Abstract
Expanding access through insurance expansion can increase healthcare utilization through moral hazard. Reforming provider incentives to introduce more supply-side cost sharing is increasingly viewed as crucial for affordable, sustainable access. Using both difference-in-differences and segmented regression analyses on a panel of 1,466 hypertensive and diabetic patients, we empirically examine Shandong province’s initial implementation of China’s 2009 Essential Medications List policy. The policy reduced drug sale markups to providers but also increased drug coverage benefits for patients. We find that providers appeared to compensate for lost drug revenues by increasing office visits, for which no fee reduction occurred. At the same time, physician agency (yielding to patient demand for pharmaceuticals) may have tempered provider incentives to reduce drug expenditures at the visit level. Taken together, the policy may have increased total spending or total out-of-pocket expenditures. Mandating payment reductions in a service that comprises a large portion of provider income may have unintended consequences.
Introduction
In 2009, China grappled with chronic challenges to healthcare access by implementing extensive reforms. The Central Communist Party and the State Council of the People’s Republic of China announced a program through their “Opinions on Deepening Pharmaceutical and Healthcare System Reform.”1 This decision initiated a host of policy instruments, draft rules and guidances, and set a new course for the organization and delivery of China’s healthcare services.
The healthcare reforms aimed primarily to address the longstanding problem of the two nations’ uninsured and under-insured populations. Yet ensuring access to essential medical services without encouraging overutilization of healthcare resources is a perennial challenge for policymakers worldwide. In the United States, for example, the Affordable Care Act seeks to contain cost while expanding access through a number of mechanisms such managed competition, payment incentives, excise taxes on high-cost plans, as well as medical homes and accountable care organizations. Likewise, China’s reforms aim to improve insurance coverage to reduce patient out-of-pocket burden, while constraining costs by incentivizing provider efficiency. If, for example, lower copayments improve adherence to recommended therapy (as in the case of patients with chronic disease faithfully taking their medications), it may also promote welfare gains by improving both risk protection and health outcomes.
However, both economic theory and previous empirical evidence suggest that implementation of a demand-side reform – such as expanding insurance or reducing patient co-payment burden for specific medications – can be complicated by a strategic supply-side response. Yet the related theory does not account for the effects on provider income (e.g. Ellis and McGuire 1993; Ma and McGuire 1997; Eggleston 2005), which can be large for primary care providers when payment for basic services changes. Furthermore, studies of these effects in developing countries are limited. This paper aims to provide an empirical analysis of the interaction of demand- and supply-side effects of Shandong Province’s initial implementation of China’s 2010 Essential Medications List – one of the four pillars of China’s 2009 healthcare reforms – which reduced providers’ margins from drug dispensing while increasing prescription drug insurance coverage for patients. The Essential Medications List policy has continued relevance today, as China remains in the process of rolling out the policy to public providers across the nation in 2016.
Empirical Case Study: The Essential Medications List in China
Prescribing and Dispensing in China
Physician dispensing and provider reliance on revenue from drug sales have deep historical and cultural roots in East Asia (Eggleston 2011). Physicians’ and hospitals’ practice of supporting themselves financially through drug sales (known as “yi yao yang yi” in Chinese)—with allowed mark-ups of 15% or more—is widely decried by the Minister of Health, and is the explicit target of China’s 2010 Essential Medication List (EML) reforms.
China’s long-term EML policy goals include several components. First, the policy required government-owned primary care organizations to implement a zero mark-up policy for dispensing drugs to their patients, and they were prohibited from dispensing drugs not included in the EML. We call this supply-side EML (SEML), although the reduction in mark-up also constitutes a reduction in price for consumers. Most local governments allowed providers a transition period in which they could continue to dispense non-EML drugs and retain some drug dispensing revenue. In the county subject to SEML that we study, for example, this transition period extended from March through June 2010, after which government primary care organizations may no longer charge a mark-up for EML drugs or dispense non-EML drugs.
Another component required more generous insurance coverage for EML drugs than non-EML drugs; we call this demand-side EML (DEML). This component of EML involved changing the benefits package of social insurance, and the timing of its implementation generally differed from SEML. In the counties we study, we designate the county that implemented SEML in June 2010 as the “Treatment County,” and the county in which SEML was not implemented as the “Control County.”2 However, provincial-level DEML took force at the beginning of 2011 in both counties as part of the annual insurance package updates for rural health insurance (the New Cooperative Medical Scheme, or “NCMS”), six months after SEML was implemented.
SEML and DEML, as outlined above, were the only two EML components that were implemented in the Treatment County (both SEML and DEML) and in the Control County (DEML only). The national EML policy also set guiding retail prices and called for provincial-level bidding for medications on the list. This may have the potential to reduce the price of EML drugs by changing the organization of the drug market. However, our study examines the first wave of Shandong’s EML policy in its initial years, so that many related policies were not yet in place. The provincial-level bidding for medications, for example, was not implemented in Shandong until August, 2011, near the end of our study period.3 In fact, Shandong’s EML policy itself expanded to 80% of the province’s prefecture in 2011,4 and covered all public providers in Shandong fully only in 2016.5 No other payment changes to government primary care organizations or subsidies occurred during the first wave of the EML program.6,7 Our empirical context thus provides an excellent framework to better study the effects of the zero mark-up policy and restriction against non-EML drugs (SEML), later combined with greater insurance benefits under DEML.
Previous Literature
Scholars have investigated the effects of EML with mixed results regarding its impact on drug prices, healthcare utilization, and patient out-of-pocket burden. Previous studies have confirmed that provider financial incentives substantially influence treatment recommendations in China. An audit study of student-simulated patients found that Chinese hospital-based physicians dramatically reduced (and in some cases, completely eliminated) prescriptions of antibiotics when the financial incentive was removed (Currie, Lin and Meng, 2014).
Several studies showed that instead of increasing utilization in primary care after EML, many patients with more complicated conditions ironically received care at higher-cost hospitals (Yang et al., 2012; Wang et al., 2012; Ye et al. 2011; Sun et al., 2011; Li et al., 2012; Sun et al., 2012; Tian et al., 2012). A possible interpretation is that without profitable drug dispensing, clinics no longer desired to treat higher-cost, more severely ill patients, and referred them to county hospitals instead.
The evidence is limited, however, by several challenges of the study designs. Many analyses compared pre-EML and post-EML trends without a comparison group, and few distinguished supply-side and demand-side impacts. In addition, no study to date has linked patient-level spending to clinical data for both an intervention and comparison group, as we do.
Conceptual Framework
This section describes a simple model of how demand- and supply-side incentives interact to influence physicians’ choice of the quantity of services to recommend to patients. The model, developed more fully in the Technical Appendix, builds upon the pioneering work of McGuire and Pauly (1991) on physician responses to fee changes, and adds a framework to analyze how demand-side incentives interact with supply-side incentives. In the Technical Appendix, we replicate their theoretical predictions with a model that controls inducement through physician agency for patients, rather than the disutility of inducement that McGuire and Pauly themselves call a “somewhat peculiar utility function.”8 We then add a demand-side component and analyze the interaction of demand- and supply-side incentives in a general context, before making specific predictions based on our empirical case. We use these predictions to study the impact of China’s EML policy with unique patient-level data from Shandong, one of China’s most populous provinces.
