Abstract
Purpose of review
Idiopathic Pulmonary Fibrosis (IPF) is the most common form of interstitial lung diseases of unknown eathiopathogenesis, mean survival of 3-5 years and limited therapeutics. Characterized by a loss of alveolar type II epithelial cells and aberrant activation of stromal cells, considerable effort was undertaken to characterize the origin and activation mechanisms of fibroblasts and myofibroblasts in IPF lungs. In this review, the origin and contribution of fibroblast and myofibroblasts in lung fibrosis will be summarized.
Recent findings
Lineage tracing experiments suggested that interstitial lung fibroblasts and lipofibroblasts, pericytes and mesothelial cells differentiate into myofibroblasts. However, epithelial and bone marrow derived cells may give rise to collagen expressing fibroblasts but do not differentiate into myofibroblasts.
Summary
There is great heterogeneity in fibroblasts and myofibroblasts in fibrotic lungs. Further, there is evidence for the expansion of pericyte derived myofibroblasts and loss of lipofibroblasts and lipofibroblast derived myofibroblasts in IPF.
Keywords: Idiopathic Pulmonary Fibrosis, Lung Fibrosis, Lung Fibroblasts, Mesenchymal progenitors, Fibroblast progenitors, fibroblast heterogeneity
Introduction
Idiopathic Pulmonary Fibrosis (IPF) is the most common clinical form of Interstitial Lung Disease (ILD), with poor prognosis, median survival of 3–5 years after diagnosis, and limited pharmacological intervention[1–3]. IPF is characterized histologically by the presence of Usual Interstitial Pneumonia (UIP), containing fibroblastic foci, which are believed to be sites of active tissue remodeling. The fibrotic triggers in IPF are unknown but it is speculated that recurring micro-injury leads to alveolar epithelial cell death, epithelial progenitor exhaustion, and subsequent aberrant repair mechanism(s) ablates the alveolus. IPF patients present with variable progression rates, with some showing a slow decline and others showing a more rapid progressive decline of lung function[4]. In addition to the variable progression rates, some IPF patients experience acute exacerbations, where diffuse alveolar damage is apparent and subsequent rapid decline of lung function ensues[5]. Indeed, various studies have focused on identifying mechanisms behind the progressive decline of lung function in IPF patients, which have identified multiple pathways modulating epithelial regeneration, immune activation, and fibroblast differentiation and invasion. In this review, the heterogeneity of mesenchymal cells in normal and fibrotic murine lungs, mechanisms propagated by these cells in preclinical models of lung fibrosis will be summarized and their potential human counterparts in IPF will be discussed. Due to wording limitations, reference to all relevant studies pertaining to stromal cell function and heterogeneity in the lung is not possible, and the authors apologize for any omissions.
Mesodermal development in the lung
Mesodermal development in the lung is a complex but poorly understood process due to a lack of good mesodermal markers. However, with the advent of cell tracing techniques, various recent studies have provided some key insight into mesodermal development in the lung. Pulmonary mesoderm is thought to be derived from the lateral plate mesoderm[6], which gives rise to the splanchnic mesoderm and subsequently to the mesodermal lineages in the heart, lung, gut, connective tissues, and blood vessels. One of the earliest mesenchymal specific transcription factor to be activated in the developing murine respiratory system is TBX4, which is observed as early as E9.25 in lung buds and is expressed most mesenchymal cells by E11.5[7, 8]. Following Tbx4 expression, Gli1 (a direct Sonic Hedgehog (Shh) signaling transcriptional target) is detected at E10.5–11.5[9], and it remains activated for the development of bronchial and vascular smooth muscle cells and various stromal cell populations in murine lungs[9, 10]. Following Shh signaling, it is speculated that Wnt singling is required for further differentiation of mesodermal progenitors into pericytes, resident interstitial fibroblasts, and smooth muscle cells[9, 11, 12]. Pericytes appear to arise from Foxn1-expressing perivascular progenitor cells, which were shown to give rise to several distinct populations of PDGFRß+ NG2+ pericytes, some of which co-express PDGFRα and collagen 1[13]. Pericyte heterogeneity is exemplified by the further differentiation of Foxj1 expressing pericyte progenitors into mature perivascular NG2-expressing pericytes[14]. Interstitial Collagen 1-expressing fibroblasts arise from mesodermal progenitors in a Wnt-[9, 12], Shh-[9] and PDGFRα-[15–17] dependent manner. The differentiation of pulmonary vascular and bronchial smooth muscle cells is a complex process[18] requiring the activation of both Shh[9] and FGF10[19] signaling, and the inhibition of FGF9 signaling[20]. Further, a subset of resident peribronchial fibroblasts, bronchial and vascular smooth muscle cells arise from Wt1- expressing mesothelial cells[21, 22]. Finally, lipofibroblasts, a neutral lipid-rich fibroblast population that are required for alveolar type II epithelial cell proliferation, differentiation, and surfactant protein production[23] arise from mesodermal progenitor cells through the activation of FGF10[24, 19] and PPARγ[25] and the inhibition of ALK5[26]. Together, these various cell types comprise the pulmonary mesenchyme and considerable effort has focused on characterizing their roles in lung remodeling and regeneration.
Fibroblast and myofibroblasts heterogeneity in injured murine lungs
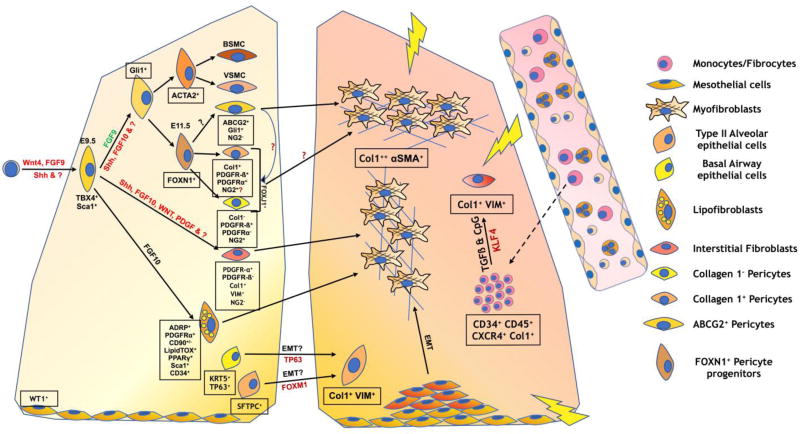
Due to a heightened interest in developing anti-fibrotic therapeutics, considerable effort has been directed at characterizing the cellular origin of fibroblasts and myofibroblasts during organ fibrosis. In this section, a summary of findings from various studies characterizing the origin of collagen - and/or αSMA-expressing fibroblasts and myofibroblasts in experimental lung injury in mice is provided. A simplified pictorial summary of key mesenchymal and hematopoietic lineages present in the lung during fibrosis and myofibroblast differentiation is shown in Figure 1 and summarized in Table 1. For additional review on this topic, the reader is referred to[27].
Figure 1.
Mesodermal development in the lung and heterogeneity of fibroblasts and myofibroblasts in fibrotic lungs. Depicted is a simplified summary of mesodermal development in normal lungs (left) and potential lineages leading to the generation of fibroblasts and myofibroblasts in remodeled lungs (right).
Table 1.
