Abstract
Background
U.S. women Veterans are at increased risk of homelessness and chronic health conditions associated with unintended pregnancy. Veterans Health Administration (VHA) provision of long acting reversible contraceptives (LARC) can assist in healthy pregnancy planning.
Objectives
To evaluate perinatal risk factors and LARC exposure in ever-homeless women Veterans.
Research Design
A retrospective cohort study of women Veterans using VHA administrative data from fiscal years 2002–2015.
Subjects
We included 41,747 ever-homeless Women Veterans age 18–44y and 46,391 housed women Veterans matched by military service period. A subgroup of 7,773 ever-homeless and 8,674 matched housed women Veterans deployed in Iraq and Afghanistan (OEF/OIF/OND) conflicts comprised a second analytic cohort.
Measures
Descriptive statistics compared demographic, military, health conditions, and LARC exposure in ever-homeless vs. housed women Veterans. Multivariable logistic regression explored factors associated with LARC exposure in the OEF/OIF/OND subgroup.
Results
All health conditions were significantly higher in ever-homeless vs. housed Veterans: mental health disorder in 84.5% vs. 48.7% (p<0.001), substance abuse in 35.8% vs. 8.6% (p<0.001), and medical conditions in 74.7% vs. 55.6% (p<0.001). LARC exposure among all VHA users was 9.3% in ever-homeless Veterans vs. 5.4% in housed Veterans (p<0.001). LARC exposure in the OEF/OIF/OND cohort was 14.1% in ever-homeless Veterans vs. 8.2% in housed Veterans (p<0.001). In the OEF/OIF/OND cohort, homelessness along Veterans with medical and mental health indicators were leading LARC exposure predictors.
Conclusions
The VHA is successfully engaging homeless women Veterans and providing LARC access. The prevalence of perinatal risk factors in ever-homeless women Veterans highlights a need for further programmatic enhancements to improve reproductive planning.
Keywords: Homelessness, Veterans, reproductive health, pregnancy
Introduction
Women Veterans are the fastest growing population utilizing Veterans Health Administration (VHA) services, numbering more than 2 million in 2015.1 Unfortunately, Veterans are four times more likely to experience homelessness than civilians and, consequently by default, the VHA has become the largest U.S. homeless healthcare provider.2,3 Providing medical care to Veterans experiencing homelessness is resource intensive due to a high prevalence of chronic health conditions in this population4 and homeless women have additional, though preventable, reproductive health risks5. Access to gender-specific services, including preconception planning, pregnancy-related care, and contraceptive management varies by location in VHA facilities due to availability of subject matter expertise and comfort level of providers. Reproductive health services, especially for those who have chronic health conditions, are essential to address perinatal risk factors and mitigate unintended pregnancies with subsequent adverse outcomes. In this regard, understanding perinatal risk factors and provision of contraceptive care in vulnerable VHA populations can assist in attaining the VHA priority of comprehensive women’s health service expansion.6
While data on the reproductive health of homeless women Veterans are sparse, civilian homeless research identifies significant disparities in access to care and adverse reproductive outcomes. Homeless civilian women experience a high rate of unintended pregnancy that can subsequently impact their ability to gain housing.7 Prenatal homelessness is a risk factor for preterm birth and low birth weight infants.8 Unfortunately, homeless women have low contraceptive utilization, are at high risk for sexual exploitation, and face challenges prioritizing reproductive health care due to competing demands in their high-stress environment.5,9 One study of homeless women Veterans found approximately 30% already have minor children in their custody and 11% have psychotic disorders.10 Additional pregnancies, especially unintended, could further destabilize an already fragile family structure. Despite a recommendation by the American College of Obstetricians and Gynecologists to increase access to long acting reversible contraception (LARC), including intrauterine devices (IUDs) and contraceptive implants, to improve pregnancy planning for homeless women, LARC availability varies widely and is quite limited across the country in non-VHA homeless healthcare organizations.11,12 These issues are compounded for homeless women Veterans who are highly reliant upon the VHA to meet their healthcare needs- including contraceptive management- as they are less likely to have access to healthcare through non-VHA insurance.13 These aspects have not been well studied and thus our research questions focus on perinatal risk factors and LARC exposure in homeless women Veterans.
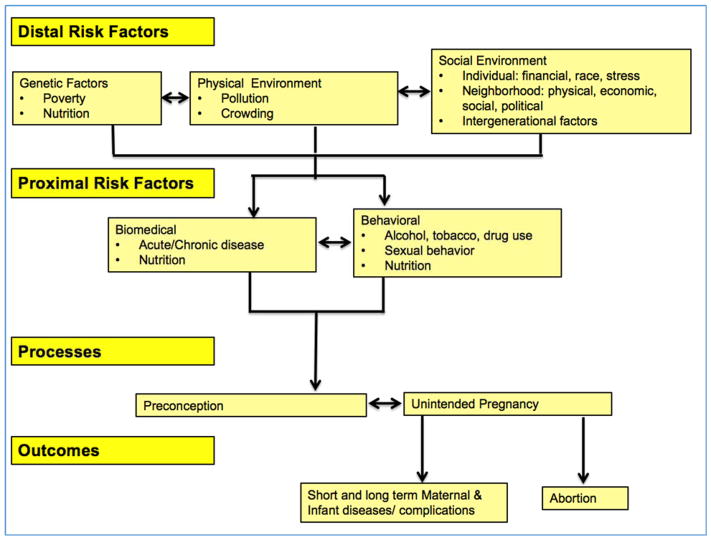
The Integrated Perinatal Health Framework (IPHF)14 is helpful in understanding the intertwined vulnerabilities of women experiencing homelessness and other health or behavioral risk factors, as well as the potential VHA role for improved LARC access for reproductive planning. (Figure 1) The IPHF emphasizes the importance of a life-course approach for studying perinatal health factors, suggesting that disparities in perinatal health and birth outcomes are influenced by stressors that may occur long before a woman becomes pregnant.14
Figure 1.
Adapted from the Integrated Perinatal Health Conceptual Framework14 to highlight the intertwined risks of homelessness, chronic health and behavioral conditions and pregnancy intention on preconception health and pregnancy outcomes
Homelessness and associated health disparities do not occur in isolation and not all homeless women Veterans are affected by the same risk factors. Previous work identified a high prevalence of chronic health conditions in homeless women Veterans accessing VHA services 13,15,16, but these studies have not focused on reproductive age women Veterans and conditions associated with pregnancy risk. The U.S. Centers for Disease Control (CDC) established a list of highest-risk chronic health conditions, such as ischemic heart disease and advanced diabetes mellitus, for which LARC methods should be used as 1st line to decrease risk of unintended pregnancy.17 Additionally, the VHA has expertise in managing behavioral risk factors, such as alcohol, drug or tobacco dependence, which the IPHF lists as proximal risk factors for adverse reproductive outcomes. (Figure 1) Identifying the impact of homelessness and high risk chronic health or behavioral conditions that impact pregnancy outcomes on LARC use for reproductive planning will allow for a richer understanding of potential VHA preventive measures to improve the outcomes for certain women Veterans.