The EML policy as implemented in Shandong’s initial program that we study contains both a supply- and a demand-side component. On the supply side, the policy requires government-owned primary care providers (known as “township health centers,” or THC) to dispense only essential medications with zero price mark-up. Prior to the policy, most health clinics derived about half of their revenues from dispensing medications directly to their patients; thus, the requirement of zero mark-up potentially entails large income effects.
Although physicians at township health centers are government employees, in Shandong they are not paid a fixed salary. Their compensation structure is determined at the provincial level by the provincial government, and is based in part on their financial performance.9 Nationwide, public hospitals only receive 6–7% of their budget from the government, and must rely on income from operations for over 90% of their budget.10 As a result, drug price markups and fee for service represent common avenues for hospitals to maximize profit, and physician compensation at public providers is intimately linked to the profitability of their institutions. Thus, the income effect of the zero mark-up policy is likely to have a large impact on physician income at township health centers, especially when the government did not initially increase reimbursement when it implemented SEML.11
The demand side of the policy requires China’s social health insurance programs to provide more coverage for medications. In the section below, we summarize the testable hypotheses generated from the model, which we take to data using Shandong’s initial implementation of China’s EML policy as our empirical study context.
Our theoretical model suggests that the impact of reducing provider’s margin for a specific service, like medication prescribing, could have an ambiguous impact on utilization:
For the service for which the fee has decreased (i.e., drugs), a reduction of the margin to 0 should entail a reduction in drug utilization because no volume-offset behavior can increase supplier profit. However, physician agency may temper this reduction (that is, physicians no longer derive economic benefit from drug prescription, but it “costs nothing” to yield to patient demand for prescription drugs). When we take demand-side incentives into consideration, patients’ desire to increase drug prescription with better insurance coverage could theoretically be offset by supply-side constraint. In the end, with multiple, sometimes conflicting forces at work, the change in prescription drug utilization following China’s EML zero mark-up policy and insurance expansion is an empirical question.
For the second service for which the fee has not been reduced (e.g., office visits), the zero mark-up policy for drugs will lead physicians to increase office visits to compensate for lost revenues from drug sales (given large provider income effects). However, patients may resist additional trips to the physician’s office because of inconvenience or concerns regarding medical or travel costs. Thus, the relative strength of the zero mark-up policy and patient resistance will together affect office visit utilization in the post-intervention period.
Materials and Methods
Data
This study uses patient-level clinical and spending data for 1,466 patients with chronic disease—hypertension and/or diabetes mellitus—treated at rural THCs in two counties in Shandong province, China.12 The two rural counties of Shandong were chosen for this study based on the ability to obtain a random sample of patients who received care in both the pre- and post-EML periods, with NCMS insurance claims and provider clinical records. The Treatment County implemented the zero mark-up policy (SEML) in June 2010, after a three-month transition period. The Control County is a matched comparison that did not implement SEML during the study period. Both are similar in terms of socioeconomic characteristics (see Chen and Eggleston 2013).
In each county, we collected clinical information from patients at twelve THCs, which are all government-owned and managed, as are the vast majority of China’s primary care providers in both urban and rural areas (except village clinics). From each THC, we selected the first 45 hypertensive and first 20 diabetic patients by visit sequence in January 2009, as identified by the presence of an ICD9 code for the respective diseases (401 for hypertension, and 250 for diabetes), who had at least one visit before and after June 2010, in order to ensure a panel of at least two observations per patient. This process yielded an initial cohort of 1,560 patients.
To account for clear coding errors and large outliers, all clinical outcome variables were trimmed to the 95% percentile and observations with incomplete information were discarded. Our final sample includes 1,466 patients, after merging the cohort with their claims from the NCMS claims data: 1,030 with a primary diagnosis of hypertension and 436 with a primary diagnosis of diabetes mellitus, with a combined total of 25,350 office or hospital visits. About a third of the patients with each diagnosis are from the Treatment County (312 hypertension patients and 149 diabetes patients). Table 1 provides the summary statistics for the data as a whole as well as by county, at the patient-, visit- and month-level.
Table 1.
Summary Statistics
| Variable | Both Counties | Treatment County | Control County | |||
|---|---|---|---|---|---|---|
|
|
|
|||||
| Mean | Std. Dev. | Mean | Std. Dev. | Mean | Std. Dev. | |
| A. Patient-level data | N = 1,466 | N = 811 | N = 655 | |||
| Age | 56.61 | 16.69 | 56.66 | 16.88 | 56.54 | 16.47 |
| Male | 0.44 | 0.53 | 0.60 | |||
| Education | ||||||
| Primary school | 0.66 | 0.72 | 0.58 | |||
| Junior high | 0.28 | 0.21 | 0.36 | |||
| High school | 0.04 | 0.04 | 0.04 | |||
| ≥ Vocational school | 0.00 | 0.00 | 0.01 | |||
| Missing | 0.02 | 0.03 | 0.01 | |||
| Occupation | ||||||
| Farmer | 0.98 | 0.99 | 0.98 | |||
| Other | 0.02 | 0.01 | 0.02 | |||
| Primary diagnosis | ||||||
| Diabetes | 0.30 | 0.29 | 0.30 | |||
| Hypertension | 0.70 | 0.71 | 0.7 | |||
| Number of visits | ||||||
| Total visits | 17.48 | 14.21 | 16.45 | 14.54 | 18.77 | 13.69 |
| pre-SEML visits | 8.12 | 8.09 | 5.71 | 6.73 | 6.61 | 6.63 |
| post-SEML visits | 9.37 | 8.10 | 10.73 | 9.71 | 12.15 | 9.13 |
| pre-DEML visits | 12.09 | 10.75 | 11.86 | 11.34 | 12.35 | 9.96 |
| post-DEML visits | 5.40 | 5.21 | 4.59 | 4.89 | 6.42 | 5.42 |
| Clinical | ||||||
| First systolic | 147.07 | 17.17 | 146.35 | 17.56 | 147.92 | 16.67 |
| Last systolic | 143.02 | 16.25 | 144.84 | 17.28 | 140.87 | 14.67 |
| First diastolic | 91.57 | 10.46 | 90.64 | 10.28 | 92.66 | 10.56 |
| Last diastolic | 89.25 | 9.86 | 90.03 | 10.18 | 88.33 | 9.40 |
| First fasting glucose | 7.86 | 2.71 | 7.47 | 1.86 | 8.23 | 3.27 |
| Last fasting glucose | 7.59 | 2.55 | 7.40 | 1.90 | 7.77 | 3.03 |
| B. Visit-level data | N=25,630 | N=13,338 | N=12,292 | |||
| Total expenditures | 211.87 | 1787.65 | 216.53 | 2050.73 | 206.82 | 1449.20 |
| Total copay | 123.73 | 1206.40 | 125.77 | 1456.55 | 121.51 | 855.98 |
| Drug expenditures | 144.79 | 842.64 | 144.79 | 842.64 | ||
| Drug copay | 83.56 | 516.63 | 83.56 | 516.63 | ||
| C. Month-level data | N=14,558 | N=7,476 | N=7,082 | |||
| Total expenditures | 373.01 | 2415.26 | 386.31 | 2799.29 | 358.97 | 1928.73 |
| Total copay | 217.83 | 1623.70 | 224.38 | 1976.58 | 210.91 | 1138.20 |
| Total drug expenditures | 246.29 | 1117.94 | 246.29 | 1117.94 | ||
| Total drug copay | 142.13 | 685.14 | 142.13 | 685.14 | ||
Patients in the Control County are mostly male, and slightly better educated than patients in the Treatment County. Control County patients also spend less on medical care than patients in the Treatment County at baseline. Although these two counties cannot be considered representative of rural China as a whole, they are reasonably representative of Shandong, which is itself close to the national average in per capita income. Records show, on average, 17.48 visits per patient during the 33 months covered by the study. Mean medical expenditures per month were 373 RMB (approximately USD $60; SD=2,415 RMB), and mean out-of-pocket expenditures were 217 RMB (SD=1,623 RMB).13
As shown in Table 1, the average systolic blood pressure (SBP) and diastolic blood pressure (DBP) prior to and after the policy change are, respectively, 147.07/91.57 and 143.02/89.25. The fasting glucose levels are, respectively, 7.86 and 7.59 before and after implementation of EML.
