Abstract
Children and adolescents in the United States spend many hours in school. Students with chronic health conditions (CHCs) may face lower academic achievement, increased disability, fewer job opportunities, and limited community interactions as they enter adulthood. School health services provide safe and effective management of CHCs, often for students with limited access to health care. A systematic review to assess the role of school health services in addressing CHCs among students in Grades K–12 was completed using primary, peer-reviewed literature published from 2000 to 2015, on selected conditions: asthma, food allergies, diabetes, seizure disorders, and poor oral health. Thirty-nine articles met the inclusion criteria and results were synthesized; however, 38 were on asthma. Direct access to school nursing and other health services, as well as disease-specific education, improved health and academic outcomes among students with CHCs. Future research needs to include standardized definitions and data collection methods for students with CHCs.
Keywords: academic achievement, attendance, chronic diseases, school health, services, student health outcomes
Background
School health services may play a key role in managing the daily needs of students with chronic health conditions (CHCs). Although these health conditions can vary widely in concept and definition, CHCs are typically accepted as having potential for functional limitations, including dependency on medication, assistive devices, or routine medical care (van der Lee, Mokkink, Grootenhuis, Heymans, & Offringa, 2007). The school nurse or a designated provider is often responsible for coordinating and conducting health assessments, as well as planning and implementing individualized health-care plans for safe and effective management of CHCs, often for those who may have limited access to health care. These health services are designed to help with access or referrals by linking school staff, students, families, community, and health-care providers together to promote the health care of students in a healthy and safe school environment (Association for Supervision and Curriculum Development [ASCD] & Centers for Disease Control and Prevention [CDC], 2014). The school-based health center (SBHC) is another model that represents an important interdisciplinary approach to providing comprehensive physical and mental health care for students. SBHCs typically deliver primary care services and may include reproductive, dental, and acute care services for students and may also coordinate with external community providers (Brown & Bolen, 2008).
The purpose of this systematic review is to assess the role of school health services or SBHCs in addressing five CHCs among school-aged youth in Grades K–12: asthma, food allergy/anaphylaxis, diabetes, seizure disorders, and poor oral health. These are examples of conditions that are commonly seen, possibly affect academic achievement, or use significant resources when addressed at school. There are position and policy statements, guidance documents, tool kits as well as issue briefs from a number of organizations with expertise in this area; however, a synthesis of primary, peer-reviewed literature addressing CHCs in school settings is lacking (American Academy of Pediatrics, 2004, 2016, 2009, 2012; National Association of School Nurses, 2013, 2014). We examine the relationship between the provision of school health services (through either traditional school nursing or SBHCs) and the health and academic outcomes of students with CHCs.
Methods
A comprehensive literature search was conducted in the following medical, public health, and education databases for articles published during 2000–2015: ERIC, PubMed, Web of Science, and CINAHL (Cumulative Index to Nursing and Allied Health Literature). Examples of key words and phrases used included the following: asthma, food allergies, anaphylaxis, diabetes, seizure disorders, epilepsy, oral health, dental caries, dental pain, individual health plan, school nurse role, academic performance, grades, attendance, medical home, insurance, emergency care, inhaler, epinephrine, care coordination, and referrals. A comprehensive list of the key words and phrases is given in Table 1. Examples of health outcomes included clinical symptomatology and measurements (e.g., peak flow [PF], spirometry), well-being and quality of life, medication administration, compliance with individual care plans, and health-care utilization, including primary care, specialist care, and emergency department (ED) visits or hospitalizations. Academic outcomes included academic performance, attendance, grades, and standardized test scores.
Table 1.
Key Words for Chronic Health Conditions in School Settings.a
| School Health Services
| |||||
|---|---|---|---|---|---|
| Asthma | Allergy | Diabetes | Epilepsy | Oral Health | (For All Conditions) |
| Medication administration | Medication administration | Medication administration | Medication administration | Dental caries | Medical home |
| School nurse role | School nurse role | School nurse role | School nurse role | Dental abscess | Referrals |
| Management of | Management of | Management of | Management of | Tooth decay | Collaboration |
| In school | In school | In school | In school | Dental pain | Coordination |
| Individual health plan | Individual health plan | Individual health plan | Individual health plan | Sealants | Discrimination |
| Role of school staff | Role of school staff | Role of school staff | Role of school staff | Toothache | Guidance |
| Prevention | Prevention | Self-carry | Treatment | Dental hygiene | Counseling |
| Treatment | Treatment | Academic outcomes | Academic outcomes | Preventive dental care | Strategy |
| Self-carry | Self-carry | Grades | Grades | Preventive dental services | Transition planning |
| Inhaler | Academic outcomes | Attendance | Attendance | Oral health examination | Coordinated school health programs |
| Quick relief | Grades | Prevention | Seizure | School-based health centers | |
| Academic outcomes | Attendance | Type 1 | Seizure disorder | Medicaid | |
| Grades | Anaphylaxis | Type 2 | Diazepam | Leadership | |
| Attendance | Epi-Pen | Hypoglycemia | Academic achievement | Insurance | |
| Rescue inhaler | Epinephrine | Hyperglycemia | Emergency care | Policy | |
| Academic achievement | Academic achievement | Insulin | Primary care | ||
| Emergency care | Emergency care | Academic achievement | Case management | ||
| Emergency care | Care coordination | ||||
Key words were combined using school health services AND/OR selected chronic health condition AND condition-specific key words in corresponding columns, AND general key words in last column.
