviour: From science to practice. Oxford University Press; Oxford: 2005a. pp. 71–90. [Google Scholar]
- Williams JMG, Barnhofer T, Crane C, Beck AT. Problem solving deteriorates following mood challenge in formerly depressed patients with a history of suicidal ideation. Journal of Abnormal Psychology. 2005b;114:421–431. doi: 10.1037/0021-843X.114.3.421. doi:10.1037/0021-843X.114.3.421. [DOI] [PubMed] [Google Scholar]