Summary of Mesodermal lineages and their contribution to myofibroblasts in injured lungs
| Cell type | Potential Markers | Myofibroblast differentiation potential |
Location | References |
|---|---|---|---|---|
| Lipofibroblasts | CD45−, EpCAM−, ADRP+, PDGFRα+ PDGFRβ−, CD90+/− PPARγ+, Sca1+ CD34+, NG2− | Yes | Interstitium, near Alveolar Type II Epithelial cells. | [29, 24, 35, 34, 25] |
| Interstitial fibroblasts | CD45−, EpCAM− ADRP−, PDGFRα+ PDGFRβ−, Col1+ VIM+, NG2− | Yes | Interstitium | [29, 34, 27, 13] |
| Pericytes (FoxJ1+) | CD45−, EpCAM−, PDGFRβ+, PDGFRα−?, NG2+, Col1−?, Foxn1+ | No | Perivascular | [14, 27, 13] |
| Pericytes (FoxJ1−) | CD45−, EpCAM−, PDGFRβ+, PDGFRα+ Col1+, NG2−?, ABCG2+?, Foxn1+? | Yes | Perivascular | [27, 13, 28] |
| Fibrocytes | CD45+, EpCAM−, CD34+, CXCR4+ Col1+ | No | Bone Marrow & Circulation | [53, 47, 48, 54, 49, 51] |
| Mesothelial cells | Wt1+, Calretinin+ | Yes? | Pulmonary pleura | [44, 43, 45, 46] |
| Basal epithelial cells | CD45−, EpCAM+ KRT5+, TP63+ | No | Pulmonary airways | [42] |
| Alveolar type II epithelial cells | CD24−, Sca1−, CD45−, EpCAM+, SFTPC+ | No | Interstitium | [40, 37, 39, 41, 14, 90] |
| Smooth muscle cells | ACTA2+, Desmin+ | No | Peribronchial and Perivascular | [14, 35] |
Pericytes
Pericytes are heterogeneous perivascular, mesenchymal-like cells that are known to regulate blood vessel formation and maintenance under physiologic conditions, and have an emerging role in lung remodeling (reviewed in[27]). In a recent study, NG2 (a cell surface pericyte marker) and Foxj1 (a pericyte and club cell specific transcription factor) were used as lineage tracers for pericytes in a mouse model of bleomycin-induced pulmonary fibrosis. In this study, no significant contribution of lineage-labeled pericytes to αSMA expressing myofibroblasts, present at day 21 after intratracheal bleomycin instillation, was observed[14]; however, the contribution of lineage-labeled cells to collagen 1-expressing fibroblasts was not assessed. In another study that employed both Foxn1 and collagen 1 as a lineage markers[13], Foxn1 labeled two distinct PDGFRß+ NG2+ pericyte lineages, one of which expressed collagen 1 (PDGFRβ+ PDGFRα+ Collagen 1+; Figure 1). At days 7 and 14 after bleomycin-induced lung injury, Foxd1-labeled cells accounted for ~45% and ~68% of αSMA expressing myofibroblasts in the lungs, respectively. Consistent with these findings, when Foxd1 and Collagen 1 chimeric reporter mice were studied, approximately 47% of Collagen 1 lineage-labeled cells were also lineage labeled for Foxd1 at day 7 after bleomycin challenge. However, this finding also highlights that approximately 53% of collagen 1 lineage-labeled cells were not labeled with the Foxd1 lineage tracer suggesting that the majority of collagen 1-expressing cells come from other sources in experimental fibrosis. In a third study using ABCG2 as a lineage tracer for a subset of NG2− pericytes[28], ABCG2+ cells gave rise to αSMA+ myofibroblasts at day 14 after intrathecal bleomycin delivery. Further, in vitro analysis indicated that AGCG2+ cells were phenotypically, genotypically, and functionally distinct from NG2+ pericytes. Collectively, these studies provide evidence for the heterogeneity of pericytes in the lung and suggest that there are several populations of NG2/Foxj1-negative pericytes, which give rise to myofibroblasts in lung fibrosis.
Resident fibroblasts and lipofibroblasts
Resident fibroblasts are defined as fibroblasts that are localized in the interstitium of uninjured lungs immediately adjacent to alveolar epithelial cells. Lipofibroblasts are resident lung fibroblasts rich in neutral lipids that have been shown to be important for alveolar epithelial type II cell homeostasis. These cells are known to express high levels of the Adipose Differentiation-Related Protein (ADRP), PPARγ and PTHrP receptor (PTH1R). Several investigators have embarked on studies to identify cell surface fibroblast specific markers but to date success has been limited. These studies have culminated on the identification of a few markers including Sca-1[29], CD248[29–32], PDGFRα[17, 33, 15, 16, 34] as good candidate markers. Among them, PDGFRα seems to best distinguish interstitial resident fibroblasts and lipofibroblasts from pericytes, where resident fibroblasts are lineage negative (Lin−; CD45− EpCAM− & CD31−), PDGFRα+, PDGFRβ−, CD90−, lipofibroblasts are Lin−, PDGFRα+, PDGFRβ−, CD90+ and LipidTOX+ (A Neutral lipid stain) and a small subset of pericytes are Lin−, PDGFRα+ & PDGFRß+[13, 17, 29]. Collagen 1 lineage-labeled PDGFRα+ PDGFRß− cells (which are distinct from lineage-labeled pericytes, see above), contributed to ~53% of collagen 1-expressing cells at day 7 after bleomycin-induced lung injury and remodeling[13]. In another study utilizing PDGFRα as a lineage tracer and pneumonectomy as a model of lung injury, two major subtypes of PDGFRα-expressing cells were identified in uninjured lungs - a more abundant PDGFRαhi and a less abundant PDGFRαlow cell types[17]. Via transcriptomic characterization, PDGFRαlow cells were enriched for various transmembrane collagens and other transcripts typically observed in myofibroblasts. However, a few reports have suggested that αSMA expression was confined to vascular and bronchial smooth muscle cells in uninjured murine lungs[14] and that these cells did not contribute to interstitial αSMA+ myofibroblasts after bleomycin injury[35], suggesting that that the PDGFRαlow population might represent a population of smooth muscle cells. PDGFRαhi cells were enriched for fibrillar collagens, matrix remodeling enzymes (Loxl2, Loxl4, MMP3, MMP17 & MMP17) consistent with interstitial fibroblasts. Flow cytometric analysis of PDGFRα lineage-labeled cells indicated that ~60% of these cells expressed Sca-1, ~50% expressed CD34, ~30% expressed CD29, <10% expressed Thy-1, CD44 and/or CD49, and a small subset (<5%) expressed CD40. After pneumonectomy, CD29-expressing, PDGFRα lineage-labeled cells were more proliferative, and expressed the highest level of αSMA, whereas CD34 and Sca1 expressing lineage-labeled cells were less abundant. Interestingly, CD34+ PDGFRα lineage-labeled cells showed the highest levels of neutral lipid content indicating that these cells might represent the PDGFRα-expressing lipofibroblast population. In addition, there were various subsets of αSMA-expressing cells, including PDGFRα+ CD34+, PDGFRα+ CD34+ CD29+ and PDGFRα+ CD34− CD29+ suggesting considerable heterogeneity in αSMA-expressing cells at day 5 after pneumonectomy. Nevertheless, this study did not address the relative contribution of PDGFRα-expressing pericytes co-expressing PDGFRβ to the αSMA-expressing myofibroblast population in this model.
To better characterize the role of lipofibroblasts in lung remodeling and repair, the lipofibroblast specific transcript adrp has been utilized as a lineage tracer. In a recent study, a subset of adrp lineage-labeled lipofibroblasts transdifferentiated into αSMA-expressing myofibroblasts in response to bleomycin injury. Interestingly, FGF10 expression and neutral lipid content was observed to increase in αSMA-expressing myofibroblasts from days 14 to 28 after bleomycin challenge. This was followed by a loss of αSMA expression and the reappearance of lipofibroblasts, suggesting that myofibroblast to lipofibroblast trans-differentiation occurs during the resolution of bleomycin-induced lung remodeling[35]. Coincidently, the PPAR-γ agonist, Rosiglitazone, which have been shown to induce lipofibroblast differentiation[25], markedly reduced αSMA expression in interstitial fibroblasts after pneumonectomy[36] and attenuated TGFß-induced human lung fibroblast to myofibroblast differentiation[35], further supporting the hypothesis that a subset of lipofibroblasts give rise to myofibroblasts after lung injury and that lipofibroblast reconstitution is required for lung regeneration. Collectively, these studies suggest that PDGFRα-expressing interstitial fibroblasts and/or lipofibroblasts respond to lung injury and differentiate into myofibroblasts, and that myofibroblast to lipofibroblasts trans-differentiation is required for the resolution of fibrosis in the mouse lung.