For our regression analyses, we use either visit-level data or aggregate spending by patient-month, and investigate only healthcare utilization at THCs to focus on the strategic response of THC providers. For the visit-level data, we have a total of 8,791 individual encounters, and for the monthly data, we have a total of 4,921 patient-month observations for visits to THCs.
This research was approved by the Institutional Review Board at Stanford University.
Empirical specifications
To focus our analysis on the behavior of THCs subject to the Shandong pilot EML program, we keep only claims from THCs in all analyses to follow. We use a general difference-in-difference regression specification, a commonly used method that subtracts the difference in the post- and pre-intervention outcomes for the control group from the difference in the post- and pre-intervention outcomes for the treatment group. This quasi-experimental approach has the following form:
| (8a) |
Or
| (8b) |
For specifications in which we aggregate the outcome variable at the month level (such as number of visits per month or log total expenditures per month), t represents month and the time fixed effects are estimated at the quarter level. For the visit-level analyses, t represents the date of visit, and the time fixed effects are estimated at the month level. Here, αi is individual patient fixed effects, inpatit is a dummy variable indicating if patients i was hospitalized during month or date t, municipal hospit represents a visit to the higher level municipal during month or date t, and εit signifies the idiosyncratic errors.
Post SEMLt and Post DEMLt are categorical variables set to 1 in the periods (t) after SEML and DEML were implemented. The interaction variable treatedSEMLit is equal to 1 for all patients i in the Treatment County for all dates after SEML was implemented (March 2010), and treatedDEMLit equals 1 for all patients i in the Treatment County for all dates after DEML was implemented (January 2011). The coefficient β2 in equation 8a and 8b respectively represent (ypostSEML,treated – ypreSEML,treated ) – (ypostSEML,control –ypreSEML,control) and (ypostDEML,treated – ypreDEML,treated) – (ypostDEML,control – ypreDEML,control).
We used both the SEML ramp-up (March 2010) and the SEML implementation (June 2010) dates as the treated SEML dummy in separate specifications, but report only the results from using March 2010 (ramp-up) after noting that effects are observed as soon as then. We note that the DID estimates for treatedDEML cannot be interpreted as the impact of DEML relative to the counterfactual of no DEML. Instead, we interpret the coefficient on treatedDEML as the DID estimate of DEML+SEML relative to DEML alone.
To the extent that outcomes diverge in the Treatment and Control Counties in the post-SEML period, the lack of pre-DEML parallel trends may confound the interpretation of the coefficients on treatedDEML. To account for this possibility, we drop all SEML-period data (March 1 to January 1, 2011) in the DEML specification, such that the pre-period is the period before March 1, 2010, and the post-DEML period is the period on and after January 1, 2011.
To ascertain that the Control County represents a plausible counterfactual for the Treatment County, we perform a Heckman-Hotz test of equality of pre-intervention trends in the outcome variables. We do so by dropping all post-SEML observations, and by regressing the outcome variables on quarter dummies, the interaction of quarter dummies and a categorical variable equal to 1 for the Treatment County, as well as other covariates used in the models above. If we find that these interaction terms are not different from 0, we may conclude that the pre-intervention trends in the outcomes between the two counties are similar, increasing the likelihood that the Control County may serve as a good counterfactual for what would have happened in the Treatment County had it not been subject to the intervention.
Because we were unable to obtain drug utilization data for the Control County, our DID approach only captures total expenditures. This specification, however, cannot detect any potential substitution effect (such as reducing drug expenditures but increasing laboratory expenditures). To test for this possibility, we use segmented regression analyses to examine the potential impact of the policy intervention on trends in pharmaceutical spending (total and out-of-pocket) using data from the Treatment County, for which we have drug utilization data.
In order to account for the sequential structure of the policy implementation, we divide the study period into four segments: (1) pre-SEML “ramp up” (SEML implemented but not yet enforced--January 2009 to February 2010); (2) post-SEML “ramp-up” – March 2010 to May 2010; (3) post-SEML – June 2010 to December 2010, and (4) post-DEML – January 2011 to June 2011. For the segmented regression specifications, periods 1–2 and 2–3 are intended to capture SEML effects (with period 1–2 serving as an additional check to investigate whether the SEML grace period had any impact of its own). Period 3–4 captures the additional impact of DEML after the implementation of SEML.
The segmented regression analyses follow the standard specification to identify breaks and changes in slopes following each intervention, as follows:
| (9) |
In the specification above, the variable quarters is a counter that starts at 1 at the beginning of the study period (Quarter 1, 2009) and advances by 1 for each passing quarter. Post ramp up, post SEML, and post DEML are categorical variables set to 1 for all visits after March 2010, June 2010, and January 2011, respectively. Quarters since ramp-up, SEML and DEML start new counters in Quarter 1, 2010, Quarter 3, 2010, and Quarter 1, 2011, respectively. The coefficient β1 indicates the slope of the pre-intervention trend starting in Quarter 1, 2009. The coefficients β3, β5, and β7 estimate the change in slope following the ramp-up period, SEML, and DEML relative to the slope of the period immediately before each intervention. In this segmented regression specification, β2, β4, and β6 represent the discontinuous breaks at the beginning of the ramp-up/grace period, SEML, and DEML, respectively. All other variables are as defined in the DID specification.
For all specifications, we report the Huber-White standard errors robust to heteroskedasticity in the error term.
Results
Difference-in-Difference Results
We did not detect any changes in total healthcare expenditures at the visit level (See Table 2, Panel I), possibly because physician agency tempered the quantity-reducing effect of a fee reduction (the zero mark-up policy, or SEML). However, we found evidence that there was inducement in the second service (office visits), given that total monthly expenditures increased at SEML providers relative to control providers (by approximately 30.4% (p<0.05), post-SEML×treat) for hypertensive patients (Table 2, Panel II). When we drop the data from the SEML implementation period (March, 2010 to January, 2011), we see that after DEML, SEML providers also subject to DEML increased total monthly expenditures more so than providers subject to DEML alone (especially for patients with hypertension, by 28.5%, p<0.1 only). (See Table 2, Panel II, specification (5), coefficients on post-DEML×treat).
Table 2.