The search yielded a total of 2,438 abstracts. The abstracts were screened by two trained reviewers for the following inclusion criteria: U.S. based and published in English; original scientific study with student health or academic outcomes as noted above; applicability to school settings (i.e., public or private, Grades pre-Kindergarten–12; no stand-alone pre-Kindergarten programs); and describing one of the preselected CHCs (i.e., asthma, seizure disorders, diabetes, food allergies/anaphylaxis, or poor oral health). Duplicates were removed, and four articles could not be identified because of missing author or journal information. We excluded studies that only measured knowledge acquisition or behavioral changes in students or that did not have at least one clinical or academic outcome as an end point.
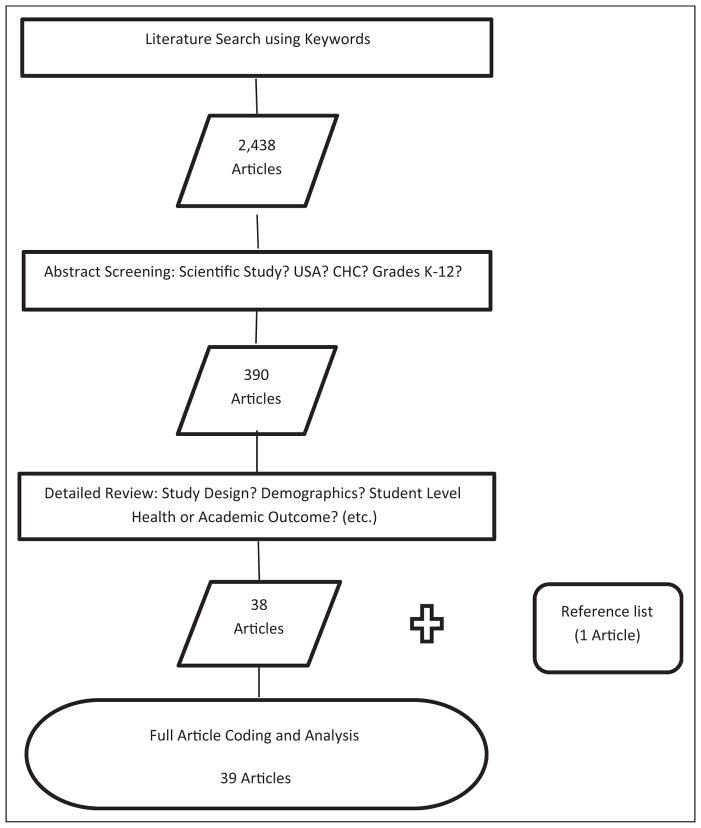
A stepwise process of selecting and assessing articles for synthesis followed. Initially, 390 abstracts met screening criteria for a full, detailed review, and one additional study from the reference list of one of these included articles was added to our review (Figure 1). An abstraction form was developed to summarize the following information from each article: purpose, study design, sample size, demographics (including measures of socioeconomic status), disease severity classification, geographic setting, methods, details of applicable interventions, outcome measures, data analysis, significant and nonsignificant results, limitations, and conclusions. Missing information was coded as not documented. Thirty-two articles were simultaneously reviewed by the authors and evaluated for concordance at each step of the process for quality control. Discordance was adjudicated by discussions with a third, senior reviewer. Subsequently, 352 articles were excluded for the following reasons: not original research studies, that is, guidelines, literature reviews, policy briefs, or commentaries (n = 89); not directly about school health services (n = 83); were descriptive studies (n = 69); did not measure student health or academic outcomes (n = 68); not specific to the CHCs being reviewed or targeted all students regardless of having condition (n = 14); not appropriate age or grade level (n = 11); were feasibility or validation studies (n = 7); were related to prevention trials (n = 6); or not U.S.-based studies (n = 5). Finally, 39 studies were eligible for synthesis of results (Figure 1). All information were entered into the Microsoft Excel 2013 database. The data abstraction form is available upon request from the lead author.
Figure 1.
Article classification system.
Results
We reviewed 39 articles that examined the effects of school health services on health or academic outcomes in children with the five selected CHCs: asthma, seizure disorders, diabetes, food allergies/anaphylaxis, or poor oral health. The vast majority focused on asthma (n = 38) and were in urban settings (n = 32). Only one study focused on oral health. Study designs varied, including 13 quasi-experimental, 12 longitudinal cohort (3 retrospective), 10 experimental (randomized controlled trials), 2 mixed methods (1 cohort and cross-sectional and 1 quasi-experimental and cross-sectional), 1 case–control, and 1 cross-sectional. Seventeen of the studies were in elementary schools, three in high schools, and eight addressed full K–12 populations; sample sizes ranged from 4 to 9,307 students. Socioeconomic status was not consistently documented: 17 studies documented free or reduced lunch data, including 13 with a population of 50% or higher free or reduced lunch, and 12 studies documented Medicaid/Children’s Health Insurance Plan (CHIP) in at least 50% or more of students.