Epithelial and mesothelial cells
The role of epithelial to mesenchymal transition (EMT) in pulmonary fibrosis remains controversial. In vitro studies have demonstrated that EMT occurs in TGFß treated alveolar type II epithelial cells[37] and pulmonary mesothelial cells[38]. To determine the contribution of alveolar type II epithelial cells to generation of lung fibroblasts and myofibroblasts in vivo, sftpc (the gene encoding for Pro-Surfactant protein C) was used as a cell lineage tracer. Utilizing an active TGFß adenoviral expression model of pulmonary fibrosis in a triple transgenic reporter mouse (sftpc-rtTA, tetO-CMV-Cre, Floxed ROSA26) to drive the permanent expression of ß-gal in sftpc-expressing cells after doxycycline treatment, sftpc lineage-traced cells were observed to express vimentin at 3 weeks after intranasal delivery of adenovirus[39]. Further, these cells made up of <20% of total vimentin-expressing cells in this model. However, there were few lineage-labeled cells that expressed αSMA (<5%), suggesting that these cells were not a major source of myofibroblasts in this study. Further, in two other studies using sftpc-Cre, R26Rosa.stop.LacZ reporter mice (which express ß-gal in all sftpc-expressing cells in the lung) sftpc lineage-labeled cells were observed to give rise to S100A4-expressing fibroblast-like cells, in response to a single dose[37] or a repetitive dosing regimen[40] of bleomycin. Also in both studies, sftpc-labeled epithelial cells were not observed to express αSMA after lung injury and remodeling. In another study using an sftpc-CreERT2,ROSA-tomato double heterozygous mice to lineage label sftpc-expressing cells after tamoxifen treatment, lineage-labeled cells were not observed to give rise to αSMA, vimentin or S100A4 expressing cells at 10 and 21 days after bleomycin challenge[14]. This was confirmed via cell sorting of lineage-labeled cells followed by qPCR analysis of the sorted cells relative to lineage-negative cell. Unlike these negative cells, lineage-labeled cells expressed negligible amounts of acta2, vim, s100a4, and col1a1 transcripts. In the same study, using a club cell specific scgb1a1-CreER; ROSA Tomato lineage tracer to label scgb1a1 expressing club cells upon tamoxifen treatment, lineage-labeled cells did not give rise to αSMA, vimentin or S100A4 expressing cells at day 21 after bleomycin challenge. Interestingly, in another study using an Acta2-Cre, R26Rosa.stop.LacZ lineage driver to label β-gal in all acta2 expressing cells, scattered bronchial epithelial cells were lineage-labeled, suggesting that acta2 expression does not readily occur in these cells[41]. Unfortunately, the relative contribution of bronchial epithelial cells to acta2 expressing myofibroblasts was not systematically examined in this study.
Discrepancies between these studies might be due to differences in the reporter system(s) or the fibrotic models utilized. The mesenchymal transition of alveolar type II epithelial cells has been observed to be dependent on the presence of deposited fibrin and/or fibronectin[39], suggesting that potential differences in fibronectin and/or fibrin deposition in different murine models of pulmonary fibrosis could potentially contribute to the divergent observations in these studies. A seminal study employing single cell RNAseq analysis of epithelial cells isolated from normal and IPF lung samples demonstrated the co-expression of basal cell markers (i.e. KRT5 and TP63) and the mesenchymal marker, vimentin, in IPF but not normal epithelial cells[42]. Collectively, these studies raise the possibility that alveolar type II and basal epithelial cells might give rise to collagen 1, vimentin and/or S100A4 expressing fibroblasts, but there is no conclusive evidence for these cells also giving rise to αSMA-expressing myofibroblasts. Future studies are warranted to better characterize the transition of Sftpc-expressing alveolar epithelial and Krt5 Tp63-expressing cells into mesenchymal cells in vivo.
Pulmonary mesothelial cells are cells lining the pulmonary pleura. Since lung remodeling in IPF is first observed in the distal subpleural regions in the lung, there is considerable interest in determining the role of these cells in this disease. Most studies characterizing pulmonary mesothelial cells in lung fibrosis utilize Wilms’ tumor suppressor gene, wt1, as a marker for these cells. Wt1 is exclusively expressed in embryonic mesothelial cells as early as embryonic day E10.5 and by E18.5 its expression levels significantly declines such that this gene is not expressed in adult lungs[21, 43]. Importantly, several studies have shown that this tumor suppressor is induced after lung injury and/or remodeling[44, 45, 43]. Two studies utilizing Wt1tm1EGFP/Cre)wtp/J to label all cells with an active wt1 promoter with EGFP have showed that lineage-labeled cells invaded into the pulmonary parenchyma and a subset of these cells expressed αSMA at 4 to 24 h after intratracheal delivery of active TGFß[44, 45]. This was confirmed using a different wt1 lineage tracing mouse strain, Wt1Tm2(Cre/ERT2)Wtp/J; B6.129S4-Gt(ROSA)-26Sortm1Sor/J to label wt1-expressing cells irreversibly with ß-gal at 4 h after intratracheal TGFß administration[44]. Further, in a CCSP/TGFα transgenic mouse model of lung fibrosis, Wt1-immunostained cells appeared to invade into the pulmonary parenchyma and express vimentin by co-immunofluorescent analysis[43]. Interestingly, utilizing a Wt1CreERT1/+ROSAmTmG/+ strain to label all cells with tdTomato and wt1-expressing cells with GFP, intradermal bleomycin administration induced pleural thickening and increased wt1 lineage-labeled cells in the pulmonary pleura but these cells were not observed to invade into the pulmonary parenchyma[43]. Indeed, a similar observation was made in another report, utilizing Wt1 CreERT2/+ROSA26mTmG/ strain in which tamoxifen was administered at postnatal day P4 to label wt1-expressing cells, and lung remodeling was induced via 8 biweekly intratracheal doses of bleomycin[22]. Surprisingly, wt1 lineage labeled cell proliferation and pleural thickening at 4 weeks after intratracheal active TGFß adenoviral overexpression did not lead to vimentin, or αSMA expression by lineage-labeled cells.
Differences observed in these studies might be due to the lineage tracing methods employed and/or the variable changes in WT1 expression after the distinct forms of pulmonary injury. It is also possible that de novo WT1 expression in invading mesothelial cells might represent a population of cells undergoing mesenchymal transition. Transient lineage labeling of wt1 expressing cells prior to lung injury might not lineage label de novo WT1 -expressing cells thereby explaining why cells invaded into the parenchyma and expressed stromal markers were observed in studies in which constitutive wt1 labeling reporters were utilized. Finally, it has been observed that pleural thickening in IPF is associated with the parenchymal localization of Wt1- or calretinin- (another marker of pleural mesothelial cells) expressing cells [44, 43, 45, 46], and the co-localization of vimentin in parenchymal Wt1-immunostained cells[43]. Collectively, these studies suggest that pulmonary mesothelial cells might contribute to the sub-pleural fibrotic response in various murine models of fibrosis and in IPF via their proliferation and mesenchymal transition to generate fibroblasts and myofibroblasts. Future studies are warranted to better characterize the in vivo mesenchymal transition of mesothelial cells using other more stably-expressed cell markers after lung injury and remodeling.