Difference-in-Differences Estimates of EML Impact on Expenditures and Visits at Township Health Centers
| VARIABLES | (1) | (2) | (3) | (4) | (5) | (6) |
|---|---|---|---|---|---|---|
| Log total/month (post SEML) | Log total/month (post DEML) | |||||
|
|
|
|||||
| All | Hypertension | Diabetes | All | Hypertension | Diabetes | |
| I. Log Total Expenditures/Visit (THCs Only) | ||||||
| post-SEML | 0.0846 (0.110) | 0.118 (0.126) | −0.0207 (0.212) | |||
| post-SEML X treat | 0.0183 (0.0645) | 0.0666 (0.0751) | −0.0656 (0.124) | |||
| post-DEML | 0.0383 (0.123) | 0.0346 (0.141) | 0.100 (0.311) | |||
| post-DEML X treat | −0.0408 (0.0834) | −0.00961 (0.105) | −0.123 (0.138) | |||
| Inpatient admission | 5.362*** (0.286) | 5.740*** (0.432) | 4.930*** (0.336) | 5.818*** (0.229) | 5.943*** (0.265) | 5.545*** (0.409) |
| Constant | 2.927*** (0.0785) | 2.823*** (0.0844) | 3.184*** (0.166) | 2.910*** (0.0796) | 2.830*** (0.0855) | 3.103*** (0.167) |
| Observations | 8,791 | 6,294 | 2,497 | 7,910 | 5,623 | 2,287 |
| R-squared | 0.09 | 0.08 | 0.14 | 0.11 | 0.11 | 0.14 |
| Number of patients | 794 | 557 | 237 | 780 | 543 | 237 |
| II. Log Total Expenditures/Month (THCs Only) | ||||||
| Post-SEML ramp-up | −0.0930 (0.142) | −0.254 (0.171) | 0.344 (0.248) | |||
| Post-SEML X treat | 0.205* (0.108) | 0.304** (0.132) | −0.0577 (0.180) | |||
| Post-DEML | −0.237** (0.119) | −0.322*** (0.122) | 0.447* (0.244) | |||
| Post-DEML X treat | 0.246** (0.124) | 0.285* (0.162) | 0.142 (0.199) | |||
| Inpatient admission | 1.226*** (0.281) | 0.945*** (0.342) | 1.793*** (0.460) | 1.294*** (0.257) | 1.114*** (0.299) | 1.745*** (0.511) |
| Municipal hospital | 0.159** (0.0748) | 0.205** (0.0997) | 0.122 (0.112) | 0.128 (0.0889) | 0.153 (0.120) | 0.112 (0.131) |
| Constant | 3.303*** (0.0550) | 3.191*** (0.0640) | 3.583*** (0.102) | 3.337*** (0.0550) | 3.231*** (0.0640) | 3.596*** (0.105) |
| Observations | 4,921 | 3,492 | 1,429 | 4,239 | 2,984 | 1,255 |
| R-squared | 0.04 | 0.03 | 0.07 | 0.06 | 0.06 | 0.08 |
| Number of patients | 794 | 557 | 237 | 780 | 543 | 237 |
| III. Total Number of Visits/Month (THCs Only) | ||||||
| Post-SEML ramp-up | −0.0965 (0.0833) | −0.136 (0.106) | −0.00483 (0.130) | |||
| Post-SEML X treat | 0.186*** (0.0630) | 0.189** (0.0826) | 0.176** (0.0884) | |||
| Post-DEML | −0.368*** (0.0794) | −0.385*** (0.101) | −0.463*** (0.115) | |||
| Post-DEML X treat | 0.388*** (0.0745) | 0.383*** (0.0957) | 0.402*** (0.113) | |||
| Inpatient admission | −0.111* (0.0654) | −0.144 (0.0940) | −0.0533 (0.0777) | −0.132** (0.0559) | −0.162** (0.0740) | −0.0722 (0.0785) |
| Municipal hospital | −1.087*** (0.0441) | −1.105*** (0.0615) | −1.053*** (0.0585) | −1.114*** (0.0435) | −1.126*** (0.0556) | −1.090*** (0.0690) |
| Constant | 1.803*** (0.0548) | 1.826*** (0.0721) | 1.750*** (0.0755) | 1.820*** (0.0547) | 1.839*** (0.0711) | 1.778*** (0.0783) |
| Observations | 9,962 | 6,826 | 3,136 | 9,621 | 6,600 | 3,021 |
| R-squared | 0.09 | 0.08 | 0.12 | 0.11 | 0.10 | 0.13 |
| Number of patients | 1,372 | 961 | 411 | 1,426 | 1,000 | 426 |
Robust standard errors in parentheses
p<0.01,
p<0.05,
p<0.1
Consistent with the prediction that a reduction in drug fees could lead to more office visits, in Table 2 Panel III, we demonstrate that the mechanism through which expenditures increased post-SEML at the aggregate monthly level likely resulted from an increase in per-month number of visits. Panel III results show that the number of visits per month increased by 0.189 (hypertension, p<0.05) and 0.176 (diabetes, p<0.05) after SEML. Thus, in our empirical context, inducement did not occur by increasing total expenditures (a proxy for service 1, drug expenditures) per visit, but by increasing the average total number of visits per month (service 2).
Results of the Heckman-Hotz test are reported in Appendix Table 1 for the pre-intervention trends in total expenditures. All of the interaction terms are not statistically different from 0, and the F tests fail to reject that the interaction terms are jointly 0. These tests generally support that our Control County is a reasonably good counterfactual for the Treatment County in monthly total expenditures for the difference-in-differences model.
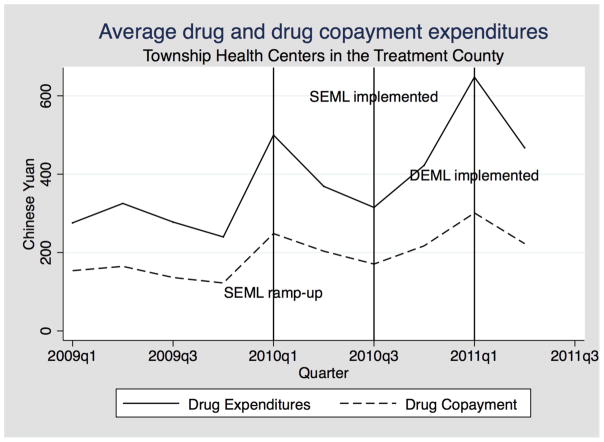
Figure 1 shows that pharmaceutical spending appears to spike when SEML was first implemented in the Treatment County (between March and June 2010). One explanation for this is providers may have been eager to sell off inventory of non-EML drugs before the June 2010 deadline for selling only EML drugs. This spending “spike,” conceptually similar to the “Ashenfelter dip” found prior to job training programs, is important to recognize when evaluating the impact of the program on prescribing behavior and patient utilization.
Figure 1. Spike in average drug expenditures per patient quarter before supply-side EML.
Note: The upper line represents average pharmaceutical expenditures per patient quarter; the lower line represents average out-of-pocket spending on pharmaceuticals per patient quarter. The first vertical line represents the SEML (“zero mark-up”) policy ramp-up period. The second represents the implementation of supply-side EML, SEML (“zero mark-up”), in June 2010. The third vertical line shows implementation of improved insurance coverage with demand-side EML (DEML).