Below are results from studies with statistically significant findings synthesized by study type for health outcomes and by type of academic achievement for academic outcomes. Results are summarized in order of study strength for those with statistically significant findings at the p ≤ .05 level; details for all studies in the review (including those without significant results) are presented in Table S1 which is available online.
Health Outcomes
Student-level health outcomes across the studies were categorized by clinical symptoms and measurements (26 studies), medical management (21 studies), and health-care utilization (25 studies). There were seven experimental, seven quasi-experimental, nine cohort, and four other study types.
Experimental Studies
Direct clinical interventions, such as providing medications or directly observed therapy (DOT) at school, led to improvements, including fewer symptom days, fewer days with activity limitations or change in family plans, fewer nighttime symptoms, decreased exhaled nitric oxide for students with asthma, decreased days using rescue inhalers, and a decrease in the likelihood of having three or more acute office or ED visits for asthma (Halterman et al., 2012; Halterman, Szilagyi, et al., 2011; Halterman et al., 2004).
Studies that focused on providing care coordination or case management (CM) saw mixed results. In one study, students in CM schools had significantly fewer urgent care or ED visits for each semester and during the entire school-year; they also had fewer hospital days (Levy, Heffner, Stewart, & Beeman, 2006). Conversely, another study showed that at 2 years, students in the control group (no CM) had fewer hospitalizations during the preceding 12 months (Bruzzese et al., 2006).
A comprehensive program that included case finding, clinical linkages, disease-specific education, and school environmental assessments found that both treatment and control groups showed an increase in being hospitalized over time. However, for a subgroup with direct access to study physicians (Table S1), the rate of increase was slowing more rapidly (Bartholomew et al., 2006). Additionally, a program using an asthma education curriculum for children and engaging caregivers showed reductions in day- and nighttime symptoms of asthma (Clark et al., 2004).
Quasi-Experimental Studies
A combination of education, providing medication, and DOT led to a larger increase in PF readings, fewer days with asthma symptoms, and more urgent medical visits in treatment students than in controls (Velsor-Friedrich, Pigott, & Louloudes, 2004). However, with the addition of nurse practitioner follow-up visits, both groups had PF increase over time with no significant differences between the groups (Velsor-Friedrich, Pigott, & Srof, 2005). Also, the provision of PF readings to health-care providers along with direct requests from school nurses led to an increase in asthma action plans placed on file for students (Pulcini, DeSisto, & McIntyre, 2007).
In a study to assess the effects of care provided at SBHCs there were 33% fewer ED visits after opening an SBHC, and students enrolled in the SBHC had 43% fewer ED visits compared to students not enrolled as well as a 2.4-fold decrease in the risk of hospitalization (Guo et al., 2005). There were also subsets of students in the SBHC group under the Managed Care Organization and CHIP program whose use of the ED decreased by 5.7% and 24.0%, respectively, versus other Medicaid students. Another study focused on case identification and screening of children with asthma found that younger children, those with a parent reported regular care asthma physician, those who had visited the ED during the past year, and those reporting more medication use were more likely to make a postreferral asthma visit (Yawn, Wollan, Scanlon, & Kurland, 2003). In addition, more children in this intervention group made an asthma-related visit and had higher rates of medication changes than in the control group.
Asthma education showed an improvement in the percentage of students who were in control of their asthma from baseline to second posttest at 14 weeks: from 56% to 76%, using the Asthma Control Test (Kouba et al., 2013). In a different study, a program teaching self-management of asthma led to improved inhaler skills for treatment students and significantly decreased hospital stays over time, when individual growth trajectories were considered (Horner & Brown, 2014). However, there were no differences between treatment and control groups.
Cohort Studies
Providing medications and a combination of DOT and motivational interviewing led to an overall reduction in asthma symptoms, an increase in symptom-free days, fewer days of slowing down or stopping usual activities, decreased rescue inhaler use, and decreased exhaled nitric oxide levels at a 2-month assessment versus baseline in a cohort of students with asthma (Halterman, Riekert, et al., 2011). An alternative method of providing direct care through mobile access was assessed in two studies. A comprehensive clinical approach that delivered services via two mobile “asthma vans” throughout the school-year and summer, with 24-hour on-call access to a physician, showed improved daytime and nighttime symptoms, exercise symptoms, pulmonary function tests, and rescue inhaler use from baseline. Moreover, 82% of children “felt better,” and ED visits and hospitalizations were decreased at follow-up (Patel et al., 2007). In a different program, children using a mobile asthma clinic for at least 1 year had ED visits decrease from 38% to 16%, multiple (≥2) ED visits decrease from 23% to 6%, and hospitalizations decrease from 19% to 3% (Liao, Morphew, Amaro, & Galant, 2006).
In a school where CM was instituted, intervention students in Years 1 and 2 of the program were more likely to have medications and PF measured at school during the following year; however, severity classifications of asthma both increased and decreased as a result of CM in Years 1–2 and 2–3 (Taras, Wright, Brennan, Campana, & Lofgren, 2004).