Several large scale projects have demonstrated significant population-level declines in rates of unintended pregnancy and abortion with increased use of LARC.18–21 The prevalence of LARC method use in the U.S. population has increased over the past decade from 2.4% of contraceptive users in 2002 to 11.6% in 2012.22 These methods are safe for women with many chronic health and behavioral conditions17, yet disparities in uptake persist due to a number of access barriers.23 We hypothesized that homeless women Veterans face barriers to obtaining LARC in the VHA and that the current uptake of LARC is lower than the general population benchmark rate of 11.6% mentioned above, based upon these access barriers and the high-risk status of homeless women Veterans compared to a matched, housed group of women Veterans. Thus, the objectives of this study are to assess (1) the prevalence of perinatal risk factors, including chronic health and behavioral conditions, and LARC exposure in homeless versus housed reproductive age women Veterans in the VHA and (2) factors associated with LARC exposure in a subgroup of homeless versus housed women Veterans who served in the recent Iraq and Afghanistan conflicts: Operations Enduring Freedom/Iraqi Freedom/New Dawn (OEF/OIF/OND).
Methods
Participants
All Veterans who accessed VHA services between FY2002–2015 with administrative evidence of homelessness at any time during the observation period (ever-homeless) were identified through a nationwide VHA research database of administrative and clinical data from VHA Corporate Data Warehouse (CDW) managed by the Veteran’s Informatics and Computing Infrastructure (VINCI). 24 We matched controls based upon period of military service available in VINCI tables. Homelessness was identified through use of previously validated International Classification of Diseases, Ninth Revision (ICD-9) codes, Homeless Care stop codes, or treatment specialty codes. 25,26 From the total cohort, we included only women Veterans age 18–44y in birth cohorts for each fiscal year (FY) from October 1, 2001 (start of FY 2002) through September 30, 2015 (end of FY 2015).
In order to address missing demographic and military variables in the full cohort of ever-homeless women Veterans, we identified a subgroup of women Veterans who separated from the military in the OEF/OIF/OND era using an established VHA/Defense Manpower Data Center roster. The full cohort of matched, housed women was also narrowed to those from the OEF/OIF/OND conflict for the subgroup comparisons. These OEF/OIF/OND subgroups had more reliable documentation of demographic and military variables that could impact LARC uptake. This study received approval from the University of Utah Institutional Review Board (IRB) and the Research and Development Committee at the Veterans Administration Salt Lake City Health Care System.
Measures
Demographic variables included age at entry into VHA services, age at first homelessness designation or entry into the VHA, marital status, race/ethnicity, and religious affiliation. Military characteristics included branch of service, combat exposure, and results (positive or negative) of screening for a history of military sexual trauma (MST) in VHA. The demographic variables and military characteristics were extracted from the VA Corporate Data Warehouse (CDW) tables for the full cohort. Combat exposure was extracted from the CDW tables and described as “a flag to indicate whether or not the patient has served in a combat zone.” 27 The MST screening tool is a universal clinical reminder that asks: “While you were in the military: (a) Did you receive uninvited and unwanted sexual attention, such as touching, cornering, pressure for sexual favors, or verbal remarks? and (b) Did someone ever use force or threat of force to have sexual contact with you against your will?” An affirmative response to either question is a positive result in the CDW tables. While MST status was not routinely screened for or reliably captured in structured data until 2004, Veterans who accessed care prior to 2004 were screened at follow-up encounters.25
The IPHF14 risk factors in Figure 1 were used to guide the variables chosen from available structured VHA data, with homelessness as a measurable proxy for the distal risk factors. The “biomedical” proximal risk factors in the IPHF14 included (1) medical conditions that increase the risk of adverse pregnancy outcomes with an unintended pregnancy based upon the Centers for Disease Control U.S. Medical Eligibility Criteria for Contraceptive Use17, (2) mental health conditions prevalent in VHA service users13, and (3) chronic medical conditions prevalent in reproductive age women28. The “behavioral” proximal risk factors in the IPHF14 included (1) ICD-9 codes for alcohol and drug use disorders and (2) evidence of smoking at any time, based on the ICD-9 codes 305.1 or V15.82, as previously validated.29 We chose to classify evidence of smoking as “ever” or “none” because effects of tobacco dependence may persist beyond cessation and impact the recommendation for certain hormonal contraceptives.17
Groupings of ICD-9 codes for chronic health conditions were compiled using the Healthcare Cost and Utilization Project (HCUP) Clinical Classifications Software (CCS; Agency for Healthcare Research and Quality, Rockville, MD).30 Women Veterans were considered to have a diagnosis for a condition if they had at least two instances of an ICD-9 code within the same HCUP group condition 30 days or more apart recorded in the VHA files at any time from entry into VHA services until end of FY 2015. We chose the Elixhauser comorbidity software to assess chronic health condition burden. 31 The Elixhauser index is a method of categorizing comorbidities based upon ICD-9 codes, each category is dichotomous (present or not), and an increasing summary score can be used to predict hospital resource use or in-hospital mortality. This index was chosen because it does not rely heavily on patient age and accounts for mental health and substance use diagnoses that are not accounted for in other comorbidity indices.32 We report both the comorbidity classification prevalence, as well as the individual median Elixhauser summary score used as a predictor of LARC exposure in modeling.
The ICD-9 and Current Procedural Terminology (CPT®) codes and service dates for intrauterine device or contraceptive implant insertion, surveillance, removal or exchange were identified for both ever-homeless and housed women. As some devices can be maintained for up to twelve years, any code from time of entry into VHA services until end of FY 2015 will count as exposure, regardless of whether it was placed prior to the homelessness designation. The date of hysterectomy or sterilization was captured for any women with a procedure during the study time frame via CPT® and ICD-9 codes.
Analyses
We created two analytic cohorts. First is the full cohort of all ever-homeless women Veterans who accessed VHA services between FY2002-FY 2015 who were matched to housed women Veterans by military service period. Differences between demographic characteristics, LARC exposure and the proportion of women with each chronic health or behavioral condition in ever-homeless and housed Veterans were explored with chi-square tests. The Elixhauser comorbidity software was used to develop a summary comorbidity score for each woman and the median score reported for the ever-homeless and housed Veterans.32
We created a second cohort that was narrowed to women who served in the recent OEF/OIF/OND conflicts to take advantage of a rich set of demographic and military service variables available for these Veterans. This second cohort allowed for exploration of factors associated with LARC exposure. A total of 59 patients were removed from the analysis for conflicting evidence of which LARC method was first used. Coast Guard veterans were also excluded due to very low numbers (n=6). In addition to the comparative analyses described for the full cohort, multivariable logistic regression examined associations of housing status, demographics, chronic health conditions, behavioral risk factors, and the Elixhauser comorbidity summary score32 to LARC exposure in the OEF/OIF/OND cohort. Though the prevalence of bariatric surgery and solid organ transplants in these women were low, these conditions were assessed separately, as the CDC recommends LARC use to decrease pregnancy risk for only two years after surgery, as compared to other chronic conditions which do not have time restrictions on LARC recommendations.17 Women not at risk for pregnancy due to hysterectomy or sterilization were excluded from the model. No modeling occurred on the full cohort. We fit four logistic regression models of descending granularity. The first fit examined the probability of having any LARC against not having any such exposure. The second estimates the model of having reversible (IUD and Implant) vs non-reversible contraceptive (Hysterectomy and Sterilization). Within reversible and non-reversible, we modeled IUD versus Implant and Hysterectomy versus Sterilization, respectively. Models were fit using a logistic regression model in R Statistical Software version 3.3.1.