Bone marrow derived cells
The role of bone marrow derived cells in pulmonary fibrosis remains controversial albeit frequently reviewed[47–52]. With the advent of GFP transgenic mice, adoptive transfer of GFP+ bone marrow into GFP− mice to create chimeras has been a popular approach to characterize the role of bone marrow-derived cells in pulmonary fibrosis. One study showed a large influx of GFP+ bone marrow derived cells in the lungs of bleomycin-challenged mice and these cells co-expressed collagen 1[53]. Specifically, flow cytometric analysis of lung cellular suspensions suggested that approximately 80% of collagen 1 expressing cells co-expressed GFP. However, this percentage is likely inflated since it is possible that GFP+ immune cells might stain positively for collagen due to the propensity of soluble collagen fragments to bind to activated integrins. In vitro culture of GFP+ fibroblasts from the fibrotic lungs of bleomycin-challenged, bone marrow chimeric mice indicated that these fibroblasts expressed collagen but lacked αSMA after stimulation with TGFß. In another study employing a lung irradiation-induced fibrosis model, GFP+ vimentin+ bone marrow-derived cells were detected in fibrotic areas of the irradiated lungs[54]. Thus, these studies suggest that bone marrow-derived cells can differentiate into collagen 1-expressing fibroblasts, but these cells fail to differentiate into myofibroblasts during fibrosis.
There are two major bone marrow-derived cell types that have been implicated in lung fibrosis, mesenchymal stem cells (MSCs), and fibrocytes. The role of MSCs in bleomycin induced lung fibrosis is controversial with some studies claiming that MSCs are protective in mice challenged with bleomycin whereas others indicating that these cells are protective only when given preventatively prior to bleomycin instillation. Still other studies have not reported any beneficial effect of these cells (reviewed in [55]). Further, a Phase 1b study addressing the safety of the infusion of placental derived mesenchymal stromal cells in IPF patients failed to show any significant changes in Forced Vital Capacity (FVC), Diffusing Capacity of the lungs for Carbon Monoxide (DLCO), 6-minute walk distance or CT fibrosis score, at 6 months after a single infusion of 1–2 million cells intravenously[56]. While it remains to be further investigated, these current studies suggest that MSC might not modulate or contribute to fibrotic remodeling in mouse or human lung.
Fibrocytes are bone marrow-derived, monocyte-like cells expressing CD45-RO, CD34, and collagen 1[57]. These cells have been extensively studied in fibrosis and cancer, and have been shown to express a plethora of general markers including CD11b, CD80, CD86, CCR2, CCR7, and CXCR4[57–59]. Further, two studies have suggested that fibrocytes may differentiate from Myeloid Derived Suppressor Cells (MDSCs) in a KLF4-dependent manner[60, 61]. Interestingly, it was recently reported that there is an expansion of circulating monocyte-like MDSCs and a positive correlation between MDSC numbers and the decline of pulmonary function was noted [62]. Two predominant populations of fibrocytes have been described and these include CD45+ Collagen 1+ CXCR4+ CCR7− and CD45+ Collagen 1+ CXCR4− CCR7+[59], but the CXCR4-expressing fibrocytes appear to be the predominant population of cells recruited to the fibrotic lungs. This is supported by another study utilizing CCR7-deficient mice, in which there were no apparent changes in fibrocyte recruitment into the lungs of CCR7-deficient lungs compared with their wildtype counterparts after bleomycin[63]. Indeed, it appears that CXCR4+ fibrocytes are the predominant population of circulating fibrocytes in IPF patients[64, 65]. Finally, it was recently reported that adoptively transferred fibrocytes enhanced the accumulation and/or proliferation of WT1+ mesothelial cells in a club cell-driven TGFα overexpression model of lung fibrosis[43]. Collectively, these studies suggest that bone marrow-derived fibrocytes might contribute to lung fibrosis and remodeling through the expression of collagens and the modulation of mesothelial cell activation but these cells do not seem to be a source of myofibroblasts in experimental fibrosis in the mouse lung.
Heterogeneity of fibroblasts and myofibroblasts in IPF
As described above, considerable effort has been undertaken to characterize mesenchymal populations in remodeled murine lungs. Collectively, these studies indicate that both fibroblasts and myofibroblasts arise from multiple cell types. Further, transcriptomic analysis on different fibroblasts and myofibroblasts lineages indicates that these cells show many variations in their response(s) to the fibrotic milieu in the lung. Because many of these cells lose the expression of their lineage identifying marker(s) after fibroblast and myofibroblast differentiation, it has been particularly difficult to translate these findings into clinical fibrotic lung diseases such as IPF. Compared with their normal counterparts, IPF lung fibroblasts and myofibroblasts exhibit key alterations in epigenetic regulation[66–71], genetic polymorphisms[72], resistance to apoptosis[73–76], elevated microbial sensing pathways[77–79], and increased invasiveness[80–86] causing IPF cells to be more pro-inflammatory, profibrotic and injurious than normal cells.
Evidence for the expansion of pericyte-derived fibroblasts and myofibroblasts in IPF
Given the heterogeneous sources of murine fibroblasts and myofibroblasts during fibrosis in the lung, it is likely that the changes observed in IPF might be due, in part, to an expansion and/or loss of comparable cell populations. Accordingly, there is a loss of ABCG2-expressing pericytes in IPF patients, which is a process also observed in experimental fibrosis characterized by a loss of ABCG2 expression in pericytes and the differentiation of these cells into myofibroblasts [87, 28], suggesting that pericytes might be giving rise to myofibroblasts in IPF lungs. Further, in the same report, an expansion of PDGFRα+ PDGFRβ+ stromal cells in IPF was noted and these cells may represent a population of collagen 1-expressing pericytes that differentiate into myofibroblasts[13]. Indeed, our mining of RNAseq datasets from lung fibroblasts derived from slow and rapid progressing IPF patient lung samples, and normal lung samples supports an expansion of a PDGFRß- and PDGFRα-expressing stromal population in IPF. Further, various studies have suggested that pericytes express higher levels of innate immune microbial sensors[13, 88] and IPF lung fibroblasts, notably from progressive IPF patients, express TLR9[78, 79] and TLR4[77], and the activation of these microbial sensors leads to myofibroblast differentiation[77–79]. Together, these studies suggest that pericyte-derived fibroblasts and myofibroblasts are present in IPF, and these cells might contribute to fibrotic progression through various mechanisms including microbial sensing pathways.
Loss of lipofibroblasts in IPF
Given the important role of lipofibroblasts in alveolar type II epithelial homeostasis and function, recent studies have addressed the state of these cells in IPF patients. There is a loss of lipofibroblast associated ADRP and PPARγ transcript expression in IPF relative to normal lungs[35]. Transcriptomic and immunohistochemical analysis suggested that FGF10 protein expression is elevated in IPF compared with normal lungs and localized to αSMA expressing cells present in heavily fibrotic areas. These findings suggest that FGF10-expressing myofibroblasts in IPF may be potentially derived from lipofibroblasts. Interestingly, a recent report characterizing mesenchymal cells in bronco-alveolar lavage (BAL) from progressive versus stable IPF showed a loss of FGF10 transcript and protein expression in progressive IPF mesenchymal cells compared with stable IPF mesenchymal cells[89], indicating a loss of lipofibroblasts or myofibroblasts derived from lipofibroblasts in these patients. Mining of RNAseq datasets from our cultured rapid IPF, slow IPF, and normal lung fibroblasts indicate that there are no significant changes in ADRP transcript but a marked reduction in PPARG and FGF10 transcript expression in both IPF groups compared with normal lung fibroblasts. Thus, FGF10 expression might predict progression in IPF, in which patients with a loss of FGF10 progress more rapidly relative to patients with high FGF10 expression due, in part, to the loss of lipofibroblasts or lipofibroblast-potent myofibroblasts. Given the role of these cells in alveolar type II epithelial cell homeostasis and in the efficient repair of bleomycin-induced lung fibrosis[35, 23], loss of lipofibroblasts in IPF further supports the hypothesis that a lack of appropriate epithelial-mesenchymal cell cross talk might lead to the chronic disrepair observed in lungs.