Education through the “Kickin’ Asthma” program—an asthma curriculum that focused on appropriate medication use and providing PF monitors and inhalers to students with asthma—was reported in two studies (Magzamen, Patel, Davis, Edelstein, & Tager, 2008; Patel Shrimali, Hasenbush, Davis, Tager, & Magzamen, 2011). Results included improved individual morbidity scores; a decrease in days with activity limitations and physician visits for asthma symptoms during 2 years; and a decrease in sleep disruption, ED use, and hospital visits during 3 years. Additionally, improvements were found across all three medication use categories: initiated reliever use when “feeling symptoms” and “before exercise” and initiated controller use when “feeling fine.” Other disease-specific educational efforts were also studied. One intervention using bilingual workshops for children and their families and providing asthma training workshops for school nurses led to decreased asthma morbidity days per week, decreased steroid use, decreased ED use (from 35% to 4%), and a decrease in hospitalization (from 11% to 2%; DePue et al., 2007). Another program using web-based education and an external organization to monitor students’ daily asthma diaries found a 34% decrease in nighttime symptoms and a 66% decrease in unscheduled physician visits at 6 months as well as a 69% decrease in daytime symptoms and 100% decrease in nighttime symptoms at 12 months (Tinkelman & Schwartz, 2004).
A study assessing SBHCs found that children attending the comparison schools without SBHCs were more likely than those in schools with SBHCs to have been hospitalized for asthma, 17.1% versus 10.5%, respectively (Webber et al., 2003). A follow-up study found improvements in medication management, reduced number of community provider visits, and halving of ED use for students enrolled in SBHCs compared to non-SBHC control schools (Webber et al., 2005).
Other Studies
In a case–control study, children at the Kunsberg School (Denver, Colorado), a specialized school for children with chronic medical conditions, showed a decrease in follow-up asthma visits by 76% and in ED visits by 55%, compared to controls (Anderson et al., 2004). Hospitalizations per year were also lower among children at Kunsberg, during post-enrollment versus preenrollment periods in the school. An at-risk subset of children with asthma at Kunsberg also saw a decrease in inpatient hospital days and the elimination of intensive care unit stays.
A study using mixed methods to assess the initiation of a school-based health center with special emphasis on asthma found a decrease in having to change family plans in their longitudinal population, increased specialist visits and decreased hospital admissions in their cross-sectional population, and decreased nighttime awakenings in both their longitudinal and cross-sectional populations (Lurie, Bauer, & Brady, 2001). In another mixed methods study, a comprehensive program that included asthma education for students with asthma, CM, and asthma training for staff showed that the odds of asthma being well controlled was 55% higher among intervention students than among comparison students in the quasi-experimental arm of the study (Rasberry et al., 2014). In the cross-sectional arm of the same study, pulmonary function tests improved at follow-up among poorly controlled asthma students; however, there was a decrease among well-controlled asthma students. In addition, descriptive frequencies showed 44.3% of students moved from the poorly to well-controlled classification, whereas 17.5% of students moved from the well- to poorly controlled classification.
A cross-sectional study that assessed SBHC adherence to National Heart, Lung, and Blood Institute (NHLBI) asthma care guidelines found that older children were more likely to have documented PF, more follow-up visits, and asthma education; there was also a nonsignificant trend toward increasing provider adherence (Oruwariye, Webber, & Ozuah, 2003). Oruwariye and colleagues also found that the use of PF meters was associated with a greater likelihood to having seen a specialist and to have had one or more ED visits during the preceding year.
Academic Outcomes
A total of 26 articles examined some component of academic performance as part of their outcome measures, including 9 experimental studies, 6 quasi-experimental studies, 9 cohort studies, 1 mixed methods (cohort and cross-sectional) study, and 1 cross-sectional study. Twenty-four studies included attendance alone, 4 included grades, and 2 included test scores. Some studies included more than one category (Table S1).
Attendance
Of 24 articles that examined attendance, 14 showed statistically significant (p < .05) reductions in school days missed and 5 described positive trends in attendance, despite either no significance testing or not reaching threshold; the remaining 5 studies showed no change at all. Interventions for those who showed positive changes in attendance included access to direct clinical services during the school day (13 studies) and asthma education curricula (e.g., “Kickin’ Asthma”, “Open Airways for Schools”) provided to students or their caregivers (6 studies). One study showed that gains in students with asthma who received school-based care were not maintained if they were exposed to second-hand cigarette smoke in the household (Halterman et al., 2004).
Grades
Four studies addressed grades. One intervention that focused on direct clinical services showed higher posttest grades for three subjects, but not in reading or math, among a subset of the student population that had physician access to develop an asthma action plan, obtain medication, and have a report sent to their community provider (Bartholomew et al., 2006). Engelke and colleagues showed a non-significant reduction in grade point average (GPA) among students who received CM. The largest average gain in GPA was when the goal of improving psychosocial support of the family was met; the largest decrease was when children did not meet the goal of disruptive classroom behavior (Engelke, Swanson, & Guttu, 2014).