Results
Ever-homeless vs. housed women Veterans from all VHA users
We identified a total of 41,747 ever-homeless women Veterans who accessed care at the VHA between FY2002–2015 and 46,391 housed women Veterans matched upon period of service. The mean number of VHA encounters (outpatient visit or inpatient admission) during the timeframe was 208 for homeless Veterans vs. 95 for housed Veterans. A total of 392 homeless and 2350 housed women Veterans in the cohort had only one VHA encounter during the study timeframe, although they could have received care before or after the study years. Mean age at 1st homeless designation was 38y. The ever-homeless Veterans were less likely to be married (19% vs. 37%) and more likely to identify as black race (43% vs 20%) and non-Hispanic ethnicity (87% vs. 69%). The ever-homeless cohort was more likely to have experienced military sexual trauma based on VHA screen results (40% vs 21%). (Table 1)
Table 1.
Characteristics of all homeless women Veterans who accessed the Veterans Healthcare Administration (VHA) between FY2002–2015 and the subgroup of homeless women Veterans from Iraq and Afghanistan conflicts compared to a matched housed cohort by period of military service.
| All VHA Users | OEF/OIF/OND VHA Users | ||||
|---|---|---|---|---|---|
| Variable* | Value | Homeless N (%) | Housed N (%) | Homeless N (%) | Housed N (%) |
| TOTAL | 41747 (100) | 46391 (100) | 7573 (100) | 8674 (100) | |
| Age Group | 18–34y | 20247 (49) | 20169 (44) | 6445 (85) | 6460 (75) |
| 35–44y | 21497 (51) | 26222 (56) | 1127 (15) | 2214 (25) | |
| Marital Status | Married | 7791 (19) | 17215 (37) | 2235 (30) | 2871 (33) |
| Divorced/Separated/Widowed | 21146 (51) | 14397 (31) | 527 (7) | 1482 (9) | |
| Single | 12658 (30) | 10662 (23) | 4801 (63) | 4840 (56) | |
| Declined/Missing | 847 (2) | 5356 (12) | 9 (0) | 8 (0) | |
| Race | White | 17884 (43) | 21883 (47) | 3111 (41) | 4896 (56) |
| Black | 17962 (43) | 9251 (20) | 3517 (46) | 2117 (24) | |
| Other | 1608 (4) | 1378 (3) | 402 (5) | 378 (5) | |
| Declined/Missing | 4293 (10) | 13879 (30) | 543 (7) | 1283 (15) | |
| Ethnicity | Hispanic | 2439 (6) | 2320 (5) | 820 (11) | 739 (9) |
| Not Hispanic | 36103 (87) | 32090 (69) | 6417 (85) | 6881 (79) | |
| Declined/Missing | 3205 (7) | 11981 (26) | 336 (4) | 1054 (12) | |
| Religion | Christian | 29614 (71) | 29546 (64) | 5463 (70) | 6086 (62) |
| Non-Christian | 557 (1) | 403 (1) | 82 (1) | 62 (1) | |
| No Preference | 10661 (26) | 16841 (36) | 2075 (27) | 3117 (32) | |
| Declined/Missing | 3147 (8) | 6320 (14) | 168 (2) | 632 (6) | |
| Branch of Service | Air Force | 6433 (15) | 7491 (16) | 744 (10) | 1134 (13) |
| Army | 22588 (54) | 19480 (42) | 5033 (66) | 6437 (74) | |
| Marine Corps | 2097 (5) | 1775 (4) | 270 (4) | 211 (2) | |
| Navy | 8803 (21) | 6560 (14) | 1523 (20) | 889 (10) | |
| Other/Missing | 2757 (7) | 11963 (26) | 3 (0) | 3 (0) | |
| Rank | Enlisted | 7440 (18) | 7788 (17) | 7440 (98) | 7788 (90) |
| Officer | 133 (0) | 886 (2) | 133 (2) | 886 (10) | |
| Missing | 34174 (82) | 37717 (81) | 0 (0) | 0 (0) | |
| Combat Exposure | No | 32940 (79) | 30311 (65) | 5070 (62) | 5293 (62) |
| Yes | 4303 (10) | 4115 (9) | 3080 (38) | 3173 (38) | |
| Missing | 4504 (11) | 11965 (26) | 0 (0) | 0 (0) | |
| MST | No | 22151 (53) | 23958 (52) | 4579 (63) | 5596 (78) |
| Yes | 16756 (40) | 9748 (21) | 2690 (37) | 1520 (22) | |
| Declined/Missing | 2840 (7) | 12685 (27) | 23 (0) | 29 (0) | |
| Elixhauser Co-morbidity Summary Score | Mean Score | 5.385 | 3.677 | 3.776 | 2.339 |
| Median Score | 5 | 3 | 3 | 2 | |
All variables significant with Chi square values <0.001, except the combat flag in the OEF/OIF cohort
VHA = Veterans Healthcare Administration; OEF/OIF/OND= Operation Enduring Freedom/Operation Iraqi Freedom/Operation New Dawn conflicts; FY = fiscal year; MST = military sexual trauma
Some variables may equal >100% due to rounding and >1 reported response, i.e. marital status, religion, branch
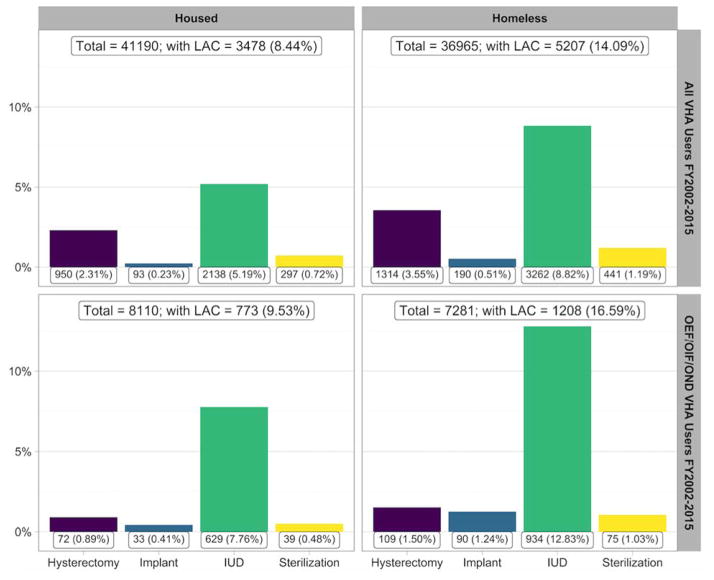
Ever-homeless Veterans were more likely to have a number of chronic health conditions with a median Elixhauser co-morbidity summary score of 5.39 vs. 3.68 as compared to the housed cohort. (Table 1) The prevalence of all chronic health conditions was significantly higher in ever-homeless vs. housed Veterans: mental health disorders in 84.5% vs. 48.7% (p<0.001), substance abuse disorders in 35.8% vs. 8.6% (p<0.001), and one or more high-risk medical conditions in 74.7% vs. 55.6% (p<0.001). The top five common chronic health conditions in ever-homeless women Veterans were noted to be hypertension, obesity, asthma, diabetes, and heart diseases. Reproductive cancers that included cervical, endometrial and ovarian diagnoses were also more frequent in ever-homeless than housed Veterans. Mental health disorders and substance use disorders were 2–4 times more common in ever-homeless Veterans, regardless of diagnoses type. Evidence of smoking was noted in nearly half of all homeless women Veterans (47.8%). (Table 2) Exposure to LARC in the overall VHA user cohort was 9.3% in homeless Veterans compared to 5.4% in housed Veterans. (p<0.001) Sterilization and hysterectomy were significantly higher in ever-homeless vs. housed women Veterans from service periods (4.7% vs. 3.0%; p=0.019) (Figure 2) (Figure 2)
Table 2.