Segmented Regression Results
In this section we report results from our segmented regression analyses for the Treatment County (for which we have drug expenditure data) to see whether the changes in total expenditures identified in the DID estimates can be corroborated using drug expenditures. The results in Table 3 (Panel I) reveal an interesting pattern of expenditures. For all diagnoses in the quarter that SEML was implemented but not enforced (the “ramp-up” period), there was an increase in monthly drug expenditures (88.6%, p<0.01), followed by a downward bend in slope (−38.7%, p<0.01) in the post-SEML ramp-up period. This “spike” is consistent with the Ashenfelter-dip explanation, as providers dispensed their drug inventory in preparation of the enforcement of SEML. Upon official implementation of SEML, there was another increase in the slope post-SEML (66.6%, p<0.01). This increase in monthly drug expenditures post-SEML suggests that the DID estimates, which uses monthly total expenditures, indeed captured an increase in monthly drug expenditures (rather than merely the non-drug component of total expenditures).
Table 3.
Segmented Regression Analysis, Impact of SEML and DEML on Expenditures and Visits
| SAMPLE | (1) | (2) | (3) | (4) | (5) | (6) |
|---|---|---|---|---|---|---|
| All | Hypertension | Diabetes | All | Hypertension | Diabetes | |
| I. Expenditures/Month | Log drug expenditures/month | Log drug out-of-pocket/month | ||||
| Quarter counter | −0.0843*** (0.0255) | −0.0691** (0.0297) | −0.124** (0.0499) | −0.0847*** (0.0255) | −0.0693** (0.0296) | −0.126** (0.0499) |
| Post-SEML ramp-up | 0.886*** (0.159) | 0.885*** (0.199) | 0.914*** (0.255) | 0.885*** (0.159) | 0.884*** (0.198) | 0.913*** (0.255) |
| Quarters since SEML ramp-up | −0.387*** (0.0986) | −0.425*** (0.119) | −0.311* (0.175) | −0.386*** (0.0984) | −0.424*** (0.118) | −0.310* (0.175) |
| Post-SEML | 0.116 (0.0974) | 0.165 (0.112) | 0.0234 (0.194) | 0.116 (0.0973) | 0.165 (0.112) | 0.0237 (0.194) |
| Quarters since SEML | 0.666*** (0.110) | 0.703*** (0.133) | 0.589*** (0.197) | 0.666*** (0.110) | 0.703*** (0.133) | 0.590*** (0.197) |
| Post-DEML | −0.0568 (0.586) | −0.512 (0.725) | 1.115 (0.875) | −0.113 (0.574) | −0.569 (0.710) | 1.060 (0.854) |
| Quarters since DEML | −0.161 (0.301) | 0.0453 (0.370) | −0.684 (0.470) | −0.133 (0.296) | 0.0734 (0.363) | −0.657 (0.460) |
| Inpatient admission | 1.461*** (0.249) | 1.202*** (0.292) | 2.152*** (0.472) | 1.431*** (0.246) | 1.172*** (0.287) | 2.120*** (0.467) |
| Municipal hospital | 0.103 (0.0825) | 0.137 (0.110) | 0.0739 (0.124) | 0.103 (0.0825) | 0.137 (0.110) | 0.0729 (0.125) |
| Constant | 3.334*** (0.0745) | 3.235*** (0.0886) | 3.586*** (0.136) | 2.979*** (0.0745) | 2.879*** (0.0885) | 3.233*** (0.136) |
| Observations | 4,962 | 3,549 | 1,413 | 4,962 | 3,549 | 1,413 |
| R-squared | 0.07 | 0.07 | 0.10 | 0.07 | 0.06 | 0.09 |
| Number of patients | 714 | 505 | 209 | 714 | 505 | 209 |
| II. Visits/Month | Visits/month | Log number of visits/month | ||||
| Quarter counter | −0.00843 (0.0278) | 0.00767 (0.0351) | −0.0439 (0.0439) | −0.00105 (0.0114) | 0.00955 (0.0132) | −0.0293 (0.0222) |
| Post-SEML ramp-up | 0.127 (0.108) | 0.0917 (0.135) | 0.209 (0.176) | 0.0565 (0.0542) | 0.0362 (0.0645) | 0.107 (0.100) |
| Quarters since SEML ramp-up | −0.0732 (0.0805) | −0.0799 (0.102) | −0.0600 (0.127) | −0.0359 (0.0367) | −0.0328 (0.0442) | −0.0391 (0.0658) |
| Post-SEML | −0.0708 (0.0747) | −0.117 (0.0949) | 0.0368 (0.116) | −0.0207 (0.0351) | −0.0313 (0.0432) | 0.00228 (0.0587) |
| Quarters since SEML | 0.198** (0.0792) | 0.220** (0.101) | 0.147 (0.122) | 0.0975** (0.0391) | 0.0872* (0.0478) | 0.119* (0.0661) |
| Post-DEML | 0.347*** (0.114) | 0.331** (0.147) | 0.388** (0.173) | 0.145*** (0.0512) | 0.140** (0.0645) | 0.156* (0.0806) |
| Quarters since DEML | −0.343*** (0.0820) | −0.369*** (0.105) | −0.284** (0.124) | −0.151*** (0.0376) | −0.150*** (0.0459) | −0.149** (0.0654) |
| Inpatient admission | −0.117* (0.0695) | −0.129 (0.0885) | −0.0825 (0.105) | 0.0320 (0.0583) | 0.0110 (0.0721) | 0.0468 (0.103) |
| Municipal hospital | −0.967*** (0.0484) | −0.975*** (0.0660) | −0.955*** (0.0708) | 0.0255 (0.0310) | 0.0554 (0.0417) | −0.0141 (0.0459) |
| Constant | 1.685*** (0.0810) | 1.674*** (0.0992) | 1.710*** (0.141) | 0.358*** (0.0333) | 0.323*** (0.0375) | 0.453*** (0.0673) |
| Observations | 7,476 | 5,157 | 2,319 | 5,815 | 4,132 | 1,683 |
| R-squared | 0.07 | 0.06 | 0.10 | 0.01 | 0.01 | 0.01 |
| Number of patients | 811 | 572 | 239 | 733 | 515 | 218 |
Robust standard errors in parentheses
p<0.01,
p<0.05,
p<0.1
In Table 3 Panel II, we present results that corroborate the DID estimates of changes in monthly visits. Following SEML enforcement, the slope for number of physician visits increased by 0.22 (p<0.05) for hypertensive patients at the township health centers, representing an increase of approximately 8.72% (p<0.1 only) in per-month number of visits. The coefficient on quarters since SEML for diabetic patients is positive but not statistically significant.
Clinical Outcomes
The model, consistent with much previous research, predicts that enhanced access from reduced co-payments may alleviate out-of-pocket burden. In turn, this may lead to improvements in health outcomes if there is better adherence to treatment regimens. An advantage of our data compared to all previous studies of EML in China is that we have patient-level clinical measures with which to study the association of clinical metrics with reduction of drug prices (SEML) and of co-payments (DEML).
At baseline, we find that these patients in rural China exhibit poor control of their chronic disease, highlighting the importance of improving chronic disease management (Table 1). The average measurements of SBP and DBP were above the clinical thresholds for diagnosis of hypertension (SBP ≥ 140 mmHg, DBP ≥ 88 mmHg) in both the pre- and post-periods, signifying uncontrolled hypertension. There was improvement in reported mean level of blood pressure control (Table 4), with a statistically significant improvement in systolic and diastolic scores in both counties (although the improvements in the Control County were greater than the Treatment County).
Table 4.