Two interventions based on asthma education curricula showed improvement in grades. One study showed higher grades for science among children in the treatment group, but not for reading, mathematics, or physical education; the other study showed a positive change in GPA for students from sixth to eighth grade in the treatment group versus controls, in an overall picture of decline for all students (Clark et al., 2004, 2010).
Test scores
There were two studies that addressed standardized test scores. Bartholomew et al. (2006) found an improvement in state reading and writing test scores in their subset of students with direct physician access. Another study showed no difference in standardized test scores for English or math among students exposed to nursing CM versus controls (Moricca et al., 2013).
Discussion
Direct access to school nursing and other health services improved clinical outcomes and reduced absences among children with CHCs. Across several studies, improvements in clinical symptoms, medication adherence, and health-care utilization were seen when interventions, such as directly observed therapy, access to medications, and active retrieval of action plans from physicians (particularly for asthma), were implemented by school nursing staff.
There is a call for increasing the proportion of elementary, middle, and senior high schools that have a full-time, registered, school nurse to student ratio of at least 1:750 (HealthyPeople.gov). In addition, the American Academy of Pediatrics recently issued a policy statement recommending at least one full-time nurse in every school (Holmes et al., 2016). Over the past several decades, children with CHCs and complex health needs have been integrated into the general education system, in addition to being seen in special education settings (McClanahan & Weismuller, 2015). Children and adolescents in the United States spend many hours in school; thus, managing CHCs can present challenges for school systems, including educators, clinicians, and staff, who are in daily contact with students. CHCs early in life can adversely affect school performance—a reciprocal relationship between education and health may be reinforced, leading to greater disparities in each (Fiscella & Kitzman, 2009).
In many instances, disease-specific educational programs can provide knowledge and skills for students to better manage their CHCs, leading to better outcomes. The education programs in the studies reviewed typically focused on understanding developmentally appropriate physiology, prevention of behavioral or environmental factors that may trigger symptoms, how medications work, how students can stop symptoms from worsening, and when to ask adults for help. Programs with a culturally appropriate component for caregivers can also reinforce specific messages at home and in other settings.
Decreasing chronic absenteeism among students with CHCs has several merits. Daily attendance strongly affects standardized test scores as well as the graduation and dropout rates of students (Balfanz & Byrnes, 2012). Chronic absenteeism may lead to possible decreased job readiness, limited future earning potential, and decreased quality of life for these students. In addition, some schools are funded on the basis of average daily attendance; a decrease in funding based on chronic absenteeism among a fraction of the student body can have far-reaching consequences on resources that serve all students.
Limitations
There were several limitations noted in this review. First, there were very few studies that actually measured health and academic outcomes among students with the selected CHCs. Second, almost all studies looked at asthma and were typically in urban areas with low socioeconomic status; therefore, these interventions may not be generalizable to other conditions or settings. Third, there were many variations in data collection methods as well as measurements for health and academic outcomes. For example, if disease severity was assessed in asthma studies, some used the National Institutes of Health NHBLI definition, whereas others used severity indicated on the student’s asthma action plan by their primary health-care provider, and others relied on school nurse professional judgment. In addition, some studies had direct measurements, such as PF and spirometry, or had access to medical records, whereas others used symptom surveys and student or parent recall of health-care utilization within a defined time period. Absenteeism data were often recorded from student/parent surveys as “days missed” and seldom verified or linked directly to the specific CHC as the reason for absence. Fourth, there may have been additional factors that altered the impact of school-based interventions on student outcomes, such as environmental exposures, medication compliance, family engagement, access to primary or specialty care outside of the study, access to community organizations, or additional educational opportunities related to managing the CHC. Finally, in comprehensive programs that employ multiple modalities, such as direct clinical intervention and disease-specific education, we cannot determine the individual component that contributed to the change in student outcomes or if it must be delivered in combination.
School Nursing Implications
School nurses work across multiple systems, including education, health care, public health, insurance, and community agencies, to assure that student needs are met (McClanahan & Weismuller, 2015). Although inadequate staffing and time may impose barriers in school settings, leveraging community partnerships may help ease this burden, especially when working with local health plans, universities, or other organizations (Taras et al., 2004; Tinkelman & Schwartz, 2004).
This systematic review helps to identify effective interventions that school nurses can employ to support students with CHCs. Many studies addressed the positive effect of specific educational strategies for improving the health and well-being of students with asthma, which is clearly within the school nurse scope of practice. Of particular interest to school nurses is the demonstrated positive effect of having a comprehensive program for managing asthma, which includes CM (Rasberry et al., 2014). When it comes to care coordination, school nurses are uniquely poised to facilitate communication between schools and health-care providers, resulting in improved collaboration for medical management, including obtaining asthma action plans (Pulcini et al., 2007). Additionally, access to SBHCs can have significant implications for students with CHCs, particularly asthma. School nurses are in an ideal position to provide referrals to SBHCs and other community health providers, thus improving access to care and ensuring better chronic disease management overall. Additionally, school nurses could benefit from developing motivational interviewing skills, a strategy that was shown to improve asthma symptoms in students (Halterman, Riekert, et al., 2011).