Prevalence of chronic health conditions in all homeless women Veterans who accessed the VHA between FY2002–2015 and the subgroup of recent Iraq and Afghanistan conflict homeless women Veterans compared to a matched housed cohort (from Operations Enduring Freedom, Iraqi Freedom, and New Dawn, OEF/OIF/OND).
| All VHA Users FY2002–2015 |
OEF/OIF/OND VHA Users FY2002–2015 |
||||
|---|---|---|---|---|---|
| Variable | Value | Homeless N (%) | Housed N (%) | Homeless N (%) | Housed N (%) |
| TOTAL | 41747 (100.00) | 46391 (100.00) | 7573 (100.00) | 8674 (100.00) | |
| Any medical diagnosis(es) | 31202 (74.74) | 25800 (55.61) | 4701 (62.08) | 3892 (44.87) | |
| CDC MEC Diagnoses | Hypertension | 16309 (39.07) | 12598 (27.16) | 1359 (17.95) | 1097 (12.65) |
| Advanced diabetes mellitus | 6351 (15.21) | 4828 (10.41) | 391 (5.16) | 319 (3.68) | |
| Reproductive cancer | 4962 (11.89) | 3870 (8.34) | 889 (11.74) | 730 (8.42) | |
| High risk cardiac disease* | 3937 (9.43) | 2784 (6.00) | 195 (2.58) | 140 (1.61) | |
| Moderate risk cardiac disease** | 2849 (6.82) | 2084 (4.49) | 224 (2.96) | 179 (2.06) | |
| Epilepsy | 1988 (4.76) | 1171 (2.52) | 221 (2.92) | 81 (0.93) | |
| Cerebral vascular accident | 1677 (4.02) | 1105 (2.38) | 93 (1.23) | 46 (0.53) | |
| Breast cancer | 837 (2.01) | 994 (2.04) | 45 (5.94) | 70 (0.81) | |
| Systemic lupus erythematosis | 600 (1.43) | 554 (1.19) | 50 (0.66) | 58 (0.67) | |
| Severe cirrhosis | 514 (1.23) | 264 (0.57) | 16 (0.21) | 7 (0.08) | |
| HIV/AIDS | 402 (0.96) | 148 (0.32) | 23 (0.30) | 14 (0.16) | |
| Tuberculosis | 220 (0.53) | 121 (0.26) | 27 (0.36) | 23 (0.27) | |
| Thrombogenic mutations | 209 (0.50) | 175 (0.38) | 21 (0.28) | 13 (0.15) | |
| Malignant liver tumors | 49 (0.11) | 25 (0.05) | 3 (0.04) | 0 (0) | |
| Sickle cell disease | 36 (0.09) | 16 (0.04) | 4 (0.05) | 1 (0.01) | |
| Bariatric surgery | 133 (0.32) | 87 (0.19) | 5 (0.07) | 4 (0.05) | |
| Solid organ transplant | 58 (0.14) | 89 (0.19) | 4 (0.05) | 4 (0.05) | |
| Prevalent medical conditions in reproductive age women | Obesity | 19466 (46.63) | 14336 (30.90) | 2834 (37.42) | 2006 (23.13) |
| Asthma or chronic obstructive pulmonary disease | 8379 (20.07) | 6272 (13.52) | 1161 (15.33) | 872 (10.05) | |
| Thyroid disease | 5627 (13.48) | 5553 (11.97) | 566 (7.47) | 628 (7.24) | |
| Inflammatory bowel diseases | 451 (1.08) | 572 (1.23) | 47 (0.62) | 61 (0.70) | |
| Rheumatoid arthritis | 992 (2.38) | 950 (2.05) | 62 (0.82) | 68 (0.78) | |
| Any psychiatric diagnosis(es) | 35280 (84.51) | 22598 (48.71) | 6461 (85.32) | 4491 (51.78) | |
| Post-traumatic stress disorder/Adjustment disorder | 25878 (61.99) | 12841 (27.68) | 5328 (70.36) | 3255 (37.53) | |
| Anxiety disorder | 11959 (28.65) | 6478 (13.96) | 1335 (17.63) | 681 (7.85) | |
| Mood disorder | 32957 (78.95) | 20593 (44.39) | 5866 (77.46) | 3755 (43.29) | |
| Schizophrenia | 4274 (10.24) | 1218 (2.63) | 315 (4.16) | 46 (0.53) | |
| Suicide attempt/self-inflicted injury | 2846 (6.82) | 677 (1.46) | 370 (4.89) | 92 (1.06) | |
| Any substance use disorder(s) | 14950 (35.81) | 3986 (8.59) | 1966 (25.96) | 507 (5.85) | |
| Alcohol abuse | 11200 (26.83) | 2704 (5.83) | 1430 (18.89) | 399 (4.60) | |
| Substance use disorder | 11734 (28.11) | 2351 (5.07) | 1384 (18.28) | 213 (2.46) | |
| Evidence of smoking | 19943 (47.77) | 11759 (25.35) | 2938 (38.80) | 1804 (20.80) | |
High risk cardiac diagnoses include coronary artery disease, prosthetic mechanical valve, complex congenital heart disease, peripartum cardiomyopathy, NYHA class II/IV, aortic root dilation >4cm, severe pulmonary hypertension, severe valvular disease with heart failure
Moderate risk cardiac diagnoses include arrhythmias, mild left ventricular dysfunction, moderate native valve disease, mild aortic root dilation, hypertrophic cardiomyopathy
VHA = Veterans Healthcare Administration; OEF/OIF/OND= Operation Enduring Freedom/Operation Iraqi Freedom/Operation New Dawn conflicts; FY= fiscal year; CDC MEC = Centers for Disease Control Medical Eligibility Criteria for Contraceptive Use conditions associated with increased adverse health outcomes as a result of pregnancy
Figure 2.