Concluding remarks
Lung remodeling and repair is a complex process driven by the activation and interplay of multiple stromal populations. Murine studies have shed light on the putative origin of highly synthetic myofibroblasts. Specifically, lung myofibroblasts predominately arise from resident fibroblasts, lipofibroblasts, a subset of pericytes, and mesothelial cells. However, other collagen-producing cells including fibrocytes and epithelial cell-derived fibroblasts might also play a role in pulmonary fibrosis. Interestingly, transcriptome sequencing studies in various populations of murine fibroblasts and myofibroblasts has elucidated the identity of the pathways elevated in fibrotic lung diseases, and demonstrated a plethora of different populations of cells with distinct activation pathway, migratory, and invasive characteristics. Further, the loss of lipofibroblast or lipofibroblast- potent myofibroblasts and an expansion of PDGFRβ+ PDGFRα+ pericyte-derived myofibroblasts might be two key cellular processes leading to progressive remodeling in IPF. Future work is warranted to better characterize the stromal populations in IPF and other fibrotic/remodeling lung diseases. It is likely that there are beneficial fibroblast and myofibroblast populations, which are required for alveolar epithelial support and lung regeneration. Thus, therapeutics specifically targeting “pathologic” populations such as pericyte-derived myofibroblasts while concomitantly promoting the expansion of “reparative/regenerative” populations of fibroblasts such as lipofibroblasts might provide beneficial effects in IPF patients.
Footnotes
Compliance with Ethics Guidelines:
Conflict of Interest:
David Habiel and Cory Hogaboam declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent:
This article does not contain any studies with human or animal subjects performed by any of the authors.
References
Recently published papers of particular interest have been highlighted as:
• Of importance
•• Of major importance
- 1.Wolters PJ, Collard HR, Jones KD. Pathogenesis of idiopathic pulmonary fibrosis. Annu Rev Pathol. 2014;9:157–79. doi: 10.1146/annurev-pathol-012513-104706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.du Bois RM. Strategies for treating idiopathic pulmonary fibrosis. Nat Rev Drug Discov. 2010;9(2):129–40. doi: 10.1038/nrd2958. [DOI] [PubMed] [Google Scholar]
- 3.King TE., Jr Clinical advances in the diagnosis and therapy of the interstitial lung diseases. Am J Respir Crit Care Med. 2005;172(3):268–79. doi: 10.1164/rccm.200503-483OE. [DOI] [PubMed] [Google Scholar]
- 4.King TE, Jr, Pardo A, Selman M. Idiopathic pulmonary fibrosis. Lancet. 2011;378(9807):1949–61. doi: 10.1016/S0140-6736(11)60052-4. [DOI] [PubMed] [Google Scholar]
- 5.Collard HR, Moore BB, Flaherty KR, Brown KK, Kaner RJ, King TE, Jr, et al. Acute exacerbations of idiopathic pulmonary fibrosis. Am J Respir Crit Care Med. 2007;176(7):636–43. doi: 10.1164/rccm.200703-463PP. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hogan BL. Morphogenesis. Cell. 1999;96(2):225–33. doi: 10.1016/s0092-8674(00)80562-0. [DOI] [PubMed] [Google Scholar]
- 7.Arora R, Metzger RJ, Papaioannou VE. Multiple roles and interactions of Tbx4 and Tbx5 in development of the respiratory system. PLoS Genet. 2012;8(8):e1002866. doi: 10.1371/journal.pgen.1002866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Xie T, Liang J, Liu N, Huan C, Zhang Y, Liu W, et al. Transcription factor TBX4 regulates myofibroblast accumulation and lung fibrosis. J Clin Invest. 2016;126(8):3063–79. doi: 10.1172/JCI85328. This study nicely shows the importance of TBX4 as a pulmonary mesodermal transcription factor, where TBX4 lineage traced cells give rise to multiple stromal lineages in the lung. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Li C, Li M, Li S, Xing Y, Yang CY, Li A, et al. Progenitors of secondary crest myofibroblasts are developmentally committed in early lung mesoderm. Stem Cells. 2015;33(3):999–1012. doi: 10.1002/stem.1911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Pepicelli CV, Lewis PM, McMahon AP. Sonic hedgehog regulates branching morphogenesis in the mammalian lung. Curr Biol. 1998;8(19):1083–6. doi: 10.1016/s0960-9822(98)70446-4. [DOI] [PubMed] [Google Scholar]
- 11.Caprioli A, Villasenor A, Wylie LA, Braitsch C, Marty-Santos L, Barry D, et al. Wnt4 is essential to normal mammalian lung development. Dev Biol. 2015;406(2):222–34. doi: 10.1016/j.ydbio.2015.08.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.De Langhe SP, Carraro G, Tefft D, Li C, Xu X, Chai Y, et al. Formation and differentiation of multiple mesenchymal lineages during lung development is regulated by beta-catenin signaling. PLoS One. 2008;3(1):e1516. doi: 10.1371/journal.pone.0001516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hung C, Linn G, Chow YH, Kobayashi A, Mittelsteadt K, Altemeier WA, et al. Role of lung pericytes and resident fibroblasts in the pathogenesis of pulmonary fibrosis. Am J Respir Crit Care Med. 2013;188(7):820–30. doi: 10.1164/rccm.201212-2297OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Rock JR, Barkauskas CE, Cronce MJ, Xue Y, Harris JR, Liang J, et al. Multiple stromal populations contribute to pulmonary fibrosis without evidence for epithelial to mesenchymal transition. Proc Natl Acad Sci U S A. 2011;108(52):E1475–83. doi: 10.1073/pnas.1117988108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Levéen P, Törnell J, Betsholtz C, Pekna M, Pekny M, Lindahl P, et al. PDGF-A signaling is a critical event in lung alveolar myofibroblast development and alveogenesis. Cell. 1996;85(6):863–73. doi: 10.1016/s0092-8674(00)81270-2. [DOI] [PubMed] [Google Scholar]
- 16.Lindahl P, Karlsson L, Hellstrom M, Gebre-Medhin S, Willetts K, Heath JK, et al. Alveogenesis failure in PDGF-A-deficient mice is coupled to lack of distal spreading of alveolar smooth muscle cell progenitors during lung development. Development. 1997;124(20):3943–53. doi: 10.1242/dev.124.20.3943. [DOI] [PubMed] [Google Scholar]
- 17.Green J, Endale M, Auer H, Perl AK. Diversity of Interstitial Lung Fibroblasts Is Regulated by Platelet-Derived Growth Factor Receptor alpha Kinase Activity. Am J Respir Cell Mol Biol. 2016;54(4):532–45. doi: 10.1165/rcmb.2015-0095OC. Utilizing a PDGFRα lineage tracer, this study nicely shows all of the PDGFRα derived myofibroblasts in naïve and injured murine lungs. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kim N, Vu TH. Parabronchial smooth muscle cells and alveolar myofibroblasts in lung development. Birth Defects Res C Embryo Today. 2006;78(1):80–9. doi: 10.1002/bdrc.20062. [DOI] [PubMed] [Google Scholar]