Impact of SEML on Health Outcomes
| VARIABLES | (1) | (2) | (3) |
|---|---|---|---|
| Log systolic | Log diastolic | Log Fast. Glucose | |
| post-SEML | −0.0510*** (0.00421) | −0.0467*** (0.00456) | −0.0747*** (0.0152) |
| post-SEML × treat | 0.0363*** (0.00630) | 0.0317*** (0.00682) | 0.0638*** (0.0195) |
| Constant | 5.011*** (0.00182) | 4.534*** (0.00196) | 2.152*** (0.00502) |
| Observations | 1,638 | 1,641 | 647 |
| R-squared | 0.20 | 0.15 | 0.11 |
| Number of patients | 968 | 970 | 378 |
Robust standard errors in parentheses
p<0.01,
p<0.05,
p<0.1
For diagnosed diabetes patients, fasting plasma glucose indicated relatively poor control of blood glucose levels (e.g. mean fasting glucose of 7.99 in the Treatment County and 10.03 in the Control County in the pre-period14), with a small improvement in the Control County and no significant improvement in the Treatment County.
In sum, our analyses show that SEML may have increased total expenditures and patient financial burden at township health centers, suggesting large income effects for physicians. While per-visit total expenditures may have remained relatively stable, patient office visits increased in township health centers in the SEML-treated county (particularly for hypertensive patients). One explanation for this finding is that physicians attempted to make up lost revenues because of the zero mark-up policy for drugs. Although clinical markers showed greater improvement in the non-SEML (Control) county (by approximately 3.17%, 3.63%, and 6.38% respectively for diastolic pressure, systolic pressure, and fasting glucose levels), the SEML-treated (Treatment) County also demonstrated some clinical improvement.
Discussion
Imperfect physician agency has long been considered a driver of escalating healthcare expenditures. Policymakers are justifiably concerned about the often-contradictory goals of increasing access through insurance coverage expansion and curtailing overutilization that does not improve health. We presented an empirical evaluation of temporally proximal supply-side and demand-side changes in incentives. Theoretically, a reduction in physician income from a service may cause providers to decrease the provision of that service, in the absence of income effects. However, physician agency may temper the reduction in a service (if such service improves patient health or if patients demand that service), which may in fact lead to quantity increases or offsets when fees to physicians are reduced. Moreover, a concurrent loosening of patient copayments may cause patients to demand more healthcare services. As a result, the total effect of the supply- and demand-side incentive changes may yield ambiguous results depending on the relative strengths of the income effects, physician agency, and demand-side incentives. Similarly, income effects, physician agency, and demand-side incentives may also shape physician and patient utilization of a complementary service in a theoretically ambiguous manner.
Taking this theoretical framework to data, we analyze the impact of Shandong’s initial implementation of China’s EML policy. On the one hand, the policy should theoretically reduce provider incentive to prescribe drugs by imposing a zero mark-up requirement on physician-dispensed pharmaceuticals at government-owned primary care providers. If the profits from drug mark-ups are indeed reduced to 0, volume off-setting behavior is unlikely. However, it is possible that the initial wave of the EML program may not have truly eliminated drug mark-ups, particularly in the early years of its implementation. Japan, for example, tackled its drug price markup problem for years before finally achieving success with a dynamic price control policy (Iizuka 2008). It is possible that even with the EML program, residual profits remained to encourage volume offsetting, consistent with the increases in drug expenditures that we found post-SEML in the Treatment County using segmented regression analysis. At the same time, physician agency is also likely important, as physicians have incentives to indulge patient demand for pharmaceuticals. It is therefore not surprising that studies find mixed results for physician fee changes. The empirical context is likely an important determinant of the ultimate impact of such policies.
Moreover, depending on the relative strengths of the supply-side and demand side incentives, income effects, and physician agency, utilization of a complementary service, such as office visits, could either increase or decrease after implementation of China’s EML policy. We found that, on net, the policy may have increased total spending or total out-of-pocket expenditures by increasing office visits. Instead of increasing average drug expenditures per visit alone, physicians appeared to have increased the total number of visits in order to compensate for lost drug profits through increased office visit registration fees. In China’s context, the supply-side incentives to increase office visits given the zero mark-up policy likely dominated other forces to hold visits in check.
As China continues to roll out its EML policy, the potential for increases in non-drug services is receiving much attention in the popular press. News reports also pointed out that removing drug price markups – a large source of provider income – without providing other sources of revenue will place increasing strain on the struggling primary care and hospital sectors in China.15,16 From this perspective, it is encouraging to note China’s commitment to address providers’ lost revenues from drug dispensing with concrete policies. The plan to compensate for lost revenues from drug sales is especially policy-relevant, as our results suggest that in its absence, physicians may increase other services and negate the expenditure-reducing intent of the EML policy.
We also found that at least in the short term, the EML policy did not improve observable patient health. While both Treatment (SEML and DEML) and Control (DEML only) Counties showed some improvement in clinical measures such as blood pressure and fasting glucose, the Control County actually showed greater improvement. This result suggests that, at the very best, increased visits (with the associated increases in patient expenditures) may not have been sufficient to improve health outcomes in the short term for patients in the Treatment County. Moreover, SEML may have restricted drug choice and/or changed physician reporting incentives in order to justify an increase in the number of office visits, but these small estimated changes in intermediate clinical measures such as blood pressure may not necessarily reflect important changes in health outcomes for patients.
Conclusion and Policy Implications
Six years after the Shandong EML pilot, China is still rolling out and refining its EML policy. Our work draws several conclusions that may have important health policy implications, both for China’s EML and for other types of fee-reducing policies. In a setting where healthcare providers rely heavily on revenues from one activity such as prescription drug dispensing, eliminating its margin may not necessarily reduce its expenditures. This is particularly true when supply-side incentives to overprescribe are supported by demand-side appetite for drug prescriptions. In this context, the traditional combination of supplier-side constraint and insurance generosity may not achieve the goal of assuring access while preventing potentially wasteful overuse. In addition, when a policy reduces a large portion of provider income, substitution into a second service for which fees have not changed may occur, perhaps even increasing total expenditures. China’s National Health and Family Planning Commission has emphasized the need to compensate providers for lost drug revenues through government assistance, adjustment to the prices of healthcare services and changes to reimbursement policy.17 Future work should investigate context-relevant policy proposals to combat China’s heavy reliance on pharmaceutical income and strong preference for prescription medications, which may not only lead to economic waste, but may also contribute to medical problems such as serious adverse events and the development of antibiotic resistant bacteria.
Although it may appear farfetched to apply our cautionary tale to other settings such as the American healthcare context, cost containment and reduced payments are common features in various health reforms. For example, the drive to reduce hospital readmissions (which represents a reduction in income), though unquestionably a laudable goal, may nevertheless potentially incentivize hospitals to increase other services either to attain this goal and/or to compensate for lost income. Theoretically, such a policy may also lead to hospitals cherry-picking healthier patients in order to reduce readmissions. Policymakers should consider the potential provider strategic responses to reductions in payment and weigh the overall costs and benefits.
Limitations and Bias
Our work has several limitations. First, our claims data only allow us to identify expenditures in yuan, not quantities or type (EML versus non-EML) of drugs dispensed. These variables related to quantities and use of EML drugs are important, because it is possible that at baseline, THCs may have and likely have already been using EML drugs, so SEML may have had a limited impact on the switching behavior of physicians from non-EML to EML drugs. This is not an unlikely scenario, given that the national and provincial governments attempted to place the most commonly prescribed hypertensive and diabetic medications on EML. Therefore, the coefficient on the treatedSEML variable may be capturing only a limited impact of SEML on health outcomes in particular if very little switching occurred. Using expenditures instead of quantities may in fact also underestimate possible increases in drug utilization if drug prices fell after SEML implementation. In this sense, our results may be biased downward and underestimate the increases in drug utilization following the adoption of EML.