Frequency of type of long acting reversible contraceptives, hysterectomy and sterilization by homelessness status in all women accessing Veterans Health Administration services from fiscal years 2002–2015 and a subgroup of Women Veterans from recent Iraq and Afghanistan conflicts (Operations Enduring Freedom, Iraqi Freedom, and New Dawn, OEF/OIF/OND).
VHA = Veterans Health Administration; LAC = long acting contraceptives, including permanent measures of hysterectomy and sterilization, as well as long acting reversible contraceptives(LARC), intrauterine devices (IUD) and implants.
Women Veterans from OEF/OIF/OND vs. all military service periods
We utilized an official roster of OEF/OIF/OND Veterans to identify a subgroup of 7,773 ever-homeless women Veterans from these recent conflicts within the full cohort of ever-homeless Veterans who accessed care at the VHA between FY2002–2015 and matched them to 8,674 housed OEF/OIF/OND women Veterans. The OEF/OIF/OND cohort was younger than the full cohort, with 79% aged 18–34 years compared to 46% of the full cohort of all VHA users, and they were more likely to be single (59% vs. 29%). Additionally, 71% of OEF/OIF/OND women affiliated with the Army as their branch of service, compared to 41% of all VHA users.
Compared to the full cohort of all VHA users, the OEF/OIF/OND cohort had a lower Elixhauser co-morbidity summary score (4.57 vs. 3.03), but this could be accounted for by the younger age. (Table 1) The prevalence of chronic health conditions was overall lower for OEF/OIF/OND Veterans compared to all VHA users, but this trend is only in the chronic medical conditions, while mental health and substance use disorders remain prevalent. Smoking evidence was noted in 39% of homeless women Veterans from OEF/OIF/OND; housed women Veterans had lower rates of smoking evidence by administrative codes. (Table 2)
Ever-homeless vs. housed women Veterans from OEF/OIF/OND
Within the OEF/OIF/OND cohort, ever-homeless women Veterans were younger, age 18–34 years (85% vs 74%), and of black race (46% vs. 24%). The OEF/OIF/OND ever-homeless Veterans were more likely than the housed Veterans to have served in the Navy (20% vs. 10%) and experienced MST based on VHA screen results (46% vs. 24%). (Table 1)
Exposure to LARC in the OEF/OIF/OND cohort was 14.1% in ever-homeless Veterans compared to 8.2% in housed Veterans (p<0.001). Additionally, despite the younger age of this cohort, sterilization and hysterectomy were non-significantly higher in ever-homeless vs. housed women Veterans from OEF/OIF/OND (2.5% vs. 1.4%; p=0.523) (Figure 2) For the overall OEF/OIF/OND cohort of women Veterans, those in the younger age group of 18–34 years and the presence of any medical or mental health indicator were strong predictors of receiving any LARC (Table 3). Furthermore, as compared to Army Veterans, those in the marines or the navy were more likely to have received any contraception. Other predictors of LARC were a history of combat exposure, positive screen for military sexual trauma, and white race. Ever homeless women Veterans were more likely to receive LARC (OR 1.22; 95%CI 1.09–1.36).
Table 3.
Variable association with long acting reversible contraceptive (LARC) exposure, sterilization, or hysterectomy among women Veterans from recent Iraq and Afghanistan conflicts (Operations Enduring Freedom, Iraqi Freedom, and New Dawn, OEF/OIF/OND).
| Variable | Level | Any contraception v. None3 | Reversible v. Non-reversible4 | IUD v. Implant | Hysterectomy v. Sterilization | ||||
|---|---|---|---|---|---|---|---|---|---|
| N | Odds Ratio (95% CI)1,2 | N | Odds Ratio (95% CI)1,2 | N | Odds Ratio (95% CI)1,2 | N | Odds Ratio (95% CI)1,2 | ||
| Age Group | 18–34 | 12733 | (Ref)*** | 1793 | (Ref)*** | 1589 | (Ref) | 204 | (Ref)*** |
| 35–44 | 2653 | 0.44 (0.37–0.52) *** | 188 | 0.19 (0.13–0.27) *** | 97 | 1.19 (0.51–3.36) | 91 | 7.64 (3.62–17.65) *** | |
| Any Medical Indicators | 8138 | 1.45 (1.29–1.63) *** | 1368 | 0.80 (0.56–1.14) | 1135 | 1.38 (0.87–2.16) | 233 | 1.17 (0.57–2.43) | |
| Any Mental Health Indicators | 10494 | 1.52 (1.31–1.77) *** | 1694 | 1.05 (0.66–1.6) | 1432 | 0.84 (0.41–1.59) | 262 | 0.83 (0.29–2.27) | |
| Any Substance Abuse Indicators | 2411 | 0.87 (0.76–1.01) | 432 | 1.30 (0.90–1.90) | 361 | 1.40 (0.82–2.43) | 71 | 0.56 (0.26–1.18) | |
| Evidence of Smoking | 4553 | 1.10 (0.98–1.22 | 769 | 0.95 (0.70–1.28) | 645 | 1.12 (0.73–1.73) | 124 | 2.35 (1.27–4.45) ** | |
| Solid Organ Transplant | 8 | 0.63 (0.03–3.77) | 1 | #N/A | 0 | (Ref) | 1 | #N/A | |
| Bariatric Surgery | 8 | 1.27 (0.18–5.66) | 2 | #N/A | 2 | #N/A | 0 | #N/A | |
| Branch of Service | Air Force | 1709 | 1.03 (0.87–1.21) | 197 | 1.02 (0.66–1.62) | 164 | 0.77 (0.42–1.48) | 33 | 0.87 (0.32–2.43) |
| Army | 10913 | (Ref)*** | 1332 | (Ref) | 1131 | (Ref) | 201 | (Ref) | |
| Marines | 471 | 1.35 (1.04–1.73) * | 80 | 1.18 (0.58–2.73) | 72 | 0.45 (0.21–1.08) | 8 | 0.51 (0.10–2.58) | |
| Navy | 2293 | 1.32 (1.15–1.51) *** | 372 | 0.95 (0.66–1.38) | 319 | 0.79 (0.48–1.33) | 53 | 0.45 (0.20–0.97) * | |
| Combat Exposure | 5993 | 1.16 (1.05–1.27) ** | 876 | 0.90 (0.69–1.17) | 735 | 1.58 (1.06–2.37) * | 141 | 2.30 (1.31–4.12) ** | |
| Ever Homeless | 7279 | 1.21 (1.09–1.36) *** | 1208 | 0.95 (0.66–1.36) | 1024 | 1.48 (0.78–2.92) | 184 | 0.77 (0.362–1.65) | |
| Marital Status | Divorced/Separated | 1291 | 1.13 (0.93–1.37) | 151 | 0.47 (0.30–0.76) ** | 106 | 1.80 (0.73–5.45) | 45 | 1.83 (0.69–5.11) |
| Married | 4697 | 1.06 (0.95–1.18) | 595 | 0.42 (0.32–0.56) *** | 462 | 1.65 (1.04–2.71) * | 133 | 0.78 (0.43–1.40) | |
| Single | 9370 | (Ref) | 1232 | (Ref) | 1115 | (Ref) | 117 | (Ref) | |
| Unknown/Other | 28 | 0.91 (0.21–2.73) | 3 | #N/A | 3 | #N/A | 0 | #N/A | |
| MST | Declined | 49 | 0.60 (0.18–1.51) | 4 | 0.22 (0.02–2.01) | 2 | #N/A | 2 | < 0.01 |
| No | 9695 | (Ref)*** | 1259 | (Ref) | 1085 | (Ref) | 174 | (Ref) | |
| Unknown | 1596 | 0.03 (< 0.01–0.07) *** | 3 | 0.42 (0.03–11.01) | 2 | 0.04 (< 0.01–1.10) * | 1 | #N/A | |
| Yes | 4046 | 1.15 (1.03–1.28) ** | 715 | 0.96 (0.72–1.28) | 597 | 0.80 (0.53–1.20) | 118 | 0.80 (0.44–1.45) | |
| Race | Black | 4012 | 0.78 (0.68–0.89) *** | 469 | 1.00 (0.69–1.44) | 394 | 0.74 (0.46–1.20) | 75 | 2.39 (1.10–5.35) * |
| Other/Unknown | 5448 | 0.94 (0.84–1.06) | 771 | 0.93 (0.67–1.29) | 656 | 1.47 (0.90–2.40) | 115 | 2.16 (1.10–4.37) * | |
| White | 5926 | (Ref)** | 741 | (Ref) | 636 | (Ref)* | 105 | (Ref) | |
| Religion | Christian | 10002 | (Ref) | 1287 | (Ref) | 1085 | (Ref) | 202 | (Ref) |
| Other | 863 | 1.15 (0.94–1.41) | 128 | 0.95 (0.57–1.64) | 107 | 1.34 (0.60–3.65) | 21 | 0.67 (0.23–1.97) | |