- 19.Ramasamy SK, Mailleux AA, Gupte VV, Mata F, Sala FG, Veltmaat JM, et al. Fgf10 dosage is critical for the amplification of epithelial cell progenitors and for the formation of multiple mesenchymal lineages during lung development. Dev Biol. 2007;307(2):237–47. doi: 10.1016/j.ydbio.2007.04.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Yi L, Domyan ET, Lewandoski M, Sun X. Fibroblast growth factor 9 signaling inhibits airway smooth muscle differentiation in mouse lung. Dev Dyn. 2009;238(1):123–37. doi: 10.1002/dvdy.21831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Dixit R, Ai X, Fine A. Derivation of lung mesenchymal lineages from the fetal mesothelium requires hedgehog signaling for mesothelial cell entry. Development. 2013;140(21):4398–406. doi: 10.1242/dev.098079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.von Gise A, Stevens SM, Honor LB, Oh JH, Gao C, Zhou B, et al. Contribution of Fetal, but Not Adult, Pulmonary Mesothelium to Mesenchymal Lineages in Lung Homeostasis and Fibrosis. Am J Respir Cell Mol Biol. 2016;54(2):222–30. doi: 10.1165/rcmb.2014-0461OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Torday JS, Torres E, Rehan VK. The role of fibroblast transdifferentiation in lung epithelial cell proliferation, differentiation, and repair in vitro. Pediatr Pathol Mol Med. 2003;22(3):189–207. doi: 10.1080/pdp.22.3.189.207. [DOI] [PubMed] [Google Scholar]
- 24.Al Alam D, El Agha E, Sakurai R, Kheirollahi V, Moiseenko A, Danopoulos S, et al. Evidence for the involvement of fibroblast growth factor 10 in lipofibroblast formation during embryonic lung development. Development. 2015;142(23):4139–50. doi: 10.1242/dev.109173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Varisco BM, Ambalavanan N, Whitsett JA, Hagood JS. Thy-1 signals through PPARgamma to promote lipofibroblast differentiation in the developing lung. Am J Respir Cell Mol Biol. 2012;46(6):765–72. doi: 10.1165/rcmb.2011-0316OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Li A, Ma S, Smith SM, Lee MK, Fischer A, Borok Z, et al. Mesodermal ALK5 controls lung myofibroblast versus lipofibroblast cell fate. BMC Biol. 2016;14:19. doi: 10.1186/s12915-016-0242-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Barron L, Gharib SA, Duffield JS. Lung Pericytes and Resident Fibroblasts: Busy Multitaskers. Am J Pathol. 2016;186(10):2519–31. doi: 10.1016/j.ajpath.2016.07.004. This review nicely highlights the role(s) of pericytes and resident fibroblasts in lung fibrosis. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Marriott S, Baskir RS, Gaskill C, Menon S, Carrier EJ, Williams J, et al. ABCG2pos lung mesenchymal stem cells are a novel pericyte subpopulation that contributes to fibrotic remodeling. Am J Physiol Cell Physiol. 2014;307(8):C684–98. doi: 10.1152/ajpcell.00114.2014. This study nicely shows the role of ABCG2+ pericytes in murine and human lung fibrosis, where these pericytes can give rise to ACTA2 and collagen 1 expressing myofibroblasts. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.McQualter JL, Brouard N, Williams B, Baird BN, Sims-Lucas S, Yuen K, et al. Endogenous fibroblastic progenitor cells in the adult mouse lung are highly enriched in the sca-1 positive cell fraction. Stem Cells. 2009;27(3):623–33. doi: 10.1634/stemcells.2008-0866. [DOI] [PubMed] [Google Scholar]
- 30.Bartis D, Crowley LE, D’Souza VK, Borthwick L, Fisher AJ, Croft AP, et al. Role of CD248 as a potential severity marker in idiopathic pulmonary fibrosis. BMC Pulm Med. 2016;16(1):51. doi: 10.1186/s12890-016-0211-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Naylor AJ, Azzam E, Smith S, Croft A, Poyser C, Duffield JS, et al. The mesenchymal stem cell marker CD248 (endosialin) is a negative regulator of bone formation in mice. Arthritis Rheum. 2012;64(10):3334–43. doi: 10.1002/art.34556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Smith SW, Croft AP, Morris HL, Naylor AJ, Huso DL, Isacke CM, et al. Genetic Deletion of the Stromal Cell Marker CD248 (Endosialin) Protects against the Development of Renal Fibrosis. Nephron. 2015;131(4):265–77. doi: 10.1159/000438754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Iwayama T, Steele C, Yao L, Dozmorov MG, Karamichos D, Wren JD, et al. PDGFRalpha signaling drives adipose tissue fibrosis by targeting progenitor cell plasticity. Genes Dev. 2015;29(11):1106–19. doi: 10.1101/gad.260554.115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ntokou A, Klein F, Dontireddy D, Becker S, Bellusci S, Richardson WD, et al. Characterization of the platelet-derived growth factor receptor-alpha-positive cell lineage during murine late lung development. Am J Physiol Lung Cell Mol Physiol. 2015;309(9):L942–58. doi: 10.1152/ajplung.00272.2014. [DOI] [PubMed] [Google Scholar]
- 35.El Agha E, Moiseenko A, Kheirollahi V, De Langhe S, Crnkovic S, Kwapiszewska G, et al. Two-Way Conversion between Lipogenic and Myogenic Fibroblastic Phenotypes Marks the Progression and Resolution of Lung Fibrosis. Cell Stem Cell. 2016 doi: 10.1016/j.stem.2016.10.004. This study nicely shows the role of lipofibroblasts in myofibroblast generation in injured murine lungs and the importance of myofibroblast to lipofibroblast transdifferentiation in lung regeneration. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Chen L, Acciani T, Le Cras T, Lutzko C, Perl AK. Dynamic regulation of platelet-derived growth factor receptor alpha expression in alveolar fibroblasts during realveolarization. Am J Respir Cell Mol Biol. 2012;47(4):517–27. doi: 10.1165/rcmb.2012-0030OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Tanjore H, Xu XC, Polosukhin VV, Degryse AL, Li B, Han W, et al. Contribution of epithelial-derived fibroblasts to bleomycin-induced lung fibrosis. Am J Respir Crit Care Med. 2009;180(7):657–65. doi: 10.1164/rccm.200903-0322OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Chen LJ, Ye H, Zhang Q, Li FZ, Song LJ, Yang J, et al. Bleomycin induced epithelial-mesenchymal transition (EMT) in pleural mesothelial cells. Toxicol Appl Pharmacol. 2015;283(2):75–82. doi: 10.1016/j.taap.2015.01.004. [DOI] [PubMed] [Google Scholar]