Conclusion
Further research is needed to examine the relationship between addressing CHCs in school settings and student outcomes. In particular, studies are needed on school health service interventions that apply across many CHCs, as often there are universal approaches, despite condition-specific requirements. Many articles in our review were excluded because of their descriptive nature or lack of specific effects on student health or academic performance (versus intermediate end points such as changes in knowledge or behavior). Furthermore, the majority of the literature focuses on students with asthma. We need more accurate definitions of CHCs as well as systematic data collection methods at the student level, such as that being established through the nationwide Step Up and Be Counted initiative (Galemore & Maughan, 2014; Maughan et al., 2014; Selekman, Wolfe, & Cole, 2016). Recently, costs and prevalence of selected CHCs among school-aged children were estimated; however, this was based on national telephone survey data with inherent biases (Miller, Coffield, Leroy, & Wallin, 2016). A solid, data-driven evidence base can encourage resource allocation for school health services, increase capacity for prevention strategies at earlier stages, reduce morbidity, and create positive, long-term health and academic outcomes for students. Finally, this review points to the need for more research to study the effectiveness of care coordination activities and interventions that school nurses employ in managing a variety of student chronic health concerns. Current research is limited and focuses primarily on the management of asthma.
Supplementary Material
Acknowledgments
Funding
The author(s) received no financial support for the research, authorship, and/or publication of this article.
Biographies
Zanie C. Leroy, MD, MPH, is with the School Health Branch, Division of Population Health, Centers for Disease Control and Prevention, Atlanta, GA, USA.
Robin Wallin, DNP, RN, CPNP, NCSN, is with the Parkway School District, St. Louis, MO, USA.
Sarah Lee, PhD, is with the School Health Branch, Division of Population Health, Centers for Disease Control and Prevention, Atlanta, GA, USA
Footnotes
Author’s Note
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
Declaration of Conflicting Interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- Association for Supervision and Curriculum Development & Centers for Disease Control and Prevention. Whole school, whole community, whole child: A collaborative approach to learning and health. 2014 Retrieved May 16, 2016, from http://www.ascd.org/ASCD/pdf/siteASCD/publications/wholechild/wscc-a-collaborative-approach.pdf.
- American Academy of Pediatrics Committee on school health. School-based mental health services. Pediatrics. 2004;113:1839–1845. doi: 10.1542/peds.113.6.1839. [DOI] [PubMed] [Google Scholar]
- American Academy of Pediatrics Council on school health. Role of the school nurse in providing school health services. Pediatrics. 2016;137:e20160852. doi: 10.1542/peds.2016-0852. [DOI] [PubMed] [Google Scholar]
- American Academy of Pediatrics; Council on school health. Policy statement–guidance for the administration of medication in school. Pediatrics. 2009;124:1244–1251. doi: 10.1542/peds.2009-1953. [DOI] [PubMed] [Google Scholar]
- American Academy of Pediatrics; Council on school health. School-based health centers and pediatric practice. Pediatrics. 2012;129:387–393. doi: 10.1542/peds.2011-3443. [DOI] [PubMed] [Google Scholar]
- Anderson ME, Freas MR, Wallace AS, Kempe A, Gelfand EW, Liu AH. Successful school-based intervention for inner-city children with persistent asthma. Journal of Asthma. 2004;41:445–453. doi: 10.1081/jas-120033987. [DOI] [PubMed] [Google Scholar]
- Balfanz R, Byrnes V. The importance of being there: A report on absenteeism in the nation’s public schools. Baltimore, MD: Johns Hopkins Univesrity School of Education, Everyone Graduates Center, Get Schooled; 2012. pp. 1–46. [Google Scholar]
- Bartholomew LK, Sockrider M, Abramson SL, Swank PR, Czyzewski DI, Tortolero SR, … Tyrrell S. Partners in school asthma management: evaluation of a self-management program for children with asthma. Journal of School Health. 2006;76:283–290. doi: 10.1111/j.1746-1561.2006.00113.x. [DOI] [PubMed] [Google Scholar]
- Brown MB, Bolen LM. The school-based health center as a resource for prevention and health promotion. Psychology in the Schools. 2008;45:28–38. [Google Scholar]
- Bruzzese JM, Evans D, Wiesemann S, Pinkett-Heller M, Levison MJ, Du Y, … Mellins RB. Using school staff to establish a preventive network of care to improve elementary school students’ control of asthma. Journal of School Health. 2006;76:307–312. doi: 10.1111/j.1746-1561.2006.00118.x. [DOI] [PubMed] [Google Scholar]