| Unknown | 4521 | 1.07 (0.96–1.19) | 566 | 1.23 (0.90–1.69) | 494 | 1.01 (0.66–1.57) | 72 | 0.85 (0.45–1.63) | |
Logistic regression models were fit with data that was limited to Army, Navy, Air Force and Marines. Also those where the type of LARC at first evidence could not be conclusively determined were excluded.
LARC= long acting reversible contraception; IUD= intrauterine device; CI= confidence interval; MST= military sexual trauma
Significance for variable overall given next to the reference level denoted by “(Ref)”. Estimates provided are the difference from the reference level and the provided significance for that coefficient specifically not the variable overall.
Significance levels are interpreted as follows: ‘***’, p-value ≤ 0.001; ‘**’, p-value ≤ 0.01; ‘*’, p-value ≤ 0.05; ‘.’, p-value ≤ 0.10, no symbol indicates the coefficient or variable was not significant.
Any = IUD, Implant, Hysterectomy, or Sterilization.
Reversible = IUD or Implant.
Discussion
This study identified a significantly larger number of homeless women Veterans accessing LARC methods within the VHA compared to a housed Veteran cohort, especially in those from the OEF/OIF/OND conflicts. The LARC uptake among homeless women Veterans, especially those from recent conflicts, compares favorably to the rates reported for the general population.22 Our study is unique in the number of ever-homeless women Veterans studied and its longitudinal nature over a fourteen-year time period. The VHA investment in homeless outreach programs and women’s healthcare services is meeting the reproductive planning needs of many homeless women Veterans, but LARC exposure remains lower than expected given the prevalence of perinatal risk factors in this population. While not every woman will choose a LARC method and respect for reproductive autonomy needs to be maintained, the high-risk conditions and complex lives of homeless women Veterans should prompt providers to screen for pregnancy risk, recommend LARC methods and minimize barriers for those desiring them.33
The IPHF14 framework outlines a life-course approach which acknowledges the multitude of preconception risks that can adversely impact pregnancy outcomes and can be used to consider options for interventions in the VHA (Figure 1). Homeless healthcare is a VHA priority with development of the Homeless Patient Aligned Care Teams (H-PACT) that have successfully increased primary care engagement and decreased costly emergency services.34,35 Addressing homelessness and housing instability will help to mitigate many of the distal risk factors in the IPHF. (Figure 1) Currently, housing and mental health engagement are first line priorities of H-PACT and reproductive health needs are not addressed until the patient is established in primary care and then may need consultant referrals to gynecology, if the primary care provider is not comfortable with gender-specific needs. Reproductive health assessments need to be part of the H-PACT screening process, as an unplanned pregnancy would destabilize attempts for housing and risk adverse pregnancy outcomes at a time of environmental and emotional stress.36 Our findings of the high prevalence of both “biomedical” and “behavioral” perinatal health proximal risk factors (Figure 1) highlights the need to incorporate reproductive risk assessments into chronic disease management, mental health interactions, and behavioral health interventions to avoid missed, reproductive planning opportunities in the VHA and could improve the life course for both the Veteran and her family.
The VHA expanded women’s health care to meet gender-specific needs, yet access barriers still persist, especially for high-risk populations. The 2015 Study of Barriers for Women Veterans to VA Health Care identified significant limitations to the VHA goal of comprehensive women’s healthcare across the healthcare system. Women veterans may bypass the nearest VHA clinic because comprehensive primary care services, including contraception, are not available. Finding transportation to specialty services was most burdensome for women with the highest levels of disability.37 For homeless women with limited resources, this access barrier may not be overcome. During the study timeframe, the VHA established “designated women’s health providers” (DWHPs) in primary care settings and this focus and training may account for the increased LARC exposure in this study. While VHA LARC exposure appears to be overall higher in homeless women Veterans, racial, ethnic and socioeconomic disparities appear to persist in access to essential reproductive health services.38–40 The higher prevalence of hysterectomy and reproductive cancers found in this study that could be managed with LARC methods and cervical cancer screening in homeless women Veterans is concerning. Many DWHPs work in rural settings with limited numbers of women Veterans, many of whom are no longer reproductive age. Ongoing DWHP training for LARC, could improve the comfort level for these providers and decrease the need for gynecology referrals at central facilities.41
Limitations of this study include the lack of data on healthcare utilization by women outside VHA facilities by means of private insurance, Medicare/Medicaid, or direct referral from VHA to community care via fee-based services or the Veterans Choice Program. Thus, we may be under-representing LARC usage in both groups, but especially in housed women Veterans who may seek non-VHA care at greater rates. Not all women Veterans access VHA services for all healthcare needs, but this gap in data is more likely to impact the housed cohort results, as homeless women often do not have other insurance coverage options and LARC services in civilian homeless clinics are limited. The use of structured data may lead to misclassification of chronic health conditions, although the prevalence is consistent with previous utilization data.4 Homelessness is not typically a constant over many years, but we chose to stratify by any housing instability (ever-homeless) compared to those with none, because many socio-economic stressors pre-date and persist beyond the administrative capture of homelessness. Smoking status may also change over time and the positive predictive value of the structured administrative data is only 69%, so misclassification may have occurred.29 Finally, LARC uptake was defined as exposure at any point due to the ability to use these methods for many years, which may misrepresent actual use during times of greatest housing instability.