- 39.Kim KK, Kugler MC, Wolters PJ, Robillard L, Galvez MG, Brumwell AN, et al. Alveolar epithelial cell mesenchymal transition develops in vivo during pulmonary fibrosis and is regulated by the extracellular matrix. Proc Natl Acad Sci U S A. 2006;103(35):13180–5. doi: 10.1073/pnas.0605669103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Degryse AL, Tanjore H, Xu XC, Polosukhin VV, Jones BR, McMahon FB, et al. Repetitive intratracheal bleomycin models several features of idiopathic pulmonary fibrosis. Am J Physiol Lung Cell Mol Physiol. 2010;299(4):L442–52. doi: 10.1152/ajplung.00026.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Wu Z, Yang L, Cai L, Zhang M, Cheng X, Yang X, et al. Detection of epithelial to mesenchymal transition in airways of a bleomycin induced pulmonary fibrosis model derived from an alpha-smooth muscle actin-Cre transgenic mouse. Respir Res. 2007;8:1. doi: 10.1186/1465-9921-8-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Xu Y, Mizuno T, Sridharan A, Du Y, Guo M, Tang J, et al. Single-cell RNA sequencing identifies diverse roles of epithelial cells in idiopathic pulmonary fibrosis. JCI Insight. 2016;1(20):e90558. doi: 10.1172/jci.insight.90558. Utilizing single cell RNA sequencing, this study nicely shows the presence of basal-like cells in IPF lungs co-expressing mesenchymal markers. This is the first study to provide strong evidence for mesenchymal transcript expression in basal cells from IPF but not normal lung explants. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Sontake V, Shanmukhappa SK, DiPasquale BA, Reddy GB, Medvedovic M, Hardie WD, et al. Fibrocytes Regulate Wilms Tumor 1-Positive Cell Accumulation in Severe Fibrotic Lung Disease. J Immunol. 2015;195(8):3978–91. doi: 10.4049/jimmunol.1500963. This study nicely shows a novel role for fibrocytes, where these cells contribute to the activation of Whilms Tumor 1+ mesothelial cells in remodeled murine lungs. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Karki S, Surolia R, Hock TD, Guroji P, Zolak JS, Duggal R, et al. Wilms' tumor 1 (Wt1) regulates pleural mesothelial cell plasticity and transition into myofibroblasts in idiopathic pulmonary fibrosis. FASEB J. 2014;28(3):1122–31. doi: 10.1096/fj.13-236828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Zolak JS, Jagirdar R, Surolia R, Karki S, Oliva O, Hock T, et al. Pleural mesothelial cell differentiation and invasion in fibrogenic lung injury. Am J Pathol. 2013;182(4):1239–47. doi: 10.1016/j.ajpath.2012.12.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Mubarak KK, Montes-Worboys A, Regev D, Nasreen N, Mohammed KA, Faruqi I, et al. Parenchymal trafficking of pleural mesothelial cells in idiopathic pulmonary fibrosis. Eur Respir J. 2012;39(1):133–40. doi: 10.1183/09031936.00141010. [DOI] [PubMed] [Google Scholar]
- 47.Lama VN, Phan SH. The extrapulmonary origin of fibroblasts: stem/progenitor cells and beyond. Proc Am Thorac Soc. 2006;3(4):373–6. doi: 10.1513/pats.200512-133TK. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Phan SH. Genesis of the myofibroblast in lung injury and fibrosis. Proc Am Thorac Soc. 2012;9(3):148–52. doi: 10.1513/pats.201201-011AW. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Gomperts BN, Strieter RM. Fibrocytes in lung disease. J Leukoc Biol. 2007;82(3):449–56. doi: 10.1189/jlb.0906587. [DOI] [PubMed] [Google Scholar]
- 50.Herzog EL, Bucala R. Fibrocytes in health and disease. Exp Hematol. 2010;38(7):548–56. doi: 10.1016/j.exphem.2010.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Maharaj S, Shimbori C, Kolb M. Fibrocytes in pulmonary fibrosis: a brief synopsis. Eur Respir Rev. 2013;22(130):552–7. doi: 10.1183/09059180.00007713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Habiel DM, Hogaboam C. Heterogeneity in fibroblast proliferation and survival in idiopathic pulmonary fibrosis. Front Pharmacol. 2014;5:2. doi: 10.3389/fphar.2014.00002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Hashimoto N, Jin H, Liu T, Chensue SW, Phan SH. Bone marrow-derived progenitor cells in pulmonary fibrosis. J Clin Invest. 2004;113(2):243–52. doi: 10.1172/JCI18847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Epperly MW, Guo H, Gretton JE, Greenberger JS. Bone marrow origin of myofibroblasts in irradiation pulmonary fibrosis. Am J Respir Cell Mol Biol. 2003;29(2):213–24. doi: 10.1165/rcmb.2002-0069OC. [DOI] [PubMed] [Google Scholar]
- 55.Srour N, Thebaud B. Mesenchymal Stromal Cells in Animal Bleomycin Pulmonary Fibrosis Models: A Systematic Review. Stem Cells Transl Med. 2015;4(12):1500–10. doi: 10.5966/sctm.2015-0121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Chambers DC, Enever D, Ilic N, Sparks L, Whitelaw K, Ayres J, et al. A phase 1b study of placenta-derived mesenchymal stromal cells in patients with idiopathic pulmonary fibrosis. Respirology. 2014;19(7):1013–8. doi: 10.1111/resp.12343. [DOI] [PubMed] [Google Scholar]
- 57.Bucala R, Spiegel LA, Chesney J, Hogan M, Cerami A. Circulating fibrocytes define a new leukocyte subpopulation that mediates tissue repair. Mol Med. 1994;1(1):71–81. [PMC free article] [PubMed] [Google Scholar]
- 58.Schmidt M, Sun G, Stacey MA, Mori L, Mattoli S. Identification of circulating fibrocytes as precursors of bronchial myofibroblasts in asthma. J Immunol. 2003;171(1):380–9. doi: 10.4049/jimmunol.171.1.380. [DOI] [PubMed] [Google Scholar]
- 59.Phillips RJ, Burdick MD, Hong K, Lutz MA, Murray LA, Xue YY, et al. Circulating fibrocytes traffic to the lungs in response to CXCL12 and mediate fibrosis. J Clin Invest. 2004;114(3):438–46. doi: 10.1172/JCI20997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Shi Y, Ou L, Han S, Li M, Pena MM, Pena EA, et al. Deficiency of Kruppel-like factor KLF4 in myeloid-derived suppressor cells inhibits tumor pulmonary metastasis in mice accompanied by decreased fibrocytes. Oncogenesis. 2014;3:e129. doi: 10.1038/oncsis.2014.44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Ou L, Shi Y, Dong W, Liu C, Schmidt TJ, Nagarkatti P, et al. Kruppel-like factor KLF4 facilitates cutaneous wound healing by promoting fibrocyte generation from myeloid-derived suppressor cells. J Invest Dermatol. 2015;135(5):1425–34. doi: 10.1038/jid.2015.3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Fernandez IE, Greiffo FR, Frankenberger M, Bandres J, Heinzelmann K, Neurohr C, et al. Peripheral blood myeloid-derived suppressor cells reflect disease status in idiopathic pulmonary fibrosis. Eur Respir J. 2016;48(4):1171–83. doi: 10.1183/13993003.01826-2015. [DOI] [PubMed] [Google Scholar]
- 63.Trujillo G, Hartigan AJ, Hogaboam CM. T regulatory cells and attenuated bleomycin-induced fibrosis in lungs of CCR7−/− mice. Fibrogenesis Tissue Repair. 2010;3:18. doi: 10.1186/1755-1536-3-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Mehrad B, Burdick MD, Zisman DA, Keane MP, Belperio JA, Strieter RM. Circulating peripheral blood fibrocytes in human fibrotic interstitial lung disease. Biochem Biophys Res Commun. 2007;353(1):104–8. doi: 10.1016/j.bbrc.2006.11.149. [DOI] [PubMed] [Google Scholar]
- 65.Andersson-Sjoland A, de Alba CG, Nihlberg K, Becerril C, Ramirez R, Pardo A, et al. Fibrocytes are a potential source of lung fibroblasts in idiopathic pulmonary fibrosis. Int J Biochem Cell Biol. 2008;40(10):2129–40. doi: 10.1016/j.biocel.2008.02.012. [DOI] [PubMed] [Google Scholar]
- 66.Hogaboam CM, Murray L, Martinez FJ. Epigenetic mechanisms through which Toll-like receptor-9 drives idiopathic pulmonary fibrosis progression. Proc Am Thorac Soc. 2012;9(3):172–6. doi: 10.1513/pats.201201-002AW. [DOI] [PubMed] [Google Scholar]