Nevertheless, even without the variables on types and quantities of drugs dispensed, we can interpret the coefficient treatedSEML in our difference-in-differences estimations as the combined effect of switching to 100% EML prescriptions, price changes of EML drugs, and volume changes in EML drugs utilized on total expenditures in the treatment county, after subtracting common temporal changes in expenditures in the control county.
Second, we lack data on drug expenditures for our control. We have, however, tested the temporal trends in drug expenditures using segmented regression analysis and confirmed that increases in monthly drug expenditures occurred, consistent with the DID estimates using monthly total expenditures. Third, in terms of our sampling strategy, we would have liked to identify all hypertensive and diabetic patients at baseline (January 2009), mark those who also had at least one office visit for their primary diagnosis after SEML, and then randomly select the required cohort from such patients. However, to the extent that the order of patient visits in a given month follows a random process, it is likely we have generated a reasonably random sample of patients for our study cohort.
Fourth, the short time horizon of our study period does not allow us to investigate longer-term impact of China’s EML policy. This short study period is particularly evident in our clinical outcome regressions, which may not have been able to capture the true impact of EML on health. Finally, the clinical regressions further suffer from limitations because only one pre-SEML and one post-SEML observation were hand-collected from medical charts. Future work should consider more in-depth chart reviews and collection of drug prescription patterns, in terms of quantities and types of medications dispensed, as China continues refining its 2009 healthcare reform agenda.
Appendix Table 1.
Heckman-Hotz Test of Pre-Intervention Equality
| VARIABLES | (1) | (2) | (3) |
|---|---|---|---|
| Log Expenditures/Month | |||
|
| |||
| All | Hypertension | Diabetes | |
| treat × 2009q1 | 0.162 (0.119) | 0.141 (0.142) | 0.149 (0.215) |
| treat × 2009q2 | −0.0107 (0.133) | −0.00459 (0.159) | 0.00576 (0.242) |
| treat × 2009q3 | −0.0437 (0.132) | 0.0454 (0.158) | −0.221 (0.240) |
| treat × 2009q4 | 0.227 (0.147) | 0.294 (0.177) | 0.0998 (0.266) |
| Constant | 3.581*** (0.0426) | 3.493*** (0.0503) | 3.769*** (0.0788) |
| F statistic | 1.67 | 1.13 | 0.78 |
| Prob > F | 0.15 | 0.34 | 0.54 |
| Observations | 5,022 | 3,410 | 1,612 |
| R-squared | 0.01 | 0.01 | 0.01 |
| Number of patients | 1,164 | 812 | 352 |
Robust standard errors in parentheses
p<0.01,
p<0.05
Acknowledgments
Karen Eggleston gratefully acknowledges support from the US National Institutes of Health/National Institute on Aging, Stanford University Center for Demography and Economics of Health and Aging (CDEHA) AG017253 seed project entitled “Socioeconomic Gradients in Health among the Elderly in China.”
Footnotes
http://www.gov.cn/zwgk/2009-04/07/content_1279256.htm, accessed April 12, 2016
Due to requirements of the health departments of the two counties which provided the data for our study, we are unable to refer to the counties by name.
Escaping the dilemma of “more bids, higher prices” – exploring Shandong’s centralized bidding for drugs, http://news.xinhuanet.com/2011-08/04/c_121815179.htm, accessed April 14, 2016
Shandong Province: EML will cover 80% of prefecture and municipal districts in 2011, http://www.gov.cn/gzdt/2010-12/07/content_1760644.htm, accessed April 14, 2016
Shandong will implement reform at all public hospitals in 2016, http://www.shandong.gov.cn/art/2015/12/2/art_322_70288.html, accessed April 15, 2016
Compensation reform: increasing salary must be accompanied by structural reforms, http://www.jkb.com.cn/news/depth/2016/0308/385455.html, accessed April 15, 2016
Zero drug mark-up policy is only the first step: Government to implement compensation plans for lost revenues, http://society.people.com.cn/n/2015/0806/c1008-27421071.html, accessed April 18, 2017
“Our main point here is that the literal target income model can be reconciled with maximization (although with a somewhat peculiar utility function)” (McGuire and Pauly 1991, p. 389).
Regulation of Township Health Centers in Shandong, available at http://www.baike.com/wiki/
 , accessed April 12, 2016).
, accessed April 12, 2016).
A quick analysis of public hospital physician compensation reform in China, available at http://www.chinahrd.net/article/2015/04-13/225634-1.html, accessed April 12, 2016).
Zero drug mark-up policy is only the first step: Government to implement compensation plans for lost revenues, http://society.people.com.cn/n/2015/0806/c1008-27421071.html, accessed April 18, 2017
The national EML includes 9 western medications for treatment of hypertension (Captopril, Enalapril, Sodium Nitroprusside, Magnesium Sulfate, Nitrendipine, Indapamide, Phentolamine, Compound Reserpine, Compound Hypotensive) and 4 for treatment of diabetes (Insulin, Metformin, Glibenclamide, and Glipizide).
One US dollar is about 6.1485 RMB yuan (or 0.1626 RMB yuan per US dollar). Average per capita income in rural areas of this prefecture (the region that includes both the Treatment and Control counties) was about 7600 RMB Yuan in 2010, indicating that the average out-of-pocket medical expenditures for these rural patients with chronic disease constituted about 13 percent (1000/7600) of annual per capita income.
These means are well above the clinical threshold for diagnosis of diabetes of ≥ 7.0 mmol per liter (FPG ≥ 126 mg/dl) recommended by both the American Diabetes Association and the World Health Organization (Inzucchi 2012; Yang et al. 2010).
Yang Quan City uses reward rather than compensation to solidify Essential Medications Policy, http://www.mof.gov.cn/xinwenlianbo/shanxicaizhengxinxilianbo/201511/t20151126_1583987.html, accessed April 18, 2016.
China drug price reform risks placing hospitals on life support, http://www.ft.com/intl/cms/s/0/19d87eb8-0379-11e5-b55e-00144feabdc0.html#axzz469FIxQQg, Financial Times, accessed on April 18, 2016.
Brief Report on Public Hospital Reform, Vol. 317: Dongying City in Shandong Strengthens Its Commitment to Public Hospital Reform, http://www.nhfpc.gov.cn/yzygj/s10006/201305/4f253c1232904c7ab7186349fcdb175c.shtml, accessed April 14, 2016.
Conflicts of Interest: The authors declare no conflicts of interest.
Contributor Information
Brian K. Chen, Arnold School of Public Health, University of South Carolina, 915 Greene Street Suite 354, Columbia, SC 29208, USA.
Y. Tony Yang, College of Health and Human Services, George Mason University.
Karen Eggleston, Walter A. Shorenstein Asia Pacific Research Center, Stanford University.