In conclusion, this study is a large, national longitudinal exploration of perinatal risk factors, including chronic health conditions and behavioral risk factors, and exposure to LARC methods in reproductive age, ever-homeless and housed women Veterans. Our results highlight modest success in addressing health disparities through LARC access for homeless women Veterans, which may impact reproductive planning and their overall health and well-being. These data can assist in targeting interventions, such as integration of family planning services into homeless care, flagging housing instability for women’s health providers and medical subspecialists to prioritize reproductive counseling, or extending LARC provider training into areas with a high prevalence of homelessness. The VHA provides a large volume of homeless healthcare in this country and strives to meet essential needs for this population, including family planning services. As an integrated healthcare system serving hundreds of thousands of women Veterans each year, addressing barriers to LARC uptake for all women Veterans could have far reaching implications on population level adverse pregnancy statistics, as well as individual Veteran outcomes. Lessons learned from VHA may have implications for underserved populations in the general community.
Acknowledgments
NIH/NICHD Grant IK12HD085816 (PI: Silver); University of Utah’s Health Equity and Inclusion Seed Grant; VA HSR&D grant #IIR 12-084 (PI: Gundlapalli) and VA Salt Lake City Center of Innovation Award #I50HX001240 from the Health Services Research and Development of the Office of Research and Development of the US Department of Veterans Affairs. Marjorie Carter for assistance in data acquisition
Footnotes
Disclosures: The authors report no conflicts of interest.
References
- 1.U.S. Department of Veterans Affairs. [Accessed November 30, 2016];Women Veterans Population [Office of Public Affairs Fact Sheet] 2016 Oct 20; Available at: http://www1.va.gov/womenvet/docs/WomenVeteransPopulationFactSheet.pdf.
- 2.Balshem H, Christensen V, Tuepker A, et al. A Critical Review of the Literature Regarding Homelessness among Veterans. 2011 VA-ESP Project #05–225. [PubMed] [Google Scholar]
- 3.Statement of Peter H. Dougherty, Director, Homeless Veterans Program. U.S. Department of Veterans Affairs; Apr 9, 2008. [Accessed November 30, 2016]. Available at: http://www.va.gov/OCA/testimony/hvac/080409PD.asp. [Google Scholar]
- 4.Breland JY, Chee CP, Zulman DM. Racial Differences in Chronic Conditions and Sociodemographic Characteristics Among High-Utilizing Veterans. J Racial Ethn Health Disparities. 2015;2:167–75. doi: 10.1007/s40615-014-0060-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kennedy S, Grewal M, Roberts EM, et al. A qualitative study of pregnancy intention and the use of contraception among homeless women with children. J Health Care Poor Underserved. 2014;25:757–70. doi: 10.1353/hpu.2014.0079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Yano EM, Bastian LA, Frayne SM, et al. Toward a VA Women’s Health Research Agenda: setting evidence-based priorities to improve the health and health care of women veterans. J Gen Intern Med. 2006;21:S93–101. doi: 10.1111/j.1525-1497.2006.00381.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Webb DA, Culhane J, Metraux S, et al. Prevalence of episodic homelessness among adult childbearing women in Philadelphia, PA. Am J Public Health. 2003;93:1895–6. doi: 10.2105/ajph.93.11.1895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cutts DB, Coleman S, Black MM, et al. Homelessness during pregnancy: a unique, time-dependent risk factor of birth outcomes. Matern Child Health J. 2015;19:1276–83. doi: 10.1007/s10995-014-1633-6. [DOI] [PubMed] [Google Scholar]
- 9.Nyamathi A, Wenzel S, Keenan C, et al. Associations between homeless women’s intimate relationships and their health and well-being. Res Nurs Health. 1999;22:486–95. doi: 10.1002/(sici)1098-240x(199912)22:6<486::aid-nur6>3.0.co;2-6. [DOI] [PubMed] [Google Scholar]
- 10.Tsai J, Mota NP, Pietrzak RH. Characteristics and Use of Services Among Literally Homeless and Unstably Housed U.S. Veterans With Custody of Minor Children. Psychiatr Serv. 2015;66:1083–90. doi: 10.1176/appi.ps.201400300. [DOI] [PubMed] [Google Scholar]
- 11.Saver BG, Weinreb L, Gelberg L, et al. Provision of contraceptive services to homeless women: results of a survey of health care for the homeless providers. Women Health. 2012;52:151–61. doi: 10.1080/03630242.2011.649829. [DOI] [PubMed] [Google Scholar]
- 12.American College of Obstetricians and Gynecologists Committee Opinion No. 576: Health Care for Homeless Women. Obstet Gynecol. 2013;122:936–40. doi: 10.1097/01.AOG.0000435417.29567.90. [DOI] [PubMed] [Google Scholar]
- 13.Katon JG, Hoggatt KJ, Balasubramanian V, et al. Reproductive health diagnoses of women veterans using department of Veterans Affairs health care. Med Care. 2015;53:S63–7. doi: 10.1097/MLR.0000000000000295. [DOI] [PubMed] [Google Scholar]
- 14.Misra DP, Guyer B, Allston A. Integrated perinatal health framework. A multiple determinants model with a life span approach. Am J Prev Med. 2003;25:65–75. doi: 10.1016/s0749-3797(03)00090-4. [DOI] [PubMed] [Google Scholar]
- 15.Tsai J, Mota NP, Pietrzak RH. U.S. Female Veterans Who Do and Do Not Rely on VA Health Care: Needs and Barriers to Mental Health Treatment. Psychiatr Serv. 2015;66:1200–6. doi: 10.1176/appi.ps.201400550. [DOI] [PubMed] [Google Scholar]
- 16.Gabrielian S, Yuan AH, Anderson RM, et al. Diagnoses Treated in Ambulatory Care Among Homeless-Experienced Veterans: Does Supported Housing Matter? J Prim Care Community Health. 2016;7:281–7. doi: 10.1177/2150131916656009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Curtis KM, Tepper NK, Jatlaoui TC, et al. U.S. Medically Eligibility Criteria for Contraceptive Use, 2016. MMWR Recomm Rep. 2016;65:1–104. doi: 10.15585/mmwr.rr6503a1. [DOI] [PubMed] [Google Scholar]
- 18.Harper CC, Rocca CH, Thompson KM, et al. Reductions in pregnancy rates in the USA with long-acting reversible contraception: a cluster randomised trial. Lancet. 2015;386:562–8. doi: 10.1016/S0140-6736(14)62460-0. [DOI] [PubMed] [Google Scholar]