- Clark NM, Brown R, Joseph CL, Anderson EW, Liu M, Valerio MA. Effects of a comprehensive school-based asthma program on symptoms, parent management, grades, and absenteeism. Chest. 2004;125:1674–1679. doi: 10.1378/chest.125.5.1674. [DOI] [PubMed] [Google Scholar]
- Clark NM, Shah S, Dodge JA, Thomas LJ, Andridge RR, Little RJ. An evaluation of asthma interventions for preteen students. Journal of School Health. 2010;80:80–87. doi: 10.1111/j.1746-1561.2009.00469.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DePue JD, McQuaid EL, Koinis-Mitchell D, Camillo C, Alario A, Klein RB. Providence school asthma partnership: School-based asthma program for inner-city families. Journal of Asthma. 2007;44:449–453. doi: 10.1080/02770900701421955. [DOI] [PubMed] [Google Scholar]
- Engelke MK, Swanson M, Guttu M. Process and outcomes of school nurse case management for students with asthma. Journal of School Nursing. 2014;30:196–205. doi: 10.1177/1059840513507084. [DOI] [PubMed] [Google Scholar]
- Fiscella K, Kitzman H. Disparities in academic achievement and health: The intersection of child education and health policy. Pediatrics. 2009;123:1073–1080. doi: 10.1542/peds.2008-0533. [DOI] [PubMed] [Google Scholar]
- Galemore CA, Maughan ED. Standardized dataset for school health services: Part 2 top to bottom. NASN School Nurse. 2014;29:187–192. doi: 10.1177/1942602x14536526. [DOI] [PubMed] [Google Scholar]
- Guo JJ, Jang R, Keller KN, McCracken AL, Pan W, Cluxton RJ. Impact of school-based health centers on children with asthma. Journal of Adolescent Health. 2005;37:266–274. doi: 10.1016/j.jadohealth.2004.09.006. [DOI] [PubMed] [Google Scholar]
- Halterman JS, Fagnano M, Montes G, Fisher S, Tremblay P, Tajon R, … Butz A. The school-based preventive asthma care trial: Results of a pilot study. Journal of Pediatrics. 2012;161:1109–1115. doi: 10.1016/j.jpeds.2012.05.059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Halterman JS, Riekert K, Bayer A, Fagnano M, Tremblay P, Blaakman S, Borrelli B. A pilot study to enhance preventive asthma care among urban adolescents with asthma. Journal of Asthma. 2011;48:523–530. doi: 10.3109/02770903.2011.576741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Halterman JS, Szilagyi PG, Fisher SG, Fagnano M, Tremblay P, Conn KM, … Borrelli B. Randomized controlled trial to improve care for urban children with asthma: Results of the School-Based Asthma Therapy trial. Archives of Pediatrics and Adolescent Medicine. 2011;165:262–268. doi: 10.1001/archpediatrics.2011.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Halterman JS, Szilagyi PG, Yoos HL, Conn KM, Kaczorowski JM, Holzhauer RJ, … McConnochie KM. Benefits of a school-based asthma treatment program in the absence of secondhand smoke exposure: Results of a randomized clinical trial. Archives of Pediatrics and Adolescent Medicine. 2004;158:460–467. doi: 10.1001/archpedi.158.5.460. [DOI] [PubMed] [Google Scholar]
- HealthyPeople.gov. Healthy People 2020. https://www.healthypeople.gov/2020/topics-objectives/topic/educational-and-community-based-programs/objectives.
- Holmes BW, Sheetz A, Allison M, Ancona R, Attisha E, Beers N, … Lerner M. Role of the school nurse in providing school health services. Pediatrics. 2016;137:e20160852. doi: 10.1542/peds.2016-0852. [DOI] [PubMed] [Google Scholar]
- Horner SD, Brown A. Evaluating the effect of an asthma self-management intervention for rural families. Journal of Asthma. 2014;51:168–177. doi: 10.3109/02770903.2013.855785. [DOI] [PubMed] [Google Scholar]
- Kouba J, Velsor-Friedrich B, Militello L, Harrison PR, Becklenberg A, White B, … Ahmed A. Efficacy of the I Can Control Asthma and Nutrition Now (ICAN) pilot program on health outcomes in high school students with asthma. Journal of School Nursing. 2013;29:235–247. doi: 10.1177/1059840512466110. [DOI] [PubMed] [Google Scholar]
- Levy M, Heffner B, Stewart T, Beeman G. The efficacy of asthma case management in an urban school district in reducing school absences and hospitalizations for asthma. Journal of School Health. 2006;76:320–324. doi: 10.1111/j.1746-1561.2006.00120.x. [DOI] [PubMed] [Google Scholar]
- Liao O, Morphew T, Amaro S, Galant SP. The Breathmobile: A novel comprehensive school-based mobile asthma care clinic for urban underprivileged children. Journal of School Health. 2006;76:313–319. doi: 10.1111/j.1746-1561.2006.00119.x. [DOI] [PubMed] [Google Scholar]
- Lurie N, Bauer EJ, Brady C. Asthma outcomes at an inner-city school-based health center. Journal of School Health. 2001;71:9–16. doi: 10.1111/j.1746-1561.2001.tb06481.x. [DOI] [PubMed] [Google Scholar]
- Magzamen S, Patel B, Davis A, Edelstein J, Tager IB. “Kickin’ Asthma”: School-based asthma education in an Urban Community. Journal of School Health. 2008;78:655–665. doi: 10.1111/j.1746-1561.2008.00362.x. [DOI] [PubMed] [Google Scholar]