References and Literature Citations
- Chandra A, Cutler D, Song Z. Who ordered that? The economics of treatment choices in medical care. Handbook of Health Economics. 2012;2:397–431. [Google Scholar]
- Chen BK, Eggleston KN. Patient Copayments, Provider Incentives and Income Effects: Theory and Evidence from China’s Essential Medications List Policy, Stanford Asia Health Policy Program working paper. 2013 Sep; doi: 10.1002/wmh3.222. ( http://asiahealthpolicy.stanford.edu/publications/list/0/0/4/) [DOI] [PMC free article] [PubMed]
- Chen M, Chen W, Wang L, Mao W. Impact of the Essential Medications Policy (EMP) on rational use of medicines in primary care institutions. Poster presented at the Second Global Symposium of Health Systems Research; Beijing, PRC. 2012. [Google Scholar]
- Currie J, Lin WC, Meng JJ. Addressing antibiotic abuse in China: An experimental audit study. Journal of Development Economics. 2014;110:39–51. doi: 10.1016/j.jdeveco.2014.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eggleston K. Prescribing institutions: Explaining the evolution of physician dispensing. Journal of Institutional Economics. 2012;8:247. [Google Scholar]
- Eggleston K. Multitasking and mixed systems for provider payment. Journal of Health Economics. 2005;24:211–223. doi: 10.1016/j.jhealeco.2004.09.001. [DOI] [PubMed] [Google Scholar]
- Eggleston K. Health Care for 1.3 Billion: China’s Remarkable Work in Progress. Milken Institute Review. 2012:16–27. [Google Scholar]
- Ellis RP, McGuire TG. Supply-side and demand-side cost sharing in health care. Journal of Economic Perspectives. 1993;7(4):135–151. doi: 10.1257/jep.7.4.135. [DOI] [PubMed] [Google Scholar]
- He J, Gu DF, Wu XG, et al. Major causes of death among men and women in China. New England Journal of Medicine. 2005;353:1124–1134. doi: 10.1056/NEJMsa050467. [DOI] [PubMed] [Google Scholar]
- Huang YF, Yang YY. Pharmaceutical pricing in china. In: Eggleston K, editor. Prescribing Cultures and Pharmaceutical Policy in the Asia-Pacific. Shorenstein Asia-Pacific Research Center and Brookings Institution Press; 2009. pp. 205–222. [Google Scholar]
- Iizuka T. Experts’ agency problems: Evidence from the prescription drug market in Japan. The Rand Journal of Economics. 2007;38:844–862. doi: 10.1111/j.0741-6261.2007.00115.x. [DOI] [PubMed] [Google Scholar]
- Iizuka T. The economics of pharmaceutical pricing and physician prescribing in Japan. In: Eggleston K, editor. Prescribing Cultures and Pharmaceutical Policy in the Asia Pacific. Shorenstein Asia-Pacific Research Center and Brookings Institution Press: 2009; 2008. pp. 47–59. [Google Scholar]
- Iizuka T. Physician agency and adoption of generic pharmaceuticals. American Economic Review. 2012;102(6):2826–2858. doi: 10.1257/aer.102.6.2826. [DOI] [PubMed] [Google Scholar]
- Jin CG, Yang HW, Luo B. Impacts of essential medicines reform pilot on the average number of medicines per prescription in primary medical institutions in Zhejiang province. Chinese Health Economics. 2012;1:014. [Google Scholar]
- Li K, Sun Q, Zuo G, Yang H, Meng Q. Study of the impact of the essential medicine system on the patient visits and cost in township hospitals: Based on the evaluation method of difference in difference. Chinese Health Economics. 2012;31(4):62–64. [Google Scholar]
- Liu X, Mills A. The influence of bonus payments to doctors on hospital revenue: results of a quasi-experimental study. Applied Health Economics and Health Policy. 2003;2:91–98. [PubMed] [Google Scholar]
- Lundin D. Moral hazard in physician prescription behavior. Journal of Health Economics. 2000;19:639. doi: 10.1016/s0167-6296(00)00033-3. [DOI] [PubMed] [Google Scholar]
- Ma CA, McGuire TG. Optimal health insurance and provider payment. American Economic Review. 1997;87(4):685–704. [Google Scholar]
- Meng Q. Shandong University Center for Health Management and Policy working paper. 2008. Case-based provider payment systems in China. Working paper submitted to “Provider Payment Incentives in the Asia-Pacific” conference. [Google Scholar]
- Miao Y, Wang L. Study on compensatory channels of village doctor’s income under the essential medicines system. China Journal of Health Policy. 2011;4(9):35–40. [Google Scholar]
- Sun Q, Santoro MA, Meng QY, Liu C, Eggleston K. Pharmaceutical policy in china. Health Affairs. 2008;27:1042–1050. doi: 10.1377/hlthaff.27.4.1042. [DOI] [PubMed] [Google Scholar]
- Sun Q, Zuo G, Li K, Meng Q, He P. Whether the Essential Medicine Policy Decreases the Medical Cost of Rural Population: Experience from Three Counties in Anhui Province. Chinese Health Economics. 2012;31(4):65–67. [Google Scholar]
- Tian X, Song YR, Zhang XP. National essential medicines list and policy practice: A case study of China’s health care reform. BMC Health Services Research. 2012a;12:1–8. doi: 10.1186/1472-6963-12-401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tian L, Shi R, Yang L, Yang H, Ross-Degnan D, Wagner AK, Zhao F. Changes in the pattern of patient visits and medical expenses after the implementation of the National Essential Medicines Policy in rural China: a segmented time series regression analysis. 2012b Unpublished manuscript. [Google Scholar]
- Wang L. Under the influence of the essential drug list, how to deal with the challenges. Chinese Primary Health Care. 2012;26(3):37–38. [Google Scholar]
- Wang X, Yang X, Chai L. The impact of the national essential medicine system on the drug-prescribing behavior of general practitioners in community hospitals. Strait Pharmaceutical Journal. 2012;24(2):285–286. [Google Scholar]
- Wu J, Xu H, Yin H. Problems and suggestions on the trial implementation of the national essential drug system. Medicine and Philosophy. 2010;31(9):41–42. [Google Scholar]
- Xiang XX, Yang CY, Wang DF, Ye J, Zhang XP. Effects of China’s national essential medicines policy on the use of injection in primary health facilities. Journal of Huazhong University of Science and Technology [Medical Sciences] 2012;32:626–629. doi: 10.1007/s11596-012-1008-4. [DOI] [PubMed] [Google Scholar]
- Yang H, Sun Q, Zuo G, Li K, Meng Q. Changes in drug usage and the structure of township hospitals under the essential medicine system: cases in three counties of Shandong province. Chinese Health Economics. 2012a;31(4):59–61. [Google Scholar]
- Yang L, Yang H, Zhao F, Tian L, Ross-Degnan D, Wagner AK. Using interrupted times series to assess the 2009 national medicine policy. Presentation at the Second Global Symposium of Health Systems Research; Beijing, PRC. 2012b. [Google Scholar]
- Yang WY, Lu JM, Weng JP, et al. Prevalence of diabetes among men and women in China. New England Journal of Medicine. 2010;362:1090–1101. doi: 10.1056/NEJMoa0908292. [DOI] [PubMed] [Google Scholar]
- Ye Y, Zhu L, Wu X, Yue Q, Wang H, Fan X, Wan Y, Zhang W. The impact of the essential medicine system on the new rural cooperative medical care. Chinese Rural Health Service Administration. 2011;12:1221–1224. [Google Scholar]
- Zhang Y, Xia LY, Xiong J, Yao L. Discussing the influence of the national system for basic pharmaceuticals on the operations of centers for community health services. The Chinese Health Service Management. 2011;11:814–816. [Google Scholar]