- 19.Peipert JF, Madden T, Allsworth JE, et al. Preventing unintended pregnancies by providing no-cost contraception. Obstet Gynecol. 2012;120:1291–7. doi: 10.1097/aog.0b013e318273eb56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Biggs MA, Rocca CH, Brindis CD, et al. Did increasing use of highly effective contraception contribute to declining abortions in Iowa? Contraception. 2015;91:167–73. doi: 10.1016/j.contraception.2014.10.009. [DOI] [PubMed] [Google Scholar]
- 21.Ricketts S, Klingler G, Schwalberg R. Game change in Colorado: widespread use of long-acting reversible contraceptives and rapid decline in births among young, low-income women. Perspect Sex Reprod Health. 2014;46:125–32. doi: 10.1363/46e1714. [DOI] [PubMed] [Google Scholar]
- 22.Kavanaugh ML, Jerman J, Finer LB. Changes in Use of Long-Acting Reversible Contraceptive Methods Among U.S. Women, 2009–2012. Obstet Gynecol. 2015;126:917–27. doi: 10.1097/AOG.0000000000001094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kavanaugh ML, Jerman J, Hubacher D, et al. Characteristics of women in the United States who use long-acting reversible contraceptive methods. Obstet Gynecol. 2011;117:1349–57. doi: 10.1097/AOG.0b013e31821c47c9. [DOI] [PubMed] [Google Scholar]
- 24.U.S. Department of Veterans Affairs. [Accessed November 30, 2016];VA Informatics and Computing Infrastructure (VINCI) [Health Service research & Development web site] 2014 Dec 17; Available at: http://www.hsrd.research.va.gov/for_researchers/vinci/
- 25.Peterson R, Gundlapalli AV, Metraux S, et al. Identifying Homelessness among Veterans Using VA Administrative Data: Opportunities to Expand Detection Criteria. PLoS One. 2015;10:e0132664. doi: 10.1371/journal.pone.0132664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Brignone E, Gundlapalli AV, Blais RK, et al. Differential Risk for Homelessness Among US Male and Female Veterans With a Positive Screen for Military Sexual Trauma. JAMA Psychiatry. 2016;73:582–9. doi: 10.1001/jamapsychiatry.2016.0101. [DOI] [PubMed] [Google Scholar]
- 27.Gonsoulin M. VIReC Factbook: Corporate Data Warehouse (CDW) Patient Domain. Hines IL: U.S Department of Veteran Affairs, Health Services Research and Development Service, VA Information Resource Center; 2016. [Google Scholar]
- 28.Rocca WA, Boyd CM, Grossardt BR, et al. Prevalence of multimorbidity in a geographically defined American population: patterns by age, sex, and race/ethnicity. Mayo Clin Proc. 2014;89:1336–49. doi: 10.1016/j.mayocp.2014.07.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Floyd JS, Blondon M, Moore KP, Boyko EJ, Smith NL. Validation of methods for assessing cardiovascular disease using electronic health data in a cohort of Veterans with diabetes. Pharmacoepidemiol Drug Saf. 2016;25(4):467–471. doi: 10.1002/pds.3921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Agency for Healthcare Research and Quality. Clinical Classifications Software (CCS) for ICD-9-CM. [Accessed November 30, 2016];Healthcare Cost and Utilization Project web site. 2016 Oct 7; Available at: https://www.hcup-us.ahrq.gov/toolssoftware/ccs/ccs.jsp.
- 31.Austin SR, Wong YN, Uzzo RG, Beck JR, Egleston BL. Why Summary Comorbidity Measures Such As the Charlson Comorbidity Index and Elixhauser Score Work. Med Care. 2015;53(9):e65–72. doi: 10.1097/MLR.0b013e318297429c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Agency for Healthcare Research and Quality. HCUP Elixhauser Comorbidity Software. Healthcare Cost and Utilization Project (HCUP) [Accessed November 30, 2016];Healthcare Cost and Utilization Project web site. 2016 Oct 6; Available at: https://www.hcup-us.ahrq.gov/toolssoftware/comorbidity/comorbidity.jsp.
- 33.Foster DG, Barar R, Gould H, Gomez I, Nguyen D, Biggs MA. Projections and opinions from 100 experts in long-acting reversible contraception. Contraception. 2015;92(6):543–552. doi: 10.1016/j.contraception.2015.10.003. [DOI] [PubMed] [Google Scholar]
- 34.O’Toole TP, Johnson EE, Borgia ML, et al. Tailoring Outreach Efforts to Increase Primary Care Use Among Homeless Veterans: Results of a Randomized Controlled Trial. J Gen Intern Med. 2015;30:886–98. doi: 10.1007/s11606-015-3193-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.O’Toole TP, Johnson EE, Aiello R, et al. Tailoring Care to Vulnerable Populations by Incorporating Social Determinants of Health: the Veterans Health Administration’s “Homeless Patient Aligned Care Team” Program. Prev Chronic Dis. 2016;13:E44. doi: 10.5888/pcd13.150567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.O’Toole TP, Buckel L, Redihan S, et al. Staying healthy during hard times: the impact of economic distress on accessing care and chronic disease management. Med Health R I. 2012;95:363–6. [PubMed] [Google Scholar]
- 37.U.S. Department of Veterans Affairs. Study of Barriers for Women Veterans to VA Health Care. [Accessed November 30, 2016];Women Veterans Health Care web site. 2015 Apr; Available at: http://www.womenshealth.va.gov/WOMENSHEALTH/index.asp.
- 38.Ramondetta LM, Meyer LA, Schmeler KM, et al. Avoidable tragedies: Disparities in healthcare access among medically underserved women diagnosed with cervical cancer. Gynecol Oncol. 2015;139:500–5. doi: 10.1016/j.ygyno.2015.10.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.American College of Obstetricians and Gynecologists Committee Opinion No. 586: Health Disparities in Rural Women. Obstet Gynecol. 2014;123:384–8. doi: 10.1097/01.AOG.0000443278.06393.d6. [DOI] [PubMed] [Google Scholar]
- 40.Owen CM, Goldstein EH, Clayton JA, et al. Racial and ethnic health disparities in reproductive medicine: an evidence-based overview. Semin Reprod Med. 2013;31:317–24. doi: 10.1055/s-0033-1348889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Seelig MD, Yano EM, Bean-Mayberry B, et al. Availability of gynecologic services in the department of veterans affairs. Womens Health Issues. 2008;18:167–73. doi: 10.1016/j.whi.2007.12.006. [DOI] [PubMed] [Google Scholar]