- 67.Huang SK, Scruggs AM, McEachin RC, White ES, Peters-Golden M. Lung fibroblasts from patients with idiopathic pulmonary fibrosis exhibit genome-wide differences in DNA methylation compared to fibroblasts from nonfibrotic lung. PLoS One. 2014;9(9):e107055. doi: 10.1371/journal.pone.0107055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Sanders YY, Liu H, Scruggs AM, Duncan SR, Huang SK, Thannickal VJ. Epigenetic Regulation of Caveolin-1 Gene Expression in Lung Fibroblasts. Am J Respir Cell Mol Biol. 2017;56(1):50–61. doi: 10.1165/rcmb.2016-0034OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Xiao X, Senavirathna LK, Gou X, Huang C, Liang Y, Liu L. EZH2 enhances the differentiation of fibroblasts into myofibroblasts in idiopathic pulmonary fibrosis. Physiol Rep. 2016;4(17):e12915. doi: 10.14814/phy2.12915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Korfei M, Skwarna S, Henneke I, MacKenzie B, Klymenko O, Saito S, et al. Aberrant expression and activity of histone deacetylases in sporadic idiopathic pulmonary fibrosis. Thorax. 2015;70(11):1022–32. doi: 10.1136/thoraxjnl-2014-206411. [DOI] [PubMed] [Google Scholar]
- 71.Sanders YY, Liu H, Liu G, Thannickal VJ. Epigenetic mechanisms regulate NADPH oxidase-4 expression in cellular senescence. Free Radic Biol Med. 2015;79:197–205. doi: 10.1016/j.freeradbiomed.2014.12.008. [DOI] [PubMed] [Google Scholar]
- 72.O’Dwyer DN, Armstrong ME, Trujillo G, Cooke G, Keane MP, Fallon PG, et al. The Toll-like receptor 3 L412F polymorphism and disease progression in idiopathic pulmonary fibrosis. Am J Respir Crit Care Med. 2013;188(12):1442–50. doi: 10.1164/rccm.201304-0760OC. [DOI] [PubMed] [Google Scholar]
- 73.Hecker L, Logsdon NJ, Kurundkar D, Kurundkar A, Bernard K, Hock T, et al. Reversal of persistent fibrosis in aging by targeting Nox4-Nrf2 redox imbalance. Sci Transl Med. 2014;6(231):231ra47. doi: 10.1126/scitranslmed.3008182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Im J, Kim K, Hergert P, Nho RS. Idiopathic pulmonary fibrosis fibroblasts become resistant to Fas ligand-dependent apoptosis via the alteration of decoy receptor 3. J Pathol. 2016;240(1):25–37. doi: 10.1002/path.4749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Moodley YP, Misso NL, Scaffidi AK, Fogel-Petrovic M, McAnulty RJ, Laurent GJ, et al. Inverse effects of interleukin-6 on apoptosis of fibroblasts from pulmonary fibrosis and normal lungs. Am J Respir Cell Mol Biol. 2003;29(4):490–8. doi: 10.1165/rcmb.2002-0262OC. [DOI] [PubMed] [Google Scholar]
- 76.Scaffidi AK, Mutsaers SE, Moodley YP, McAnulty RJ, Laurent GJ, Thompson PJ, et al. Oncostatin M stimulates proliferation, induces collagen production and inhibits apoptosis of human lung fibroblasts. Br J Pharmacol. 2002;136(5):793–801. doi: 10.1038/sj.bjp.0704769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Ebener S, Barnowski S, Wotzkow C, Marti TM, Lopez-Rodriguez E, Crestani B, et al. Toll-like receptor 4 (TLR4) activation attenuates pro-fibrotic response in control lung fibroblasts but not in fibroblasts from IPF patients. Am J Physiol Lung Cell Mol Physiol. 2016 doi: 10.1152/ajplung.00119.2016. [DOI] [PubMed] [Google Scholar]
- 78.Meneghin A, Choi ES, Evanoff HL, Kunkel SL, Martinez FJ, Flaherty KR, et al. TLR9 is expressed in idiopathic interstitial pneumonia and its activation promotes in vitro myofibroblast differentiation. Histochem Cell Biol. 2008;130(5):979–92. doi: 10.1007/s00418-008-0466-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Trujillo G, Meneghin A, Flaherty KR, Sholl LM, Myers JL, Kazerooni EA, et al. TLR9 differentiates rapidly from slowly progressing forms of idiopathic pulmonary fibrosis. Sci Transl Med. 2010;2(57):57ra82. doi: 10.1126/scitranslmed.3001510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Chilosi M, Zamo A, Doglioni C, Reghellin D, Lestani M, Montagna L, et al. Migratory marker expression in fibroblast foci of idiopathic pulmonary fibrosis. Respir Res. 2006;7:95. doi: 10.1186/1465-9921-7-95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Kirillov V, Siler JT, Ramadass M, Ge L, Davis J, Grant G, et al. Sustained activation of toll-like receptor 9 induces an invasive phenotype in lung fibroblasts: possible implications in idiopathic pulmonary fibrosis. Am J Pathol. 2015;185(4):943–57. doi: 10.1016/j.ajpath.2014.12.011. [DOI] [PubMed] [Google Scholar]
- 82.Li Y, Jiang D, Liang J, Meltzer EB, Gray A, Miura R, et al. Severe lung fibrosis requires an invasive fibroblast phenotype regulated by hyaluronan and CD44. J Exp Med. 2011;208(7):1459–71. doi: 10.1084/jem.20102510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Ahluwalia N, Grasberger PE, Mugo BM, Feghali-Bostwick C, Pardo A, Selman M, et al. Fibrogenic Lung Injury Induces Non-Cell-Autonomous Fibroblast Invasion. Am J Respir Cell Mol Biol. 2016;54(6):831–42. doi: 10.1165/rcmb.2015-0040OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Cai GQ, Zheng A, Tang Q, White ES, Chou CF, Gladson CL, et al. Downregulation of FAK-related non-kinase mediates the migratory phenotype of human fibrotic lung fibroblasts. Exp Cell Res. 2010;316(9):1600–9. doi: 10.1016/j.yexcr.2010.01.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Suganuma H, Sato A, Tamura R, Chida K. Enhanced migration of fibroblasts derived from lungs with fibrotic lesions. Thorax. 1995;50(9):984–9. doi: 10.1136/thx.50.9.984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Shea BS, Tager AM. Role of the lysophospholipid mediators lysophosphatidic acid and sphingosine 1-phosphate in lung fibrosis. Proc Am Thorac Soc. 2012;9(3):102–10. doi: 10.1513/pats.201201-005AW. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Jun D, Garat C, West J, Thorn N, Chow K, Cleaver T, et al. The pathology of bleomycin-induced fibrosis is associated with loss of resident lung mesenchymal stem cells that regulate effector T-cell proliferation. Stem Cells. 2011;29(4):725–35. doi: 10.1002/stem.604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Leaf IA, Nakagawa S, Johnson BG, Cha JJ, Mittelsteadt K, Guckian KM, et al. Pericyte MyD88 and IRAK4 control inflammatory and fibrotic responses to tissue injury. J Clin Invest. 2016 doi: 10.1172/JCI87532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Chanda D, Kurundkar A, Rangarajan S, Locy M, Bernard K, Sharma NS, et al. Developmental Reprogramming in Mesenchymal Stromal Cells of Human Subjects with Idiopathic Pulmonary Fibrosis. Sci Rep. 2016;6:37445. doi: 10.1038/srep37445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Liang J, Zhang Y, Xie T, Liu N, Chen H, Geng Y, et al. Hyaluronan and TLR4 promote surfactant-protein-C-positive alveolar progenitor cell renewal and prevent severe pulmonary fibrosis in mice. Nat Med. 2016;22(11):1285–93. doi: 10.1038/nm.4192. [DOI] [PMC free article] [PubMed] [Google Scholar]