- Maughan ED, Johnson KH, Bergren MD, Wolfe LC, Cole M, Pontius DJ, … Patrick K. Standardized data set for school health services: Part 1–getting to big data. NASN School Nurse. 2014;29:182–186. doi: 10.1177/1942602x14538414. [DOI] [PubMed] [Google Scholar]
- McClanahan R, Weismuller PC. School nurses and care coordination for children with complex needs: An integrative review. Journal of School Nursing. 2015;31:34–43. doi: 10.1177/1059840514550484. [DOI] [PubMed] [Google Scholar]
- Miller GF, Coffield E, Leroy Z, Wallin R. Prevalence and costs of five chronic conditions in children. Journal of School Nursing. 2016;32:357–364. doi: 10.1177/1059840516641190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moricca ML, Grasska MA, Marthaler BM, Morphew T, Weismuller PC, Galant SP. School asthma screening and case management: Attendance and learning outcomes. Journal of School Nursing. 2013;29:104–112. doi: 10.1177/1059840512452668. [DOI] [PubMed] [Google Scholar]
- National Association of School Nurses. Coordinated school health. Washington, DC: National Association of School Nurses; 2013. [Google Scholar]
- National Association of School Nurses. Transition planning for students with chronic health conditons. Washington, DC: National Association of School Nurses; 2014. [Google Scholar]
- Oruwariye T, Webber MP, Ozuah P. Do school-based health centers provide adequate asthma care? Journal of School Health. 2003;73:186–190. doi: 10.1111/j.1746-1561.2003.tb03601.x. [DOI] [PubMed] [Google Scholar]
- Patel B, Sheridan P, Detjen P, Donnersberger D, Gluck E, Malamut K, … Qing H. Success of a comprehensive school-based asthma intervention on clinical markers and resource utilization for inner-city children with asthma in Chicago: The Mobile C.A.R.E. Foundation’s asthma management program. Journal of Asthma. 2007;44:113–118. doi: 10.1080/02770900601182343. [DOI] [PubMed] [Google Scholar]
- Patel Shrimali B, Hasenbush A, Davis A, Tager I, Magzamen S. Medication use patterns among urban youth participating in school-based asthma education. Journal of Urban Health. 2011;88:73–84. doi: 10.1007/s11524-010-9475-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pulcini J, DeSisto MC, McIntyre CL. An intervention to increase the use of Asthma Action Plans in schools: A MASNRN study. Journal of School Nursing. 2007;23:170–176. doi: 10.1622/1059-8405(2007)023[0170:AITITU]2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- Rasberry CN, Cheung K, Buckley R, Dunville R, Daniels B, Cook D, … Dean B. Indicators of asthma control among students in a rural, school-based asthma management program. Journal of Asthma. 2014;51:876–885. doi: 10.3109/02770903.2014.913620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Selekman J, Wolfe LC, Cole M. What data do states collect related to school nurses, school health, and the health care provided? Journal of School Nursing. 2016;32:209–220. doi: 10.1177/1059840515606786. [DOI] [PubMed] [Google Scholar]
- Taras H, Wright S, Brennan J, Campana J, Lofgren R. Impact of school nurse case management on students with asthma. Journal of School Health. 2004;74:213–219. doi: 10.1111/j.1746-1561.2004.tb07935.x. [DOI] [PubMed] [Google Scholar]
- Tinkelman D, Schwartz A. School-based asthma disease management. Journal of Asthma. 2004;41:455–462. doi: 10.1081/jas-120033988. [DOI] [PubMed] [Google Scholar]
- van der Lee JH, Mokkink LB, Grootenhuis MA, Heymans HS, Offringa M. Definitions and measurement of chronic health conditions in childhood: A systematic review. Journal of the American Medical Association. 2007;297:2741–2751. doi: 10.1001/jama.297.24.2741. [DOI] [PubMed] [Google Scholar]
- Velsor-Friedrich B, Pigott T, Srof B. A practitioner-based asthma intervention program with African American inner-city school children. Journal of Pediatric Health Care. 2005;19:163–171. doi: 10.1016/j.pedhc.2004.12.002. [DOI] [PubMed] [Google Scholar]
- Velsor-Friedrich B, Pigott TD, Louloudes A. The effects of a school-based intervention on the self-care and health of African-American inner-city children with asthma. Journal of Pediatric Nursing. 2004;19:247–256. doi: 10.1016/j.pedn.2004.05.007. [DOI] [PubMed] [Google Scholar]
- Webber MP, Carpiniello KE, Oruwariye T, Lo Y, Burton WB, Appel DK. Burden of asthma in inner-city elementary schoolchildren: Do school-based health centers make a difference? Archives of Pediatrics and Adolescent Medicine. 2003;157:125–129. doi: 10.1001/archpedi.157.2.125. [DOI] [PubMed] [Google Scholar]
- Webber MP, Hoxie AM, Odlum M, Oruwariye T, Lo Y, Appel D. Impact of asthma intervention in two elementary school-based health centers in the Bronx. New York City Pediatric Pulmonology. 2005;40:487–493. doi: 10.1002/ppul.20307. [DOI] [PubMed] [Google Scholar]
- Yawn BP, Wollan P, Scanlon PD, Kurland M. Outcome results of a school-based screening program for under-treated asthma. Annals of Allergy, Asthma & Immunology. 2003;90:508–515. doi: 10.1016/s1081-1206(10)61844-3. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.